Puerperium
It is a term refers to the six weeks period after completion
of the third stage of labour.
Physiological Changes:
1- Uterine involution
It is the process by which the postpartum uterus weighing
about 1kg returns to its pre-pregnancy state of less than 100gm.
Clinically the uterine fundus should lies 4cm below the
umbilicus or 12cm above the symphyses pubis immediately
after labour, and after (2) weeks the uterus should be no longer
palpable above the symphyses. These changes occur because a
process of autolysis where the muscle cells diminish in size but
not in number, and it is accelerated by oxytocin,
Causes of delayed involution:-
- Full bladder
- Loaded rectum
- Uterine infection
- Retained products of conception.
- Fibroids
- Broods ligament hematoma.
2- Genital tract changes:-
The lower segment of the cervix and uterus appears flappy
and sometimes have small lacerations. In the first few days the
cervix can admit (2) fingers, by the end of first week passing
only one finger, by the end of 2nd week the cervix should be
closed.
3- Lochia:-
It is blood stainedd uterine discharge compromised of
blood and necrotic decidua.
It is red in the first few days, concerting to pink then after
that becoming serous by the end of the 2nd week.
Persistently red lochia indicating delayed involution either
due to infection or retained tissue. Offensive lochia indicating
infection if associated with tender uterus and by pyrexia,
RX By antibiotics and evacuation of retained products.
4-Bladder function:-
Voiding difficulty and over distension are not uncommon
after child birth specially if associated with regional aesthesia.
Risk Factors:-
1- Regional anaesthesia:-
Bladder may take up to 8hr.s to again normal sensation. so
induelling catheter should be maintained for at least 12hr.s in
pt.s with regional anasthesia to prevent bladder distension and
detrusor overstretching.
2- Antidiuretic effect of high concentration of oxytocin.
3- Increased post-partum diuresis.
4- Increased fluid intake by breast feeding mothers.
5- Women with traumatic delivery such as instrumental
delivery, multiple vulvovaginal lacerations vulvo-
vaginal haematoma, prolapsed haamorriod, anal
fissures, abdominal wound haemotomas or even fecal
impaction may interfere with voiding.
Every women who has not passed urine within 4 hours
of delivery should be encouraged to urinate before
catheterization . women with difficulties in urination
should have urine sample sent for microscopy culture
and sensitivity and if the residual urine
a
catheter should be left in to allow free drainage for 48
hr.s.
5- Bowel function:-
Constipation is common problem during puerperium. So
advice about adequate fluid intake and fibre intake is necessary.
prolapsed hachorroid, anal fissure sutured perineum, women
with third or fourth degree tear should avoid constipation and
straining. So should be prescribed lactulose or methyl cellulose
for (2) weeks immediately after the repair.
6-Normal emotional and psychological changes
The ‘pinks’: for the first 24–48 hours following delivery, it is
very common for women to experience an elevation of mood, a
feeling of excitement, some
overactivity and difficulty sleeping.
The ‘blues’: as many as 80% of women may experience the
‘postnatal blues’ in the first 2 weeks after delivery. Fatigue,
short temper, difficulty sleeping, depressed mood and
tearfulness are common but usually mild, and resolve
spontaneously in the majority of cases.

Puerperal disorders:-
Daily maternal observation include temperature, pulse,
blood pressure, urinary and bowel functions, breast examination
and feeding, assessment of uterine involution, lochia, perineal
inspection, examination of legs and pelvic floor exercises,
hemoglobin checking of day (3) and a level of 8gm or less is an
indication for transfusion.
1- Perineal complications:
About 80% of women complain of pain in the first (3) days
after delivery. Which is more in patients with perineal tears or
episiotomy local cooling, topical aneasthesia diclofenac
,paracetol are usually helpful.
Spontaneous opening of repaired perineal treas and
episiotomies is usually the result of secondary infection, the
treatment is with wound irrigation twice daily, and healing with
secondary intention. Large gaping wound should be sutured
with secondary repair only after infection has cleared.
2- Bowel and bladder dysfunction
3-2 PPH:-
Defined as fresh bleeding from the genital tract between
24hr.s and 12 weeks after delivery. Most common cause is
retained placental tissue. Other causes are endometeritis,
hormonal contraception ,bleeding disorders VWD and rarely
choriocarcinoma.

Mgx include intravenous infusion, crossmatched blood,
syntocinon ,examination under aneasthesia, antibiotics if
placental tissue is found, and evacuation of the uterus.
