Hair
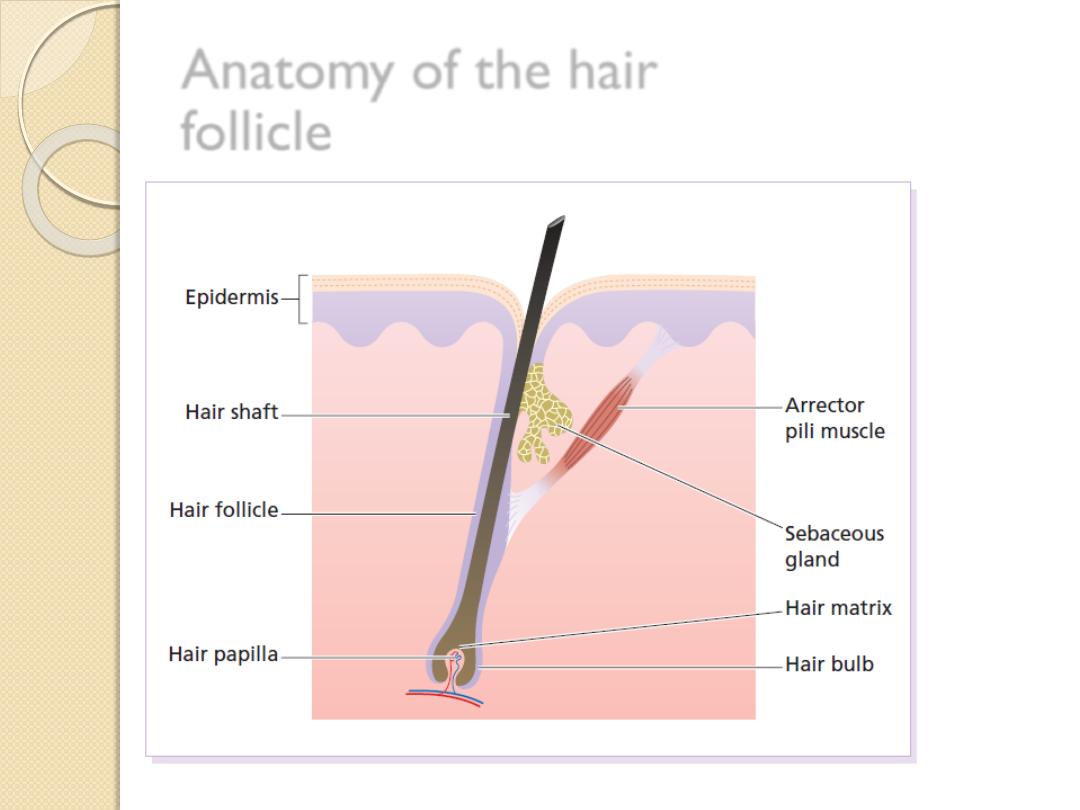
Anatomy of the hair
follicle
Classification of hair
Hairs are classified into three main types.
1. Lanugo hairs Fine long hairs covering the foetus,
but shed about 1 month before birth.
2. Vellus hairs Fine short unmedullated hairs
covering much of the body surface. They replace
the lanugo
hairs just before birth.
3. Terminal hairs Long coarse medullated hairs
seen, for example, in the scalp or pubic regions.
Their growth is often influenced by circulating
androgen levels.
The hair cycle
Each follicle passes, independently of its
neighbours
1. Anagen The active phase of hair
production.
2. Catagen A short phase of conversion from
active growth to the resting phase. Growth
stops, and the end of the hair becomes club-
shaped.
3. Telogen A resting phase at the end of
which the club hair is shed.

The hair cycle
Physiology
On the scalp said to contain an average of
100 000 hairs, anagen lasts for up to 5
years, catagen for about 2 weeks and
telogen for about 3 months.
As many as 100 hairs may be shed from
the normal scalp every day as a normal
consequence of cycling.
Physiology
On the scalp, about 85% are normally in
anagen and 15% in the telogen phase
The length of hair is determined by the
duration of anagen
There are important racial differences in
hair.
Asians tend to have straight hair, Negroids
woolly hair and Europeans wavy hair.
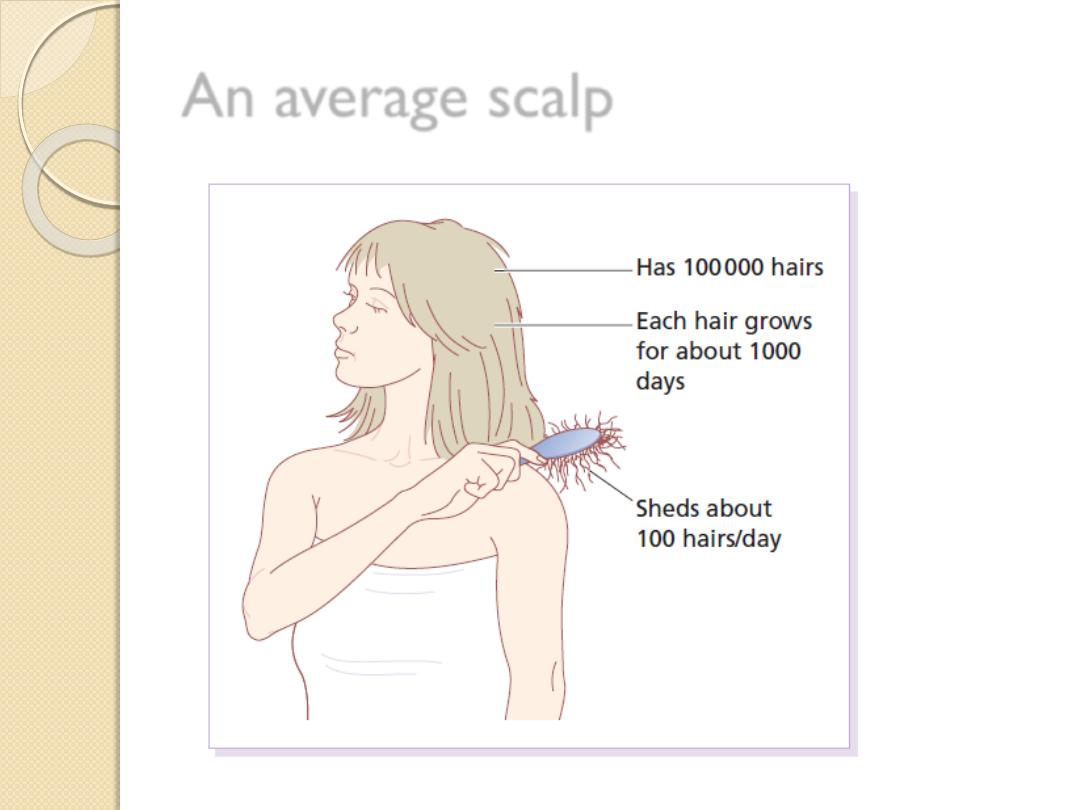
An average scalp
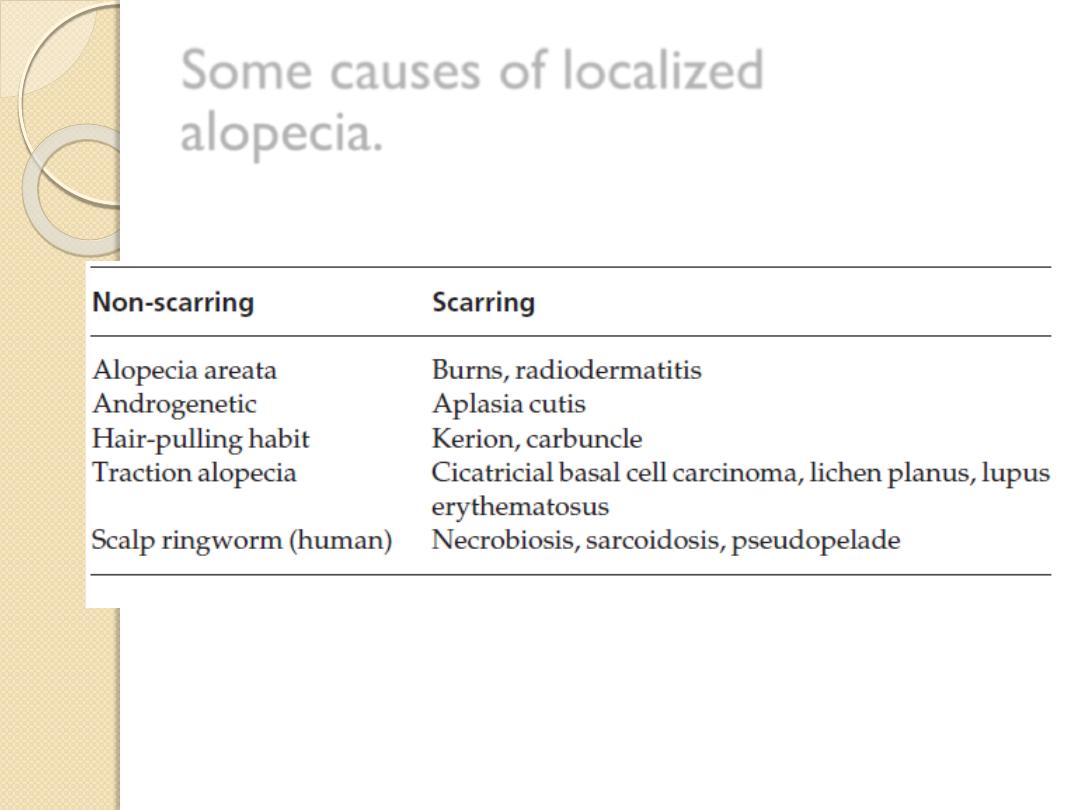
Some causes of localized
alopecia.
