Papulosquamous diseases
Lichen planus
Pityriasis rosea
Psoriasis
Cause
unknown, but may be mediated immunologically.
There may be a genetic susceptibility to idiopathic
lichen planus
Rarely, familial.
Lichen planus is also associated with autoimmune
disorders, such as alopecia areata, vitiligo and
ulcerative colitis
Contact allergy to mercury compounds (in dental
amalgam fillings) seems to be an important cause of
oral lichen planus
Drugs
Some patients have a hepatitis C infection.

Presentation
Skin lesions
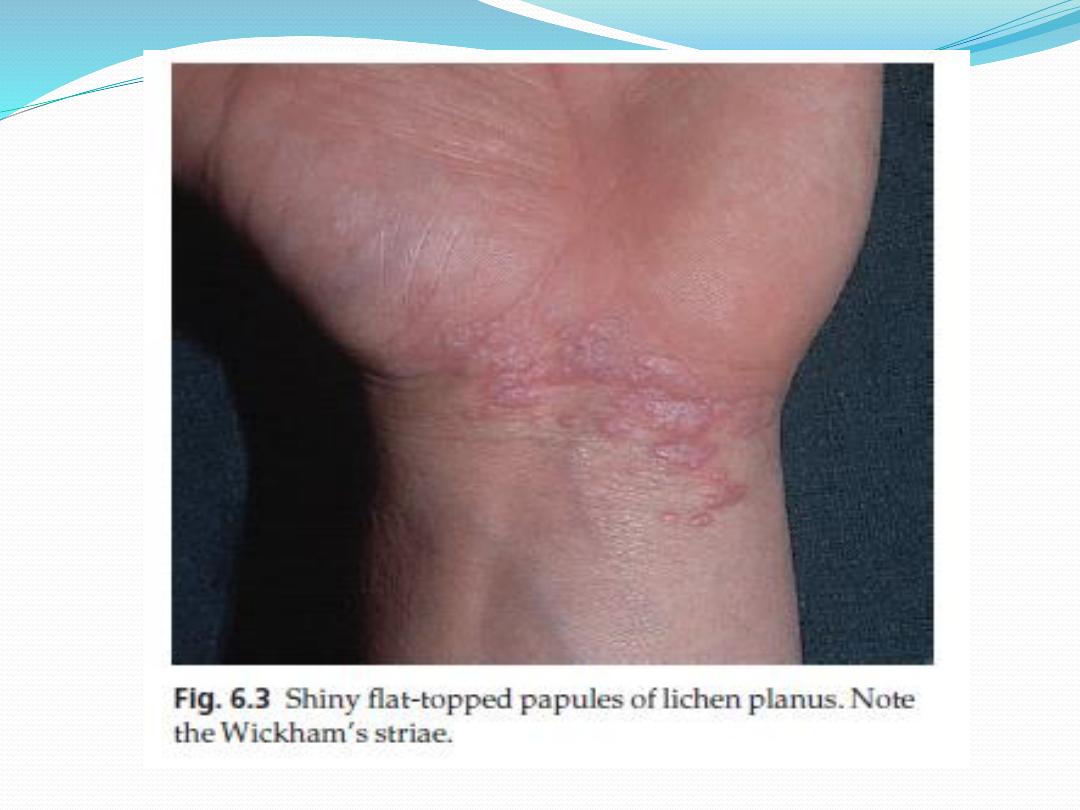
Typical lesions are violaceous or lilac-coloured, intensely itchy, flat-
topped papules that usually arise on the extremities, particularly on the
volar aspects of the wrists and legs
A close look is needed to see a white streaky pattern on the surface of
these papules (Wickham’s striae).
patients rub rather than scratch, so that excoriations are uncommon.
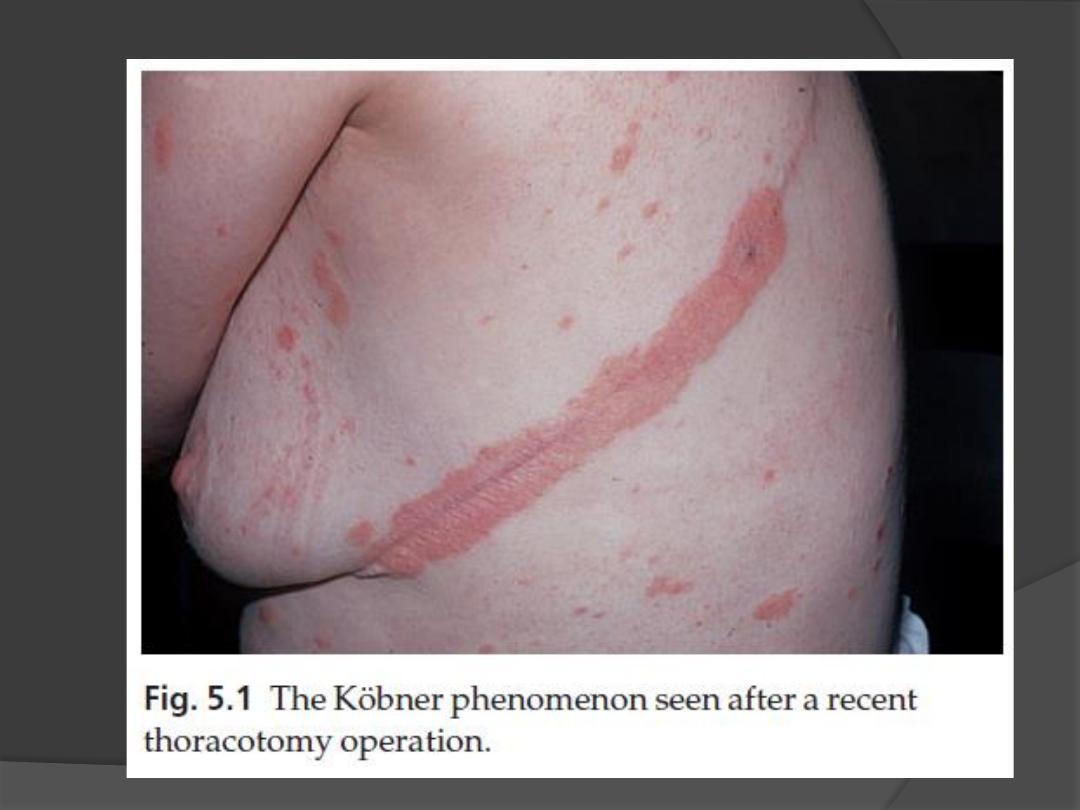
Köbner phenomenon may occur
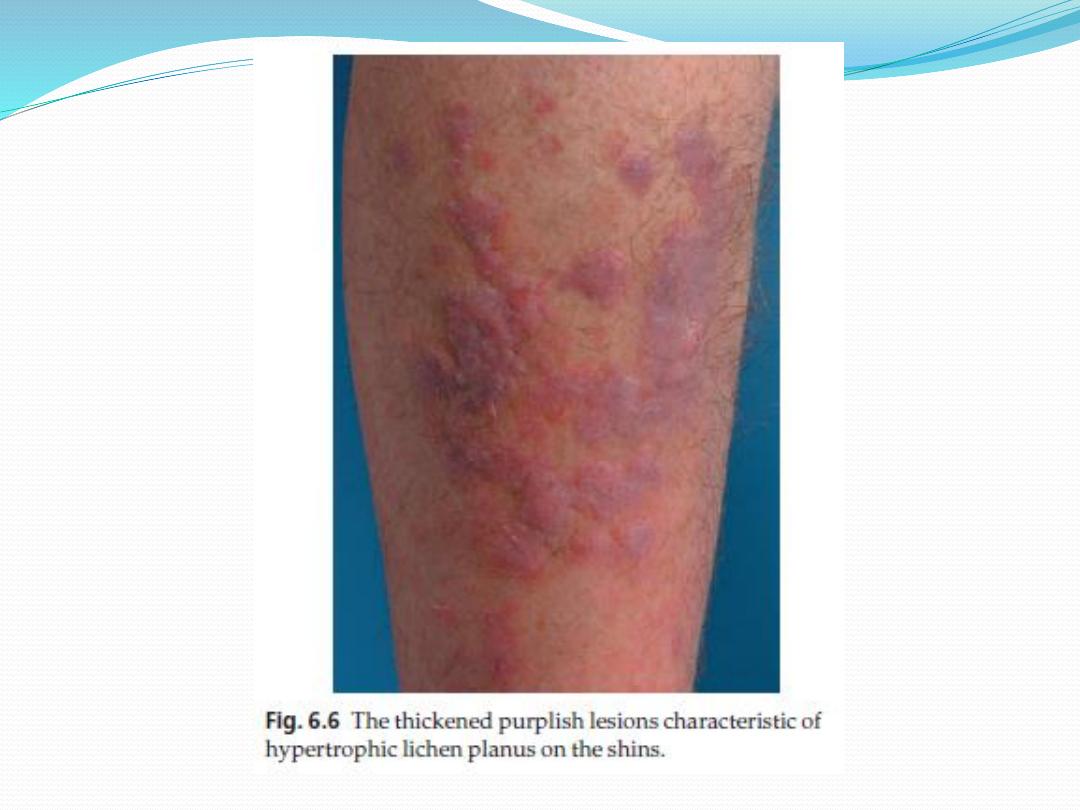
Variants of lichen planus.
Annular
Atrophic
Bullous
Follicular
Hypertrophic

