
Occupational Skin Diseases
By
Dr. Ashraf Hussain
Msc, PhD. Com. Med.
بسم ﷲ الرحمن الرحيم
الذي خلق الموت والحياة ليبلوكم ايكم احسن عمﻼ
وهو العزيز الغفور
صدق ﷲ العلي العظيم
Introduction
Occupational skin diseases (also known as occupational
dermatoses) are skin diseases caused by exposures to
hazards at work
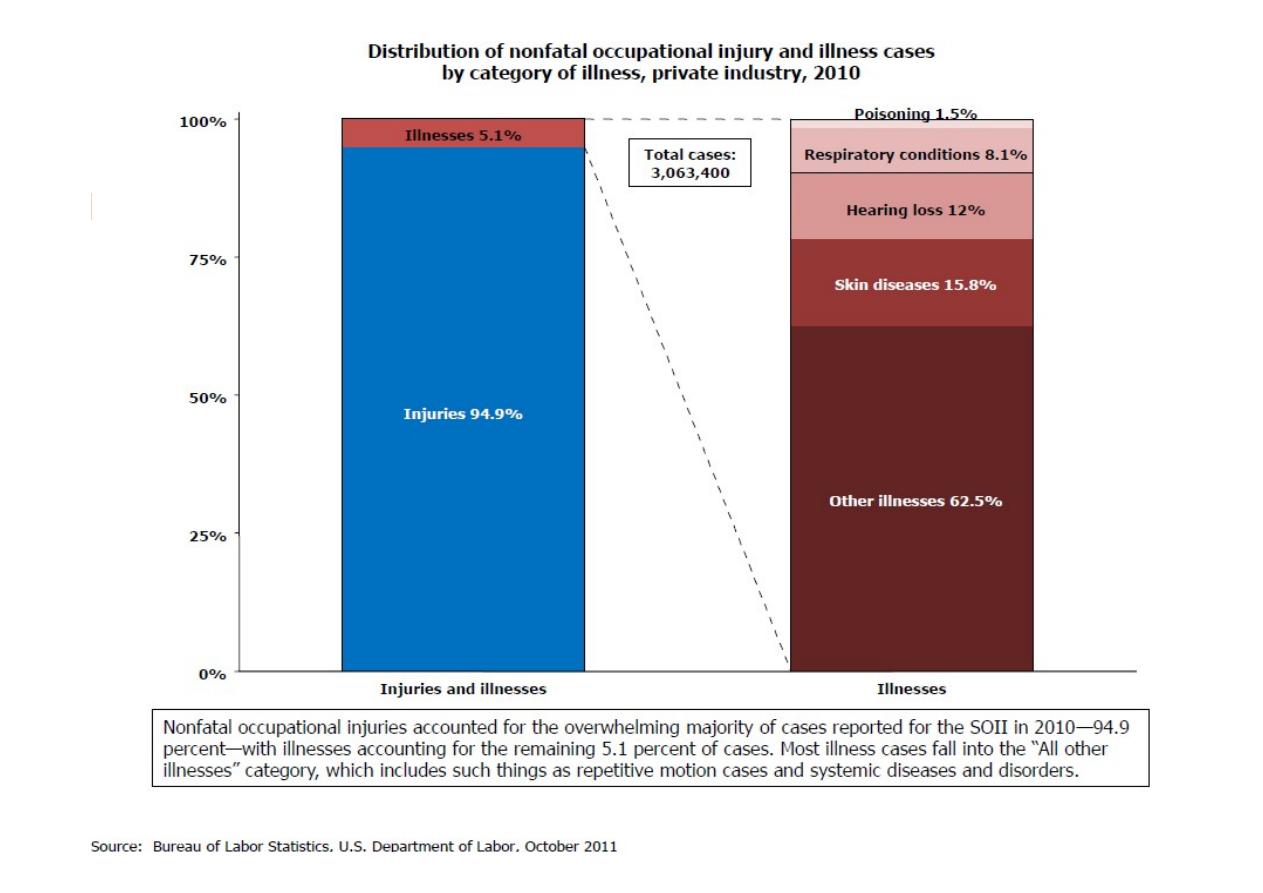
It is estimated that they comprise 20-30% of occupational
diseases capture one of the three most common
occupational diseases

Occupational skin Hazards
Chemical hazards are irritants, sensitising,
photosensitising and acnegenic agents.
Biological hazards range from bacteria, fungi, viri,
to skin parasites.
