WOUNDS
The SKIN
- is the outer envelope of the body.
- is the largest organ of the body.
- measures about 2 square meter surface
area.
The anatomical features of skin,
including its
-thickness
-amount of dermis
-hair distribution
-number of its appendages and
-pigmentation
are variable from one area to another.
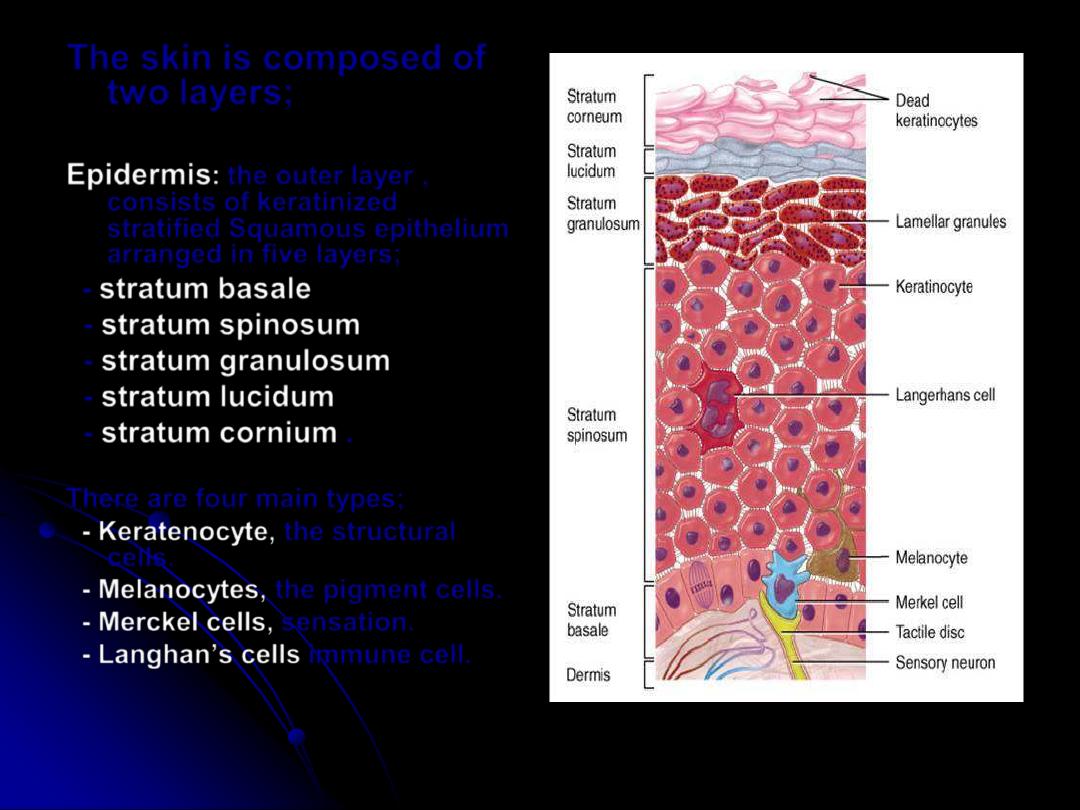
The skin is composed of
two layers;
Epidermis
:
the outer layer ,
consists of keratinized
stratified Squamous epithelium
arranged in five layers;
-
stratum basale
-
stratum spinosum
-
stratum granulosum
-
stratum lucidum
-
stratum cornium
.
There are four main types;
- Keratenocyte,
the structural
cells.
- Melanocytes,
the pigment cells.
- Merckel cells,
sensation.
-
Langhan’s cells
immune cell.