Presentation
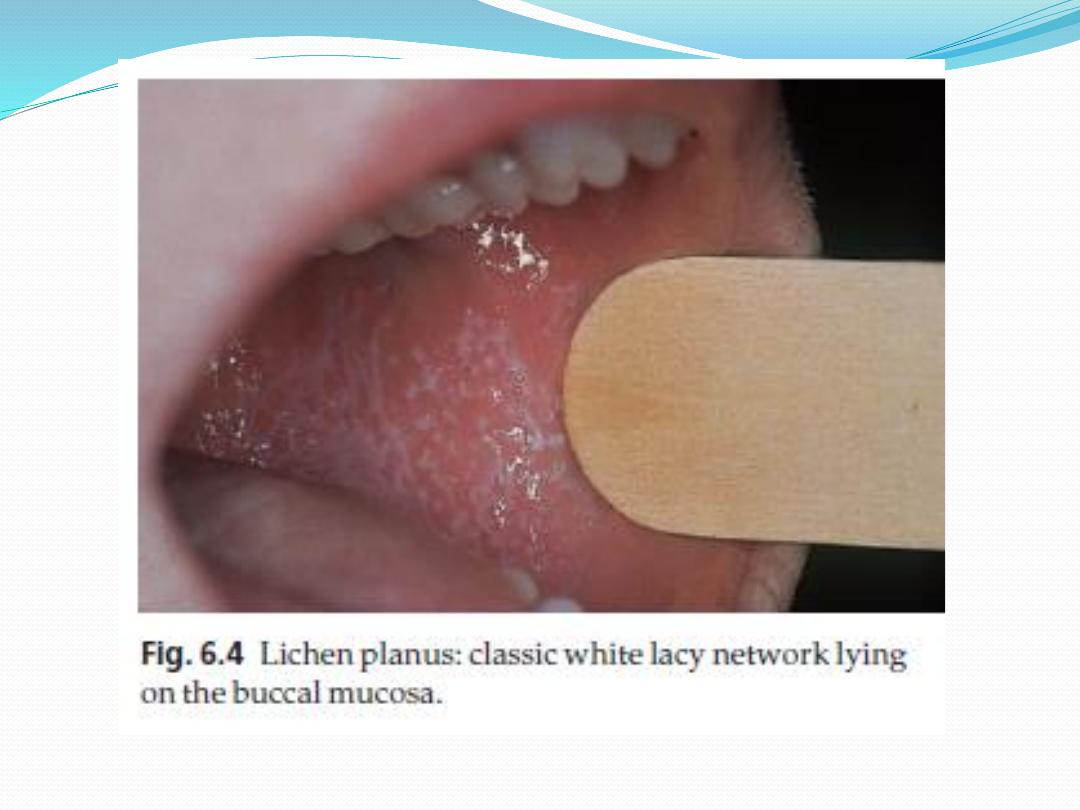
Oral and genital skin lesions
White asymptomatic lacy lines, dots, and occasionally
small white plaques, are also found in the mouth,
particularly inside the cheeks, in about 50% of patients and
oral lesions may be the sole manifestation of the disease.
Nail
The nails are usually normal, but in about 10% of patients
show changes ranging from fine
longitudinal grooves to destruction of the entire nail fold
and bed
Scalp
lesions can cause a patchy scarring alopecia.


Course
Individual lesions may last for many months and the eruption as
a whole tends to last about 1 year.
the hypertrophic variant often lasts for many years.
As lesions resolve, they become darker, flatter and leave discrete
brown or grey macules.
About one in six patients will have a recurrence.
Complications
Nail and hair loss can be permanent
The ulcerative form of lichen planus in the mouth may lead to
squamous cell carcinoma.
Ulceration, usually over bony prominences, may be disabling,
especially if it is on the soles

Differential diagnosis
Lichenoid drug reactions
can mimic lichen planus closely.
Gold and other heavy metals, antimalarials, beta-blockers, non-
steroidal anti-inflammatory drugs, para-aminobenzoic acid,
thiazide diuretics and penicillamine.
Contact with chemicals
used to develop colour photographic film can also produce
similar lesions.
Generalized discoid lupus erythematosus
it may be hard to differentiate from lichen planus
Wickham’s striae or oral lesions favour the diagnosis of lichen
planus.
Oral candidiasis
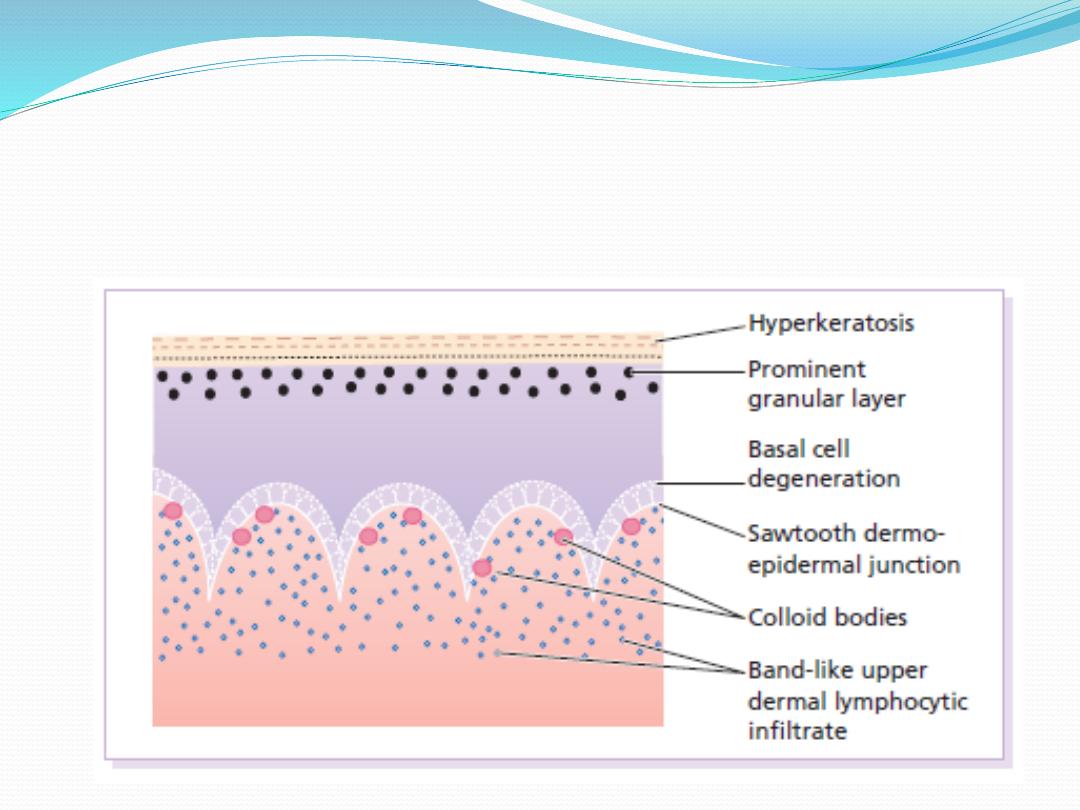
Investigations
histology is characteristic

Treatment
If drugs are suspected as the cause, they should be stopped
and unrelated ones substituted.
Potent topical steroids.
Systemic steroid are recommended in special situations
(e.g. unusually extensive involvement, nail destruction or
painful and erosive oral lichen planus).
PUVA or narrowband UVB
Oral ciclosporin or acitretin with stubborn lichen planus.
Antihistamines may blunt the itch.
Mucous membrane lesions, both oral and genital need no
treatment or use corticosteroid or calcineurin inhibitor.

Pityriasis rosea is a mild inflammatory exanthem
characterized by salmon-colored papular and macular
lesions that are at first discrete but may become
confluent.

Cause
may be caused by reactivation of either human herpes
virus 7 or human herpes virus 6.
The disease may occur in clusters, both geographical
and temporal, and seems not to be contagious.