Physical hazards include rubbing, mechanical
pressure, radiations and temperature.

Causes of OSD include
are the main cause of occupational skin diseases and
disorders.
These agents are divided into two types: primary irritants
and sensitizers.
Primary or direct irritants act directly on the skin though
chemical reactions.
Sensitizers may not cause immediate skin reactions, but
repeated exposure can result in allergic reactions.
Chemical agents
A worker’s skin may be exposed to hazardous
chemicals through:
direct contact with contaminated surfaces.
deposition of aerosols.
immersion, or
splashes.
Contact Dermatitis
Dermatitis is an inflammation of the skin causing itching, pain,
redness, swelling and small blisters.
Contact dermatitis is an eczematous eruption caused by
external agents, which can be broadly divided into:
Irritant substances that have a direct toxic effect on the skin
(irritant contact dermatitis, ICD)
Allergic chemicals where immune delayed hypersensitivity
reactions occur (allergic contact dermatitis, ACD).
The symptoms and presentation of ICD and
ACD are so similar, it is extremely difficult to
distinguish between them without history and
clinical testing (e.g. patch testing).
Irritant contact dermatitis (ICD)
The most common occupational skin disease
Covering around 50-80% of cases and around five
times more frequent than allergic contact dermatitis
is a non-immunologic reaction that manifests as an
inflammation of the skin caused by direct damage to
the skin.
Common chemical agents include acids, alkalies,
organic solvents and detergents.
chronic cumulative exposures to mild irritants (e.g.,
water, detergents, weak cleaning agents)
The reaction is typically localized to the site of
contact.
The effect on the skin depends not only on the
chemical properties and the intensity of contact, but
the concentration of the chemical as well.
Wet work is the leading cause of ICD
Symptoms range from dryness, burning red rashes
(erythema) and swelling (oedema) to the
development of bullas (blistering), necrosis and
peeling (desquamation) in more severe cases.
Chronic, repeated exposures trigger the
development of fully-fledged eczema: itching,
cracking, crusting and flaking, oozing or even
bleeding that may be present alongside the
signs mentioned above
Patch tests are negative in ICD that has no
allergic component
Phototoxic Dermatitis
Skin inflammation due to the combined exposure of a
chemical substance and light can lead to developing vesicles
and bullas (blistering) on the inflamed skin, which is followed
by a characteristic skin tan (hyperpigmentation).
The most frequent chemicals involved in phototoxic
dermatitis are:
1.
Psoralens in plants ,which make gardeners, florist and
manufacturer of cosmetic particularly vulnerable.
2.
Tar derivatives, which make road construction and building
insulation workers particularly vulnerable;
3.
Pharmaceuticals, to which exposure may be present in
certain pharmaceutical plants
This form of skin inflammation is acquired after contact
with a sensitising chemical substance
The sensitisation process can take weeks, months or
even years and there is no allergic reaction to be seen
on the skin during that period.
The hypersensitivity to the given chemical will
practically last for life, although avoiding further
contact with the chemical agent may lower the level of
reaction.
This allergy is a late onset cell-mediated immune
response to the chemical substance, which explains why
its symptoms have a latency period of days, which is
longer than that of contact urticaria.
Allergic contact dermatitis (ACD)
Clinical signs of ACD are very similar to that of ICD,
although itching is predominant over burning, furthermore
skin lesions are not limited to the contact site but might
develop at unexposed parts too.
The most important occupational allergens are
1.
metals - chromium, nickel, cobalt, mercury
2.
p-phenylenediamine (PPD)
3.
rubber additives
4.
natural resins and artificial resins
5.
preservatives
6.
animal feeds
7.
plants
8.
pharmaceuticals
Photoallergic Contact Dermatitis
A special form of ACD.
Here the chemical compound transforms into a
complete sensitising agent only when exposed to
ultraviolet light (mainly from the A-band spectrum).
1.
Fragrances (e.g., in cleaning, chemical industry),
2.
optical brighteners (e.g., in laundries, washing
powder manufacturing)
3.
Dyes (e.g., in textile industry)
4.
Pharmaceuticals are the most common chemicals
involved in photoallergic contact dermatitis
The severity of contact dermatitis is highly variable
and depends on many factors including:
Characteristics of the hazardous agent (irritant
and/or allergen)
Concentration of the hazardous agent (irritant
and/or allergen)
Duration and frequency of exposure to the
hazardous agent (irritant and/or allergen)
Environmental factors ( e.g., temperature, humidity)
Condition of the skin (e.g., healthy vs. damaged skin,
dry vs. wet)
Contact urticaria (CU)
The symptoms of CU are itching and hives (urticaria).