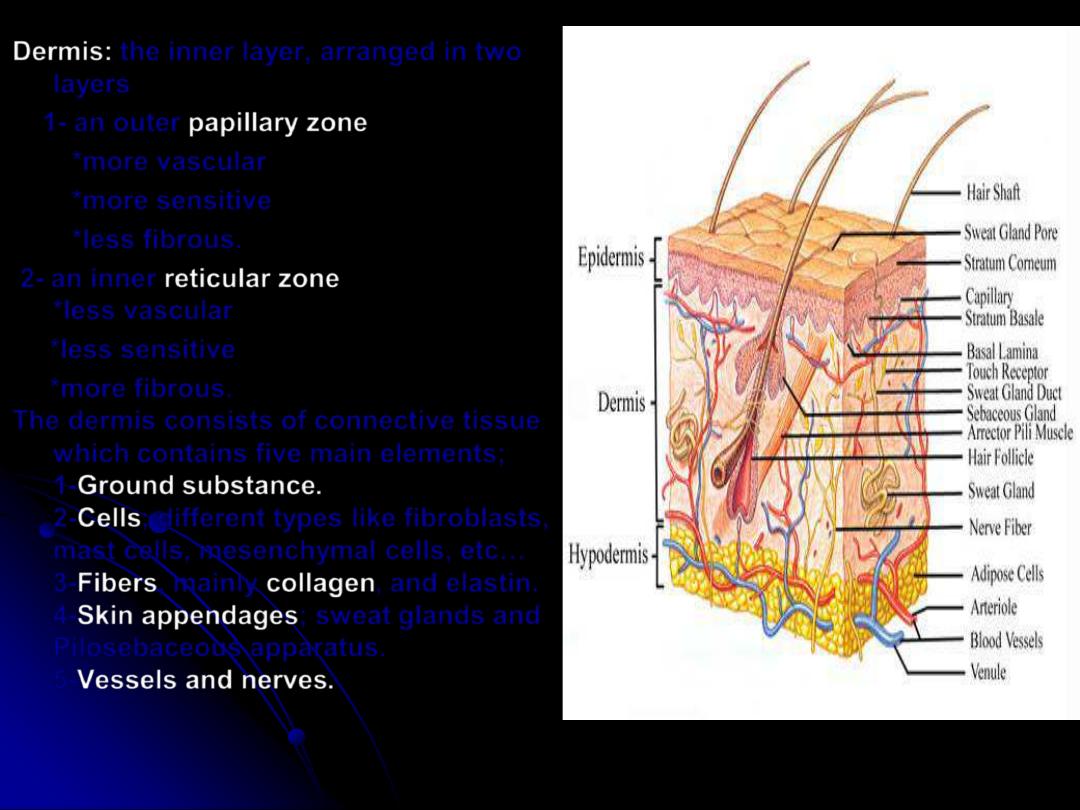
Dermis
:
the inner layer, arranged in two
layers
1- an outer
papillary zone
*more vascular
*more sensitive
*less fibrous.
2- an inner
reticular zone
*less vascular
*less sensitive
*more fibrous.
The dermis consists of connective tissue
which contains five main elements;
1-
Ground substance
.
2-
Cells
; different types like fibroblasts,
mast cells, mesenchymal cells, etc…
3-
Fibers
, mainly
collagen
, and elastin.
4-
Skin appendages
; sweat glands and
Pilosebaceous apparatus.
5-
Vessels and nerves
.
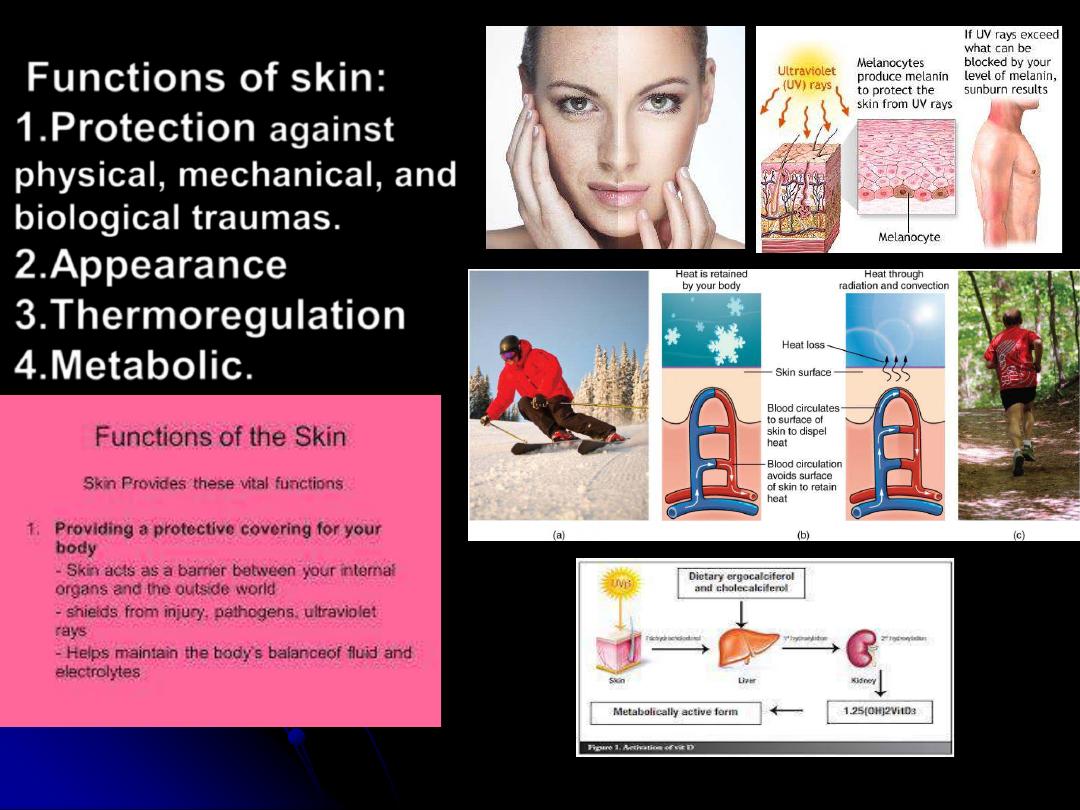
Functions of skin:
1.
Protection
against
physical, mechanical, and
biological traumas.
2.
Appearance
3.
Thermoregulation
4.
Metabolic
.
Wound:
break in tissue continuity.
