
RESPIRATORY PROBLEMS
1. Carbon monoxide(CO) poisoning
: CO
gas is one of the product of combustion, it has
an ability to bind to hemoglobin instead of
Oxygen. Hemoglobin affinity for CO is 210
than that for Oxygen. The clinical
manifestation include headache, disturb
conscious level may presented as confusion or
even comma with pink color spot on skin
especially on neck & chest. Treatment is
rapid removal from site of accident, high
tension Oxygen & hyperparic Oxygen.
2. Circumferential chest burn
: If the skin
of the whole chest circumference involved by
full thickness burn that result in loss of its
elasticity & reduction in chest expansion
during inspiration &tidal volume. The
treatment is Escheratomy ( Incision in the
Escher) along the anterior axillary lines
&subcostal margin.
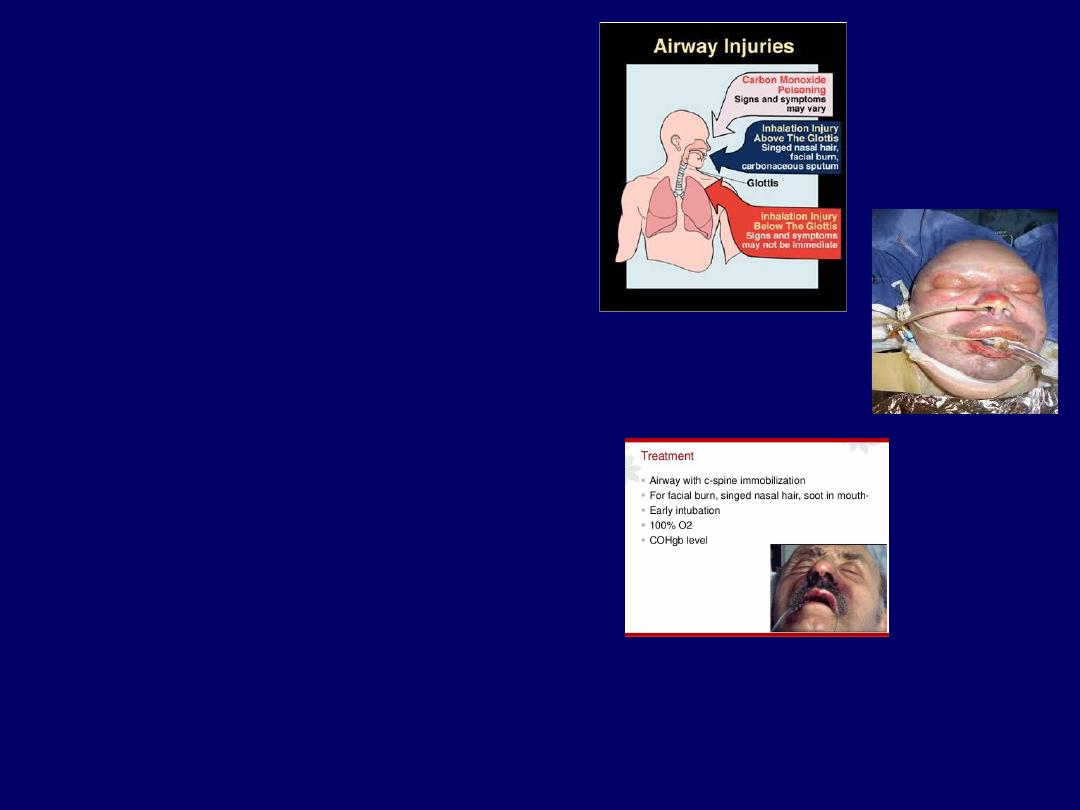
3. Burn face & neck.
4. Burn of upper respiratory tract.
The3rd & 4
th
problems presented as upper
airway obstruction by edema & secretion. The
treatment is proper positioning of the patient as
elevation of the head &chest, Oxygen, Steroids,
and maintaining patent airway(this may need
Intubation or even tracheostomy).