In immunologic CU the reaction is an immunglobulin E
mediated early immunoresponse against the sensitising
chemical substance.
Thus in contact urticaria the chemical compound causes
hives at the place of contact usually within an hour.
This can be accompanied by (allergic) rhinitis,
conjunctivitis, asthma and rarely anaphylaxis.
There is also a non-allergic route (non-immunologic CU),
where the chemical directly triggers histamine release in
the skin causing urticaria.
A well-known form of allergic CU is latex-allergy
among healthcare, catering and cleaning workers
who are wearing latex gloves.
Direct CU can be caused by stinging-nettle,
preservatives and additives.
Tackling CU is more difficult, because it requires a
total elimination of the allergen due to the risk of
the more serious complications; thus change of job is
more frequently recommended to avoid/ prevent
exposure
2. Occupational Skin Cancers
The second m/c form of occupational skin diseases
About 17% of all cases of occupational skin diseases
Risky exposures include:
Ultraviolet light
Ionizing radiation
Poly cyclic aromatic hydrocarbones
Arsenic
Pitch, tar, soot, anthracene and coal tar distillation
products.

3. Other occupational skin ailments:
Occupational acne
These are comedos (pinheads), papules and
pustules caused mostly by industrial oils and
greases .
Caused by exposure to industrial chemicals.
Unlike common acne, these eruptions manifest at the
site of skin contact.
Suspected in : a. Unusual sites of involvement e.g.
forearms. b. Unusual age e.g. middle age males.

Car mechanics, maintenance workers are most at
risk.
Tar derivatives and certain pharmaceuticals may
cause acne
(Corticosteroids, lithium, anticonvulsants,
barbiturates, androgenic
steroids and medications
that contain
bromides or iodides)
Hyper pigmentation
Darkening of the skin from chronic physical
irritation (e.g., itching)
Some chemicals may stimulate the
production of melanin (thus darkening)