ALOPECIA AREATA
Alopecia areata
Cause
An immunological basis is suspected because of an
association with autoimmune thyroid disease, vitiligo
and atopy.
Alopecia areata is probably inherited as a complex
genetic trait; sometimes HLA-DQ3, -DR11 or -DR4
act as susceptibility factors, with an increased
occurrence in the first-degree relatives of affected
subjects and twin concordance.
It affects some 10% of patients with Down’s
syndrome, suggesting the involvement of genes on
chromosome 21.
Environmental factors may trigger alopecia areata in
the genetically predisposed
Alopecia areata
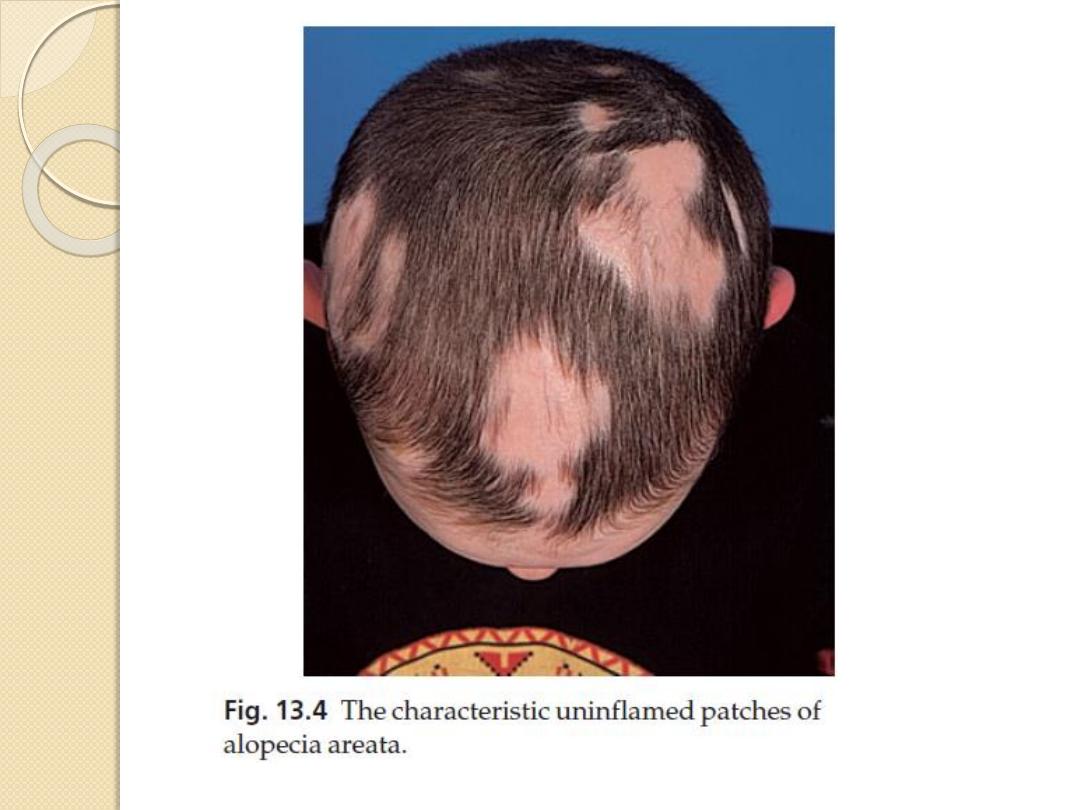
Presentation
A typical patch is uninflamed, with no scaling, but with
empty hair follicles
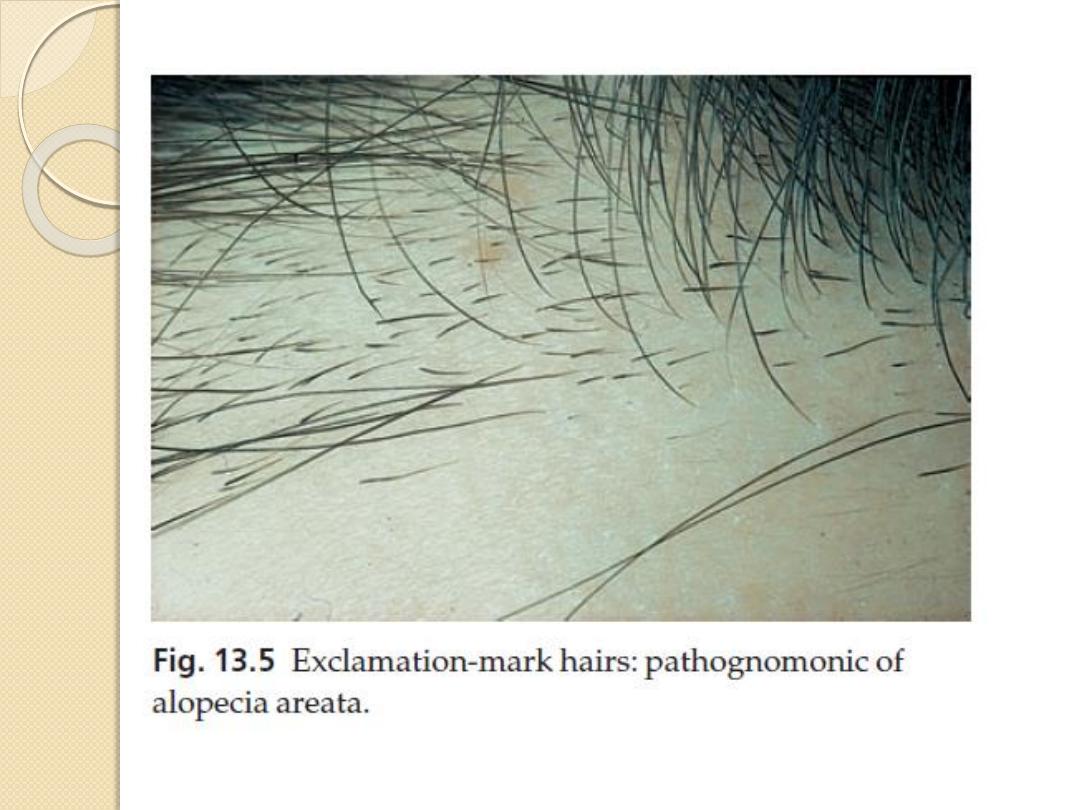
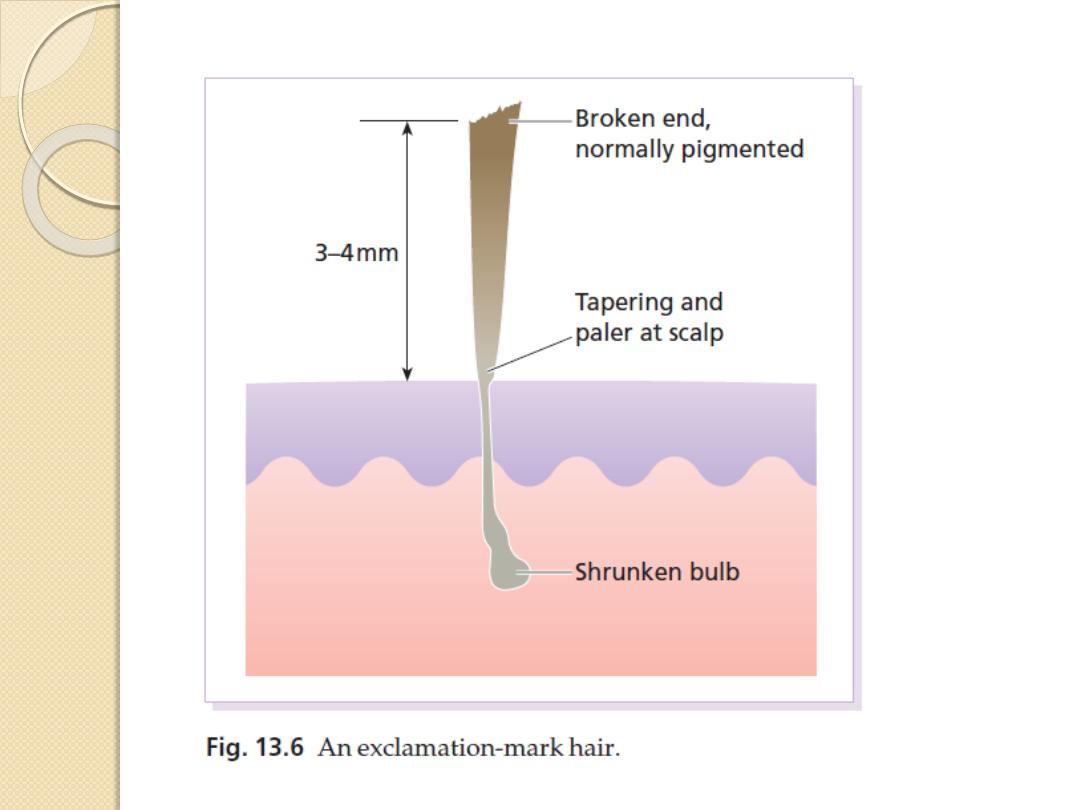
Pathognomonic ‘exclamation-mark’ hairs may be
seen around the edge of enlarging areas. They are
broken off about 4 mm from the scalp, and are
narrowed and less pigmented proximally.
