Megaloplastic Anaemia
Dr. Mohamed Ghalib
Internal Medicine
TUCOM
Objectives
1- Define megaloblastic anemia.
2- Identify the metabolism of vitamin B12.
3- Identify the causes of vitamin B12
deficiency.
4- Identify the metabolism of folic acid.
5- Identify the causes of folic acid
deficiency.
6- Identify the clinical features of
megaloblastic anemia.
7- Identify the investigations of
megaloblastic anemia.
8- Recognize the treatment of
megaloblastic anemia
.
Definition of Anaemia
Greek term for “no blood”
Term used to refer to a shortage of
red blood cells (RBC) or a reduction
in their haemaglobin (Hb) content.
Hb is a molecule in RBCs that
carries oxygen.
May be due to low red cell mass, or
increased plasma volume (eg.
pregnancy)
Male <13.5 g/dL
Female <11.5g/dL
Erythropoeisis
RBCs develop in the bone marrow
as stem cells, then evolve into
erythroblasts.
Erythropoeitin (EPO) is a hormone
secreted (90%) from proximal renal
tubules.
EPO stimulates stem cells in the
bone marrow to
RBC production.
Iron essential in latter phase as Hb
incorporated into reticulocytes and
released into circulation as RBCs
2/3
rds
of iron in the body is in Hb
Classification of Anaemia
Mean cell volume (MCV)
average size of one RBC
Microcytic MCV < 80
Normocytic 80 - 100
Macrocytic > 100
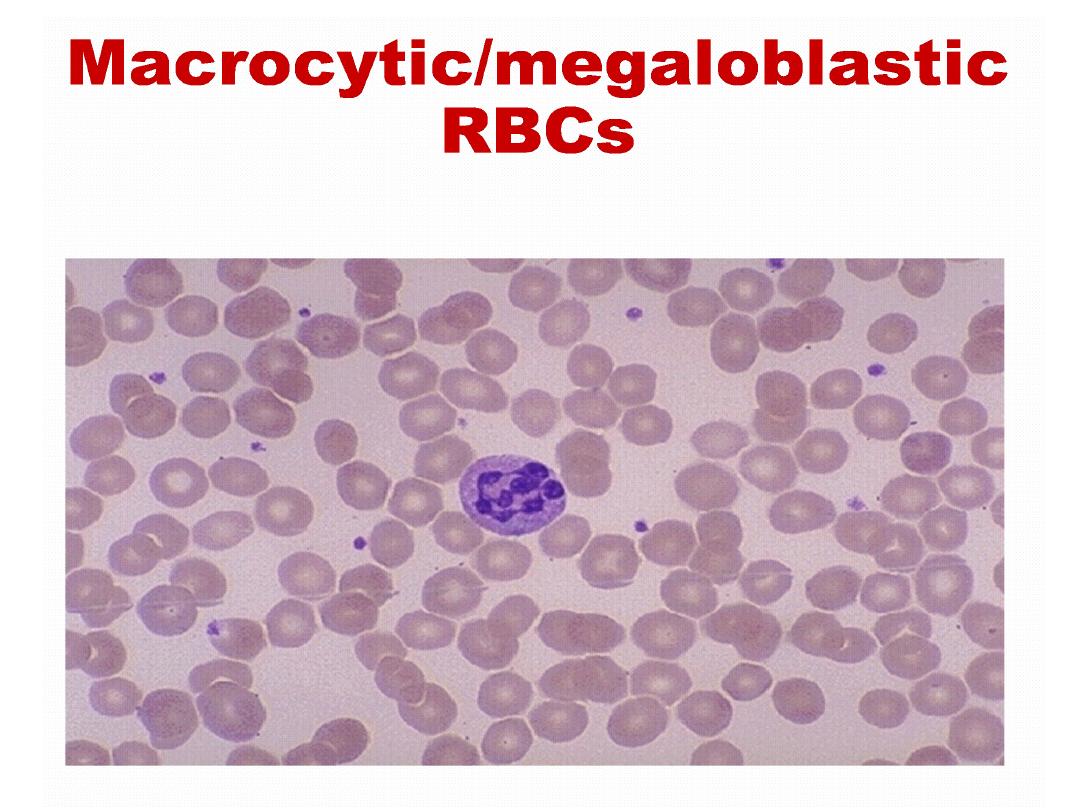
Define Megaloplastic Anemia
Megaloblastic anemias result from a block
in the synthesis of critical nucleotide
precursors of DNA, which leads to a cell
cycle arrest in S phase. Cytoplasmic
maturation occurs, but maturation of the
nucleus is arrested. Cells take on a bizarre
appearance, with large immature nuclei
surrounded by more mature-appearing
cytoplasm.