•5.Inhalation injury(Adult Respiratory Distress
Syndrome ARDS):
Inhalation of toxic gases &
smokes may happen during burn accident
especially when it occurs in a narrow closed
poorly ventilated spaces. The product of
combustion may include SO2, Nitrous oxide,
Cyanides, and other derivatives of hydrocarbon
materials. These toxic substances will cause
damage of small bronchioles &alveoli that result
in damage of alveolar-capillary membrane and
disturbance in gas exchange and leak of fluid
into the alveoli which result in pulmonary
edema.
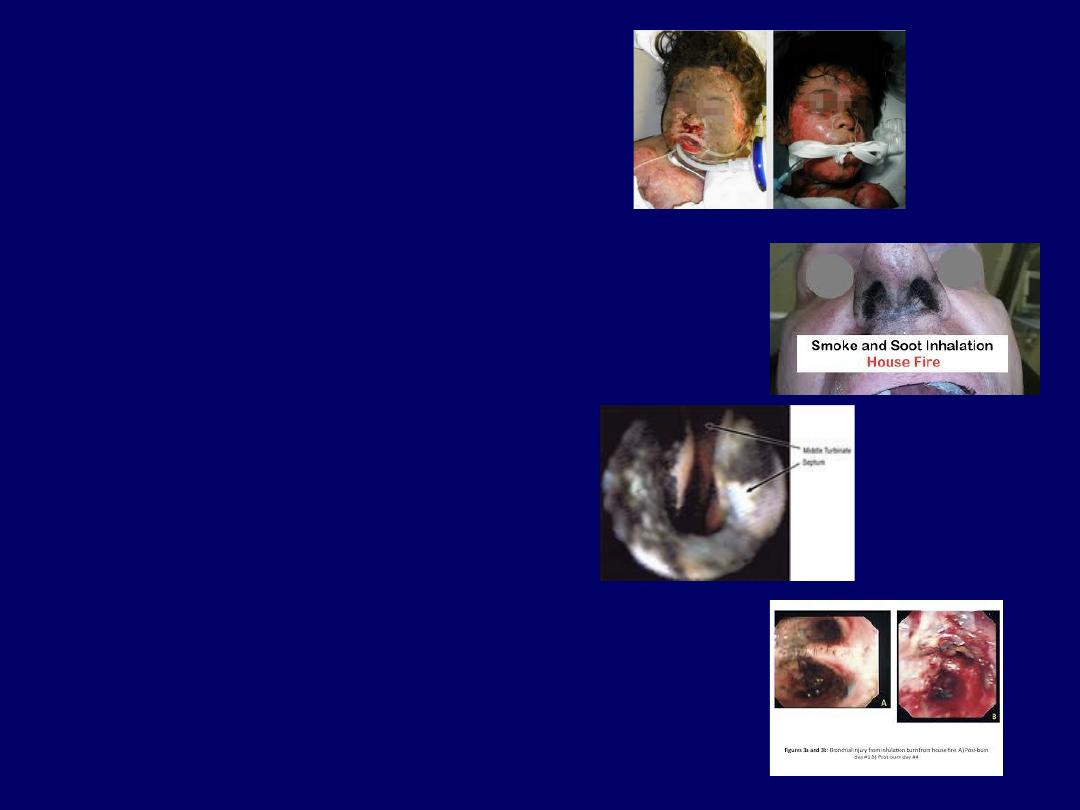
The diagnosis is usually by suspicion as
the history of the accident in a narrow
closed poorly ventilated space, dyspnoea,
productive with soot; on examination there
is burn of face,neck&upper airway, soot on
the nasal opening, burn nasal hair, soot is
seen in the upper airways by direct
laryngoscopy. Clinically, it is usually
manifested during the 3
rd
-5
th
post burn day,
the patient get dyspnoea, tachypnoea,
hypoxia, hypercapnoea, rhonchi, wheezes,
crepitation, disturb conscious level, and
respiratory failure. On Chest X-ray there is
signs of pulmonary edema. The mortality is
very high & it is 50% in the best centers
treatment includes; elevation of the head
&chest, high tension humidified Oxygen,
bronchodilators, systemic antibiotics,
steroids, and even Intubation.