Patches are most common in the scalp and beard but
other areas, especially the eyelashes and eyebrows, can
be affected too.
Up to 50% of patients show fine pitting or wrinkling of
the nails.
A few of those who go on to have chronic disease lose
all the hair from their heads (alopecia totalis) or from
the whole skin surface (alopecia universalis).
Alopecia areata
Course
The outcome is unpredictable.
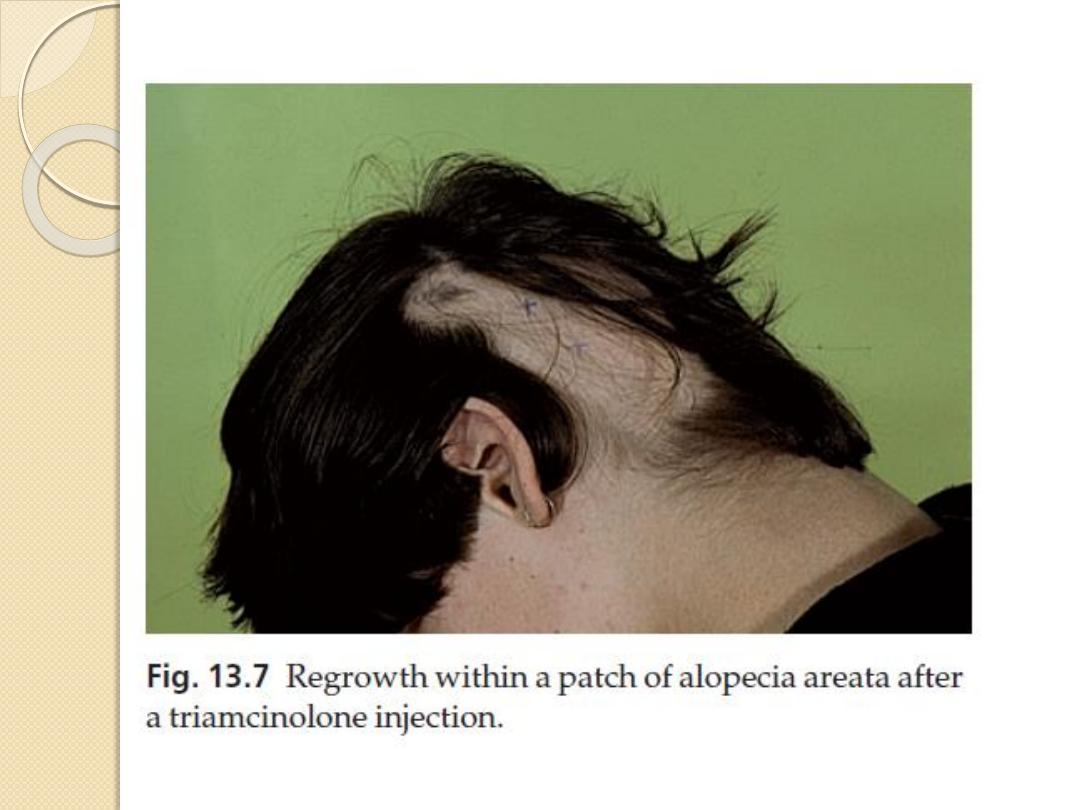
In a first attack, regrowth is usual within a few months.
New hairs appear in the centre of patches as fine pale down,
and gradually regain their normal thickness and colour
Fifty percent of cases resolve spontaneously without
treatment within 1 year, and only 10% go on to have severe
chronic disease.
Subsequent episodes tend to be more extensive and
regrowth is slower.
Hair loss in some areas may coexist with regrowth in others.
Alopecia areata
Factors suggesting poor prognosis:
1. onset before puberty;
2. association with atopy or Down’s
syndrome;
3. unusually widespread alopecia; and
4. involvement of the scalp margin
(ophiasiform type), especially at the nape
of the neck.
Alopecia areata
Differential diagnosis
ringworm
lupus erythematosus
lichen planus
Secondary syphilis can also cause a ‘moth-
eaten’ patchy hair loss
Pseudopelade
Alopecia areata
Investigations
Syphilis can be excluded with serological
tests
Alopecia areata
Treatment
reassured about regrowth.
Topical corticosteroid creams of high potency can be
prescribed
systemic steroids should be avoided in most cases
the intradermal injection of 0.2 ml intralesional
triamcinolone acetonide (5–10 mg/ml), side effect is
dermal atrophy
Mild irritants, such as 0.1–0.25% dithranol, have been
used but with limited success.
Ultraviolet radiation or even psoralen with ultraviolet A
(PUVA) therapy may help extensive cases, but hair fall
often returns when treatment stops.
Wigs are necessary for extensive cases.
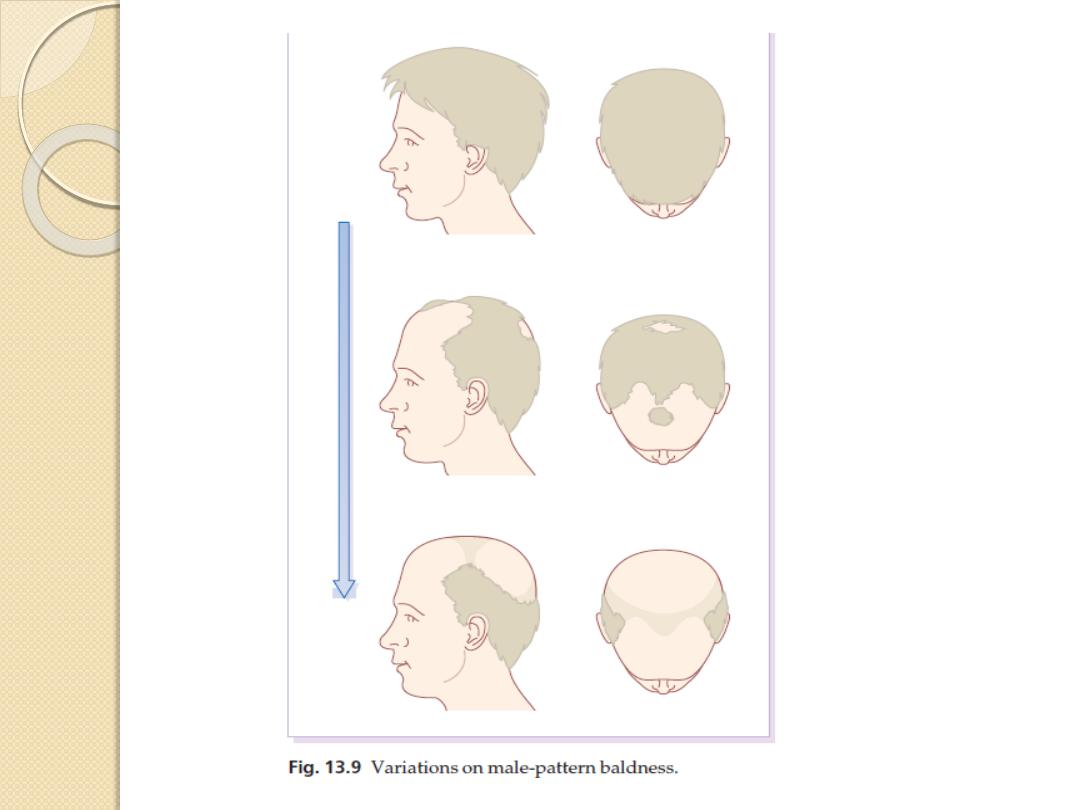
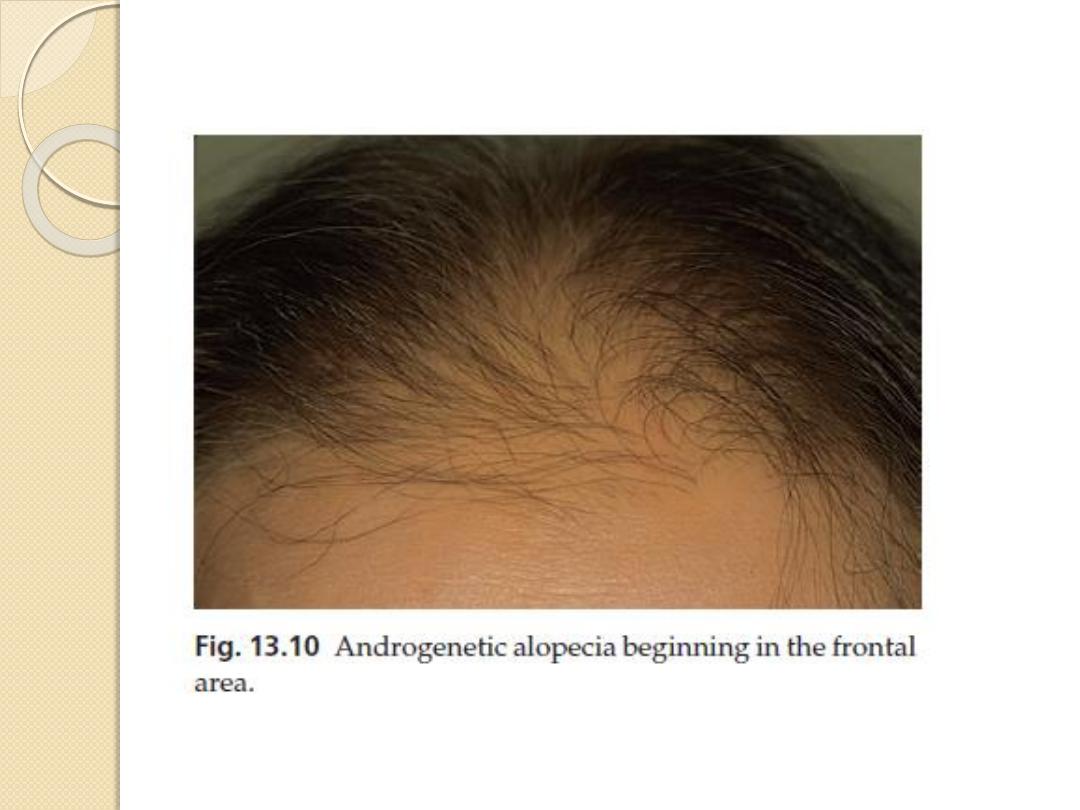
Androgenetic alopecia
(male-pattern baldness)
Androgenetic alopecia (male-pattern
baldness)
Cause
Familial but the exact mode of inheritance
has not yet been clarified.