Types:
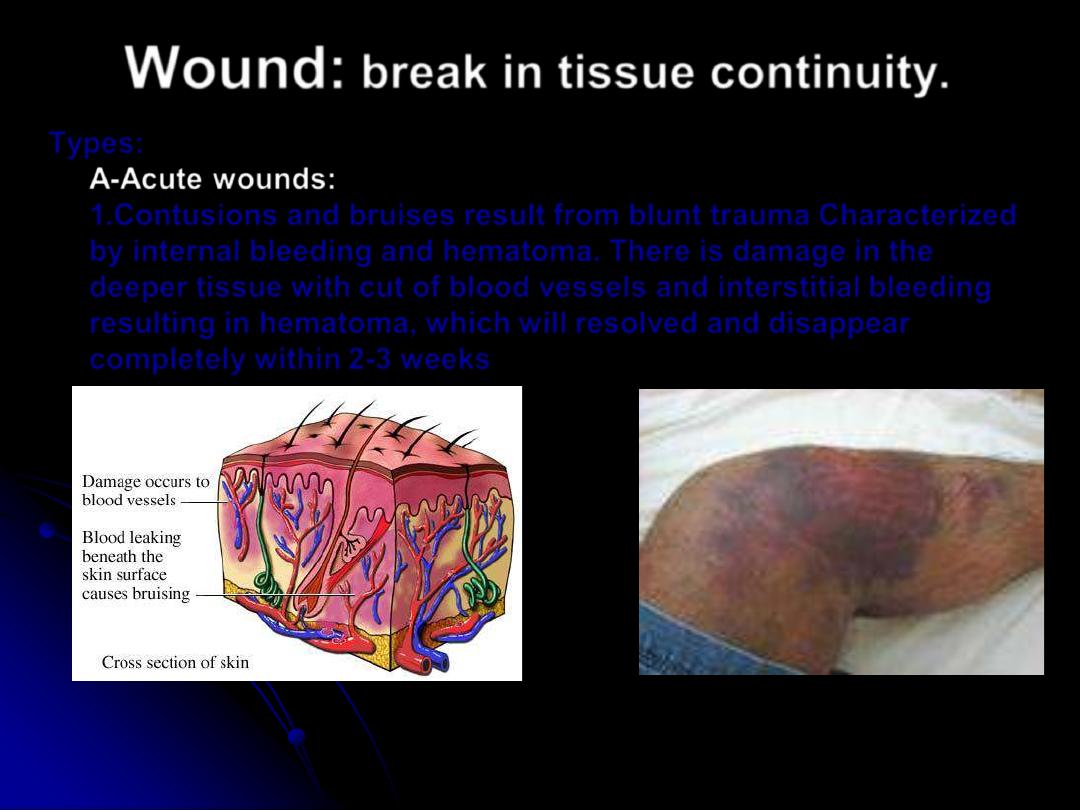
A-Acute wounds:
1.Contusions and bruises result from blunt trauma Characterized
by internal bleeding and hematoma. There is damage in the
deeper tissue with cut of blood vessels and interstitial bleeding
resulting in hematoma, which will resolved and disappear
completely within 2-3 weeks
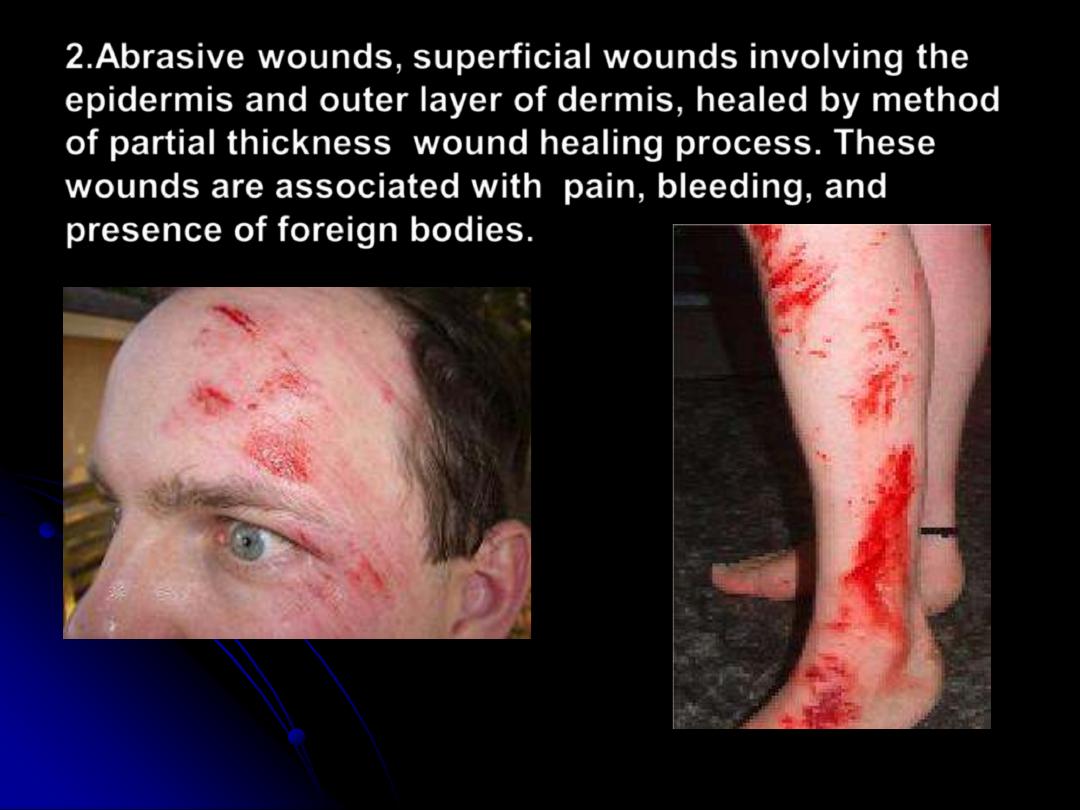
2.Abrasive wounds,
superficial wounds involving the
epidermis and outer layer of dermis, healed by method
of partial thickness wound healing process. These
wounds are associated with pain, bleeding, and
presence of foreign bodies.