Presentation
Pityriasis rosea is common, particularly during the winter.
It mainly affects children and young adults, and second
attacks are rare.
Most patients develop one plaque (the ‘herald’ or ‘mother’
plaque) before the others: It is larger (2–5 cm diameter)
than later lesions, and is rounder, redder and more scaly.
After several days many smaller plaques appear, mainly on
the trunk, but some also on the neck and extremities.
About half of patients complain of itching. An individual
plaque is oval, salmon pink and shows a delicate scaling,
adherent peripherally as a collarette.
Their longitudinal axes run down and out from the spine in
a ‘fir tree’ pattern, along the lines of the ribs.
The herald plaque of pityriasis rosea is usually on the
trunk and is larger than the other lesions. Its annular
configuration is shown well here.
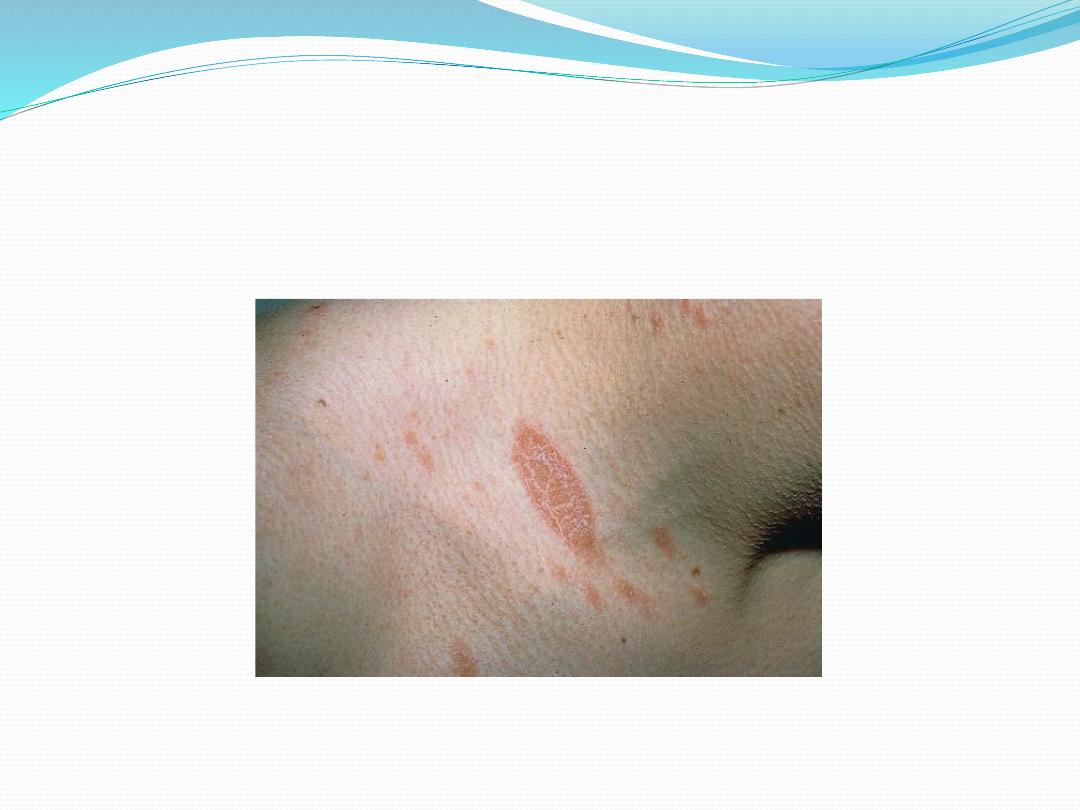
Herald patch of pityriasis rosea

Extensive pityriasis rosea showing
a ‘fir tree’ distribution on the back.
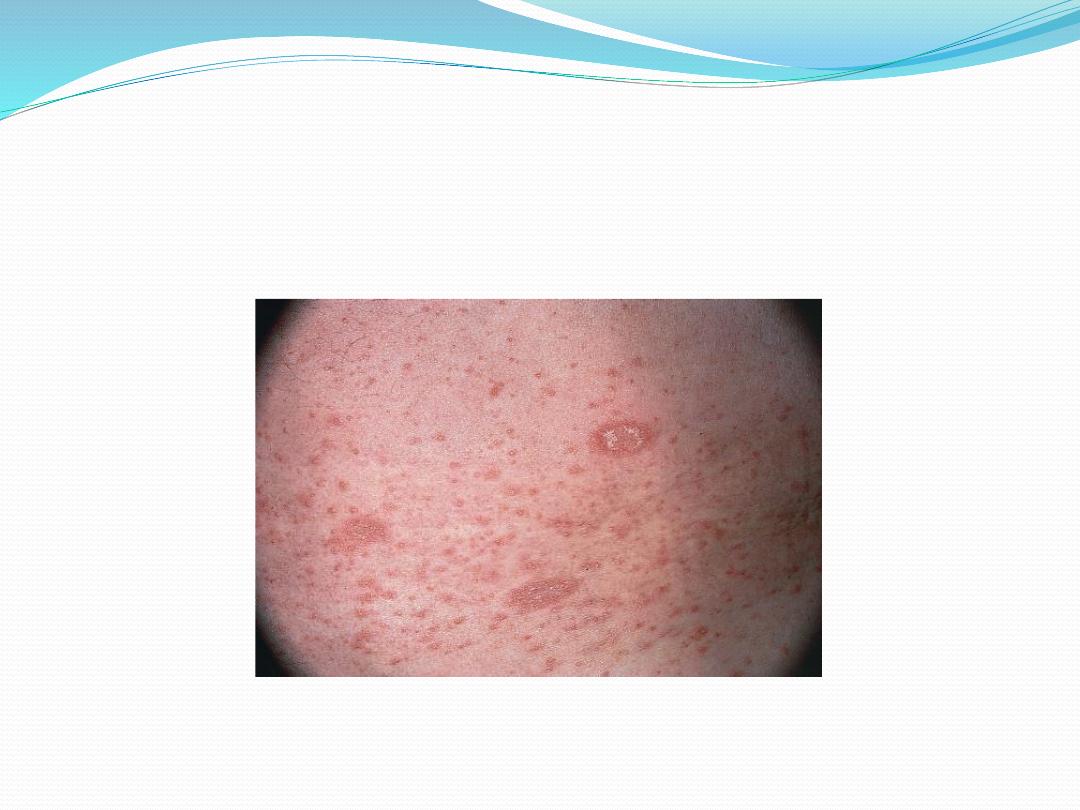
Pityriasis rosea

Course
The herald plaque precedes the generalized eruption
by several days.
Subsequent lesions enlarge over the first week or two.
A minority of patients have systemic symptoms such
as aching and tiredness.
The eruption lasts 2–10 weeks and then resolves
spontaneously, sometimes leaving hyperpigmented
patches that fade more slowly.

Differential diagnosis
Although herald plaques are often mistaken for ringworm
(tinea corporis), the two disorders most likely to be
misdiagnosed early in the general eruption are guttate
psoriasis and secondary syphilis.
Tinea corporis and pityriasis versicolor can be
distinguished by the microscopical examination of scales,
secondary syphilis by its other features (mouth lesions,
palmar lesions, condylomata lata, lymphadenopathy,
alopecia) and by serology.
Gold and captopril are the drugs most likely to cause a
pityriasis rosea-like drug reaction, but barbiturates,
penicillamine, some antibiotics and other drugs can also do
so.
Treatment
No treatment is curative, and active treatment is
seldom needed.
A moderately potent topical steroid or calamine lotion
will help the itching.
One per cent salicylic acid in soft white paraffin or
emulsifying ointment reduces scaling.
Sunlight or artificial UVB often relieves pruritus and
may hasten resolution.
So far, treatment with antiviral agents has not been
helpful.

Psoriasis
Psoriasis is a chronic, non-infectious,
inflammatory skin disorder, characterized by
well-defined salmonpink plaques bearing large
adherent silvery centrally attached scales.
1-3 % of most populations have psoriasis
uncommon in American black people and
almost non-existent in American Indians.
It can start at any age but is rare under 10
years, and appears most often between 15
and 40 years.
Its course is unpredictable but is usually
chronic with exacerbations and remissions.

