Anatomy of female genital tract
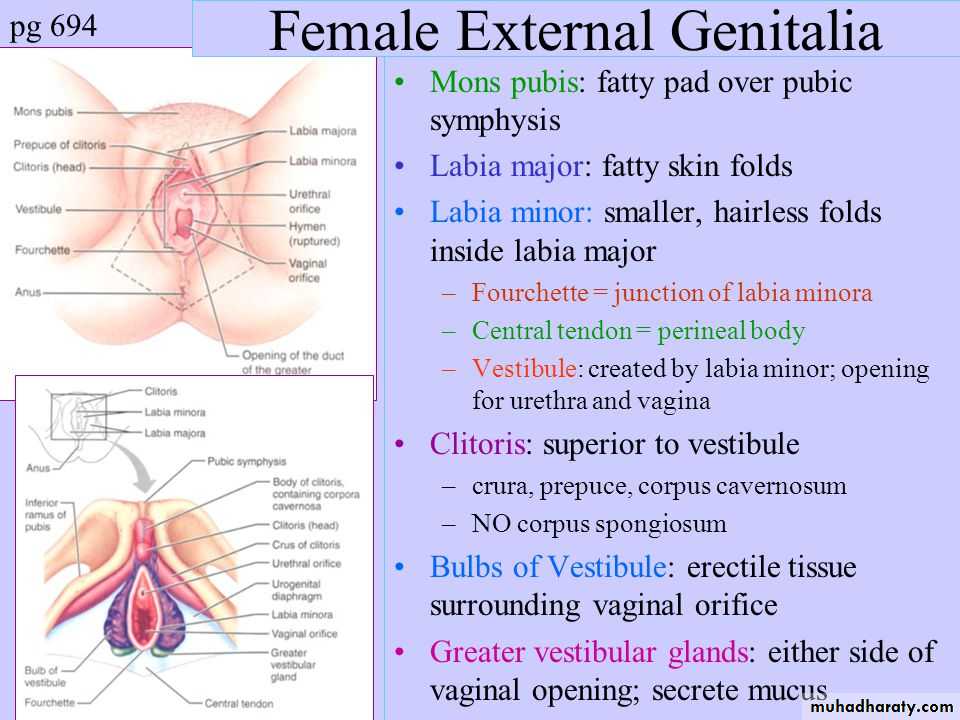
The external genitaliaIs commonly called the vulva
Includes the
1.mons pubis
Fibro fatty pad covered by hair bearing skin which covers the body of pubis bone
2.labia majora
. are two folds of skin with underlying adipose tissue either side of the vagina opening. they contain sebaceous and sweat glands and few specialized apocrine glands
.in the deepest part of each labium are the core of fatty tissue continuous with that of inguinal canal and the round ligament terminate her
3.labia minora
. are two thin folds of skin that lie between the labia majora. these vary in size and may protrude beyond the labia majora where they are visible but also my concealed by labia majora
. anteriorly the divide into two to form prepuce and frenulum of clitoris (clitoris hood)
Posteriorly they divide to form fold of skin called fourchette
They contain sebaceous glands but have no adipose tissue
They are not well developed before puberty and atrophy after menopause
4.clitoris
is an erectile structure measuring approximately 0.3 -3.5 cm in length
Body of clitoris made up of paired of corpora cavernosa (which is columns of erectile tissue and vascular tissue)
These become crura at the bottom of the clitoris
5. vestibule
Is the cleft between the two labia minoraIt contains opening of the urethra, Bartholin glands and vagina
6.Bartholin glands
Bilateral about the size of peaThey opening via 2 cm duct into the vestibule below hymen
Contribute to lubrication during intercourse
7.Hymen
Is a thin covering of mucus membrane across the entrance of the vagina is usually perforated which allow menstruation?Remaining part of the hymen after rupture are called carunculate myrtiforms
The internal reproductive organs
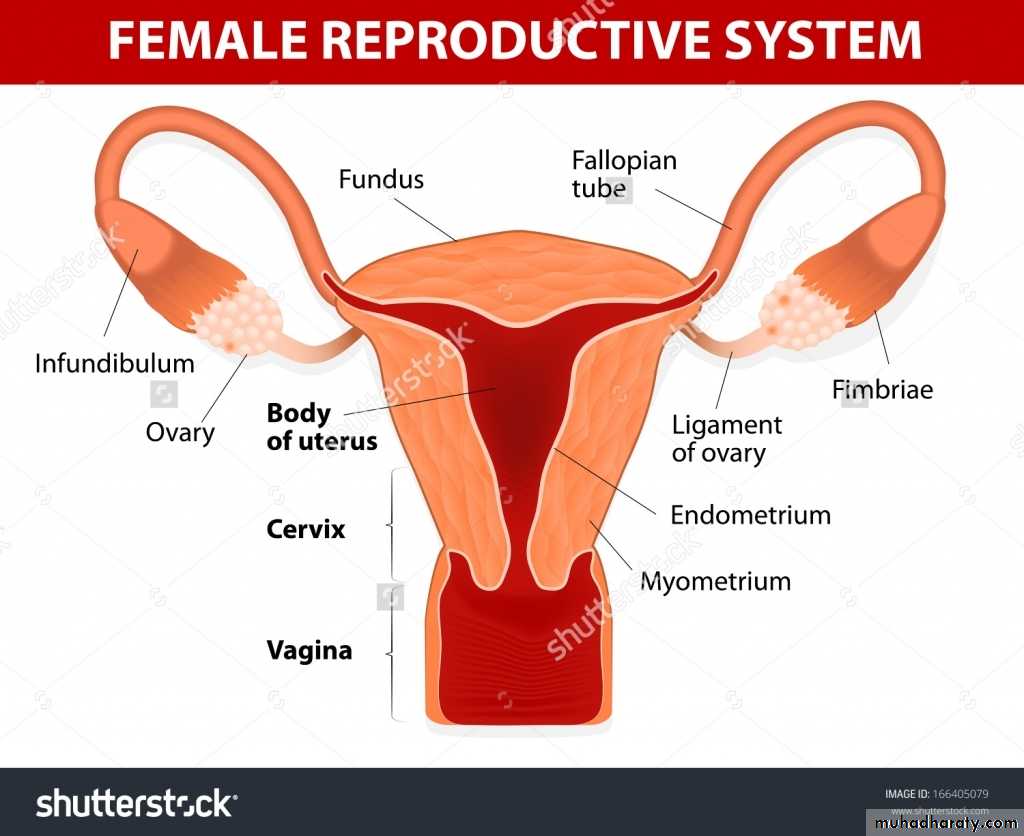
+The vagina
.is fibromuscular canal lined with stratified squamous epithelial that leads from the uterus to the vulva
.its longer in the posterior wall 9 cm than in the anterior wall 7 cm
. the vaginal wall usually in apposition except at the vault where they are separated by the cervix
The vault of the vagina is divided into four fornices posterior, anterior and two lateral
The vaginal wall lined with transverse folds
Has no gland and is kept moist by the secretions from uterine and cervical gland and from transudation from its epithelial lining
.the epithelium is thick and rich in glycogen but absent before puberty and after menopause due to lack of estrogen
The upper posterior wall forms the anterior peritoneal reflection of the pouch of Douglas