4- Obstetric palsy:-
A condition in which one or both lower limbs may develop
signs of a motor or sensory neuropathy following delivery.
Peroneal n. palsy can occur when the nerve is compressed
between the head of the fibula and the lithotomy pole
unilateral foot drop.
RX is by bed rest with afirm board beneath the mattress,
analgesia and physiotherapy.
5- Symphysis Pubis diastasis:-
It is separation of sym.Pub either spontaneously or by
delibrate surgical seperation (symphysiotomy).
Risk factors are forcepes delivery, rapid second stage of labour
severe abduction of the thighs during delivery.
RX bed rest, antinflamatory agents, physiotherapy and a pelvic
corset to provide support and stability.
6- Thromboembolism:-
The risk increase to 5 flods in pregnancy and puerperium.
Majority of deaths are after C\S.
7-Puerperal Pyrexia:-

A temperature of 38C or higher on any two of the first 10
d.s post-pertum, exclusive of throat, breasts, urinary tract, pelvic
organs, cesarean or perineal wounds and legs.
-Chest complications, atelactasis, and aspiration
pneumonia.
-Genital tract infection:-
It is referred to as puerperal sepsis, it is oetiology:-
Following delivery natural barriers to infection are
temporarily removed and therefore arganisms with pathogenic
potential can ascend from the lower genital tract into the uterine
cavity. Placental separation exposes a large raw area equivalent
to an open wound and retained products and clots can provide
an excellent culture media for infection, in addition if there is
any lacerations in the genital tract.
Factors which determine the clinical coarse are virulence
of offending organisms, presence of haematoma or retained
products ,timing of antibiotic therapy and associated risk factors.
Risk factors are:-
- Antenatal I.U. infection.
- Cervical circlage.
- Prolonged ROM.
- Prolonged labour.multiple vaginal examinations.
- Instrumental delivery.
- Manual removal of placenta.
- Retained products of conception.
- Others like obesity, DM. HIV.
Methods of spread of infection are:-
1- Ascending infection, from lower genital tract, or infection
of placental site via fallopian tubes to the ovaries,
salpingo -opteritis peritonitis pelvic abcess.
2- By contiguity directly into the myometrium and
perametrium meteritis and parametritis
pelvic cellulitis peritonitis and pelvic abcess.
3- By lymphafics and blood vessels:-
By uterine vessels into the IVC or via ovarian vessels
septic thrombo phlebitis, or septicaemia.
Symptoms of puerperal pelvic infection:-
Malaise, headache, fever, rigor abdominal discomfort,
vomiting diarrhea, offensive lochia and 2 PPh. pelvic
thrombophlebitis cherecterised by spiking fever for 7-10
days despise antibiotic therapy.
Signs:-
Pyrexia and tachycardia, boggy tender large uterus,
infected wounds, peritonism, paralytic ileus, indurated
adnexae.
Investigation:-
Full blood count, urea and electrolytes, high vaginal swab,
pelvic U\S, clotting screen 7 and arterial blood gas, blood
culture.
Treatment:-
It is with broad spectrum antibiotics e.g. co- amaxiclav or
cephalosporine, plus metronidazole, the anibiotics should
be continued for at least 48 hr.s after the pt. becoming
afebrile, Major pathogen resistant to this RX is
Bacteroides fragilis, which is sensitive to clindamycin with
either aminoglycosides or penicillin. If pelvic
thrombophlebitis is suspected or clinically diagnosed
heparin should be instituted and may continue for weeks or
months according to which pelvic vein is involved.
Necrotising fasciitis:
It is a rare but fatal infection of skin muscle and
fascia, can originate in perineal areas, episiotomies and
C\S wound. Commonest organism is unaerobes, Clostridia
perfnrgens.
It needs wide debridement of necrotic tissues under
GA. Skin graft may be needed. In addition to mgx of
septic shock if developed.
Prevention of puerperal Sepsis:-
1- General hyegine and a septic surgical approach.
2- Prophylactic antibiotics during emergency C\S
with a single intra-operative antibiotic dose before
clamping of cord.
3- Prophylaxes of elective C\S is recommended in
units with background of infectious morbidity.