Tars, arsenic compounds, plant sensitizers.
Skin diseases of physical origin
Physical exposures range from direct stimuli and
thermal conditions to radiation.
Mechanical trauma
Recurrent rubbing or increased pressure can thicken
the inflamed skin with “crazy-paving pattern”
(lichenification) and callosity.
Called occupational stigmas are frequent at body
parts exposed: shoulders of sack carriers, fingertips
of guitarist.

Temperature
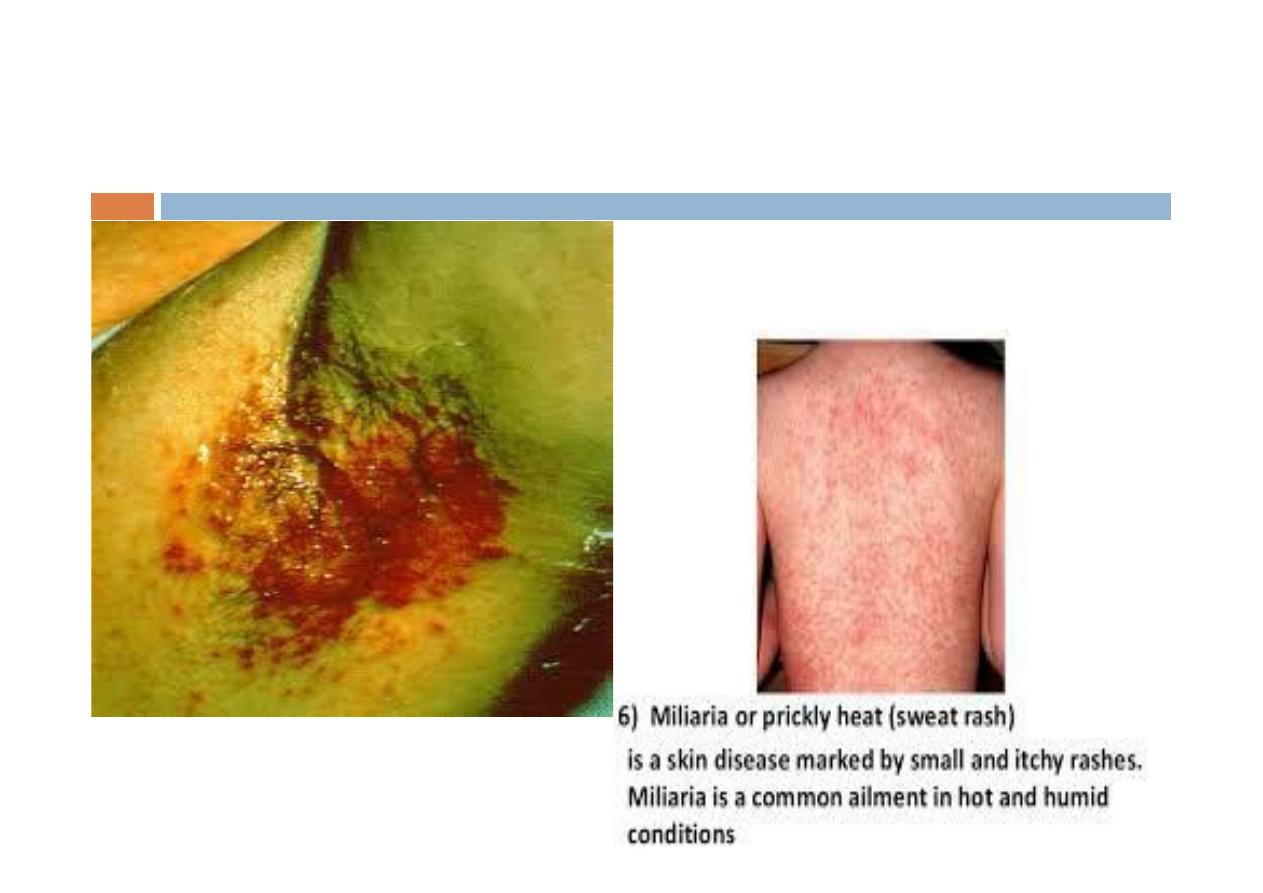
Heat
Sweat stagnation can cause miliaria .
Overlapping skin surfaces can become sodden, ending up in
intertrigo.
Cold temperature
Reynaud-like symptoms (blanching attacks of fingers)
frostbites.
Ionising Radiation
Acute radiodermatitis
After a single high dose, local redness (erythema),
swelling (oedema) and loss of skin colour develops.
After days, the disease may progress with a painful
inflammation with vesicles and bullas (blistering) and
necrosis that heals with scar, atrophy and loss of hair.
Chronic radiodermatitis
Repeated exposure to smaller doses causes atrophic
indurated plaques, spider veins (telangiectasia) or even
thickening (hyperkeratosis), a syndrome called termed
poikiloderma.
Skin cancer can arise after months or years on the
grounds of poikiloderma
Non-ionising radiation
Concerning occupational skin diseases, workplace
exposure to ultraviolet radiation is among the most
important physical risk factors.
Excessive exposure to ultraviolet radiation is
harmful: it damages the skin and the eyes, causes
mutation of the DNA and suppresses normal
immunologic responses
Infectious skin disease
Bacterial infections
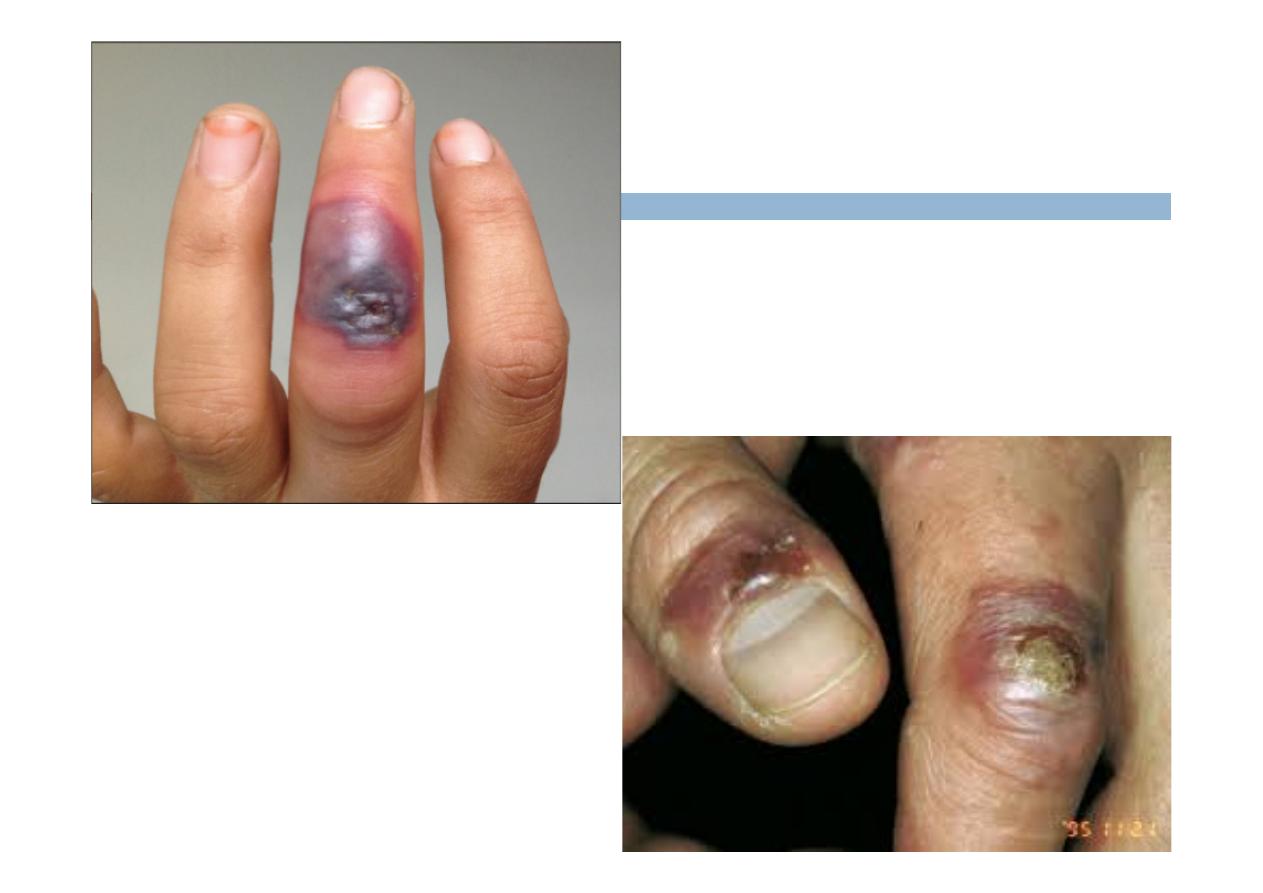
Occupational pyodermas (folliculitis, furuncle, carbuncle,
impetigo, ecthyma, paronychia, etc.) can be caused by
the Streptococcus and Staphylococcus bacteria which
generate pus.
These infections are common among those working in
dirty environments (e.g., car mechanics, sewerage
cleaners) where microtrauma (bruises, cuts) of the skin