Middle third separated from rectum by pelvic fascia and the lower third abuts the perineal body
Anteriorly the vagina is direct contact with bladder base
Laterally the vagina is related to the cardinal ligament
Below levator muscle and ischiorectal fossa
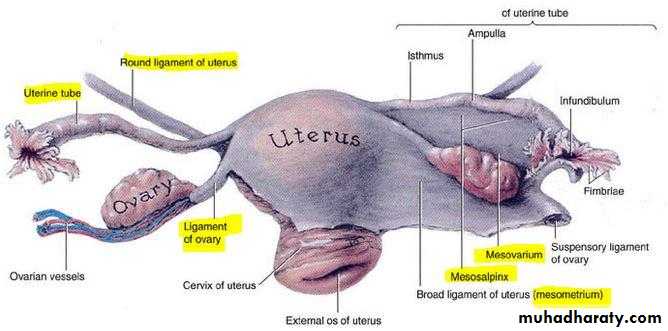
The uterus
. shape like inverted pear tapering inferiorly to the cervix and is situated entirely within the pelvis
. hallow thick muscular structure
.7.5 cm long 5cm wide 3 cm thick 70 gm weight
. upper part called body, the area of insertion of each fallopian tube is called cornu , fundus is the part of the body above the cornu , isthmus is small lower constricted area
. direction anteversion the longitudinal axis of the uterus at right angle to the vagina
Ant flexion the uterus flexed foreword on itself at the isthmus
Retroversion the uterus tilted backward 20 % of female
. three layer outer serous layer (peritoneal) middle muscular layer (myometrium) and the inner mucous layer (endometrium)
The myometrium forms the bulk and is made of interlacing smooth muscle fibers
intermingling with areolar tissue blood vessel and lymphatics
.the endometrium is covered with single ciliated columnar epithelial varies thickness 1-5 according to the cycle
The cervix
.2.5 cm lengthLateral to cervix connective tissue called parametrium
Upperpart mostly consist of involuntary muscle whereas lower part is mainly fibrous connective tissue
.the membrane of cervical canal (endocevix) has ant and post columns from which folds radiate out ,the arbour vitae .it has numerous deep glandular follicle that secrete clear alkaline mucus the main component of physiological vaginal discharge
.ciliated columnar epithelial in upper 2/3 and change to stratified epithelial around the region of external os and the junction of these two types of epithelial is called squamocolumner junction or transformation zone
The fallopian tubes
Each tube is about 10 cm long run in upper margin of broad ligaments connect between the uterus one side and the peritoneal cavity on the other side
Describe in four parts
.the interstitial portion
The isthmus
The ampulla
The infundibulum or fimbrial portion
The muscular fibers of the wall of the tube are arranged in the inner circular and an outer longitudinal layer
There is no submucosa and there are no gland
The epithelial of the tube contain ciliated cell
The ovary
The size and appearance of the ovaries depend on the the age and the state of the menstrual cycle
Almond shaped and measure approximately 3 cm long 1.5 cm width and 1 cm thick