Interference
with
DNA
synthesis affects all rapidly dividing cells,
so patients with megaloblastic syndromes
often
have
pancytopenia
and
gastrointestinal
symptoms
such
as
diarrhea and malabsorption
.
This results from a deficiency of vitamin
B
12
or folic acid, or from disturbances
in folic acid metabolism. Folate is an
important substrate of, and vitamin B
12
a co-factor for, the generation of the
essential amino acid methionine from
homocysteine. This reaction produces
tetrahydrofolate, which is converted to
thymidine
monophosphate
for
incorporation into DNA. Deficiency of
either vitamin B
12
or folate will
therefore produce high plasma levels
of homocysteine and impaired DNA
synthesis.
All
proliferating
cells
will
exhibit
megaloblastosis;
hence
changes
are
evident in the buccal mucosa, tongue,
small intestine, cervix, vagina and uterus.
The high proliferation rate of bone marrow
results
in
striking
changes
in
the
haematopoietic system in megaloblastic
anaemia. Cells become arrested in
development and die within the marrow;
this ineffective erythropoiesis results in an
expanded
hypercellular
marrow.
The
megaloblastic changes are most evident in
the early nucleated red cell precursors,
and haemolysis within the marrow results
in
a
raised
bilirubin
and
lactate
dehydrogenase (LDH), but without the
reticulocytosis characteristic of other forms
of haemolysis.
Iron stores are usually raised. The
mature red cells are large and oval,
and sometimes contain nuclear
remnants. Nuclear changes are
seen in the immature granulocyte
precursors and a characteristic
appearance
is
that
of
„giant‟
metamyelocytes
with
a
large
„sausage-shaped‟ nucleus. The
mature
neutrophils
show
hypersegmentation of their nuclei,
with cells having six or more nuclear
lobes. If severe, a pancytopenia may
be present in the peripheral blood.
Macrocytic
B12 or folate deficiency
Alcohol excess or liver disease
Reticulocytosis (eg. With
haemolysis)
Cytotoxics
Myelodysplastic syndromes
Marrow infiltration
Anti-folate drugs (eg. Phenytoin)
Hypothyroid
Cobalamin Metabolism
Cobalamin (vitamin B
12
)is absorbed from
animal protein in the diet.
The process of cobalamin absorption and
metabolism is complex because cobalamin
is always bound to other proteins.
In the stomach, protein-bound vitamins are
released by digestion with pepsin and are
bound to haptocorrin (transcobalamin I).
Within the proximal duodenum, pancreatic
proteases digest cobalamin away from
haptocorrin, and cobalamin binds to
intrinsic factor (IF), also known as
transcobalamin III.