Psoriasis
The precise cause of psoriasis is still unknown. But
there is :
1.
genetic predisposition
2.
environmental trigger
There are two key abnormalities in a psoriatic
plaque:
1.
hyperproliferation of keratinocytes
2.
inflammatory cell infiltrate in which neutrophils,
tumour necrosis factor and probably Th17 type T
lymphocytes predominate.
Both of these abnormalities can induce the other,
leading to a vicious cycle of keratinocyte proliferation
and inflammatory reaction

Psoriasis
Precipitating factors
1. Trauma If the psoriasis is active (Köbner phenomenon)
2 .
Infection Tonsillitis caused by β-haemolytic
streptococci often triggers guttate psoriasis.
3 .Hormonal Psoriasis frequently improves in pregnancy
only to relapse postpartum.
4 .Sunlight Improves most psoriatics but 10% become
worse.
5 .Drugs Antimalarials, beta-blockers, IFN-
α and steroid
6 .Cigarette smoking and alcohol
7 .Emotional upset

Pathogenisis

Genetics
There are two inheritance modes.
One type has onset in youth and a more common family
history of psoriasis, and the other has onset in late adulthood
in patients without obvious family history.
Inheritance is polygenic
A child with one affected parent has a 16% chance of
developing the disease, and this rises to 50% if both parents
are affected.
psoriatic fathers are more likely to pass on the disease to
their children than are psoriatic mothers.
If non-psoriatic parents have a child with psoriasis, the risk
for subsequent children is about 10%.

Genetics
concordant is 70% of monozygotic twins but in
only 20% of dizygotic ones.
Early-onset psoriasis shows a genetic linkage
with a psoriasis susceptibility locus (PSOR-1)
located on 6p21
PSORS-1 is the most important locus in
psoriasis, accounting for up to 50% of genetic
susceptibility to the disease
Eeight other loci (PSORS-2 to 9) have been
identified.
HLA-Cw6 genotype developing psoriasis is 20
times that of those without it

Epidermal cell kinetics
The epidermis of psoriasis replicates too
quickly
Keratinocytes proliferate out of control, and
an excessive number of germinative cells
enter the cell cycle.
The growth fraction of epidermal basal
cells is greatly increased to almost 100%
compared with 30% in normal skin
The epidermal turnover time is greatly
shortened, to less than 10 days compared
with 30 to 60 days in normal skin.

Inflammation
Immune events may well have a primary
role in the pathogenesis of the disease
of psoriasis
Inflammatory cells especially neutrophils
and lymphocytes
Release of inflammatory cytokines and
mediators

Histology
The main changes are the following.
1 Parakeratosis (nuclei retained in the horny layer).
2 Irregular thickening of the epidermis over the rete
ridges, but thinning over dermal papillae. Bleeding
may occur when scale is scratched off (Auspitz
’s sign).
3 Epidermal polymorphonuclear leucocyte
infiltrates
and micro-abscesses (described originally by Munro).
4 Dilated and tortuous capillary loops in the dermal
papillae.
5 T-lymphocyte infiltrate in upper dermis.
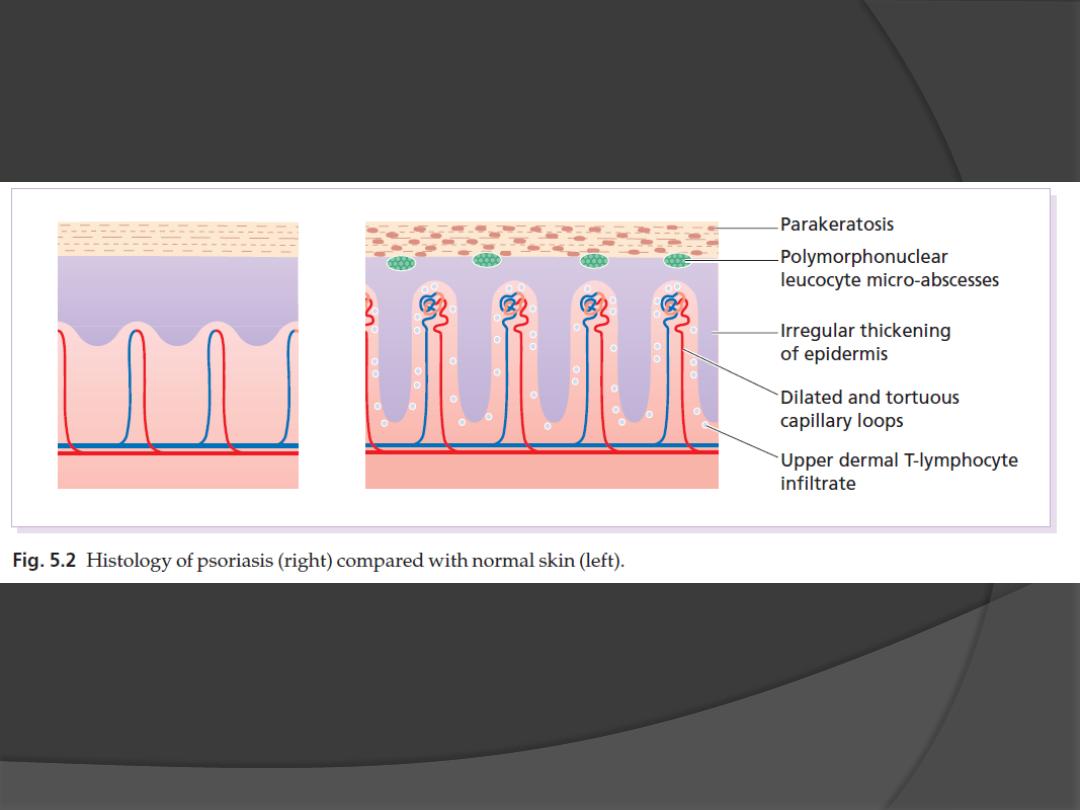
Histology

Psoriasis
Plaque pattern
•
most common type
•
Lesions are well demarcated and range from a
few millimetres to many centimetres in diameter
•
The lesions are pink or red with large, centrally
adherent, silvery white, polygonal scales.
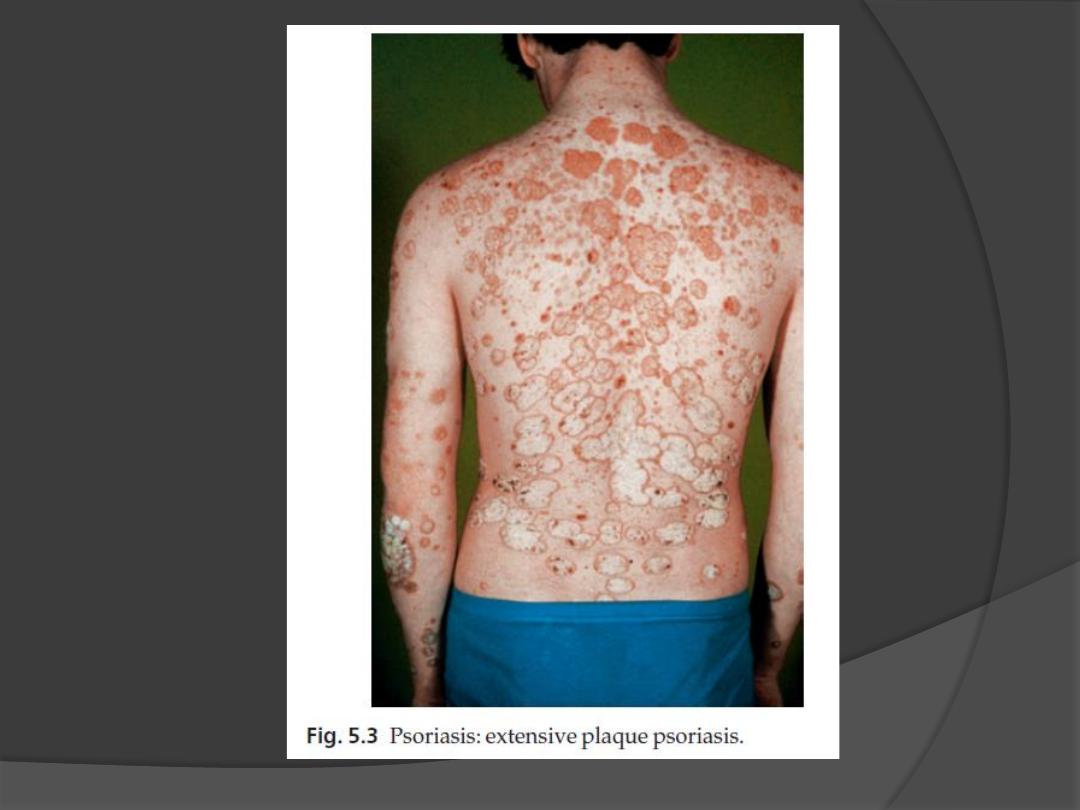
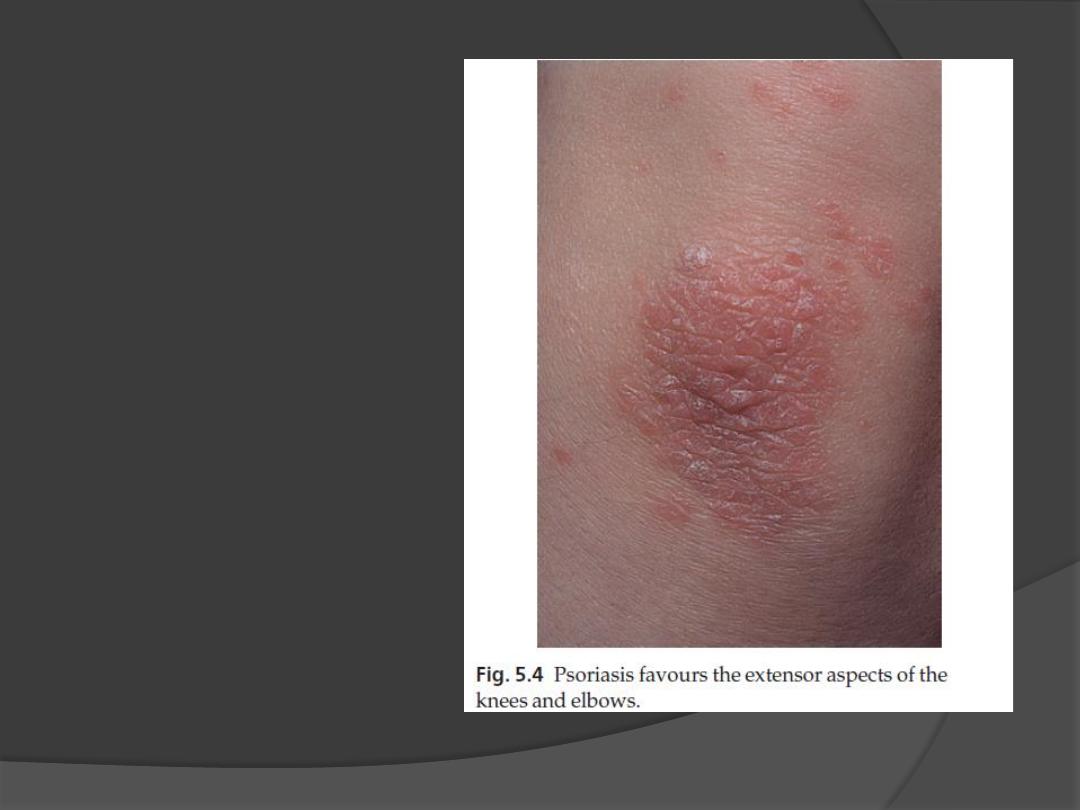
•
Symmetrical sites
on the elbows,
knees, lower back
and scalp are sites
of predilection
Psoriasis