Each ovary is attached to the cornua of the uterus by ovarian ligment and at the hilum to the broad ligment by mesovarium which contains its supply of blood vessels and nerves
The ovary is the only intraperitoneal structures not covered by peritoneum
Has central vascular medulla and outer thicker cortex
The vestigial structures
Remains of the mesonephric duct and tubules are always present in young children
Variable structures in adult the epoophoron ,paroophoron in the broad ligament
The duct of Gartner is the caudal part of mesonephric duct running alongside the uterus to internal os
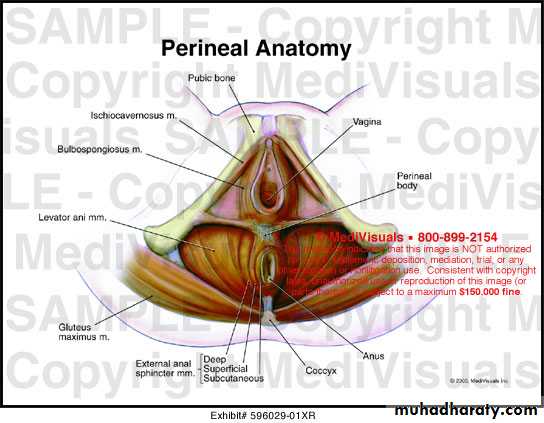
The pelvic muscles ligaments and fascia
The pelvic diaphragmIs formed by the levetor ani muscles which are broad flat muscles the fiber of which pass down wards and inwards, one on either side constitute the pelvic diaphragm
The muscle is described in two parts
.the pubococcygeus which arises from the pubis bone and the anterior part of the tendinous arch of pelvic fascia (white line )
.the iliococcygeus which arises from the posterior part of the tendinous arch and ischial spine
Urogenital diaphragm
Is triangular ligament made up of two layers of pelvic fascia which fill the gap between the descending pubic rami and lies beneath the levator ani muscles. the deep transvers perineal muscles lie between the two layers and diaphragm is pierced by the urethra and the vagina
The perineal body
This is mass of muscular tissue that lies between the anal canal and the lower third of the vaginaIts apex is at the lower end of the rectovaginal septum at the point where the rectum and posterior vagineal walls come into contact. the base is covered with the skin and extend from the fourchette to the anus
Ligament
.broad ligament its peritoneal reflection from lateral borders of the uterus so despite the name its not ligament and does not support the uterus
.the ovarian ligament from the medial pole of the ovary to the uterus just below the point of the entry of the fallopian tube
.the round ligament is the continuation of the same structure and run forwards under the anterior leaf of peritoneum to enter the inguinal canal ending in the subcutaneous tissue of the labium major
.the cardinal ligaments (transverse cervical ligaments) provide the essential support of the uterus and vaginal vault .these are two strong fan shaped fibromuscular bands which pass from the cervix and vagineal vault to the side wall of the pelvis on either side
.the uterosacral ligament run from the cervix and vaginal vault to the sacrum