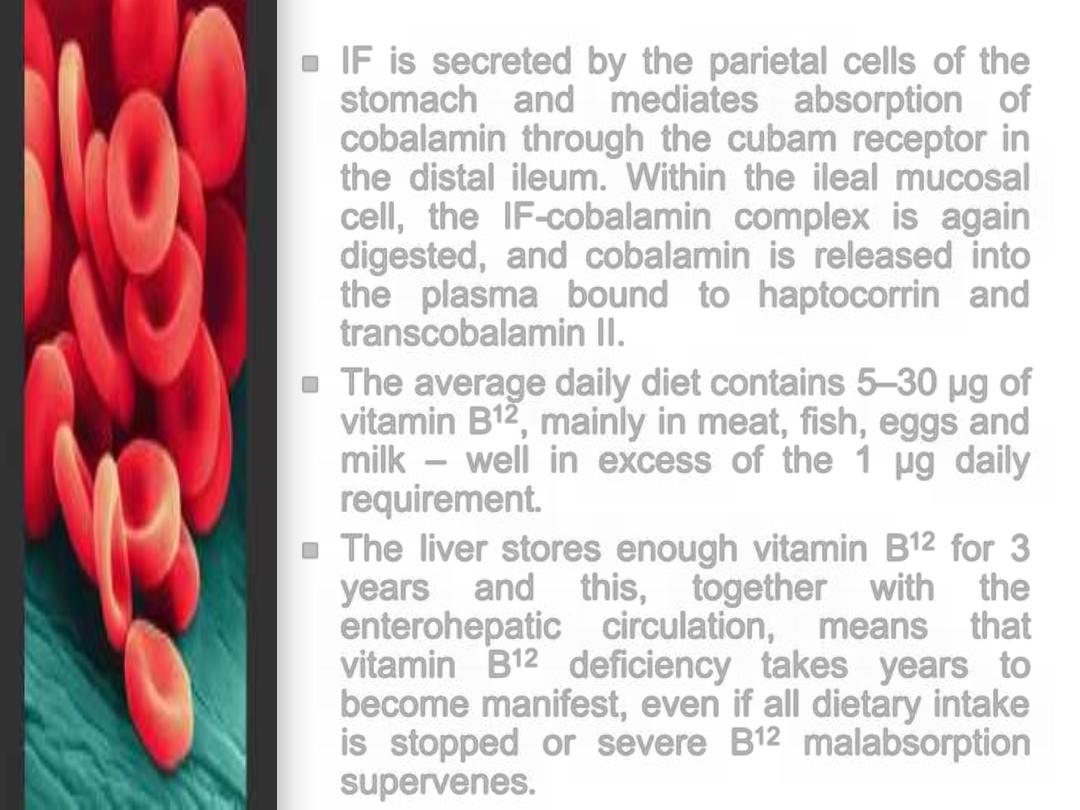
IF is secreted by the parietal cells of the
stomach and mediates absorption of
cobalamin through the cubam receptor in
the distal ileum. Within the ileal mucosal
cell, the IF-cobalamin complex is again
digested, and cobalamin is released into
the plasma bound to haptocorrin and
transcobalamin II.
The average daily diet contains 5
–30 µg of
vitamin B
12
, mainly in meat, fish, eggs and
milk
– well in excess of the 1 µg daily
requirement.
The liver stores enough vitamin B
12
for 3
years
and
this,
together
with
the
enterohepatic circulation, means that
vitamin B
12
deficiency takes years to
become manifest, even if all dietary intake
is stopped or severe B
12
malabsorption
supervenes.
