
P a g e | 1 UTI G:E
URINARY TRACT INFECTION :
is an inflammatory response of the
urothelium to bacterial invasion that is usually associated with bacteriuria
and pyuria.
BACTERIURIA: IS THE PRESENCE OF BACTERIA IN THE URINE,
WHICH IS NORMALLY FREE OF BACTERIA (SYMPTOMATIC OR
ASYMPTOMATIC) BACTERIURIA WITHOUT PYURIA INDICATES
BACTERIAL COLONIZATION RATHER THAN INFECTION
Pyuria: is the presence of white blood cells (WBCs) in the urine. Pyuria
without bacteriuria warrants evaluation for tuberculosis, stones, or cancer.
Uncomplicated INFECTION: an infection in a healthy patient with a
structurally and functionally normal urinary tract
Complicated describes an infection in a patient who is compromised and/or
has a urinary tract with a structural or functional abnormality that would
increase the chance for acquiring infection and/or reduce the efficacy of
therapy
CLASSIFICATION: UTI CAN BE DIVIDED INTO THREE CATEGORIES:
(1)
isolated infections: First infections or those isolated from previous
infections by at least 6 months (occur in 25% to 30% of women between
the ages of 30 and 40 years, but these occur infrequently in men with a
normal urinary tract)
(2) unresolved infections: if any of the bacteria that caused the infection are
present in the urine during therapy (i.e. urine culture is positive during or
after the course of treatment) the bacteria have not been eradicated (i.e.
unresolved) The most common cause is that the infecting organisms are
resistant to the antimicrobial agent selected to treat the infection.
(3) RECURRENT INFECTIONS: (THE URINE CULTURE MUST SHOW NO
GROWTH AFTER THE PRECEDING INFECTION.) ARE DUE TO
EITHER REINFECTION OR BACTERIAL PERSISTENCE.
a. Reinfection: is recurrent infection with different bacteria from outside
the urinary tract (More than 95% of all recurrent infections in females
are reinfections of the urinary tract)
P a g e | 2 UTI G:E
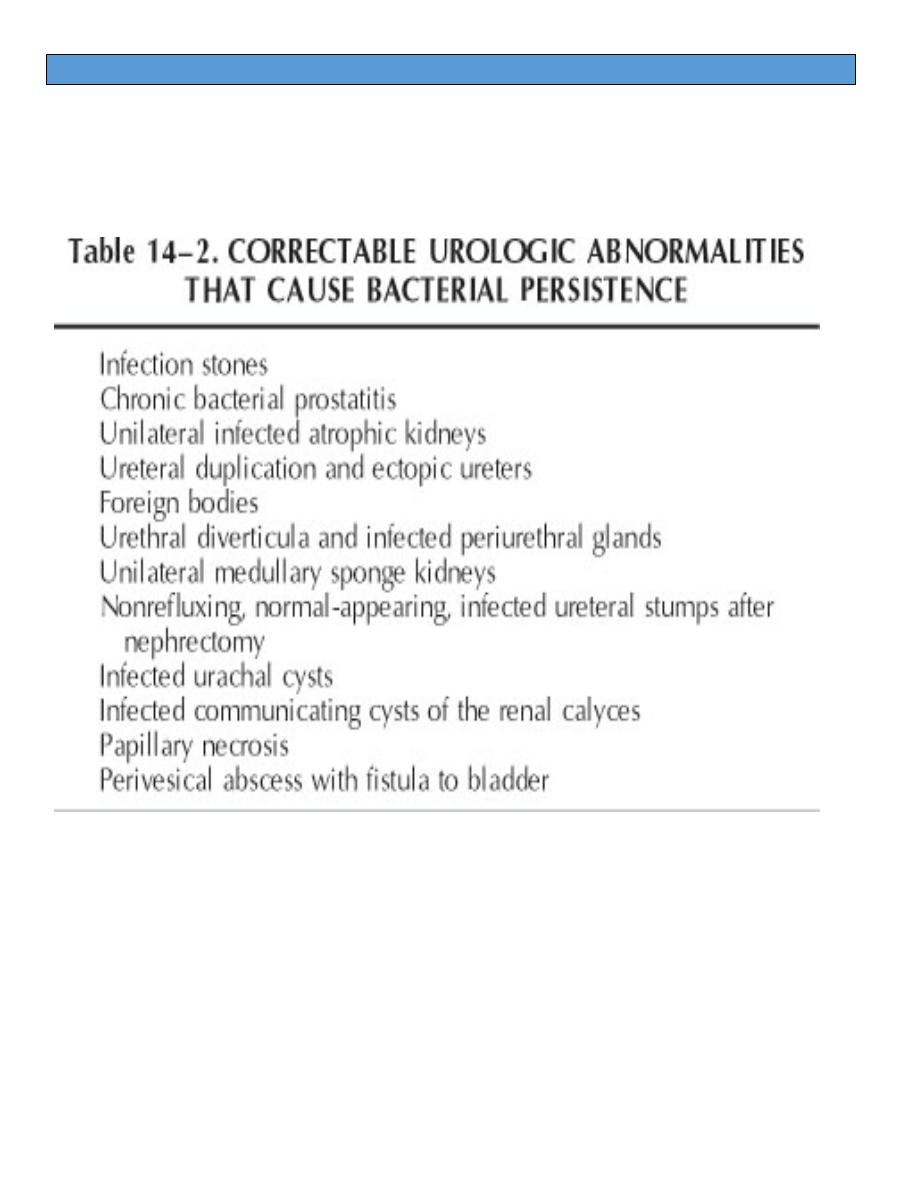
b. Bacterial persistence: refers to a recurrent UTI caused by the same
bacteria from a focus within the urinary tract, such as an infection
stone or the prostate.