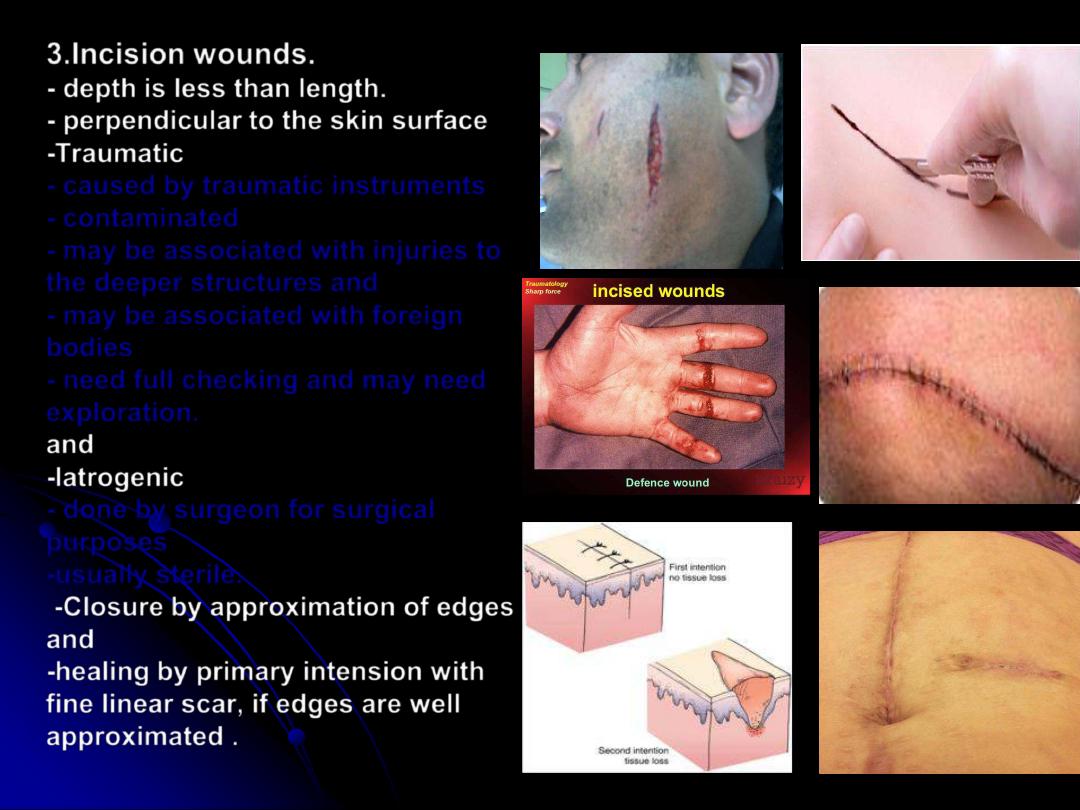
3.Incision wounds.
-
depth
is less than length.
- perpendicular
to the skin surface
-
Traumatic
- caused by traumatic instruments
- contaminated
- may be associated with injuries to
the deeper structures and
- may be associated with foreign
bodies
- need full checking and may need
exploration.
and
-
Iatrogenic
- done by surgeon for surgical
purposes
-usually sterile.
-Closure
by approximation of edges
and
-healing
by primary intension with
fine linear scar, if edges are well
approximated .

4.Penetrating wounds
- depth
is more than surface length
- including
different types;
puncture, stab and perforating
wounds.
Associated
with injuries to
deeper structures
Need full checking and mostly
need exploration
*bullet injuries
cause
perforating wounds with
unpredictable pathways and
shock wave, need exploration
like laparotomy.
5.Laceration wounds
usually
multiple and parallel, and oblique in
direction.
To get linear scar need to be
converted to incision wound

6.Crush wounds;
result from trauma by
heavy object with high velocity and
associated injury to deeper tissues.