Folates Metabolism
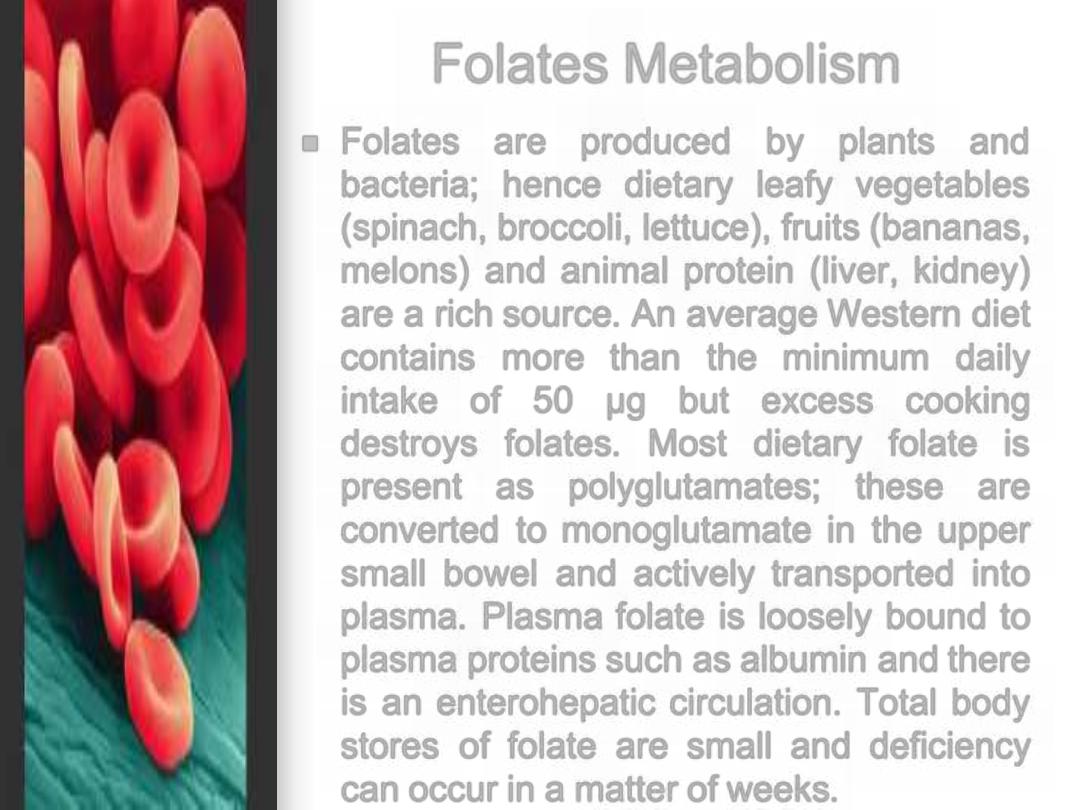
Folates are produced by plants and
bacteria; hence dietary leafy vegetables
(spinach, broccoli, lettuce), fruits (bananas,
melons) and animal protein (liver, kidney)
are a rich source. An average Western diet
contains more than the minimum daily