6. Pneumonia.
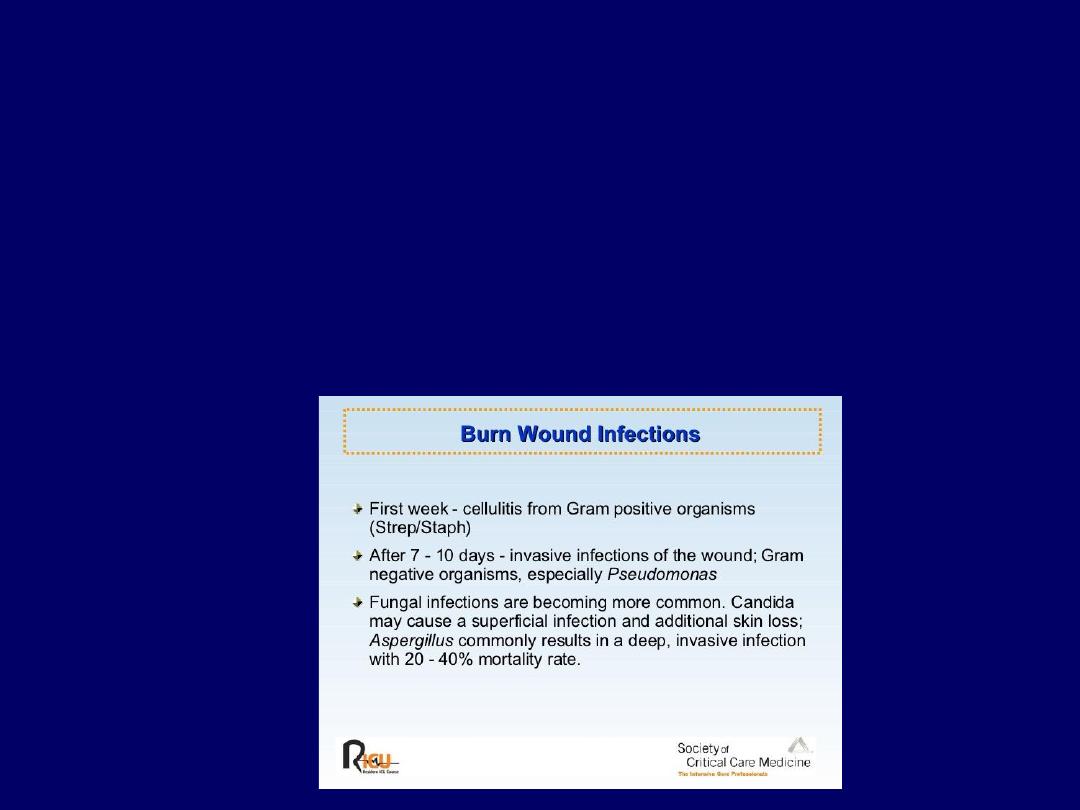
BURN WOUND INFECTIONS
Usually occur after the 5
th
post burn day.
The burn patient is more liable for infection because of break-down of the
mechanical barrier(skin), Malnutrition, hypoproteinemia, anemia, long period of
hospitalization, cross infection.
Source of infection either endogenous from inside the body, usually Gram
positive like Streptococci and Staphylococci Or exogenous from external
environment( medical &nursing staff or from other patient), usually Gram
negative like Pseudomonas & Proteus.

Diagnosis:1.Local symptoms &
signs as pain, redness & swelling at
wound margin, Change in color of
Escher, bad odor, pus discharge,
earlier Escher separation, dusky
color granulation tissue, septic spot
on non burn skin.
2. systemic;
fever(Temperature>39C),
tachycardia, poor appetite, nausea,
vomiting, ileus, diarrhea, disturb
level of consciousness.
3. Laboratory Leucocytosis, high
ESR, positive bacteriological test
as wound swab & wound biopsy.