They need good checking, investigations
and exploration
7. Avulsion wounds.
Are associated with
separation or loss of tissue at the level of an
avascular plain loose areolar tissue
8.Bites
including
insect bites,
animal
and human bites
.
Human bite is more contaminating
than animal bite.

Chronic wounds
like;
-
leg and foot ulcers ( varicose , infective, neurotrophic,
traumatic, diabetic, ischemic, etc….)
-pressure ulcer
-malignant ulcers
-
chronic discharging sinuses and fistulas, etc…
Clinical features:
1.
Pain
.
2.
Bleeding
.
3.
Deformities
.
4.
Symptoms and signs
of
inflammations
like;
Swelling
(edema), redness, hotness,
tenderness.
5
.Manifestations of deeper tissue
injuries.
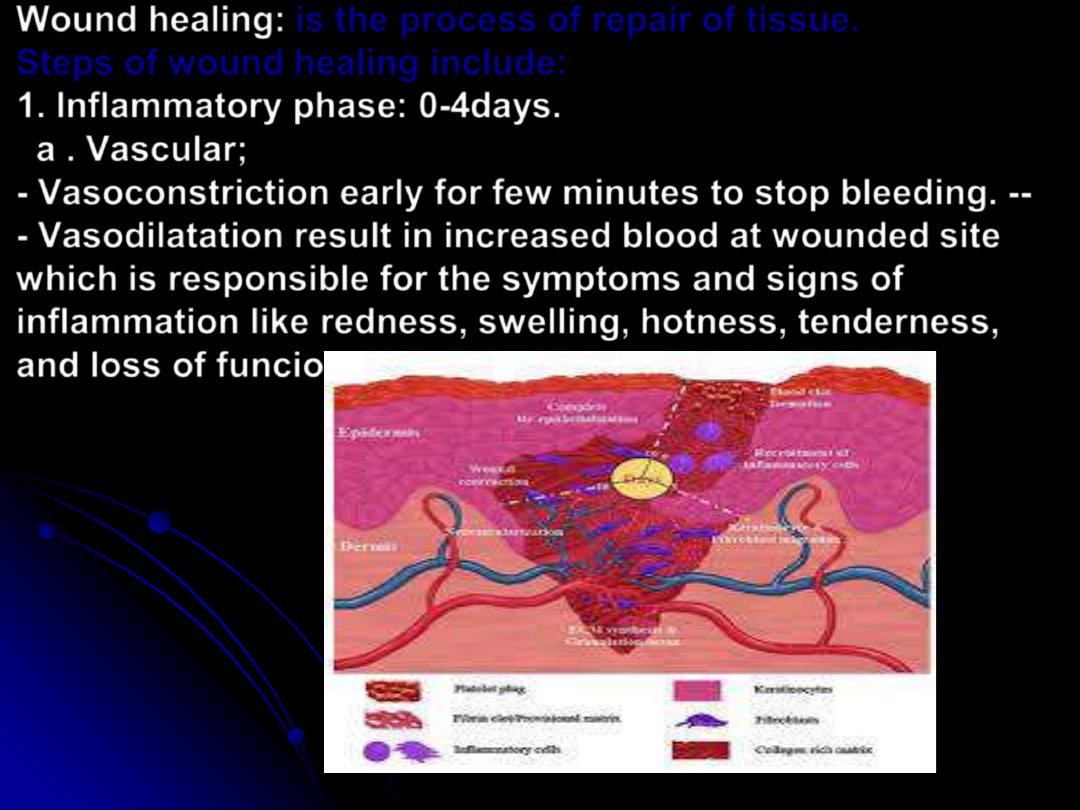
Wound healing
:
is the process of repair of tissue.
Steps of wound healing include:
1.
Inflammatory phase
: 0-4days.
a .
Vascular;
- Vasoconstriction
early for few minutes to stop bleeding. --
- Vasodilatation
result in increased blood at wounded site
which is responsible for the symptoms and signs of
inflammation like redness, swelling, hotness, tenderness,
and loss of funcion.
B .
Cellular
;
platelets
are the first reaching to the
wounded area, play a rule in hemostasis and
release factor that promote wound healing
process
Neutrophiles
Reach the wounded area within
the first 48 hours and as a phagocytic cells
only.
Macrophages
are modified monocytes and
are the dominant cells at the wound site at the
end of inflammatory phase. Their functions are
phagocytosis, releases of factors that control
wound healing, and antigen processing.
Lymphocyte
are chronic inflammatory cells
and reached late in this phase.