intake of 50
µg but excess cooking
destroys folates. Most dietary folate is
present as polyglutamates; these are
converted to monoglutamate in the upper
small bowel and actively transported into
plasma. Plasma folate is loosely bound to
plasma proteins such as albumin and there
is an enterohepatic circulation. Total body
stores of folate are small and deficiency
can occur in a matter of weeks.
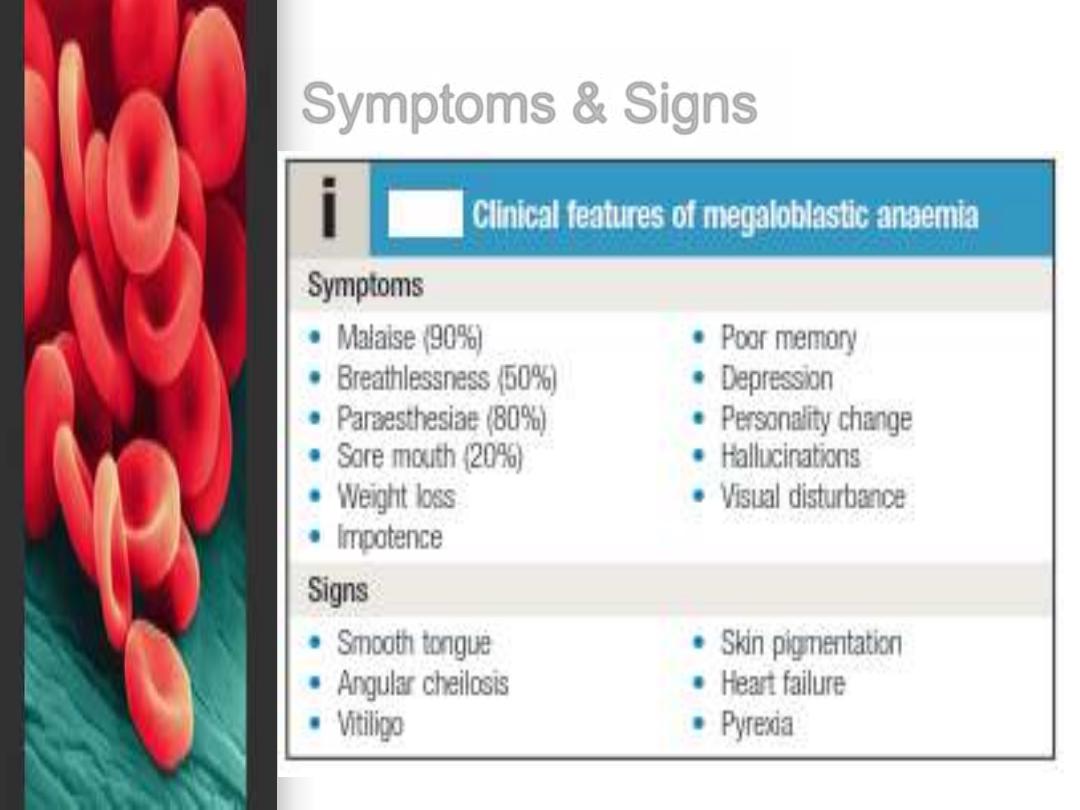
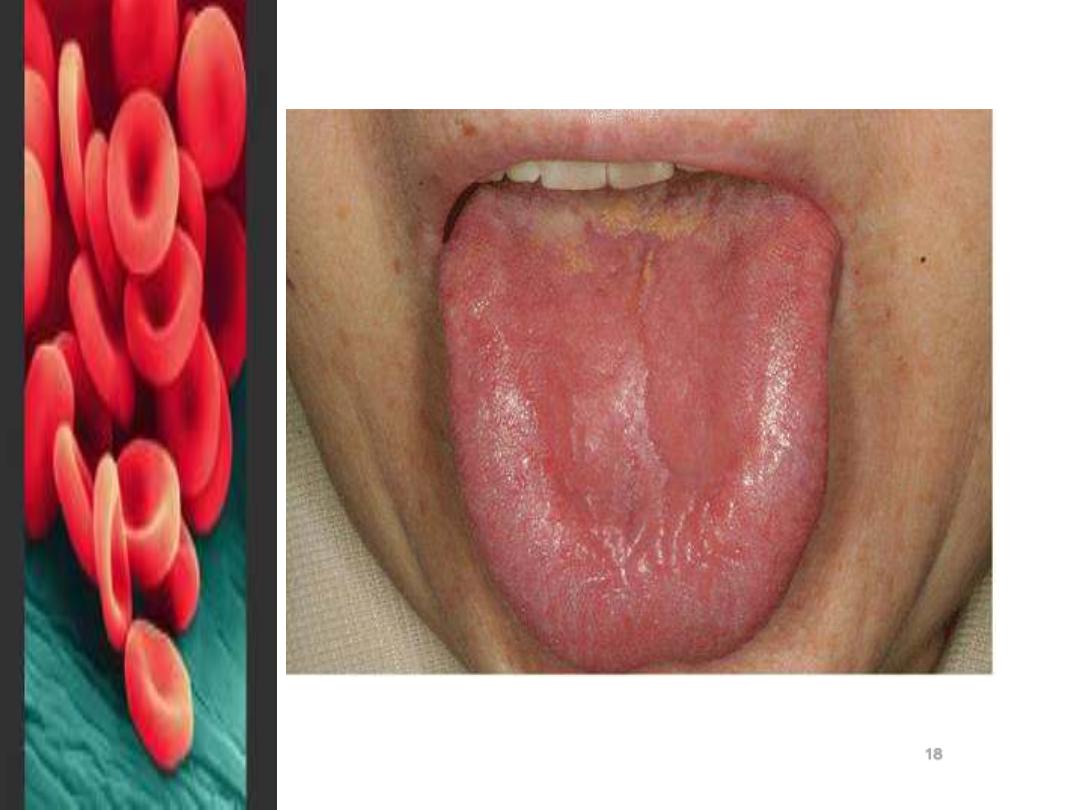
Symptoms & Signs
18
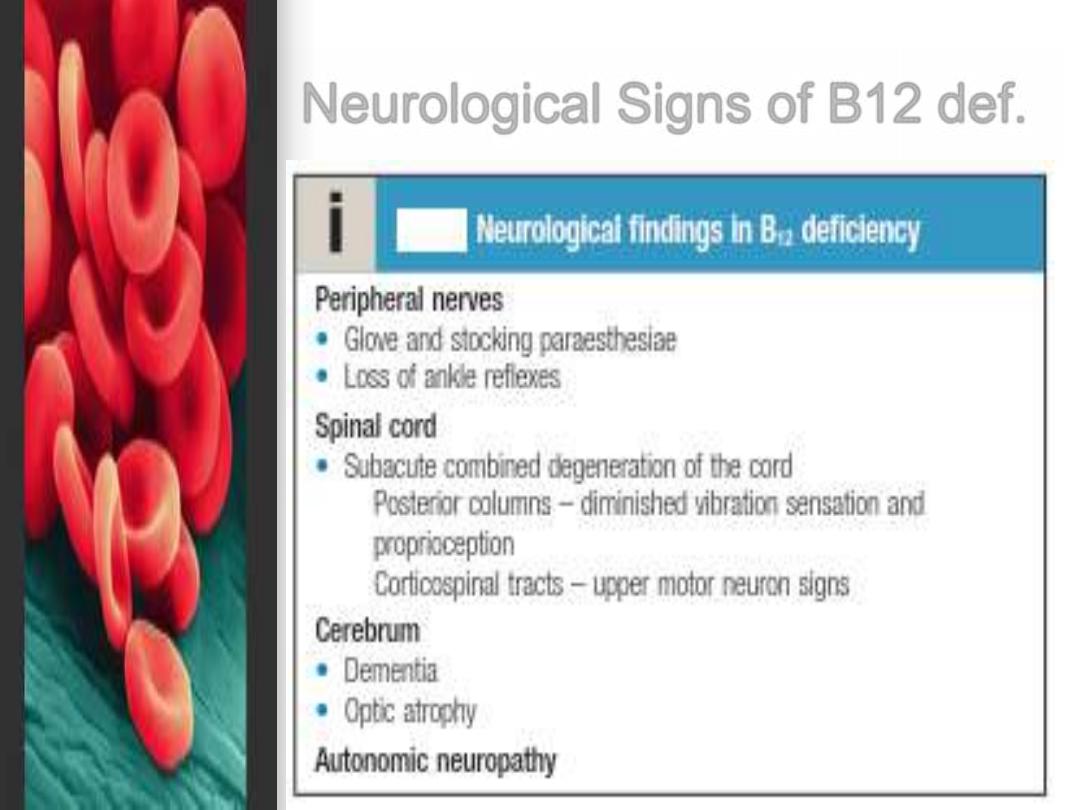
Neurological Signs of B12 def.