are common (e.g., butchers, slaughterhouse workers,
machining of metals), or who may be in contact with
infected persons (e.g., nurses, hairdressers, manicurists)
Others, Cutaneous TB, Anthrax.
Fungal infections (mycoses)
Yeast infections
Mainly caused by Candida albicans, occurs usually on the
hands: onychomycosis (nail), paronychia (around the nail
bed), interdigital mycosis (between the fingers or toes).
Workers in canneries and confectioneries, and health care
workers are at risk.
Wearing rubber gloves and boots (wet work) and
handling of sweets can be contributing factors to the
development of these infections
Dermatophyte infections (ringworm)
Viral skin diseases
Milker's nodules are caused by the Paravaccinia
virus. The source is the udder of the cow, sheep or
goats. Milkers and other animal handlers may
develop the skin lesion which heals spontaneously
without scarring within weeks
Orf is caused by a Parapox virus, which is common
in sheep and goats. The tender skin lesion may be
accompanied by regional inflammation of the
lymph vessels and nodes. The disease may be
contracted by shepherds, goatherds, veterinarians.
Parasitic skin lesions
Arthropod bites from animal parasites or granary
mites are common in agricultural workers
Bee and wasp stings are important, because their
venom may cause serious and even life-threatening
allergic complications
Scabies is caused by Sarcoptes scabiei.
Prevention of Occupational Skin Damage
Elimination
substitution
Engineering Controls
process re-design to eliminate or reduce contact, automation,
closed systems
Make plans for spills and leaks
Administrative Controls
Training, personal hygiene (remember lead and ingestion), barrier
creams, rotation
Requires all workplaces contain a basin for washing, hot and cold
running water, soap, clean towels or hot air dryers
PPE: gloves, aprons, boots, full body suits, face shields, goggles
Provide a barrier; meet specifications for degradation and
permeation