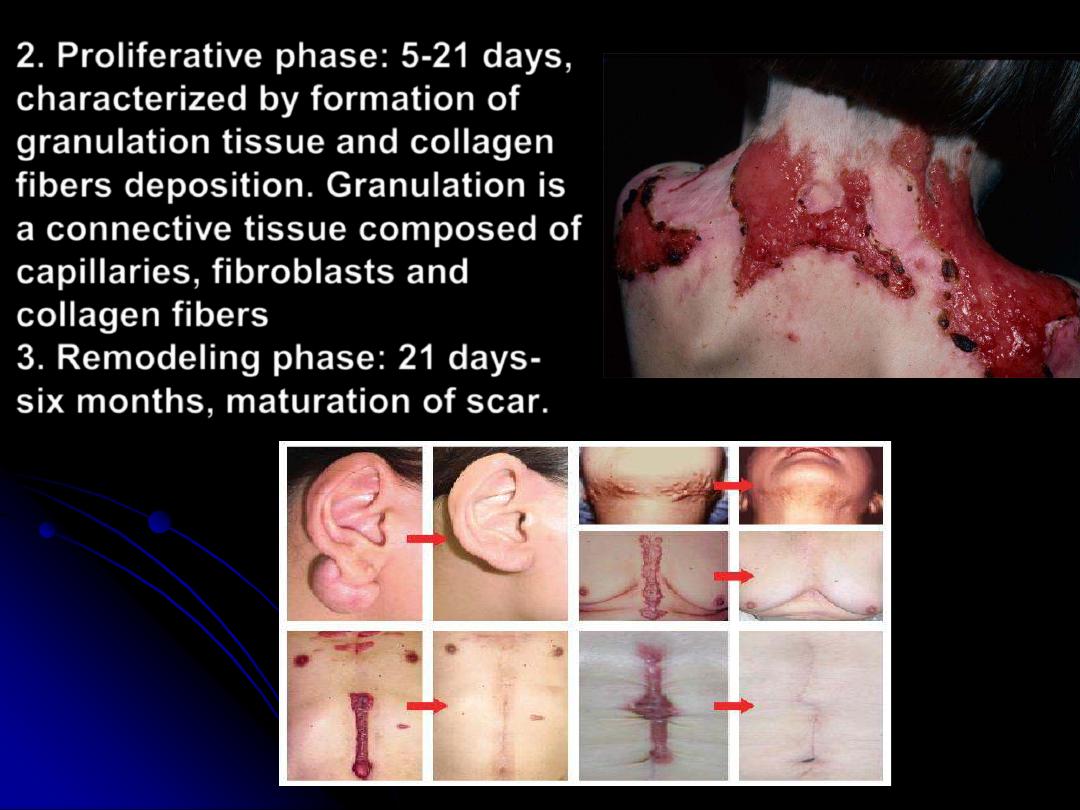
2.
Proliferative phase:
5-21 days,
characterized by formation of
granulation tissue
and collagen
fibers deposition. Granulation is
a connective tissue composed of
capillaries, fibroblasts and
collagen fibers
3.
Remodeling phase:
21 days-
six months, maturation of scar.
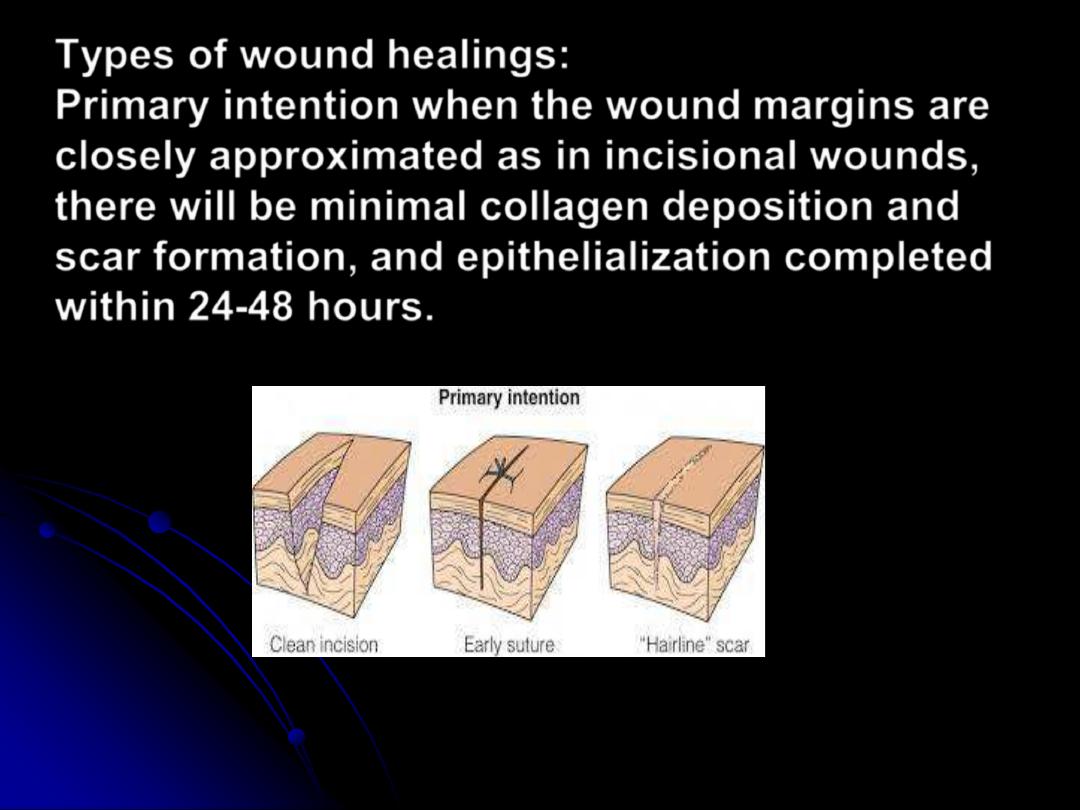
Types of wound healings:
Primary intention
when the wound margins are
closely approximated as in incisional wounds,
there will be minimal collagen deposition and
scar formation, and epithelialization completed
within 24-48 hours.