Suggested polygenic type of inheritance.
Male-pattern baldness is androgen
dependent; in females, androgenetic alopecia
(female-pattern hair loss), with circulating
levels of androgen within normal limits, is
seen only in those who are strongly
predisposed genetically.
Androgenetic alopecia (male-
pattern baldness)
Presentation
The common pattern in men is the loss of hair first from the
temples, and then from the crown
In women the hair loss may be much more diffuse, particularly
over the crown
In bald areas, terminal hairs are replaced by finer vellus ones.
Clinical course
Hair loss follow the family pattern, with some losing hair quickly
and others more slowly.
The diffuse pattern seen in women tends to progress slowly.
Complications
Even minor hair loss may lead to great anxiety
Investigations
None are usually needed. In women, virilization may have to be
excluded
Androgenetic alopecia (male-
pattern baldness)
Treatment
1.
Scalp surgery
2.
hair transplants
3.
wigs
4.
Topical application of minoxidil lotion may slow early hair loss and even
stimulate new growth of hair but the results are not dramatic. Small and
recently acquired patches respond best. When minoxidil treatment stops,
the new hairs fall out after about 3 months.
5.
Antiandrogens help some women
6.
Finasteride (Propecia), an inhibitor of human type II 5a-reductase, reduces
serum and scalp skin levels of dihydrotestosterone in balding men.
At the dosage of 1 mg/day, it may increase hair counts and so lead to a
noticeable improvement in both frontal and vertex hair thinning. However,
the beneficial effects slowly reverse once treatment has stopped.
This treatment is not indicated in women or children.
Side-effects are rare, but include decreased libido, erectile dysfunction and
altered prostate-specific antigen levels.

Telogen effluvium
Cause
triggered by any severe illness, particularly those
with bouts of fever or haemorrhage, by childbirth
and by severe dieting.
All of these synchronize catagen so that, later on,
large numbers of hairs are lost at the same time.
Presentation and course
The diffuse hair fall, 2–3 months after the
provoking illness, can be mild or severe.
Beau’s lines may be seen on the nails.
Regrowth, not always complete, usually occurs
within a few months.

Telogen effluvium
Differential diagnosis
This is from other types of diffuse hair loss
In androgenetic alopecia in females the onset is
gradual in mid-adulthood, and hairs remain rather
firmly anchored to the scalp. In telogen effluvium
the onset is abrupt and follows acute illness, an
operation or pregnancy by 1–2 months. Hair fall
is prominent and lightly pulling on scalp hairs
dislodges.
Treatment
This condition is unaffected by therapy, but
patients can be reassured that their hair fall will
be temporary.
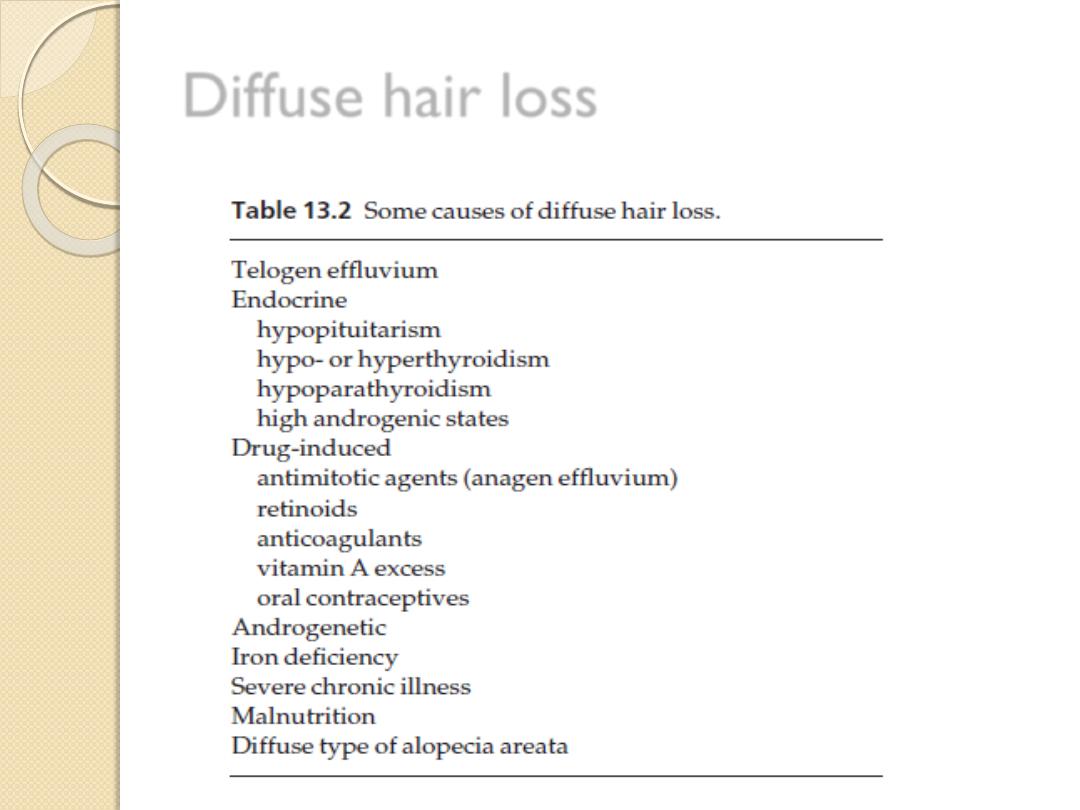
Diffuse hair loss
Scarring alopecia
If the follicular openings can no longer be seen
with a lens, regrowth of hair cannot be expected.
cause scarring alopecia
1.
a severe burn
2.
trauma
3.
a carbuncle
4.
inflammatory scalp ringworm
5.
Discoid lupus erythematosus
6.
lichen planus
7.
morphoea
8.
pseudopelade
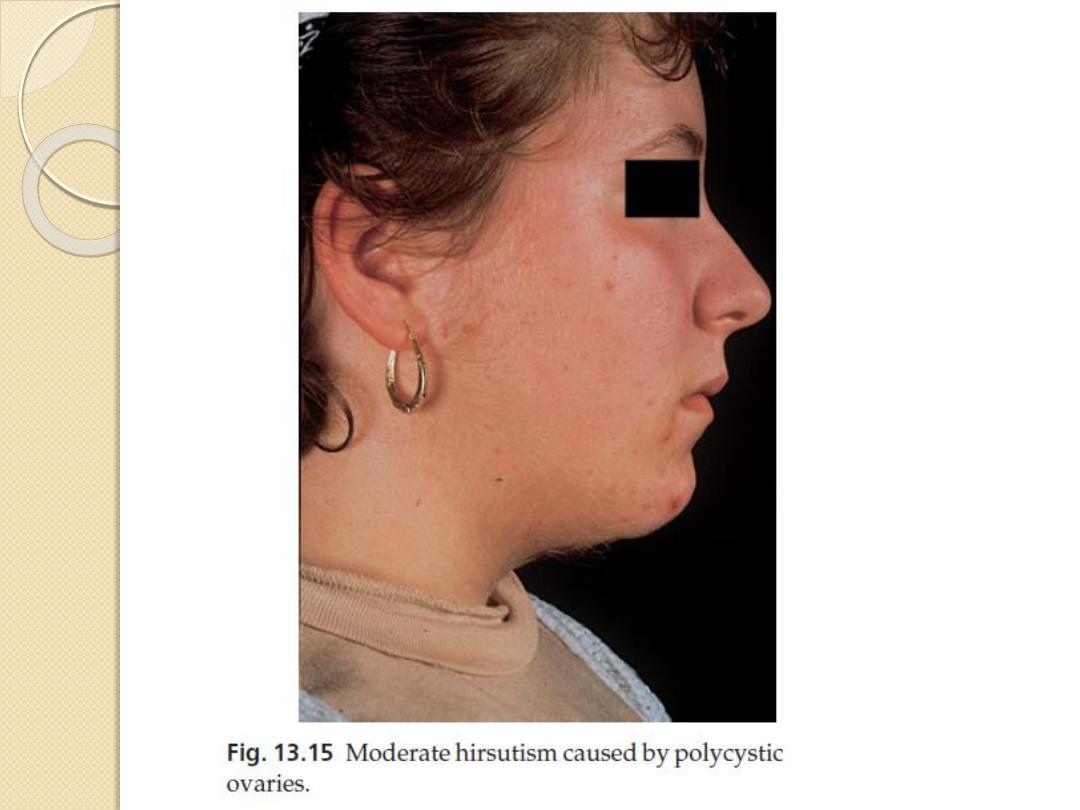
Hirsutism and hypertrichosis
Hirsutism is the growth of terminal hair
in a woman, which is distributed in the
pattern normally seen in a man.