Routes of Infection:
(1) Ascending Route: Most bacteria enter the urinary tract from the fecal
reservoir via ascent through the urethra into the bladder.
(2) Hematogenous Route: Infection of the kidney by the hematogenous
route is uncommon in normal individuals. However, the kidney is
occasionally secondarily infected inpatients with Staphylococcus
aureus bacteremia from oral sites or with Candida
(3)
Lymphatic Route: Direct extension of bacteria from the adjacent
organs via lymphatics may occur in unusual circumstances such as a
severe bowel infection or retroperitoneal abscesses.
P a g e | 3 UTI G:E
Urinary Pathogens:
- E. coli is by far the most common cause of UTI, accounting for 85% of
community-acquired and 50% of hospital-acquired infections.
- Other gram-negative Enterobacteriaceae including Proteus and
Klebsiella and gram-positive E. faecalis and Staphylococcus
saprophyticus are responsible for the remainder of most community-
acquired infections.
- Complicated or nosocomial infections are frequently caused by E. coli
and E. faecalis as well as by Klebsiella, Enterobacter, Citrobacter,
Serratia, Pseudomonas aeruginosa, Providencia, and S. epidermidis.
- Clinically symptomatic UTIs in which only anaerobic organisms are
cultured are rare,
UPPER TRACT INFECTIONS
Acute Pyelonephritis:
pyelonephritis is defined as inflammation of the kidney and renal pelvis.
Clinical Presentation: The classic presentation is an abrupt onset of chills,
fever, and unilateral or bilateral costovertebral angle tenderness. These so-
called upper tract signs are often accompanied by dysuria, increased
urinary frequency, and urgency. Acute renal failure may be present in the
rare case
physical examination: Tenderness to deep palpation in the costovertebral
angle
Laboratory Findings:
- GUE:
increased WBCs, WBC casts, and red blood cells.
Bacterial rods or chains of cocci are often seen
Urine cultures are positive
- Blood tests:
polymorphonuclear leukocytosis,
increased erythrocyte sedimentation rate (ESR),
elevated C-reactive protein levels,
elevated creatinine levels if renal failure is present.
Blood cultures may be positive.

P a g e | 4 UTI G:E
Radiologic Findings:
- Intravenous Urogram:
1. Generalized or focal renal enlargement (20%).
2. Delayed and impair contrast agent excretion in the calyces and
diminished nephrogram and pyelogram.
3. Dilatation of the ureter and renal pelvis without any obstructive cause
- Renal Ultrasonography:
- is useful to show renal size and collecting system obstruction and to
delineate focal bacterial nephritis.
- In most infected kidneys, no findings are seen on ultrasonography that
are not seen on the urogram.
Computed Tomography:
- CT is not indicated unless
- The diagnosis cannot be established by an intravenous urogram or
- The patient does not respond after 72 hours of therapy.
Treatment:
- In all cases antimicrobial therapy should be initiated that will be active
against potential uropathogens and achieve antimicrobial levels in
renal tissue as well as urine. The patient can then be treated with
selective parenteral or oral antimicrobial therapy once susceptibility
testing is available.