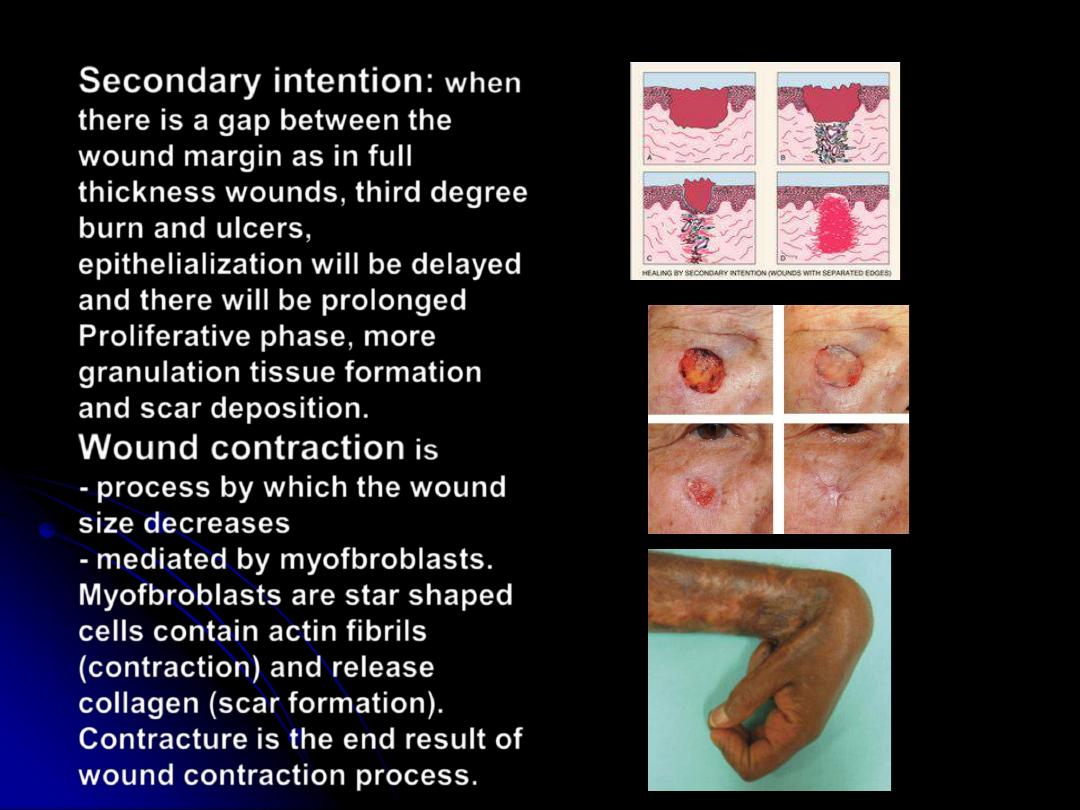
Secondary intention:
when
there is a gap between the
wound margin as in
full
thickness wounds, third degree
burn and ulcers,
epithelialization will be delayed
and there will be prolonged
Proliferative phase, more
granulation tissue formation
and scar deposition.
Wound contraction
is
- process by which the wound
size decreases
- mediated by myofbroblasts.
Myofbroblasts
are star shaped
cells contain actin fibrils
(contraction) and release
collagen (scar formation).
Contracture
is the end result of
wound contraction process.

Healing of partial thickness wound
;
as in
-abrasive wounds
-second degree burn
-donor sites of split thickness skin graft
characterized by less scar formation and
epithelialization from wound margins and skin
appendages in the base of the wound.
Factors affecting wound healing:
A-Systemic factors;
1.
Nutrition
as
proteins, carbohydrates
(calories), fat, Vitamins, minerals, and trace
elements.
2.
Age
.
3.
Systemic diseases
;
Anemia, Diabetes
mellitus, systemic acute (septicemia) and
chronic (tuberculosis) infections, neoplastic
diseases, uremia, jaundice,etc….
4.
Associated traumas
.
5.
Drugs;
like steroids and cytotoxics.
B-Local factors
:
1. Site.
2. Size.
3. Shape.
4. Local circulation.
5. Edema.
6. Infection.
7. Foreign bodies.
8. Trauma.
9. Irradiation. Etc…
Management:
History
: Cause, Mechanism , duration,
symptoms, etc
…
Clinical examination
: -Local site,
shape, size, type, injury to the deeper
stractures,etc
…
.
-Systemic as manifestation of shock,
associated trauma,etc
…
.