Hypertrichosis is an excessive growth
of terminal hair that does not follow an
androgen-induced pattern
Hirsutism
Cause
Some degree of hirsutism may be a racial or
familial trait, and minor facial hirsutism is
common after the menopause.
some patients without a family background
of hirsutism become hirsute in the absence
of any demonstrable hormonal cause
(idiopathic hirsutism).
Finally, some patients with most commonly
the polycystic ovarian syndrome.
Hirsutism
Presentation
An excessive growth of hair appears in the beard
area, on the chest and shoulder-tips, around the
nipples and in the male pattern of pubic hair.
Androgenetic alopecia may complete the picture.
Course
Familial, racial or idiopathic hirsutism tends to
start at puberty and to worsen with age.
Complications
Virilization is associated with infertility
Psychological disturbances are common.
Hirsutism
Investigations
Investigations are needed if:
1.
hirsutism occurs in childhood
2.
there are other features of virilization, such as
clitoromegaly or voice change
3.
the hirsutism is of sudden or recent onset
4.
there is menstrual irregularity or cessation.
The tests used will include measurement of the
serum testosterone, sex hormone-binding globulin,
dehydroepiandrosterone sulphate,
androstenedione and prolactin.
Transvaginal ovarian ultrasound is useful if
polycystic ovaries are suspected.
Hirsutism
Treatment
Any underlying disorder must be treated.
Home remedies for minor hirsutism include commercial
depilatory creams
waxing or shaving, or making the appearance less obvious by
bleaching
Plucking should probably be avoided as it can stimulate hair
roots into anagen.
Electrolysis
laser
Topical therapy with eflornithine, an inhibitor of ornithine
decarboxylase, can slow regrowth.
Oral antiandrogens (e.g. cyproterone acetate, Dianette; or
spironolactone) may sometimes be helpful, but will be needed
long term.
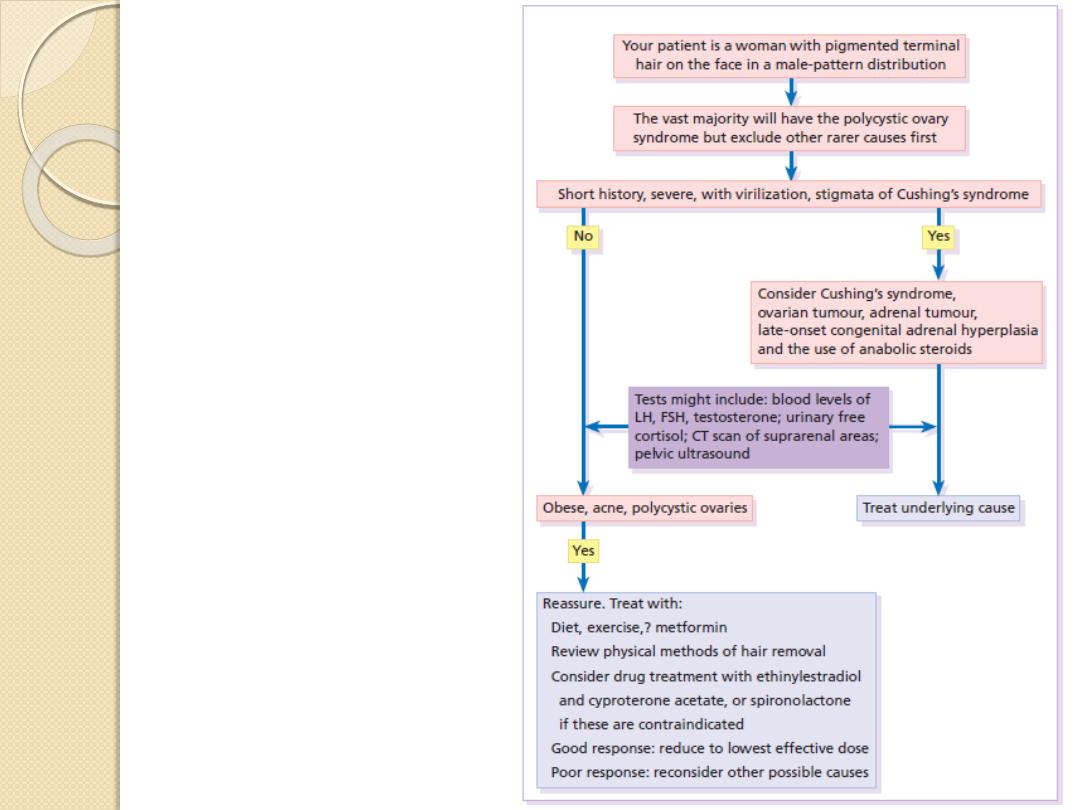
An approach to hirsutism.
CT, computer tomography;
FSH, follicle-stimulating hormone;
LH, luteinizing hormone.
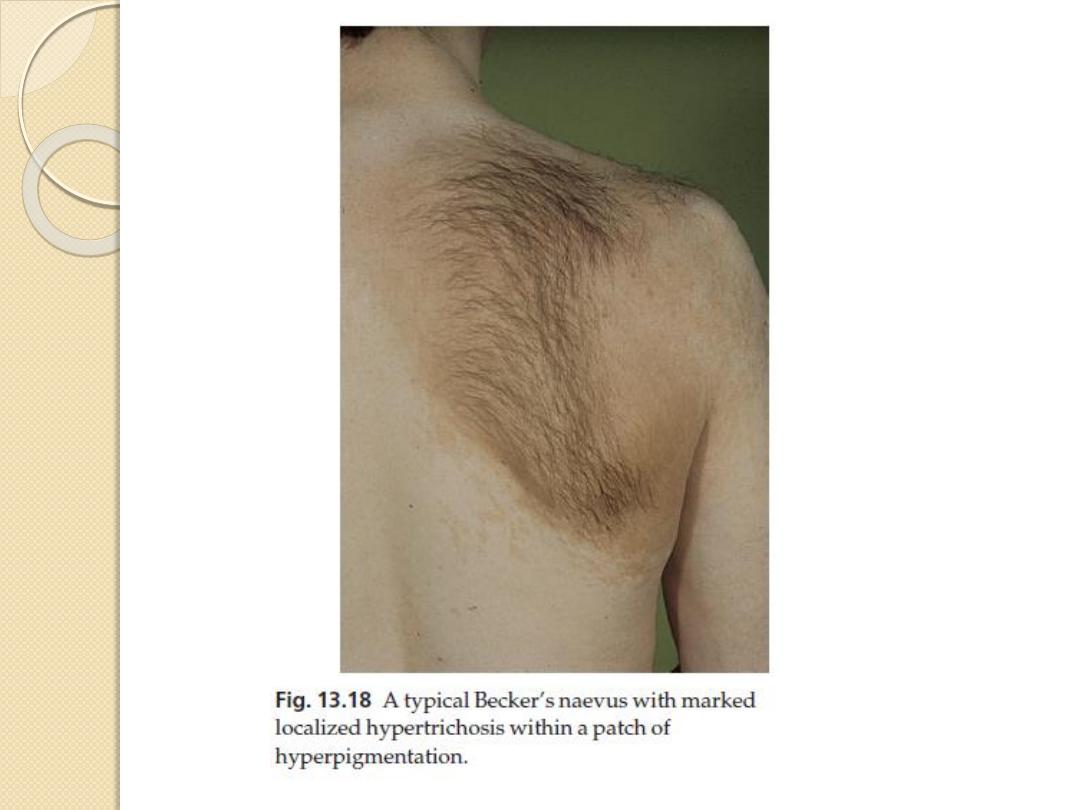
Hypertrichosis
The localized type is most commonly seen
over melanocytic naevi including Becker’s naevi
a ‘satyr’s tuft’ –in some patients with spina bifida.
Excessive amounts of hair may grow near
chronically inflamed joints or under plaster casts.
Repeated shaving does not bring on
hypertrichosis although occupational pressure
may do so (e.g. from carrying weights on the
shoulder).
Generalized hypertrichosis.
1.
Anorexia nervosa, starvation
2.
Drug-induced (minoxidil, diazoxide,
ciclosporin)
3.
Cutaneous porphyrias
4.