Prevention : by correction of nutritional state, anemia, and
hydration state; systemic prophylactic antibiotics in the first 5 days;
proper wound care & local antibiotic; isolation of patient.
Treatment: Systemic antibiotic according to the culture
&sensitivity result, supportive measures as correction of anemia&
nutritional state, proper wound care and local antibiotic.
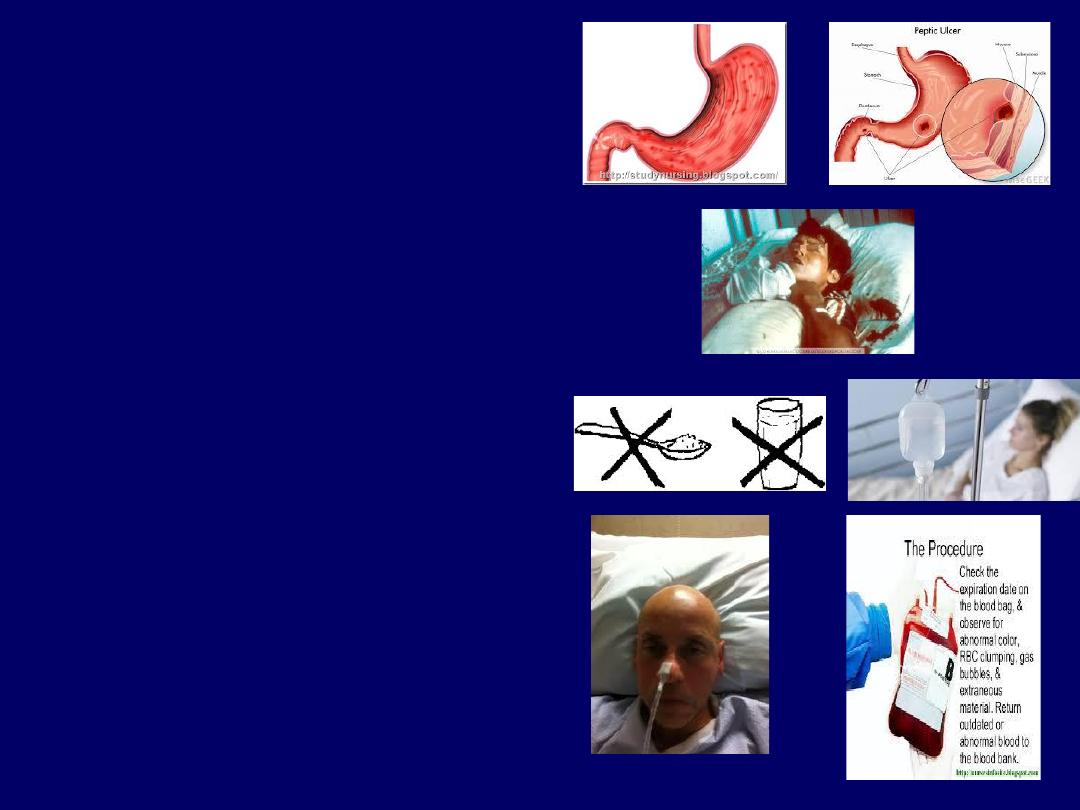
Gastrointestinal
problems
The shock (hypovelemia) state
&stress of burn result in poor
circulation & increase in vagal to
the Gastrointestinal tract, as a
result there will be poor absorption
and decreases motility. Clinical
manifestations are thirst, nausea,
vomiting, acidity, Hematamesis,
malena, ileus, & constipation or
diarrhea.
The prevention of GIT problems
include; adequate fluid
replacement, avoiding non-steroid
anti-inflammatory analgesia, use of
antacid & H2- blockers like
Cimitidine.
Treatment include the same lines
in the prevention in addition to stop
of oral feeding(temporarily) &
blood transfusion in case of GIT
bleeding.
Nutrition.
The burn patient get
increment in his Basal metabolic rate by
about 135%(from 2000 kcal reach up to
4500 Kcal) & in protein
requirement(from 42gm/day up to180
gm/day), so there is a need for proper
feeding. This include: Nothing by mouth
& i.v. fluid till shock state is relieved,
start small amounts of water then
increase it gradually, fluid diet, then
feeding with high calorie & protein diet
as frequent small meals.