- Infection in patients with acute pyelonephritis can be subdivided into:
(1) uncomplicated infection that does not warrant hospitalization: Oral
fluoroquinolones (7 days) are particularly attractive for individuals
who receive outpatient therapy. TMP-SMX (14 days) is another but
less effective alternative. If gram-positive bacteria are suspected,
amoxicillin or amoxicillin– clavulanic acid is recommended.
(2) uncomplicated infection in patients with normal urinary tracts who
are ill enough to warrant hospitalization for parenteral therapy:
parenteral fluoroquinolone, an aminoglycoside with or without
ampicillin, or an extended-spectrum cephalosporin with or without an
aminoglycoside has proven efficacy against Enterobacteriaceae,
Pseudomonas, and other gram-negative bacilli.

P a g e | 5 UTI G:E
(3) complicated infection associated with hospitalization, catheterization,
urologic surgery, or urinary tract abnormalities: requires aggressive
broad-spectrum parental therapy.
- In group (2) and (3) parenteral therapy should be continued for 7 days
if blood culture is positive.
- If blood cultures are negative, 2- to 3-day parenteral therapy is
sufficient. Then, parenteral therapy can be discontinued and
appropriate oral therapy should be continued for an additional 7 to 14
days.
- If symptoms persist beyond 72 hours, however, the possibility of
perinephric or intrarenal abscesses, urinary tract abnormalities, or
obstruction should be considered and radiologic investigation with
ultrasonography or CT performed.
- Repeat urine cultures should be performed 5 to 7 days after initiation of
therapy and 4 to 6 weeks after discontinuation of antimicrobial therapy
to ensure that the urinary tract remains free of infection.
Chronic Pyelonephritis:
- chronic pyelonephritis refers to the small, contracted, atrophic kidney
or to the coarsely scarred kidney that has been produced by bacterial
infection, whether recent or remote.
- In contrast to the patient with clinical acute pyelonephritis, the patient
with chronic pyelonephritis is diagnosed by radiologic and pathologic
means
- The association of the small, scarred, clubbed kidney with VUR is
called reflux nephropathy.
Clinical Presentation:
- Many patients diagnosed as having chronic pyelonephritis have no
urologic symptoms, and the condition is discovered incidentally.
- Many are diagnosed because of symptoms related to the
complications of chronic renal failure
- These patients may have VUR or recurrent UTIs.
Laboratory Findings:
- GUE
- urinary concentrating capacity is impaired.
- Serum creatinine levels may be increased

P a g e | 6 UTI G:E
- creatinine clearance may be decreased.
Radiologic Findings:
1. Intravenous Urogram: The involved kidneys are usually small and
atrophic. Focal coarse renal scarring with clubbing of the
underlying calyx is characteristic
2. Voiding Cystourethrogram:
3. Radionuclear renal scan: is the best technique for diagnosing
chronic pyelonephritis.
Emphysematous Pyelonephritis:
- is an acute necrotizing parenchymal and perirenal infection caused by
gas-forming uropathogens.
- It seems more reasonable to postulate that impaired host response
caused by local factors such as obstruction or a systemic condition
such as diabetes allows organisms with the capability of producing
carbon dioxide to use necrotic tissue as a substrate to generate gas in
vivo
Women are affected more often than men.
The condition usually occurs in diabetic patients
The overall mortality is 43%.
Clinical Presentation:
- The usual clinical presentation is severe, acute pyelonephritis that fails
to resolve during the first 3 days of treatment.
- Almost all patients display the classic triad of fever, vomiting, and flank
pain.
- Pneumaturia is absent unless the infection involves the collecting
system.
- Results of urine cultures are invariably positive.
Radiologic Findings:
- The diagnosis is established radiographically.
- The hallmark is intraparenchymal gas.
Abdominal x-ray
CT
Management:
- Patients should be started on appropriate antimicrobial agents
P a g e | 7 UTI G:E
- Treatment of diabetes must be initiated.
- Obstruction of the affected kidney, if present, must be eliminated,
- function of the contralateral kidney must be established, because 10%
of the reported cases have been bilateral.
- If treatment ineffective; then surgical drainage or nephrectomy is
needed.
Renal Abscess:
- Renal abscess or carbuncle is a collection of purulent material
confined to the renal parenchyma.
- Since about 1970, gram-negative organisms have been implicated in
the majority of adults with renal abscesses.