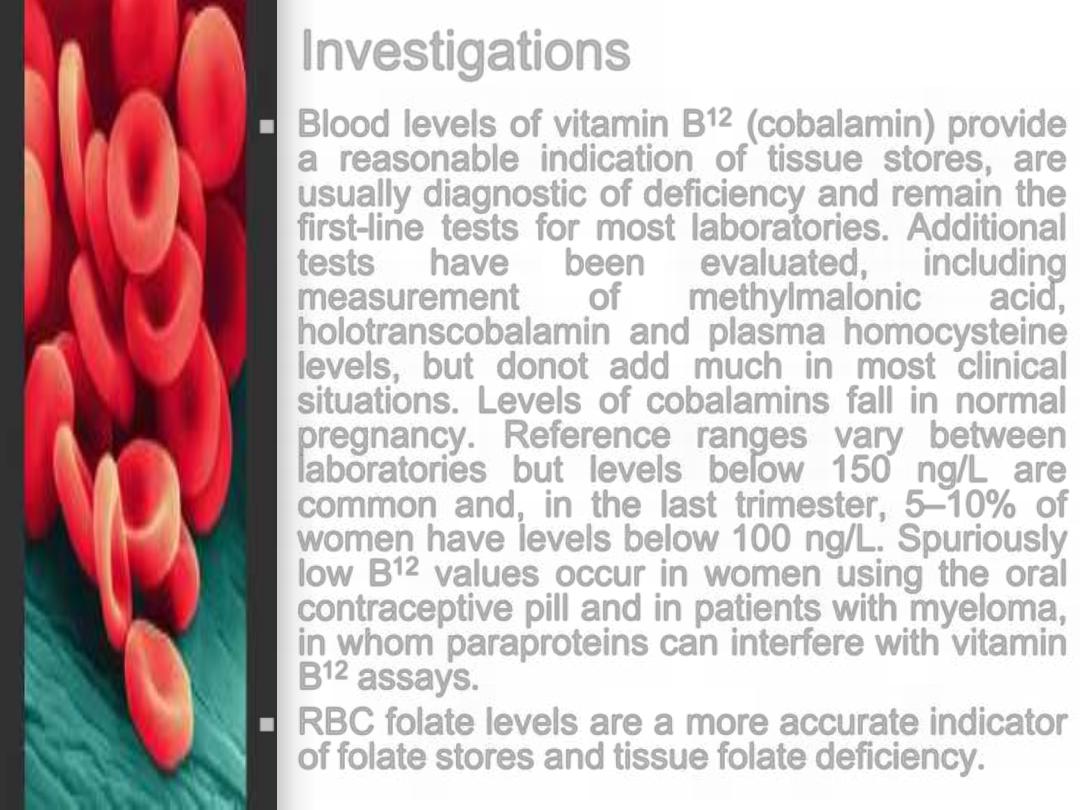
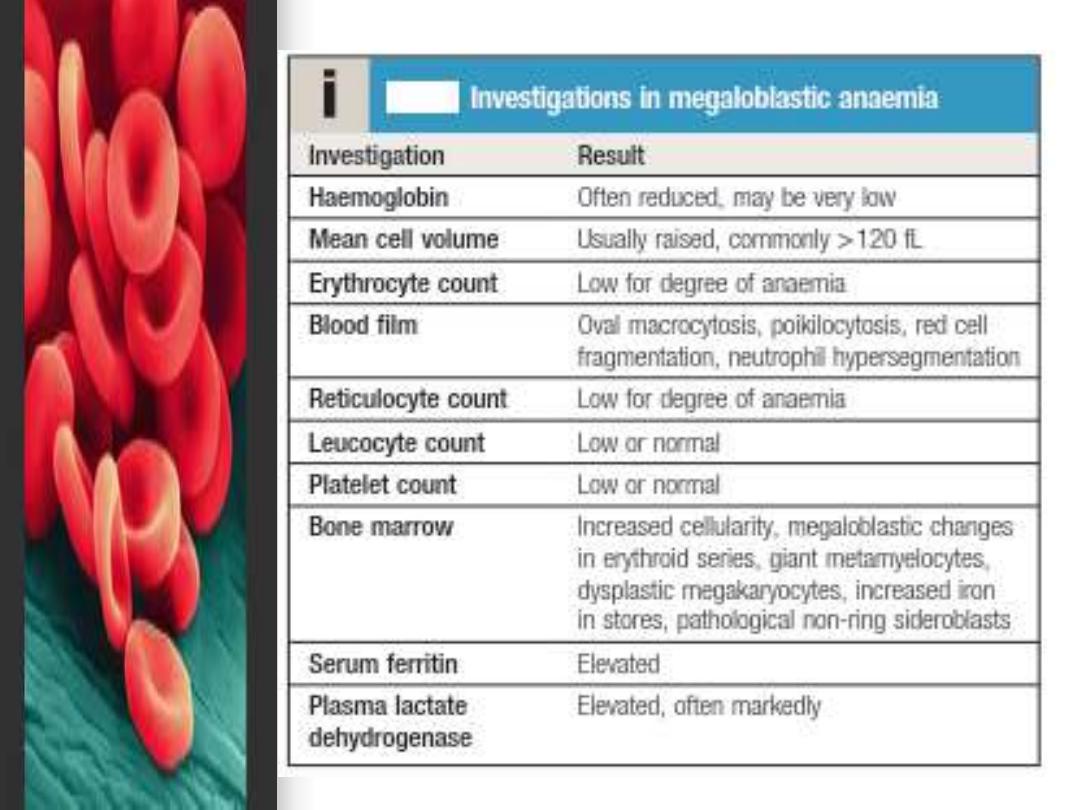
Investigations
Blood levels of vitamin B
12
(cobalamin) provide
a reasonable indication of tissue stores, are
usually diagnostic of deficiency and remain the
first-line tests for most laboratories. Additional
tests
have
been
evaluated,
including
measurement
of
methylmalonic
acid,
holotranscobalamin and plasma homocysteine
levels, but donot add much in most clinical
situations. Levels of cobalamins fall in normal
pregnancy. Reference ranges vary between
laboratories but levels below 150 ng/L are
common and, in the last trimester, 5
–10% of
women have levels below 100 ng/L. Spuriously
low B
12
values occur in women using the oral
contraceptive pill and in patients with myeloma,
in whom paraproteins can interfere with vitamin
B
12
assays.
RBC folate levels are a more accurate indicator
of folate stores and tissue folate deficiency.
Treatment
If a patient with a severe megaloblastic
anaemia is very ill and treatment must be
started before vitamin B
12
and red cell folate
results are available, that treatment should
always include both folic acid and vitamin
B
12
. The use of folic acid alone in the
presence of vitamin B
12
deficiency may
result in worsening of neurological features.
Rarely, if severe angina or heart failure is
present, transfusion can be used in
megaloblastic anaemia.
Treatment of B12 Deficiency