Anemia
; due to loss of RBCs as a result
of burn accident( the PCV decreases by
about 40%), as result of hypermetabolic
state blood loss during wound care
&surgical sessions, so there is a need
frequent checking of PCV & hemoglobin
level, and Frequent blood transfusions
especially in extensive burns.

Wound care
By; daily wash with warm, isotonic,
sterile, non-toxic solution like water
or normal saline & bland soap, to
remove separated dead tissue &tissue
debris, clean the wound, & get rid
of large number of micro-organisms,
use of local antibacterial agent that
could penetrate the Escher like 1%
Silver salfadiazine cream, 1%
Mefenide cream, and 0.5% Silver
nitrate solution.
Blister of 2
nd
degree thermal burn
should be left intact because it
contain sterile fluid. Indications for
blister removal include; already
ruptured blisters, blisters contain pus
or blood or turbid color fluid, and
large blisters that interfere with
functions.

Escheratomy
: incision of Escher, is
indicated for circumferential burn of
limb with compartment syndrome and
circumferential burn of chest with
respiratory embracement.
Open method means leave the burn
wound open without dressing under
humid environment (cage). The
advantages are less accumulation of
discharge, no pain on removal of
dressing as in closed method, and not
coasty, but it may be associated with
dryness of wound & pain.
Closed method mean dressing of
burn wound after cleaning. The
advantages are; the wound is not liable
for dryness, less pain, the wound is
always under humid environment, but
it is painful on removal, may result
accumulation of pus, and it is coasty.

Escherectomy (Excision of Escher) & wound
excision under anesthesia may be needed for
cleaning & preparation for skin grafting of deep(
full thickness) burn wounds.
Early excision & Immediate grafting of the burn
wound is the method of treatment used for deep
(2
nd
)dermal & 3
rd
degree burn.

Rehabilitation
: include proper
positioning of the burn patient as
elevation of the head of the bed to
relieve respiratory embracement,
elevation of burn limbs to reduce
edema, proper position of flexor
surfaces to prevent contracture,
continuous change of position of the
patient to prevent pressure ulcers, &
encourage the patient to move all
joints to prevent stiffness.
Psychology: The patient may have
psychological problems, psychiatric
diseases or social problems that led
him to suicidal attempts Or may get
psychiatric problems as a result of
burn like depression, nightmares. So
there is a need for psychiatric
treatment which best provided by
psychiatrist.

Cold injuries
: exposure of the
tissues to extremely low
temperature result in partial or
full thickness damage. This
exposure may be industrial as
in accidental spills of liquid
nitrogen or similar substances
or environmental as in injuries
of very cold weather. Frost bite
is due prolonged exposure to
cold and there is often an
element of ischaemic
damage(due to associated
vasoconstriction). Treatment is
gradual worming of the affected
area for the wound is same for
thermal burn.

Chemical injuries
: Numerous
chemicals(like strong acids & alkali)
in industrial and domestic situations
can cause burns. Tissue damage
depends on the strength and
quantity of the agent and duration of
contact. Pathologically there is local
coagulation of proteins and necrosis
of tissues with possible systemic
effects( like toxic effect of phenol on
liver, kidney, and body tissues).The
treatment includes; dilution with
running water initially then continue
with same treatment as that for
thermal burns(here the blisters
should excised as it may contain
chemicals).

Electric burns
:
The passage
of current through the tissues
causes heating that results in
cellular damage. Heating depends
on resistance of tissue, duration of
contact, square of the current. The
bone has the highest resistance
while the least resistant tissues are
nerves and blood vessels. Bone can
therefore become very hot and
cause secondary damage to tissues
near to the bone like muscles. The
muscle damage result in
compartment syndrome locally,
and delivery of myoglobin to the
circulation result in acute tubular
necrosis (acute renal failure) in
kidneys.