- Ascending infection associated with tubular obstruction from prior
infections or calculi appears to be the primary pathway for the
establishment of gram-negative abscesses
Clinical Presentation:
- The patient may present with fever, chills, abdominal or flank pain, and,
occasionally, weight loss and malaise.
- Symptoms of cystitis may occur.
Laboratory Findings:
- The patient typically has marked leukocytosis.
- The blood cultures are usually positive.
- Pyuria and bacteriuria may not be evident unless the abscess
communicates with the collecting system.
- Because gram-positive organisms are most commonly blood-borne,
urine culturesin these cases typically show no growth or a
microorganism different from that isolated from the abscess.
- When the abscess contains gram-negative organisms, the urine
culture usually demonstrates the same organism isolated from the
abscess.
Radiologic Findings:
KUB:
- renal enlargement with distortion of the renal contour
- Obliteration of the corresponding psoas shadow
- Scoliosis is often present,
P a g e | 8 UTI G:E
Ultrasonography
- An echo-free or low–echo-density space-occupying lesion
CT Scan:
appears to be the diagnostic procedure of choice for renal abscesses
- obliteration of adjacent tissue planes,
- thickening of Gerota's fascia,
- a round or oval parenchymal mass of low attenuation,
- and a surrounding inflammatory wall of slightly higher attenuation that
forms a ring when the scan is enhanced with contrast material. The
ring sign is caused by the increased vascularity of the abscess wall.
Management:
The classic treatment for an abscess has been percutaneous or open
incision and drainage
Infected Hydronephrosis and Pyonephrosis:
Infected hydronephrosis: is bacterial infection in a hydronephrotic kidney.
Pyonephrosis: refers to infected hydronephrosis associated
withsuppurative destruction of the parenchyma of the kidney, in which there
is total or nearly total loss of renal function.
Clinical Presentation:
- The patient is usually very ill, with high fever, chills, flank pain, and
tenderness.
Radiologic Findings:
- Renal ultrasonography is the most useful procedure to diagnose
pyonephrosis.
(1) persistent echoes from the inferior portion of the collecting system,
(2) a fluid-debris level with dependent echoes that shift when the patient
changes position
(3) strong echoes with acoustic shadowing from air in the collecting
system,
(4) weak echoes throughout a dilated collecting system.
Excretory urography:
shows a poorly functioning or nonfunctioning hydronephrotic kidney
P a g e | 9 UTI G:E
Management:
- Once the diagnosis of pyonephrosis is made, the treatment is initiated
with appropriate antimicrobial drugs and drainage of the infected pelvis.
- A ureteral catheter can be passed to drain the kidney, but if the
obstruction prevents this, a percutaneous nephrostomy tube should be
placed.
Perinephric Abscess:
- collection of purulent material located within Gerota's fascia.
- When a perinephric infection ruptures through Gerota's fascia into the
pararenal space, the abscess becomes paranephric.
- Perinephric abscesses are thought to arise from hematogenous
seeding from sites of infection or from renal extension of an ascending
UTI
Clinical Presentation:
- The most common complaints are fever, flank or abdominal pain, chills,
and dysuria
- physical findings showed flank or abdominal tenderness and fever.
- A flank mass may present in 47% of the patients.
Radiologic Findings:
KUB:
- missing psoas shadows,
- apparent
renal
masses,
- absent
renal
outlines,
- calculi, and retroperitoneal gas.
Ultrasonography
- demonstrate a diverse sonographic appearance ranging from a nearly
anechoic mass displacing the kidney to an echogenic collection that
tends to blend with normally echogenic fat within Gerota's fascia.
- Diagnostic aspiration under ultrasound guidance carries minimal
morbidity
CT scan:
- defines renal distortion and perirenal fluid or gas associated with
perinephric abscesses in excellent anatomic detail.
Management:
P a g e | 10 UTI G:E
- surgical drainage, or nephrectomy if the kidney is nonfunctioning or
severely infected, is the classic treatment for perinephric abscesses.
- antimicrobial agents are useful to control sepsis and to prevent spread
of infection
Xanthogranulomatous Pyelonephritis
- Xanthogranulomatous pyelonephritis is a rare, severe, chronic renal
infection typically resulting in diffuse renal destruction.
- Most cases are unilateral and result in a nonfunctioning, enlarged
kidney associated with obstructive uropathy secondary to
nephrolithiasis.
- It is important, however, because it is "a great imitator". It is often
misdiagnosed as a renal tumor.
LOWER TRACT INFECTIONS
Uncomplicated Cystitis:
- Uncomplicated cystitis occasionally occurs in prepubertal girls, but it
increases greatly in incidence in late adolescence and during the
second and fourth decades of life.