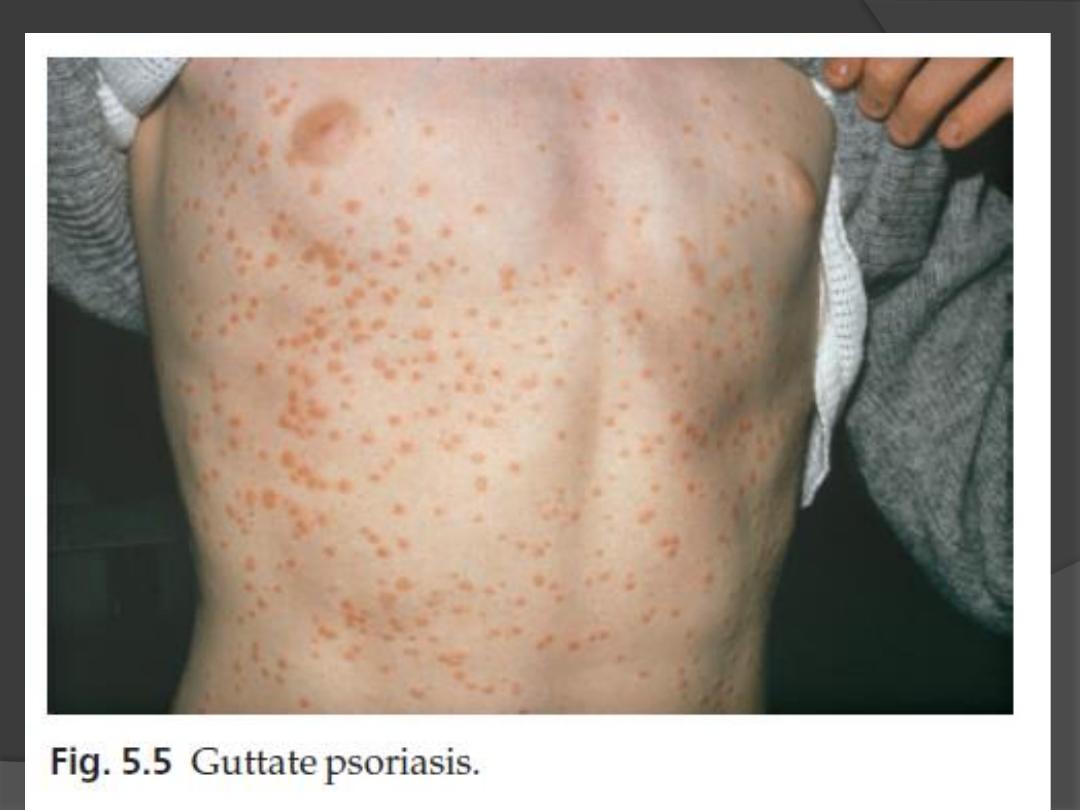
Guttate psoriasis
•
The word
‘guttate’ means ‘drop-shaped’.
•
seen in children and adolescents
•
may be the first sign of the disease
•
often triggered by streptococcal tonsillitis.
•
Numerous small round red macules come up
suddenly on the trunk and soon become scaly
•
The rash often clears in a few months but
plaque psoriasis may develop later
Psoriasis
Psoriasis
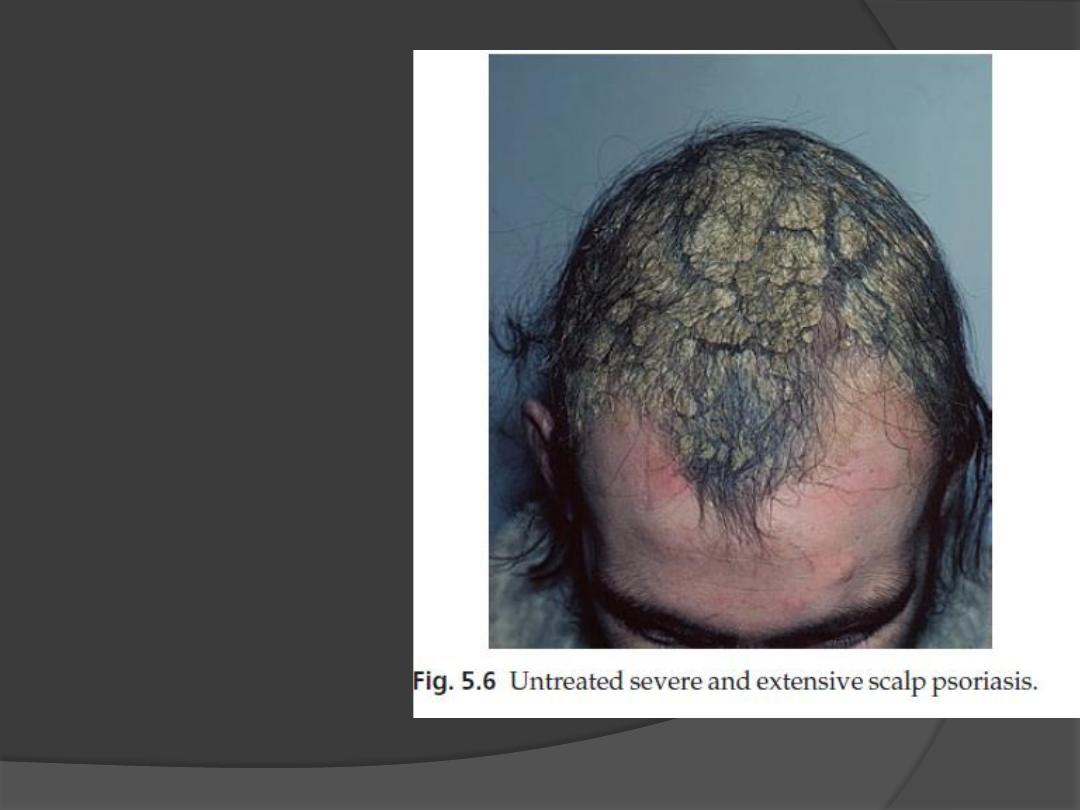
Scalp
•
often involved
•
the psoriasis
overflows just
beyond the scalp
margin
•
Significant hair
loss is rare