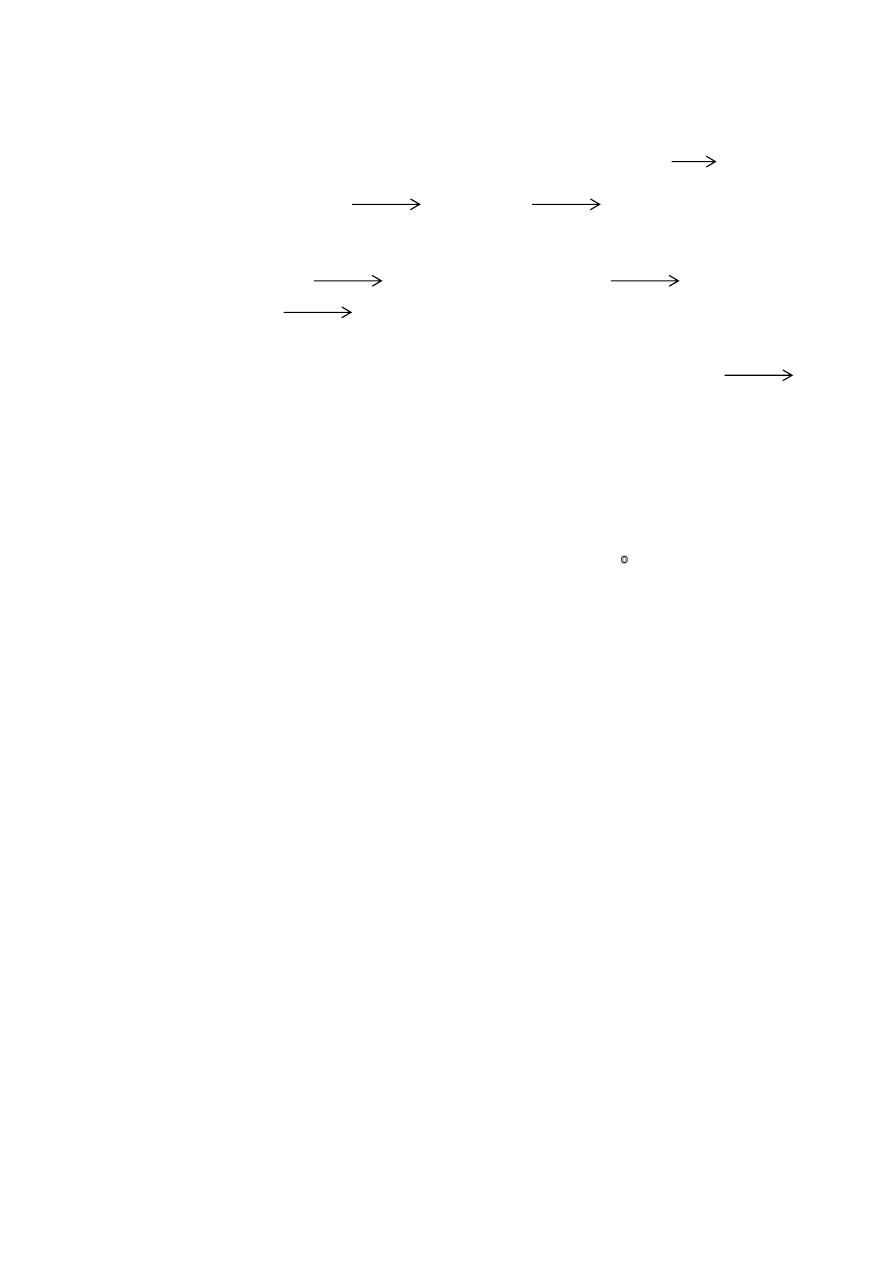
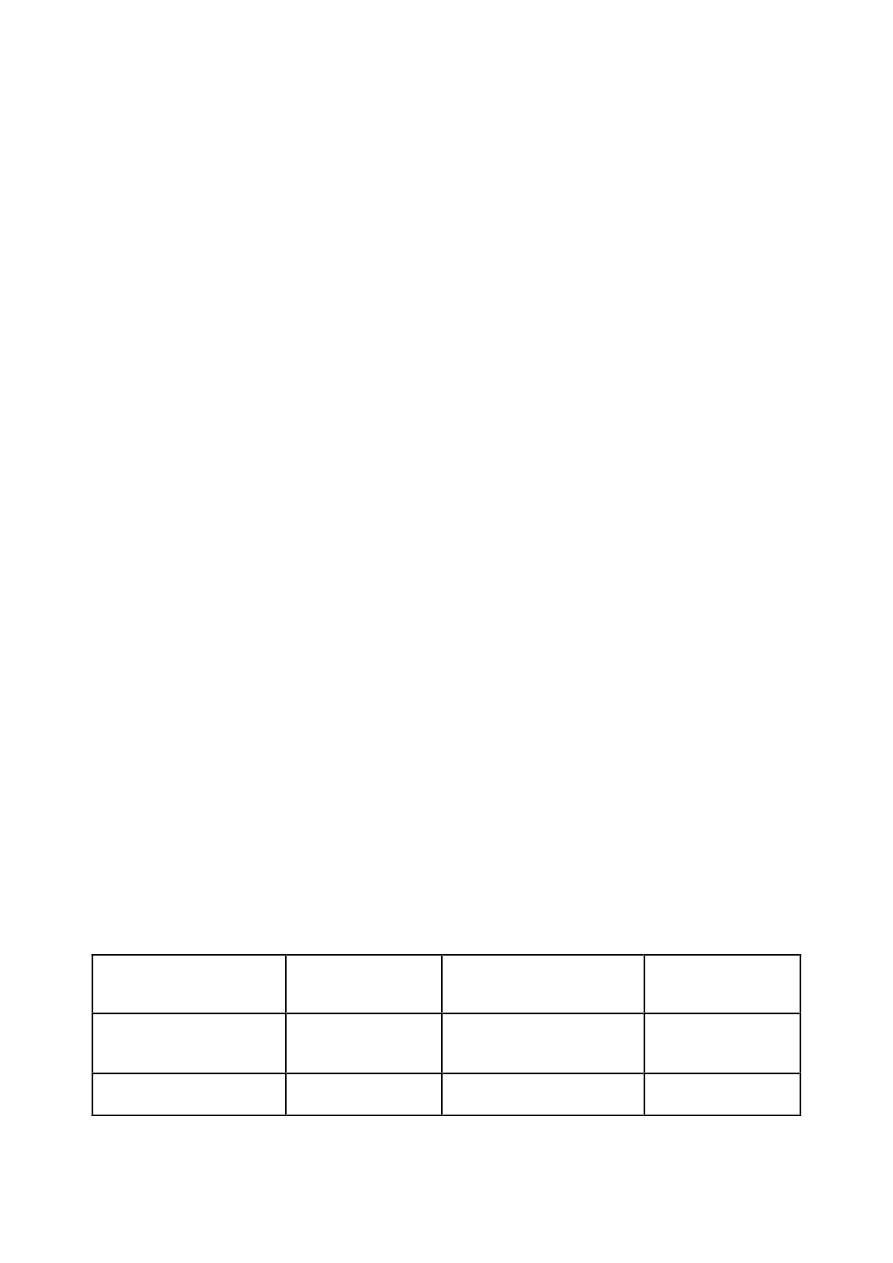
Diagnosis and management of puerperal pyrexia
ﻟ
ﻼ
ط
ﻼ
ع
Symptoms
Diagnosis
Special
investigation
management
Cough
Chest
infection
Sputum M.C and S
Physiotherapy
Purulent sputum
Pneumonia
Chest x.ray
Antibiotics
Breasts Disorders:-
-Blood stained nipple discharge:-
It is bilateral due of epi. Proliferation. Usually occur in the 2
nd
or
3
rd
trimester, It is self-limited, needing just reassurance.