- 25% to 30% of women between the ages of 20 and 40 years have had
UTIs.
- E. coli in 80%, and S. saprophyticus in 5% to 15%. Other organisms
less commonly involved include Klebsiella species, P. mirabilis, or
enterococci.
Clinical Presentation:
Clinical symptoms include
- Dysuria,
- Frequency,
- Urgency,
- Voiding of small urine volumes,
- Suprapubic or lower abdominal pain.
- Hematuria or foul-smelling urine may develop
- On examination, suprapubic tenderness may be present.
Laboratory Diagnosis:
GUE:
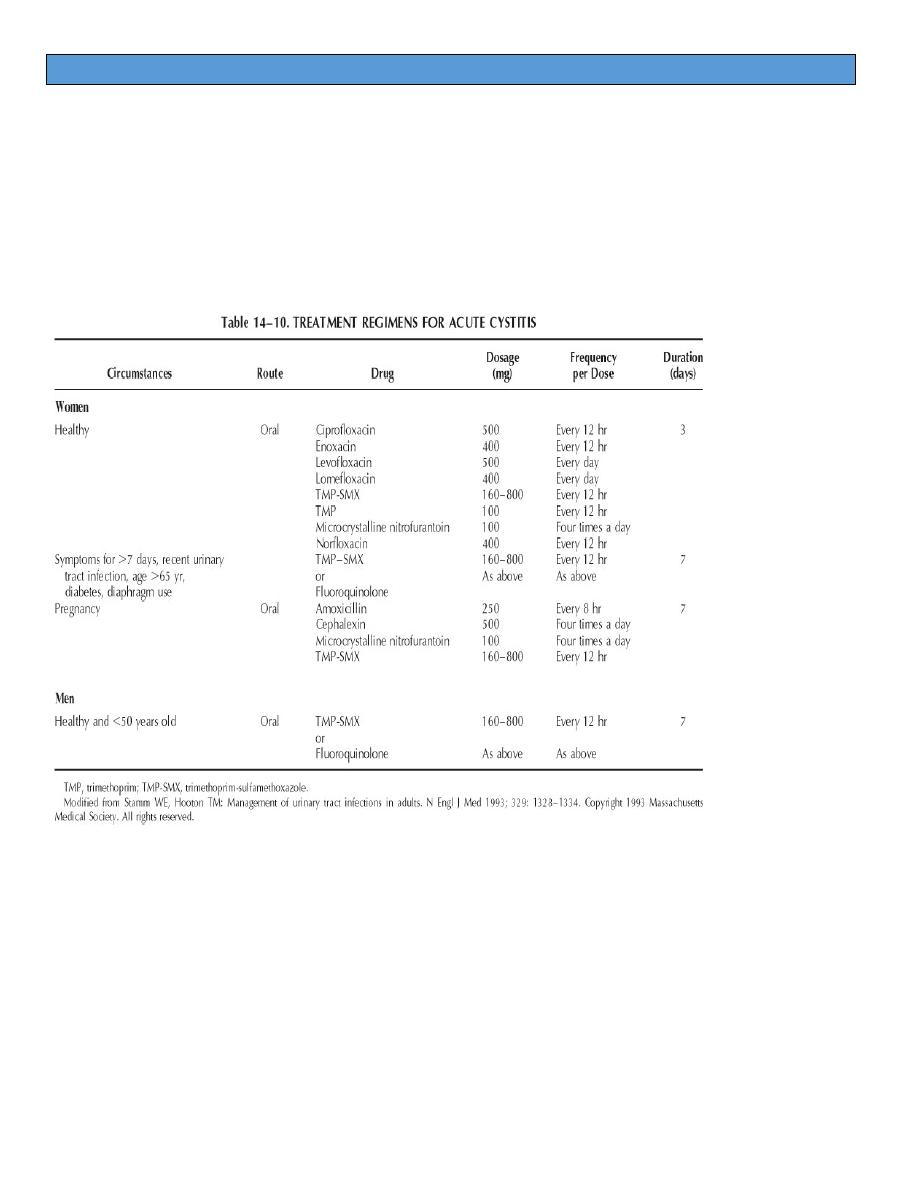
P a g e | 11 UTI G:E
- bacteriuria,
- pyuria,
- hematuria
Urine culture remains the definitive test (Pretreatment urine culture is
recommended in all men. But not in all women)