•
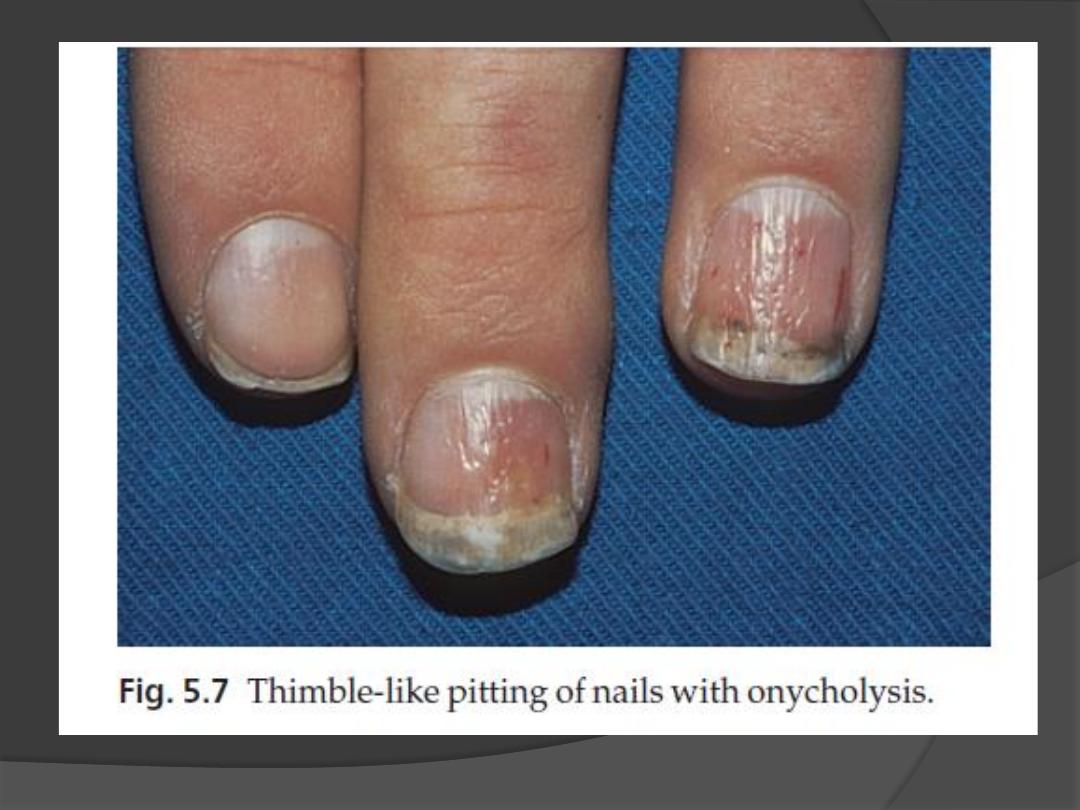
Involvement of the nails is common
•
Thimble pitting
•
onycholysis (separation of the nail from
the nail bed
•
sometimes subungual hyperkeratosis
Psoriasis
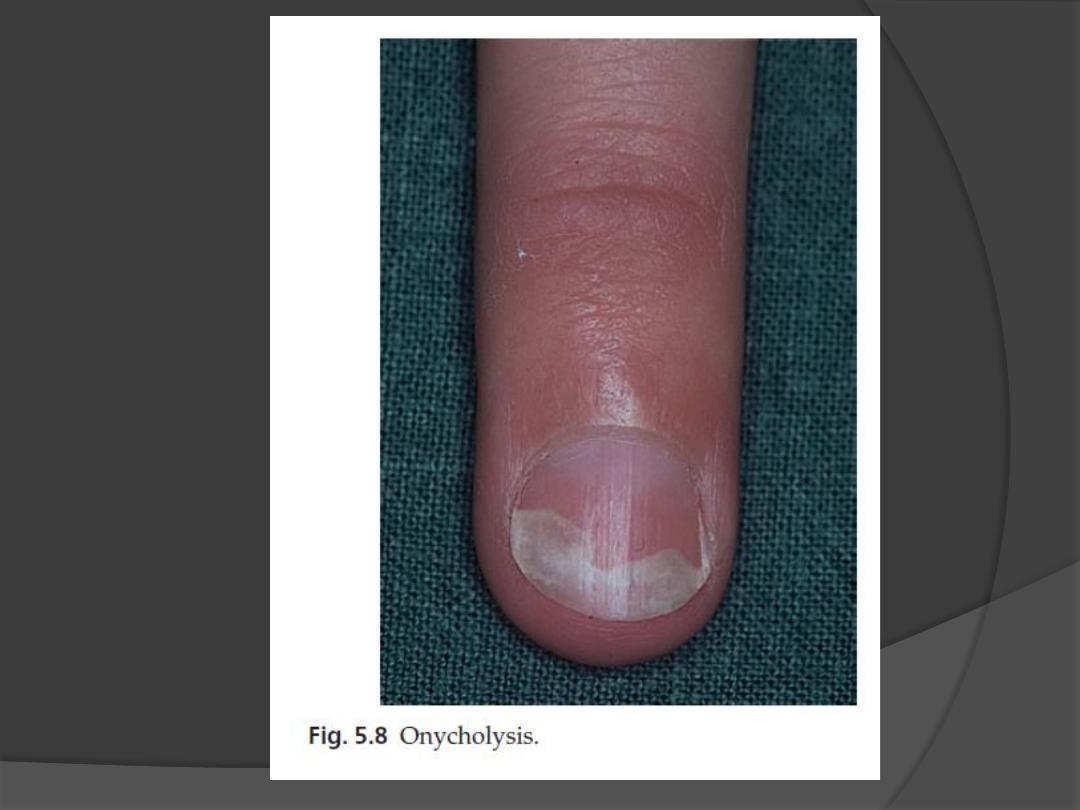
Onycolysis

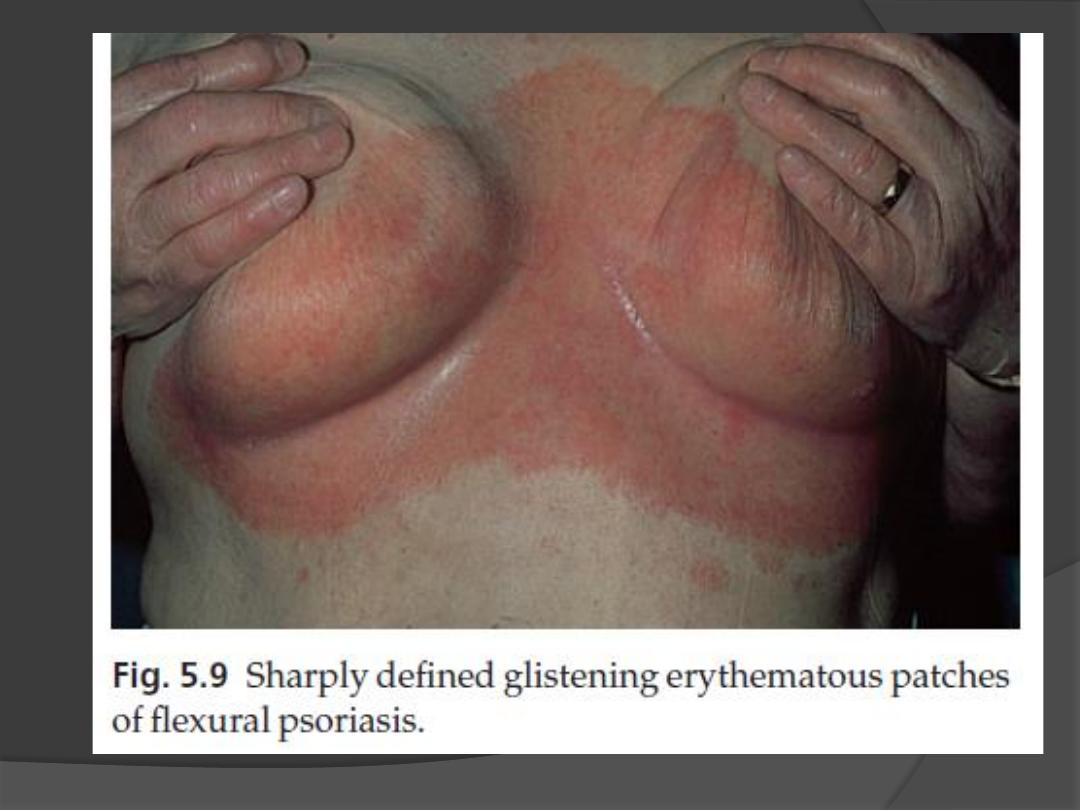
Flexures
•
Psoriasis of the submammary, axillary and anogenital
folds is not scaly although the glistening sharply
demarcated red plaques often with fissuring in the depth
of the fold, are still readily recognizable.
•
Flexural psoriasis is most common in women and in the
elderly, and is more common among HIV infected
individuals
Psoriasis