Foetal alcohol and foetal phenytoin
syndromes
Nail
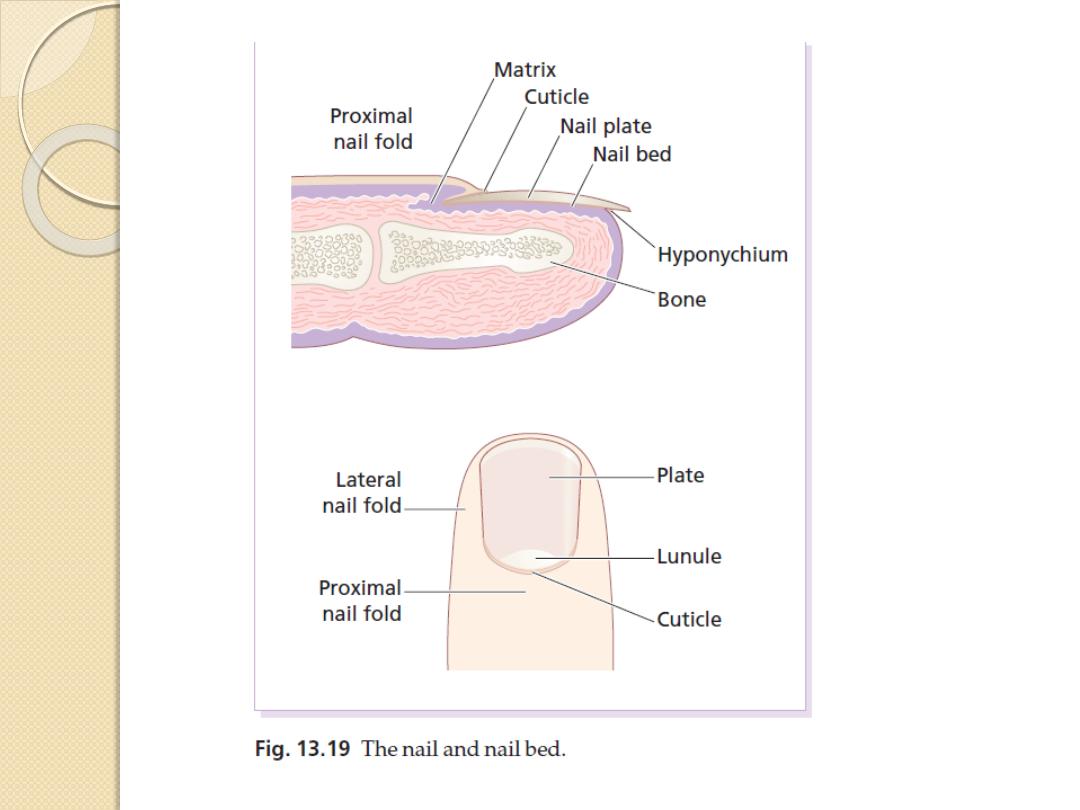
Effects of trauma
Permanent ridges or splits in the nail plate can follow
damage to the nail matrix
Splinter haemorrhages
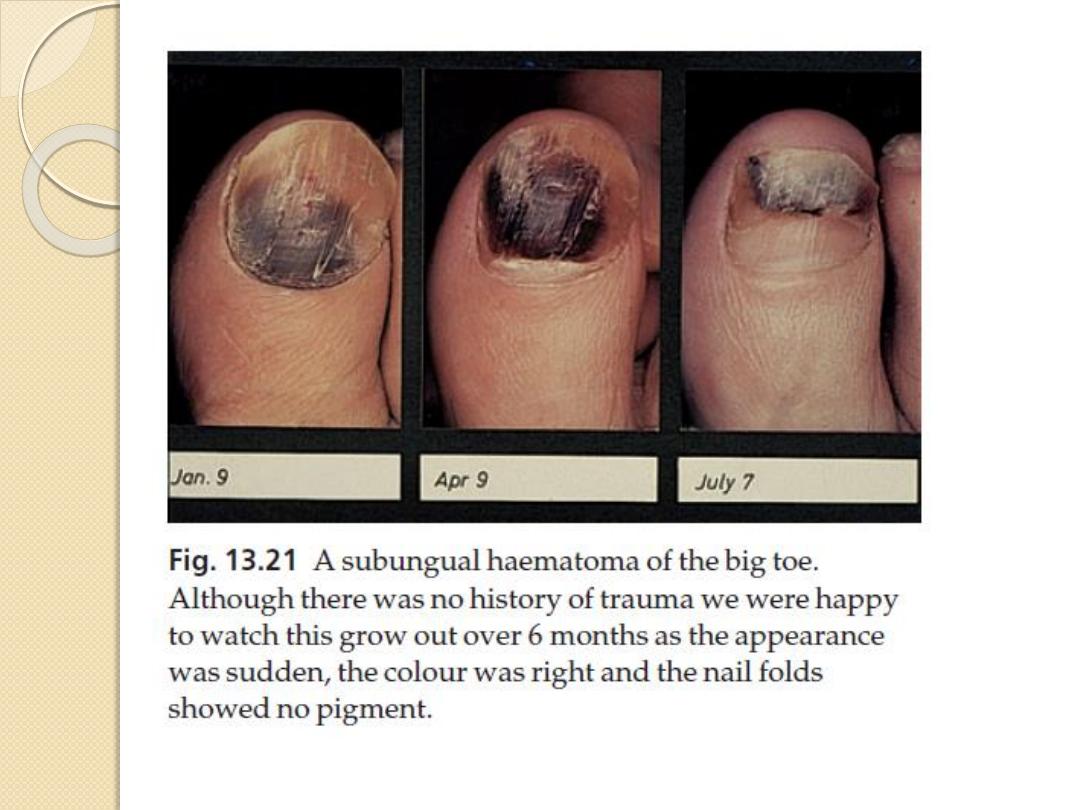
Subungual haematomas, dark areas of altered blood can
raise worries about the presence of a subungual melanoma.
Chronic trauma from sport and from ill-fitting shoes
contributes to haemorrhage under the nails of the big toes, to
the gross thickening of toenails known as onychogryphosis and to
ingrowing nails
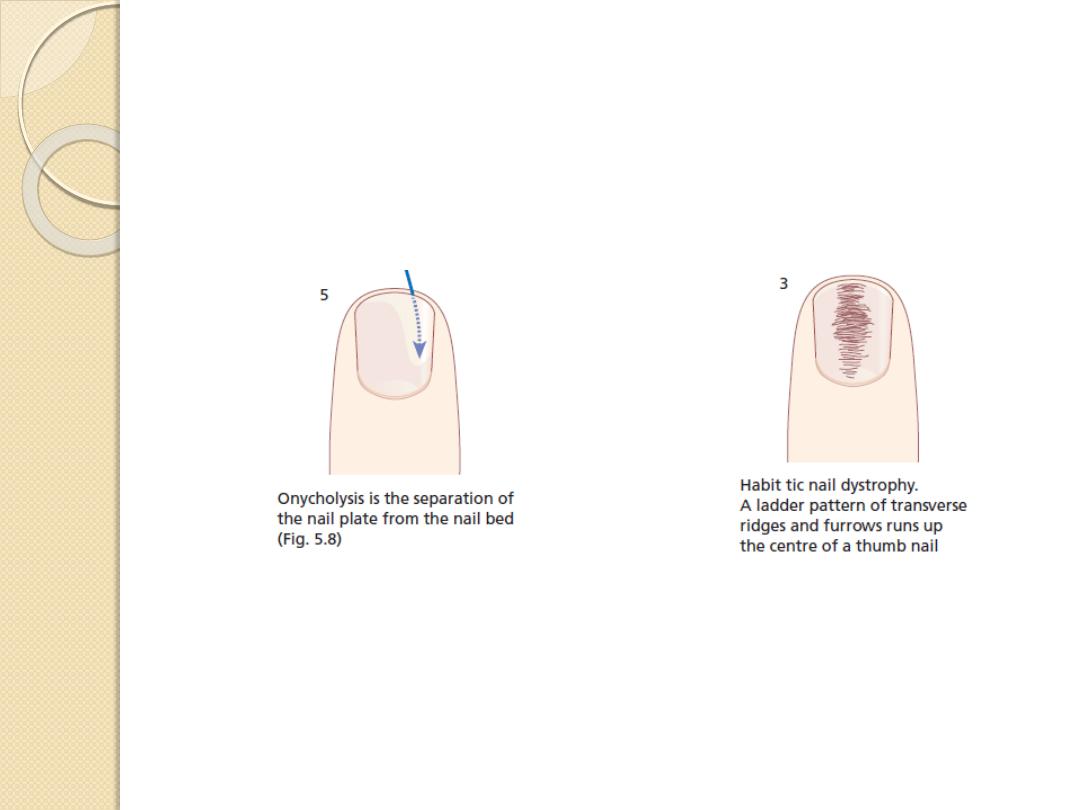
Onycholysis, a separation of the nail plate from the nail bed,
may be a result of minor trauma and psoriasis, phototoxic
reactions, repeated immersion in water, after the use of nail
hardeners. The space created may be colonized by yeasts, or by
bacteria such as Pseudomonas aeruginosa, which turns it an ugly
green colour
Effects of trauma
Bitten nails are short and irregular
Tic nail dystrophy, a common habit, the cuticle of the
thumbnail is the target for picking or rubbing. This
repetitive trauma causes a ladder pattern of transverse
ridges and grooves to run up the centre of the nail plate
Lamellar splitting of the distal part of the fingernails,
so commonly seen in housewives, has been attributed to
repeated wetting and drying
Contact Allergy in attempts to beautify nails
Contact dermatitis caused by allergens in nail polish
itself seldom affects the fingers but presents as small
itchy eczematous areas where the nail plates rest against
the skin during sleep. The eyelids, face and neck are
favourite sites

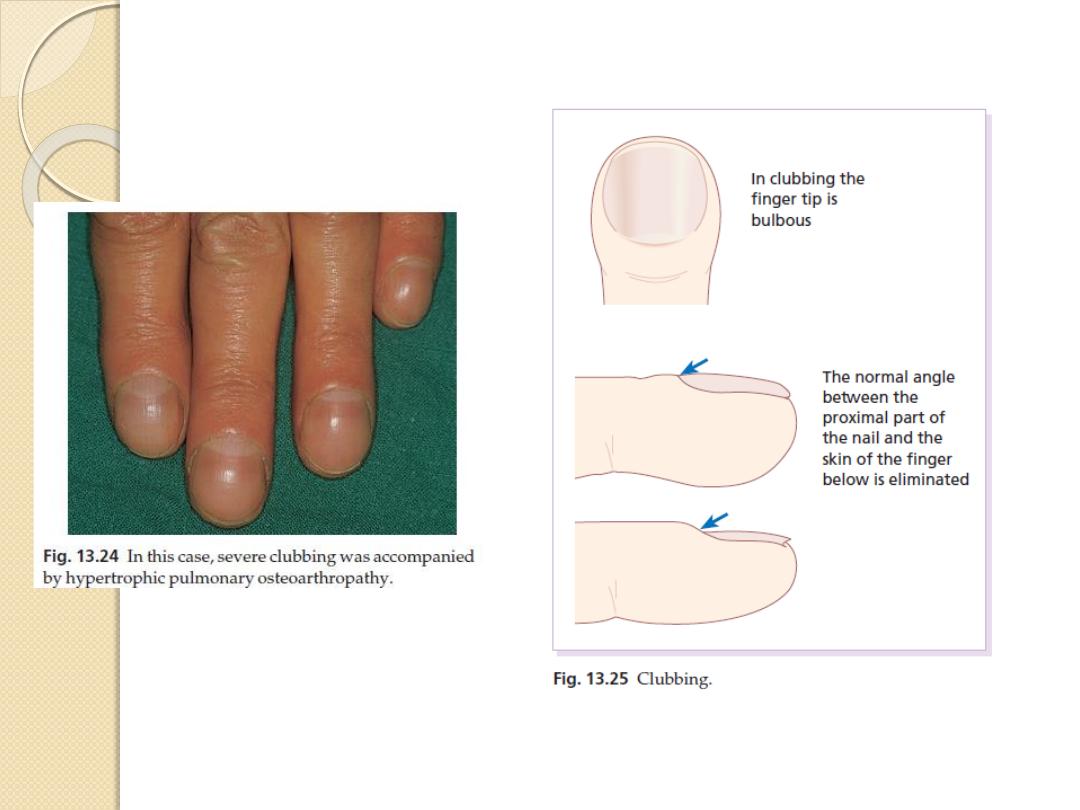
The nail in systemic disease
Clubbing
A bulbous enlargement of the terminal
phalanx with an increase in the angle
between the nail plate and the proximal fold
to over 180°.