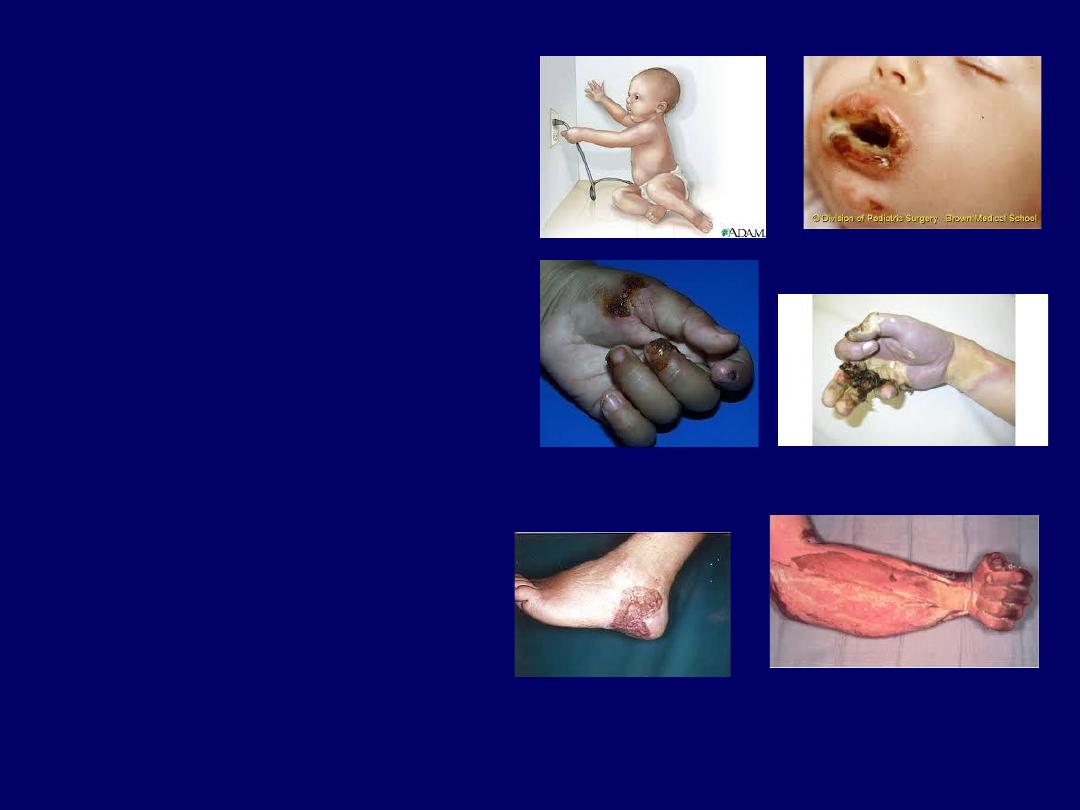
There are two types of electric
injuries
;
1 1. Low (tension)voltage(<1000
volts)injuries as from domestic
supply 220volts. This is
associated with local tissue
damage, the common sites are
fingers and lips especially in
children. It may cause cardiac
arrest.
2.
High(tension)voltage(>1000volt
s)injuries cause damage by
•
i - flash from an arc may cause
a cutaneous burn and ignite
clothing.
ii- high-voltage current
transmission will result in
cutaneous entrance and exit
wounds and deep damage. It
may result in coma or
convulsion attack, respiratory
muscles paralysis, or cardiac
arrest according to the axis of
the current between entrance
and exit.

Treatment
;
1. Cardiopulmonary
resuscitation, ECG monitoring
and intensive care for 1
st
24hours.
2.Intravenous fluid; the
amount of fluid given should
ensure urine output of 100ml/hr
in adult &2ml/kg/hr in children to
prevent renal failure.
3. Other lines of treatment as
systemic antibiotic, analgesia,
tetanus prophylaxis, ----etc.
L 4. Local wound care as
fasciotomy in case of
compartment syndrome, cleaning
, local antibiotics, wound excision,
amputation, reconstructions.