The bladder is supported laterally by the condensations of the vesical pelvic fascia one each side and by the sheath of pubocervical fascia which lie beneath it anteriorlyThe blood supply
The ovary ovarian arteries from abdominal aortaRight vein to inferior vena cava ,left vein to left renal vein
The uterus main supply from uterine artery which is branch of internal iliac artery
Uterine branch of ovarian artery on each sideOther parts of the pelvic organs are supplied by branches of internal iliac artery which includes vaginal artery ,vesical artery ,rectal artery ,pudendal artery
Major nerve supply of the pelvis comes from the pudendal nerves which arise from the second third and forth sacral nerves
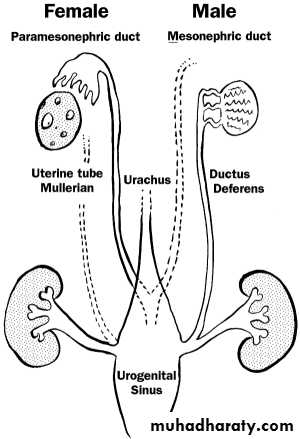
The embryology
.the primitive gonad is formed between 5-7 weeks of gestation ,when undifferentiated germ cell migrate from the yolk sac to the genital ridges
.in the absence of male determinants, the primitive gonad becomes an ovary
.granulosa cells derived from the proliferating coelomic epithelium surround the germ cells and form primordial follicles
.theca cells develop from the proliferating coelomic epithelium and are separated from the granulosa cells by basal lamina
.the maximum number of primordial follicles is reached at 20 weeks gestation when at this time there are six million primordial follicles present
.the number of these reduce by atresia and by birth one to two million are present .atresia continues throughout childhood and by menstruation 300 000 – 400 000 are present
The uterus and vagina
. the genital system develops in close association with the urinary system. 5 th week of embryonic life the nephrogenic duct develops from the mesoderm and forms the urogenital ridge and mesonephric duct
.the mesonephric duct (wolffian duct ) develops under the influence of testosterone into vas deferens, epididymis and seminal vesicle
.the female reproductive tract develop from paired ducts which are adjacent to the mesonephric duct and so are called the paramesonephric ducts or Mullerian ducts .these extend caudally to project into posterior wall of the urogenital sinus as the mullerian tubercle
.these fuse in the midline distally to form the uterus ,cervix and proximal two thirds of the vagina
.the unfused caudal segments form the fallopian tubes
.the distal vagina is form the sinovaginal bulb in the upper portion of urogenital sinus
The external genitalia
.5th to 7th weeks of life the cloacal folds which are a pair of swellings adjacent to the cloacal membrane fuse anteriorly to become the genital tubercle. This will become the clitoris