Its association with chronic lung disease and
with cyanotic heart disease is well known.
Rarely, clubbing may be familial with no
underlying cause.
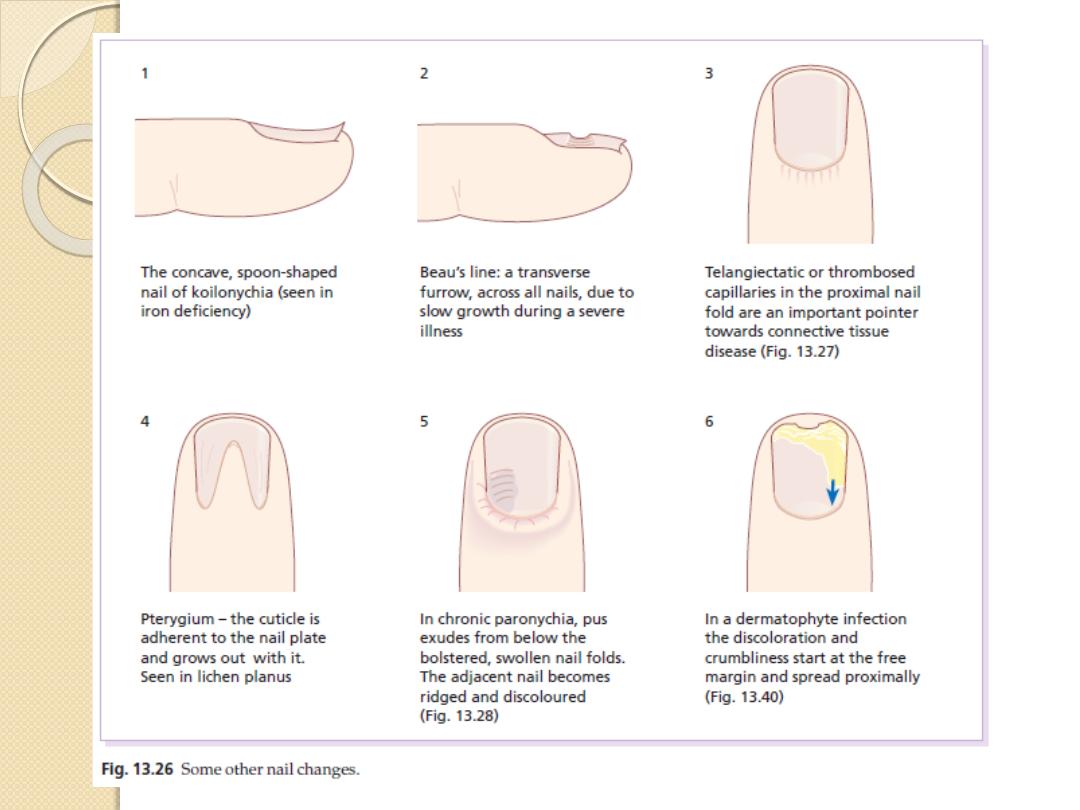
Koilonychia
A spooning and thinning of the nail plate,
indicating iron deficiency
The nail in systemic disease
Colour changes
The ‘half-and-half’ nail, with a white proximal
and red or brown distal half, is seen in a minority
of patients with chronic renal failure.
Whitening of the nail plates may be related
to hypoalbuminaemia, as in cirrhosis of the liver.
Some drugs, notably antimalarials, antibiotics and
phenothiazines, can discolour the nails.
Beau’s lines
Transverse grooves that appear synchronously on
all nails a few weeks after an acute illness and
which grow steadily out to the free margin
The nail in systemic disease
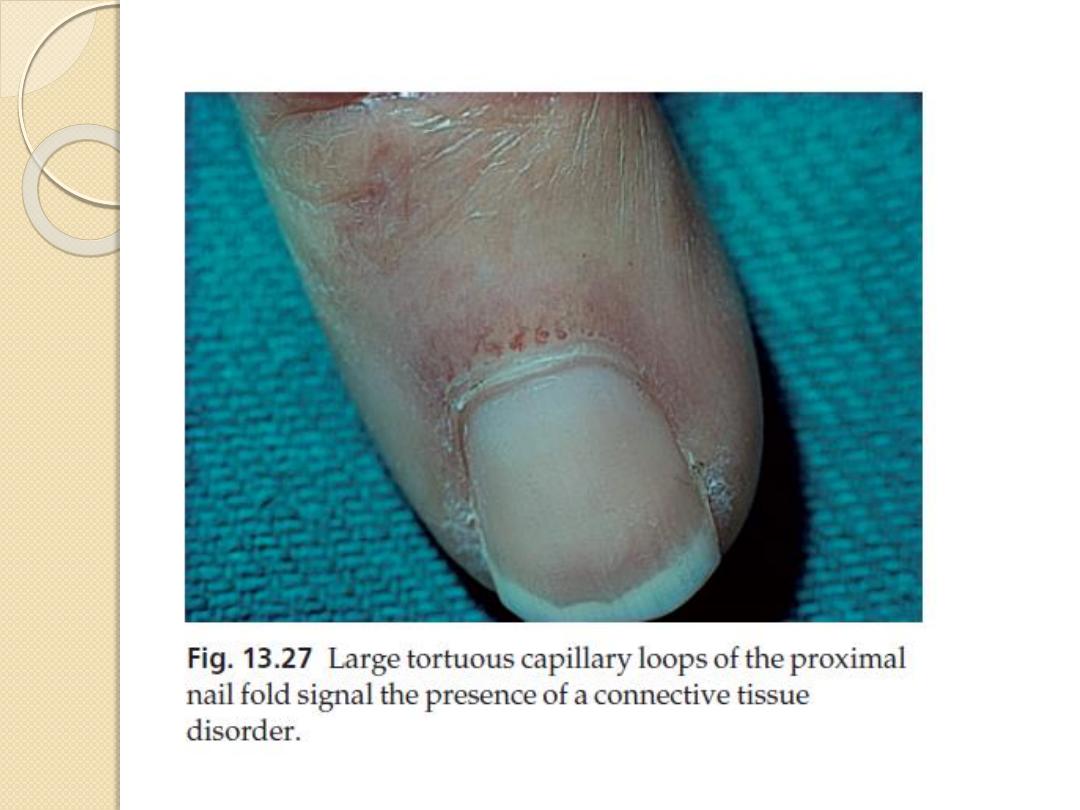
Connective tissue disorders
Nail fold telangiectasia or erythema is
a useful physical sign in dermatomyositis,
systemic sclerosis and systemic lupus
erythematosus.

Nail changes in the common
dermatoses
Psoriasis
severe nail involvement is more likely in the presence of
arthritis.
The best-known nail change is pitting of the surface of the nail
plate
Psoriasis under the nail plate, showing up as red or brown
areas resembling oil spots, often with onycholysis
Eczema
Some patients with itchy chronic eczema bring their nails to a
high state of polish by scratching.
eczema of the nail folds may lead to a coarse irregularity with
transverse ridging of the adjacent nail plates.