Investigations
hematological as blood
grouping , radiological as X ray, CT scan,
MRI and Ultrasonagraphy
Treatment:
1. Hemostasis.
2. Cleaning as wash.
3. Debridment (wound excision).
4. Wound closure (with consideration of repair
of deeper tissue injuries).
5.Dressing:
consist of Greased gauze, dry
gauze, cotton, bandages and adhesive tapes
according to the site, shape and type of the
wounds. The aims and functions of dressing
include:
a. Protection against traumas.
b. Immobilization.
c. Pressure for hemostasis.
d. Absorption.
e. Appearance.

Scar :
is the end result of wound healing
process
Is a connective tissue composed
mainly of collagen fibers and
fibroblasts
Types
- Immature scar:
red, elevated irregular
surface, itchy, tender and
sometimes painful. It starts to
appear after 3 weeks and may
continue for 6months-2 years
duration.
-Mature scar:
white, pale, or skin
colored, flat or depressed, not
itchy, not tender, not painful. It
indicates full scar maturation.
-Hypertrophic scar:
elevated, red or skin
colored, without itching or
tenderness. NOT extends beyond
wound margins
-Keloid:
overgrowth of scar that extends
beyond wound margins.
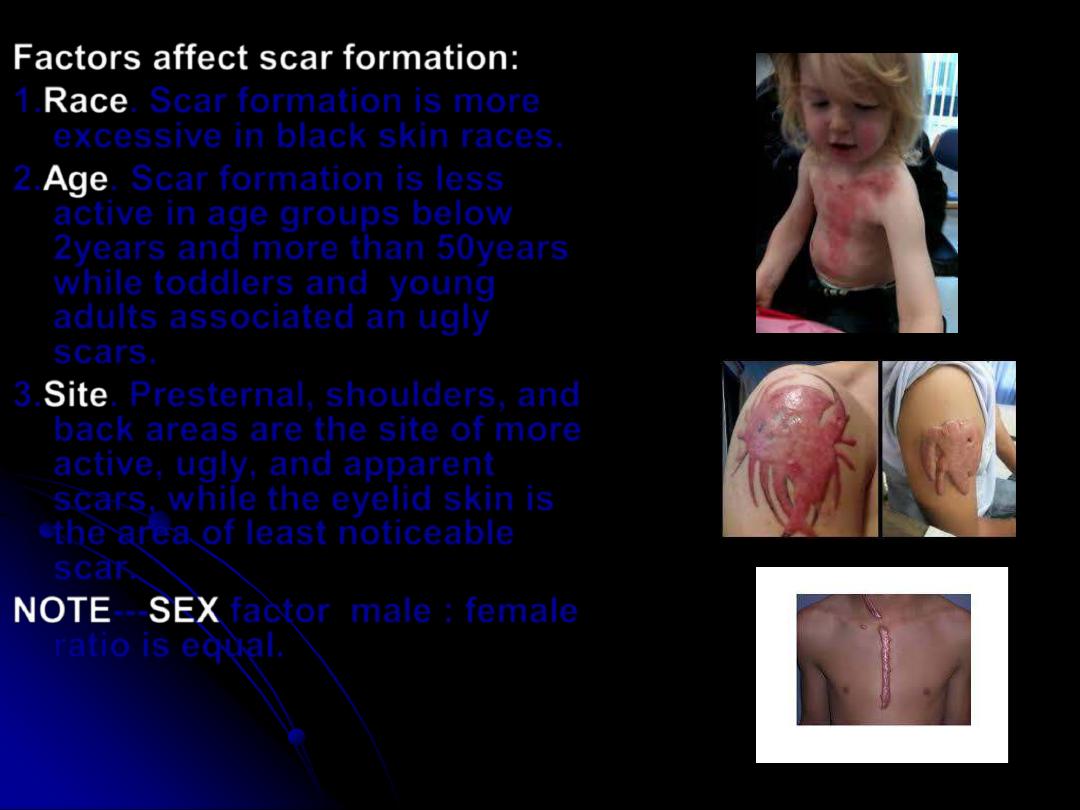
Factors affect scar formation:
1.
Race
. Scar formation is more
excessive in black skin races.
2.
Age
. Scar formation is less
active in age groups below
2years and more than 50years
while toddlers and young
adults associated an ugly
scars.
3.
Site
. Presternal, shoulders, and
back areas are the site of more
active, ugly, and apparent
scars, while the eyelid skin is
the area of least noticeable
scar.
NOTE
---
SEX
factor male : female
ratio is equal.
Treatments:
1.
Reasurance
: of patient, parents that scar will
improve with time waiting for maturation.
2.
Pressure
: by elastic bandaging, tube grip,
pressure garments that will act to redirect
collagen fibers deposition in proper (parallel
or organised)directions.
3.Soothing agents and antihistamines
. To
relieve itching .
4.Silicon gel and sheets
.
5.
Steroids
: as local and intralesional injections.
6.
Laser
.
7.
Radiations
.
8.
Surgery
. As redirection, revision, excision
and grafting, and release of contractures.