.the perineum develops and divides the cloaca membrane into an anterior urogenital membrane and posterior anal membrane
.the cloacal folds anteriorly are called the ureteral folds which form the labia minor
Another pair of folds within the cloacal membrane form the labioscrotal fold which eventually become the labia majora
The urogenital sinus become the vestibule of the vagina
The external genitalia are recognizable female by the end of 12 weeks' gestation
1.the vagina has two wall anterior and posterior one which are equal in length
2.the vaginal wall is rich in glandular tissue which responsible on acidity of vaginal discharge3.the serous layer of the uterus is varying in its thickness according to menstrual cycle
4.the widest part of fallopian tube is isthmus part5.the ovary has central thick avascular medulla and outer loose cortex
6.the perineal body is a mass of muscular tissue lies between the urethra and lower third of the vagina7.the broad ligament is the main support of the uterus
8.the ovarian artery is branch of internal iliac artery
9. the fused mesonephric duct form the future uterus and cervix10. the external genitalia are recognizing as female by the 9 weeks' gestation
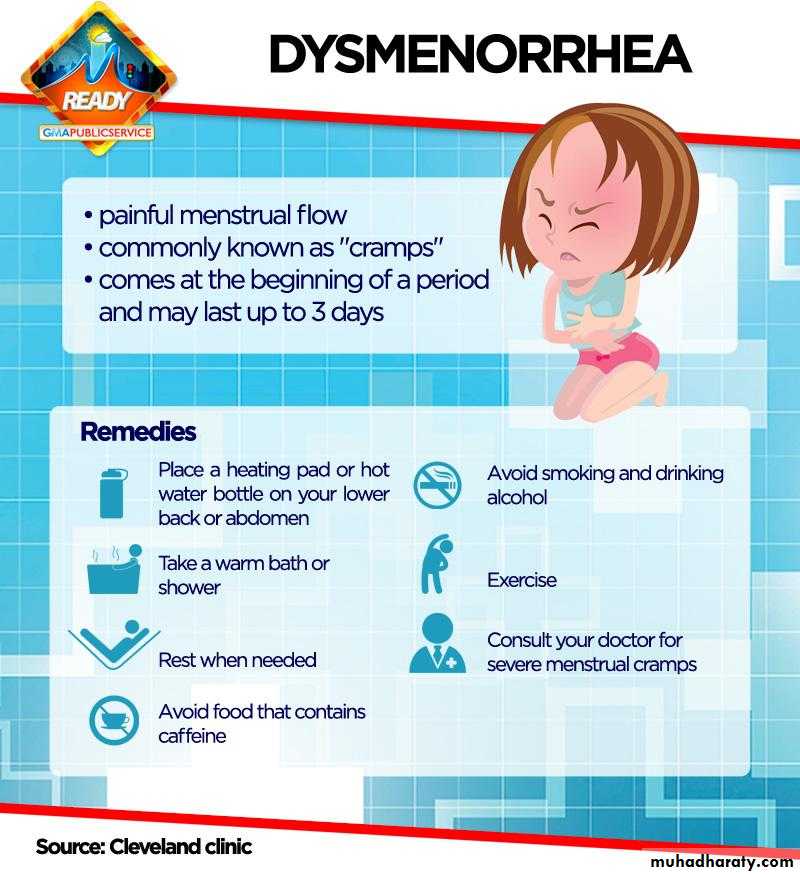
DYSMENORRHEA
Definition is painful menstruation
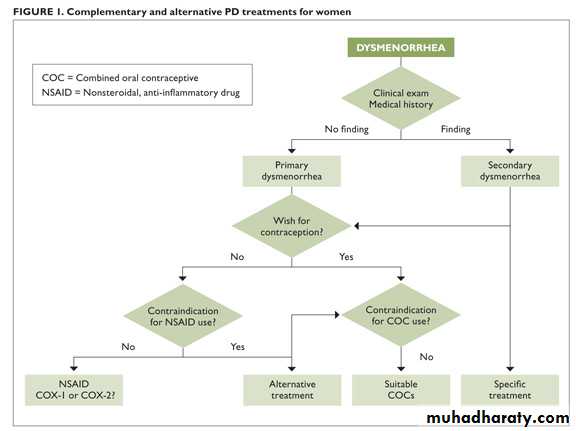
Classification :1. primary dysmenorrhea2.secondary dysmenorrhea
Epidemiology
. the age and parity are inversely related to the incidence of dysmenorrhea. family history
. stress increase incidence
. smoking . low body mass index
. early menarche . heavy menstrual loss
. exercise and high intake of fruit and vegetables reduce incidence
. psychological morbidity . sexual abuse
Causes
Primary dysmenorrhea. uterine myometrium hyperactivity
. excess prostaglandin production during menstruation –increase myometrium contraction –reduction uterine blood flow –increase ischemia and pain
. physiological
. ovulatory cycle is essential for development
Secondary dysmenorrhea
. underlying pathological causes. causes gynecological
. endometriosis . adenomyosis. uterine fibroid
. cervical stenosis and other obstructive causes
. pelvic venous congestion
. residual \trapped ovary syndrome
. pelvic adhesion . pelvic inflammatory disease
Gastrointestinal: irritable bowel syndrome
Chronic constipation
Urinary tract :bladder pain syndrome (interstitial cystitis )
Musculoskeletal :pelvic floor myalgia
Myofascial pain
Neurology :nerve entrapment
Symptoms and sign
Primary spasmodic dysmenorrhea:.is colicky cramping suprapubic pain that may radiate to the back and thigh