Vitamin B
12
deficiency is treated with
hydroxycobalamin.
In cases of uncomplicated deficiency, 1000
µg im for 6 doses 2 or 3 days apart, followed
by maintenance therapy of 1000
µg every 3
months for life, is recommended.
In the presence of neurological involvement,
a dose of 1000
µg on alternate days until
there is no further improvement, followed by
maintenance as above, is recommended.
The reticulocyte count will peak by
the 5th
–10th day after starting
replacement therapy.
The haemoglobin will rise by 10 g/l
every week until normalised.
A sensory neuropathy may take 6
–
12 months to correct; long-standing
neurological
damage
may
not
improve.
Treatment of Folate deficiency
Oral folic acid (5 mg daily for 3 weeks) will
treat acute deficiency and 5 mg once
weekly is adequate maintenance therapy.
Prophylactic folic acid in pregnancy
prevents megaloblastosis in women at risk,
and reduces the risk of fetal neural tube
defects.
Prophylactic supplementation is also given
in chronic haematological disease
associated with reduced red cell lifespan
(e.g. haemolytic anaemias).
There
is
some
evidence
that
supraphysiological supplementation (400
µg/day) can reduce the risk of coronary
and cerebrovascular disease by lowering
plasma homocysteine levels. This has led
the US Food and Drug Administration to
introduce fortification of bread, flour and
rice with folic acid.

Thanks