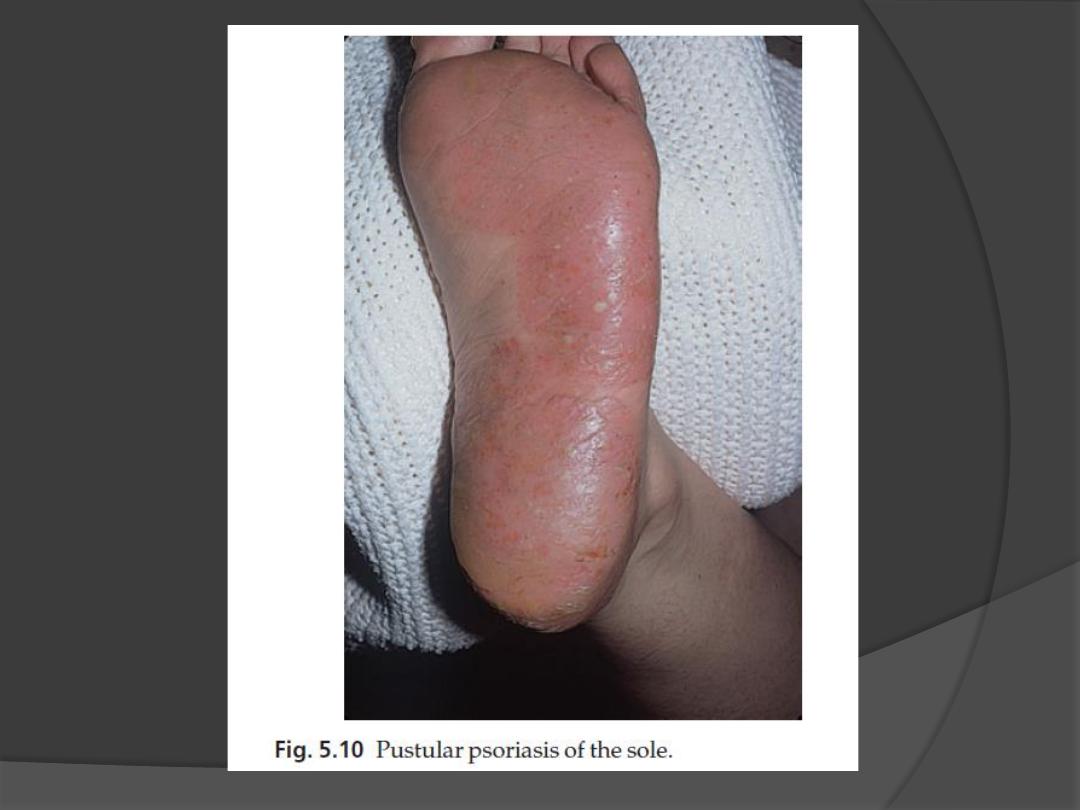
Palms and soles
•
Palmar psoriasis may be hard to recognize, as its
lesions are often poorly demarcated and barely
erythematous.
•
The fingers may develop painful fissures.
•
At other times lesions are inflamed and studded with
1
–2 mm pustules (palmoplantar pustulosis)
Psoriasis

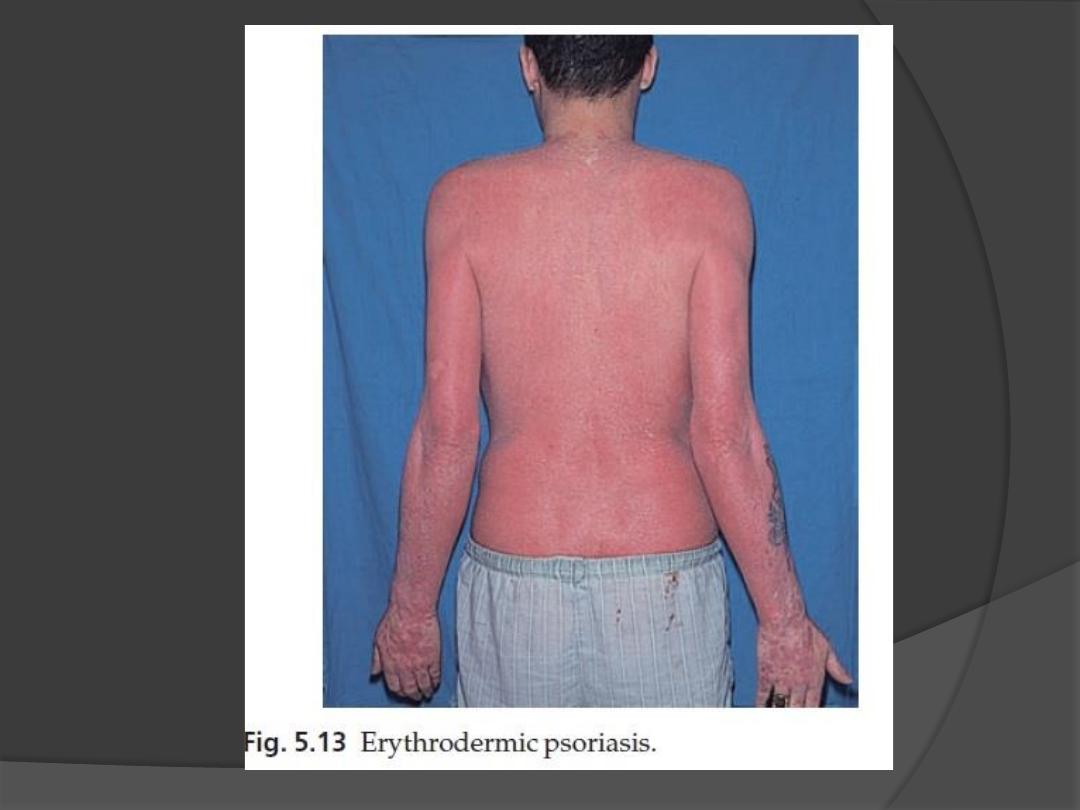
Erythrodermic psoriasis
•
Rare
•
Sparked off by:
1.
irritant effect of tar or dithranol
2.
by a drug
3.
by the withdrawal of potent topical or systemic steroids.
•
The skin becomes universally and uniformly red with variable
scaling.
•
Malaise is accompanied by shivering and the skin feels hot and
uncomfortable.
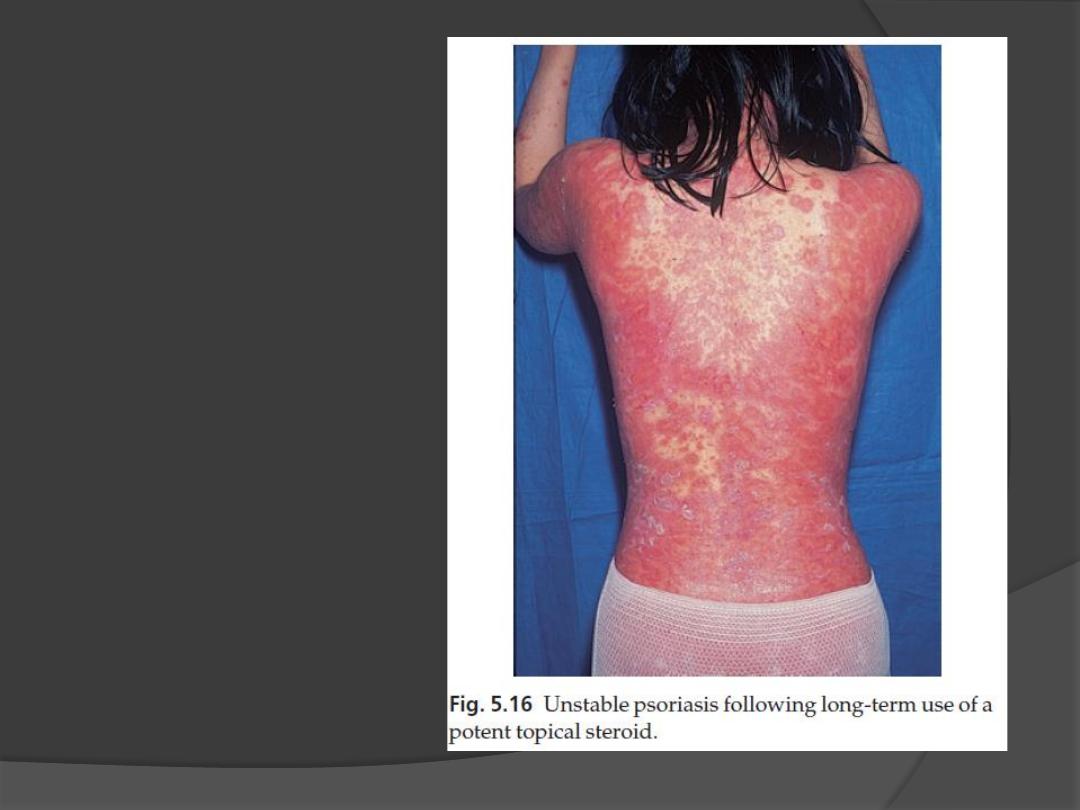
Unstable psoriasis.
following long-term use
of potent topical steroid