Nail changes in the common
dermatoses
Lichen planus
Some 10% of patients with lichen planus have nail
changes.
reversible thinning of the nail plate with irregular
longitudinal grooves and ridges.
pterygium in which the cuticle grows forward
over the base of the nail and attaches itself to the
nail plate
Alopecia areata
The more severe the hair loss, the more likely
there is to be nail involvement.
fine pitting and the lunulae may appear mottled.
Infections
Acute paronychia
The portal of entry for the organisms is a
break in the skin or cuticle as a result of
minor trauma
usually staphylococci
Aute inflammation, often with the formation
of pus in the nail fold or under the nail
requires systemic treatment with
flucloxacillin, cephalexin or erythromycin and
appropriate surgical drainage.
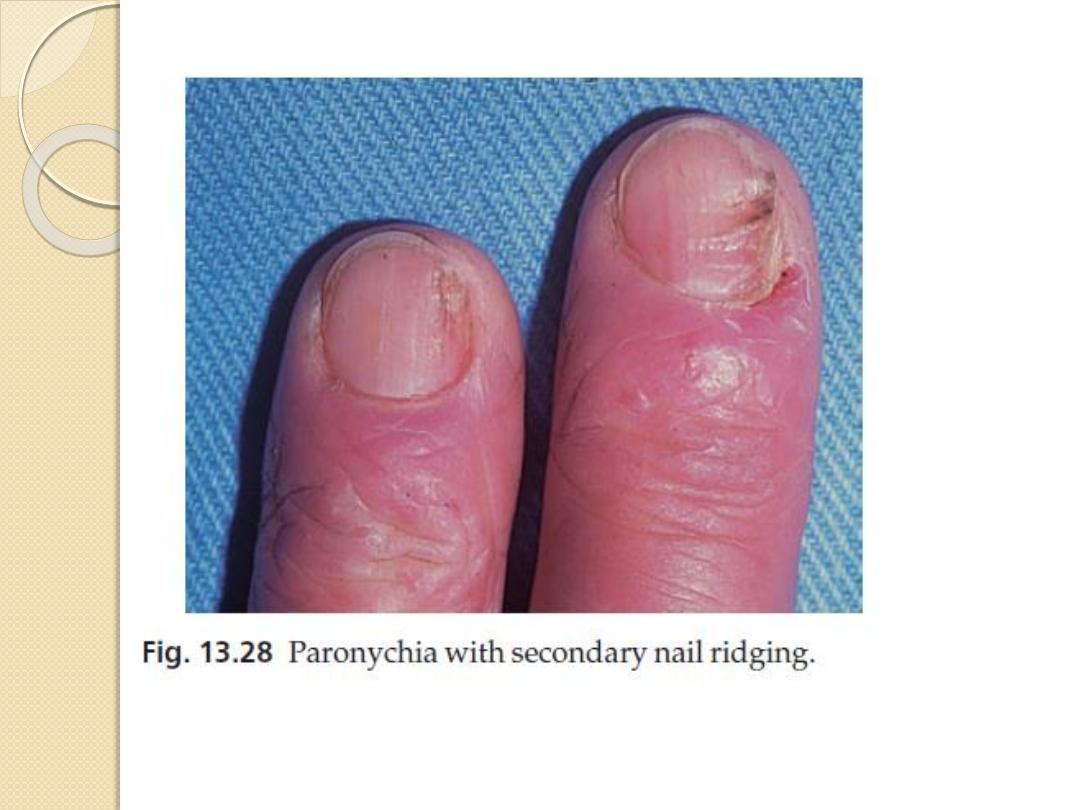
Chronic paronychia
Cause
A combination of circumstances can allow a
mixture of opportunistic pathogens (yeasts,
Gram-positive cocci and Gram-negative
rods) to colonize the space between the nail
fold and nail plate, producing a chronic
dermatitis.
Predisposing factors include a poor
peripheral circulation, wet work, working
with flour, diabetes, vaginal candidosis and
overvigorous cutting back of the cuticles.
Chronic paronychia
Presentation and course
The nail folds become tender and swollen and small
amounts of pus are discharged at intervals.
the adjacent nail plate becomes ridged and
discoloured.
The condition may last for years.
Differential diagnosis
amelanotic melanoma
Paronychia should not be
dermatophyte infection
Investigations
Test the urine for sugar, check for vaginal and oral
candidosis. Pus should be cultured.
Chronic paronychia
Treatment
Treatment is aimed at both the infective and
dermatitic elements of the condition.
The hands should be kept as warm and as dry as
possible
the damaged nail folds packed several times a day
with an imidazole cream
Highly potent topical corticosteroid creams
applied for 3 weeks also help.
If there is no response, and swabs confirm that
Candida is present, a 2-week course of
itraconazole should be considered
Dermatophyte infections
Cause
The common dermatophytes that cause tinea pedis can
also invade the nails
Presentation
Toe nail infection is common and associated with tinea
pedis.
The early changes often occur at the free edge of the
nail and spread proximally.
The nail plate becomes yellow, crumbly and thickened.
The finger nails are involved less often and usually
confined to one hand.
Nail infection in patients with HIV infections often
involve the proximal subungual skin without distal
involvement.
Dermatophyte infections
Clinical course
The condition seldom clears spontaneously.
Differential diagnosis
Psoriasis
Coexisting tinea pedis favours dermatophyte
infection of the nail.
Investigations
The diagnosis is confirmed by microscopic
examination of potassium hydroxide-treated nail
clippings
Cultures should be carried out in a mycology
laboratory.
Dermatophyte infections
Treatment
Most symptom-free fungal infections of the
toe nails need no treatment at all.
Topical nail preparations
Both amorolfine and tioconazole nail
solutions can be used as adjuncts to
systemic therapy
Systemic
Terbinafine
Gresofulvin
Itraconazole

Tumours
Periungual warts
Periungual fibromas in patients with
tuberous sclerosis.
Glomus tumours small red or bluish lesions
are exquisitely painful if touched and when
the temperature changes.
Subungual exostoses, protrude painfully
under the nail plate. Usually secondary to
trauma to the terminal phalanx, the bony
abnormality can be seen on X-ray.

Tumours
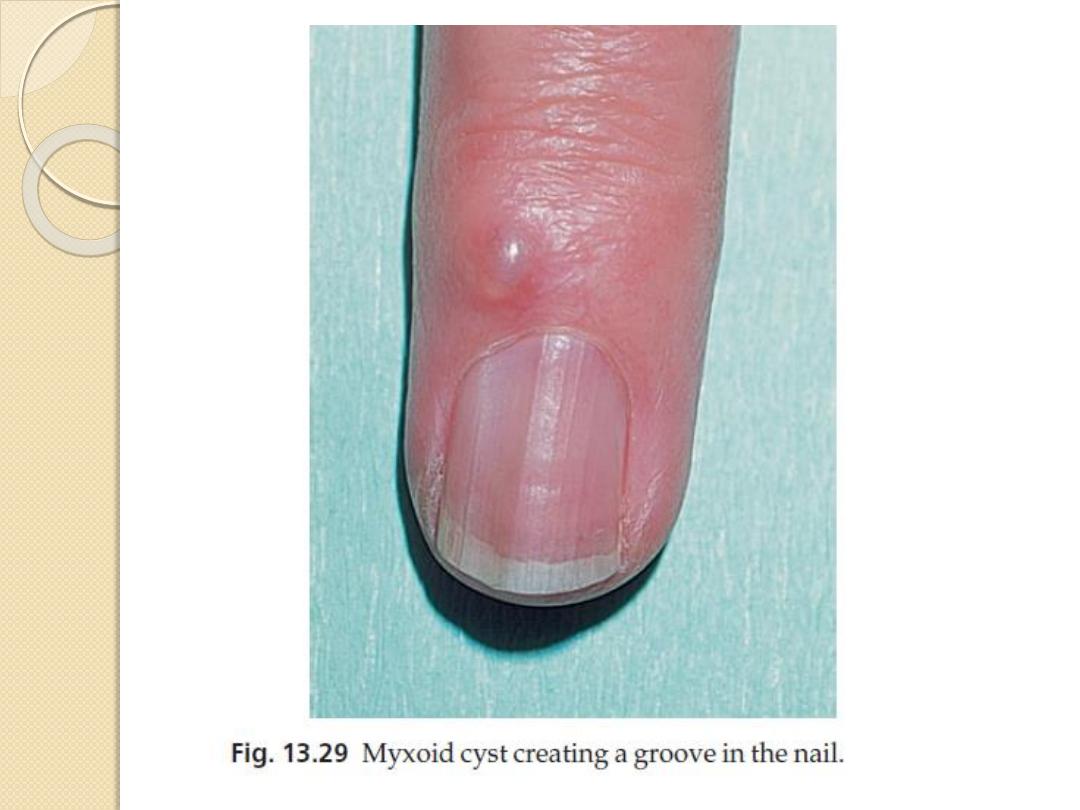
Myxoid cysts occur on the proximal nail
folds, usually of the fingers. The smooth
domed swelling contains a clear jelly-like
material that transilluminates well. A groove
may form on the adjacent nail plate.
Malignant melanoma should be
suspected in any subungual pigmented lesion,
particularly if the pigment spreads to the
surrounding skin (Hutchinson’s sign).
Subungual haematomas may cause confusion
but ‘grow out’ with the nail.
The END