-Painful nipples:-
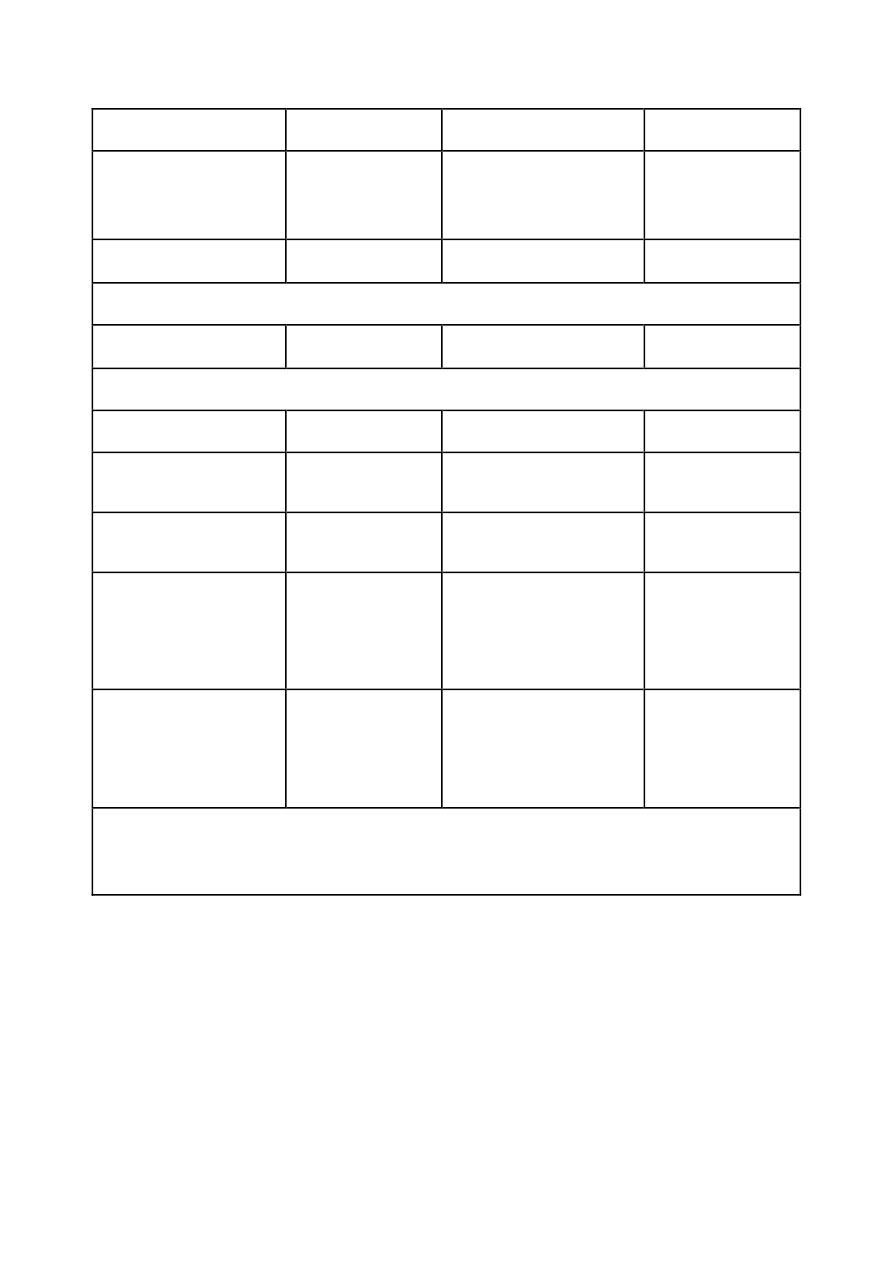
Sore throat
Tonsillitis
Throat swab
Antibiotics
Cervical
lymphadenopathy
Headaches
Meningitis
Lumbar puncture
Antibiotics
Neck stiffness (epidural/spinal anesthetic)
Dysuria
Pyelonephritis
Urine M.c and s
Antibiotics
Loin pain and tenderness
Secondary PPH
Metritis
Pelvic ultrasound
Antibiotics
Tender bulky
uterus
Retained
placental
Uterine tissue
Pelvic/calfpain/
Tenderness
Deep vein
thrombosis
Doppler/venogram
of legs
Heparin
Chest pain
Pulmonary
embolism
Chest x-ray and
blood gases
Lung
perfusion
scan
angiogram
Painful engorged
breasts
Mastitis
Abscess
Milk c and s
Express milk
Antibiotics
Incision and
drainage
VI, c and s. microscopy, culture and sensitivity; PPH. postpartum
haemorrhage.
It is due to nipple fissuring or denuded covered epithelium,
either d.t poor positioning or candidiasis.
RX with nipple rest, manual milk experession and then reint-
roduce feeding gradually.
Galactocele:-
It is cretention cyst of the memmary duct. Usually resolves
spondeheausely, if not aspertion.
Breast engorgerment:-
Usually begins by the 2
nd
or 3
rd
postpartum day and may give
rise to puerperal fever of up to 39C .
RX by allowing the baby easy access to the breast with manual
expression, firm support, ice bag and breast pump.
Mastitis:-
It is either d.t infection or duct obstruction. The affected
segment of the breast appear red. Painful and edematous. Flue
like symptoms develop associated with a tacthycardia and
pyrexia. It is usually present in the third or fourth post-partum
week and is usually unilat. The most common arganism is S.
aureus other like coagulase negative staph and strepto coccus
veridens.
Mgx include isolation of the mother and baby ceasing B.F from
affected breast, expression of milk manually and sending a milk
for culture and sensitivity. Flucloxacillin can be commenced
while awaiting sensitivity results. If breast abcess develop
drainage under G.A.