Complications
Psoriatic arthropathy
occurs in about 5
–20% of psoriatics.
Distal arthritis involves the terminal interphalangeal
joints of the toes and fingers, especially those with
marked nail changes
involvement of a single large joint; one that mimics
rheumatoid arthritis and may become mutilating
Tests for rheumatoid factor are negative and nodules
are absent.
In patients with spondylitis and sacroiliitis there is a
strong correlation with the presence of HLA-B27.

Differential diagnosis
Discoid eczema
Seborrhoeic eczema
Pityriasis rosea
Secondary syphilis
Cutaneous T-cell lymphoma
Tinea unguium

Investigations
1.
Biopsy is seldom necessary
2.
Throat swabbing for
β-haemolytic
streptococci is needed in guttate
psoriasis.
3.
Skin scrapings and nail clippings
may be required to exclude tinea.
4.
Radiology and tests for rheumatoid
factor are helpful in assessing arthritis.

Treatment
General measures
Explanations and reassurances
treatment must never be allowed to be more
troublesome than the disease itself.
At present there is no cure for psoriasis; all
treatments are suppressive and aimed at
either inducing a remission or making the
condition more tolerable.
spontaneous remissions will occur in 50%of
patients.
Concomitant anxiety and depression should
be treated on their own merits

Treatment
Local treatments
Vitamin D analogues
Calcipotriol (calcipotriene, USA), calcitriol and
tacalcitol
Used for mild to moderate psoriasis affecting less
than 40% of the skin
Patients like calcipotriol because it is odourless,
colourless and does not stain.
It seldom clears plaques of psoriasis completely, but
does reduce their scaling and thickness.
Local and usually transient irritation may occur with
the recommended twice-daily application

Treatment
Local retinoids
Tazarotene is a topically active retinoid
It is recommended for chronic stable
plaque psoriasis on the trunk and limbs
covering up to 20% of the body.
its main side-effect is irritation
The drug should not be used in pregnancy
or during lactation or children below 12
year.
Females of child-bearing age should use
adequate contraception during therapy

Treatment
Topical corticosteroids
topical corticosteroids are most helpful and use them as
the mainstay of their long-term management of stable
plaque psoriasis.
Patients like them because they are clean and reduce
scaling and redness.
Used if other treatments are ineffective or contraindicated
or for localized psoriasis
SE
dermal atrophy
tachyphylaxis
early relapses
the occasional precipitation of unstable psoriasis
rarely, in extensive cases, of adrenal suppression caused
by systemic absorption.

Treatment
Dithranol (anthralin)
it inhibits DNA synthesis and form free
radicals of oxygen.
Dithranol is too irritant to apply to the
face, the inner thighs, genital region or
skin folds
It also stain clothes purple
–brown

Treatment
Coal tar preparations
The less refined tars are smelly, messy and
stain clothes, but are more effective than
the cleaner refined preparations.
Calcineurin inhibitors (topical
immunomodulators)
Both tacrolimus and pimecrolimus have
been used, but they are usually too weak
to do much except for psoriasis on the
face, genitals or intertriginous areas

Treatment
Ultraviolet radiation
Most patients improve with natural sunlight and
should be encouraged to sunbathe
Both broadband and narrowband UVB can be used.
Narrowband UVB at wavelength 311 nm is especially
effective for clearing psoriasis while minimizing
exposure to potentially carcinogenic wavelengths
less than 300 nm
The main risk of UVB therapies in the short term is
acute phototoxicity (sunburn-like reaction) and, in the
long term, the induction of photodamage and skin
cancer

Special situations
Scalp psoriasis
This is often recalcitrant.
Oily preparations containing 3
–6% salicylic acid are useful
They should be rubbed into the scalp three times a week
and washed out with a tar shampoo 4
–6 h later.
Salicylic acid and tar combinations are also effective.
Guttate psoriasis
A course of penicillin V or erythromycin is indicated for
any associated streptococcal throat infection.
Bland local treatment is often enough as the natural trend
is towards remission.
Suitable preparations include emulsifying ointment and
zinc and ichthammol cream. Tar
–steroid preparations are
reasonable alternatives.

Systemic treatment
A systemic approach should be considered
for extensive psoriasis (more than 20%
of the body surface) that fails to improve
with prolonged courses of tar or
dithranol
for patients whose quality of life is low

PUVA
An oral dose of 8-methoxypsoralen (8-MOP) or 5-
methoxypsoralen (5-MOP) is followed by exposure to
long-wave ultraviolet radiation (UVA: 320
–400 nm).
inhibits DNA synthesis and epidermal cell division.
Psoralens may also be administered in bath water
for those unable to tolerate the oral regimen.
Treatment is given two or three times a week with
increasing doses of UVA, depending on erythema
production and the therapeutic response.
Protective goggles are worn during radiation and
UVA opaque plastic glasses must be used after
taking the tablets and for 24 h after each treatment

PUVA
Side-effects
Painful erythema is the most common side-effect
One-quarter of patients itch during and immediately
after radiation
Long-term side-effects include premature ageing of
the skin (with mottled pigmentation, scattered
lentigines, wrinkles and atrophy), cutaneous
Malignancies , cataract formation. The use of UVA-
blocking glasses for 24 h after each treatment should
protect against the latter.
The long-term side-effects relate to the total amount
of UVA received over the years; this must be
recorded and kept as low as possible
Retinoids
Acitretin (10
–25 mg/day) is an analogue of vitamin A, and is one
of the few drugs helpful in pustular psoriasis
Retinoids and PUVA act synergistically and are often used
together in the so-called Re-PUVA regimen. This clears plaque
psoriasis quicker than PUVA alone, and needs a smaller
cumulative dose of UVA
S.E
1.
Minor side effects are frequent and dose related. They include
dry lips, mouth, vagina and eyes, peeling of the skin, pruritus
and unpleasant paronychia.
2.
Hair thinning or loss is common
3.
Liver damage and hyperlipidemia
4.
most important side-effect is teratogenicity so acitretin should
not normally be prescribed to women of child-bearing age.
Effective oral contraceptive measures must be taken for 2 years
after treatment has ceased.
Blood donation should be avoided for a similar period

Methotrexate
inhibition of both dihydrofolate reductase, and (AICAR)
transferase
Folate supplementation may reduce methotrexate toxicity,
Minor and temporary side effects, such as nausea and malaise,
are common in the 48 h after administration.
The most serious drawback to this treatment is hepatic fibrosis
Monitored by liver biopsy to exclude active liver disease has
been advised for those with risk factors, and repeated after
every cumulative dose of 1.5
–2 g or serial assays of serum
procollagen III aminopeptide (PIIINP)
Blood checks to exclude marrow suppression, and to monitor
renal and liver function, should also be performed
The drug is teratogenic and should not be given to females in
their reproductive years. Oligospermia has been noted in men
and fertility may be lowered

Ciclosporin
inhibits cell-mediated immune reactions
effective in severe psoriasis
side-effects of long-term treatment include
hypertension, kidney damage and persistent
viral warts with a risk of skin cancer
Combination therapy
If psoriasis is resistant to one treatment, a
combination of treatments used together may
be the answer. Combination treatments can
even prevent side-effects by allowing less of
each drug to be used.

Anti TNF-a
1.
Etanercept, recommended as the first
line biological agent
2.
Infliximab
Inhibits T-cell activation drugs:
1.
Alefacept
2.
Efalizumab
They all are very effective, but also very
costy
Thanks