. associated with gastrointestinal and systemic symptoms.is usually begin few hours before or within the onset of menstruation
. continue for 8 to 72 hour
. typically, in young female
. onset within 6- 12 months after menarche
. cause significant morbidity and negative pelvic pathology
Secondary dysmenorrhea
. pain associated with identifiable pelvic pathology.is more sever before menstruation
. exacerbated by menstruation and continue throughout the cycle
. usually associated with deep dyspareunia
. usually more common in older woman
INVESTIGATION
Investigation of primary dysmenorrhea is unnecessary unless there are atypical symptoms or abnormal finding on pelvic examination
. ultrasound: endometriomata, PID sequelae, fibroid, congenital abnormalities
.STI screan including chlamydia swab. laparoscopy is usually reserved for woman with ultrasound abnormalities, medical treatment failure or those with concomitant subfertility
. hystrosalpingogram useful to identify intrauterine adhesion
.MRI
TREATMENT
In the majority nothing more than general advice, reassurance and empirical relief of painThe girl should realize that her complaint is likely to be short lived
NSAIDs :produce moderate or excellent pain relief
More effective than paracetamolSelection according to cost and patient preference (naproxen ,mefenamic acid ,diclofenac ……)
Limited by its side effect
May be used in combination with another drug like codeine and paracetamol
Calcium channel blocker
Oral contraception
For inhibition of ovulationLNG-IUS
Effective for pain and as contraceptionGnRH analogues
Act through induce hypo estrogen stateLimited use
Relive the symptom if waiting for hysterectomy or as a form of assessment as to the benefits of hysterectomy
Heat :effective as NSIAD in relieving pain
Life style changes.low fat ,vegetable diet may improve the symptoms
.exercise may improve symptoms by improving blood flow to the pelvis
.vitamin B1 and magnesium
Treatment of underlying pathology in case of secondary dysmenorrhea
Therapeutic laparoscopy :diagnosis and management of endometriosis adhesion and PID.hysterectomy is now rare
. laproscopic uterine nerve ablation is not currently recommended.injection of pelvic plexus with anesthetic agent
.dilation of the cervix
Self-assessment
Q1: how can you clinically differentiate between primary and secondary dysmenorrheaQ2:what types of birth control methods help control dysmenorrhea ?
Q3: what is the surgery done to treat dysmenorrhea
Q4 :what alternative treatment help ease dysmenorrhea (non medical)
..