ANTI-CHOLINERGIC DRUGS
Dr. Hussain Addai aljabery
M.B.Ch.B M.Sc. ( Pharm .)
D.M.R.D F.I.B..M.S ( Radio)
OBJECTIVES
•
• Classify anticholinergic drugs
•
• Describe the mechanism of action,
•
pharmacological actions, therapeutic uses
•
and adverse effects of anticholinergic
•
drugs
•
• Describe the treatment of atropine toxicity
•
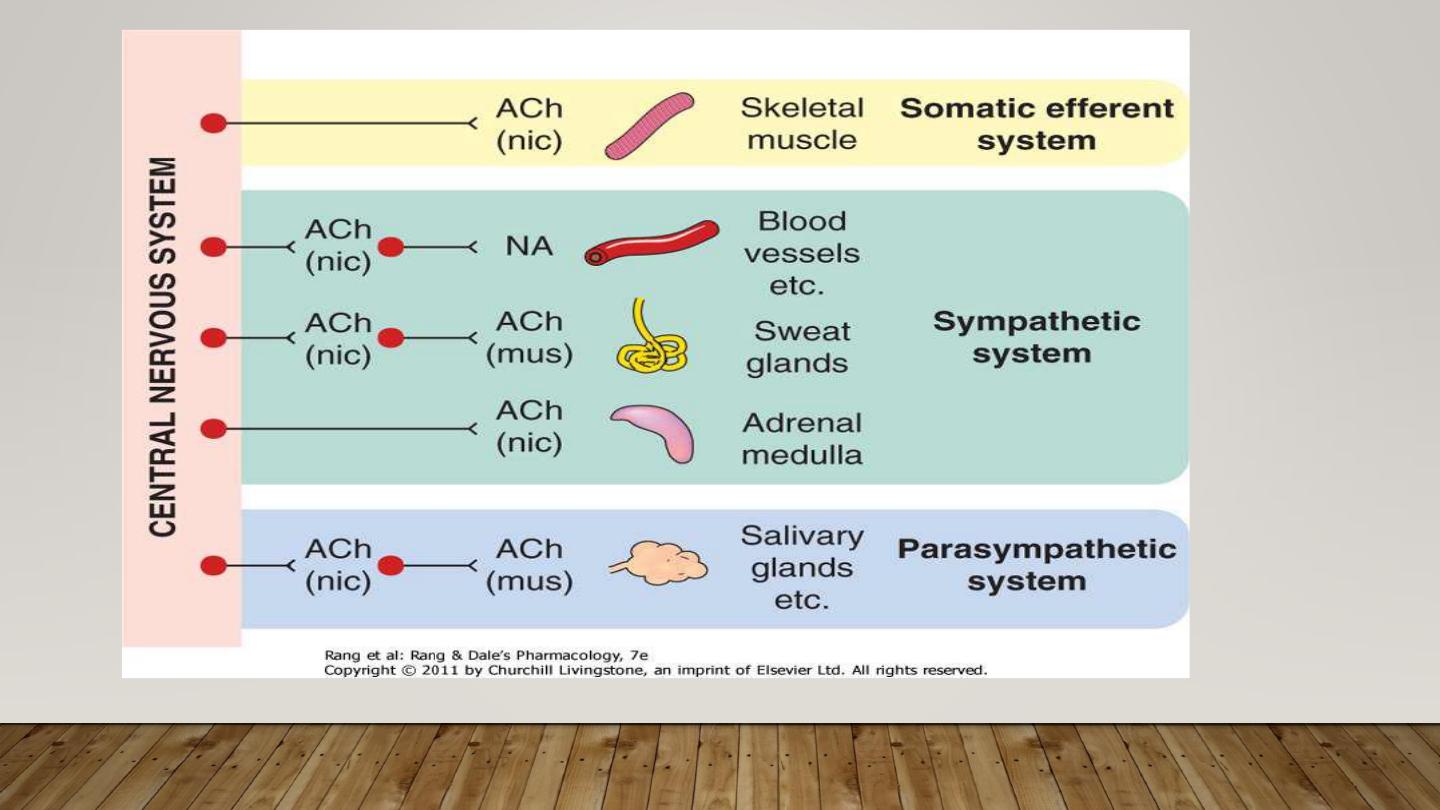
An anticholinergic agent is a substance that blocks the neurotransmitter acetylcholine
in the central and the peripheral nervous system they inhibit parasympathetic nerve
impulses by selectively blocking the binding of the neurotransmitter acetylcholine to its
receptor in nerve cells
ANTIMUSCARINIC DRUGS
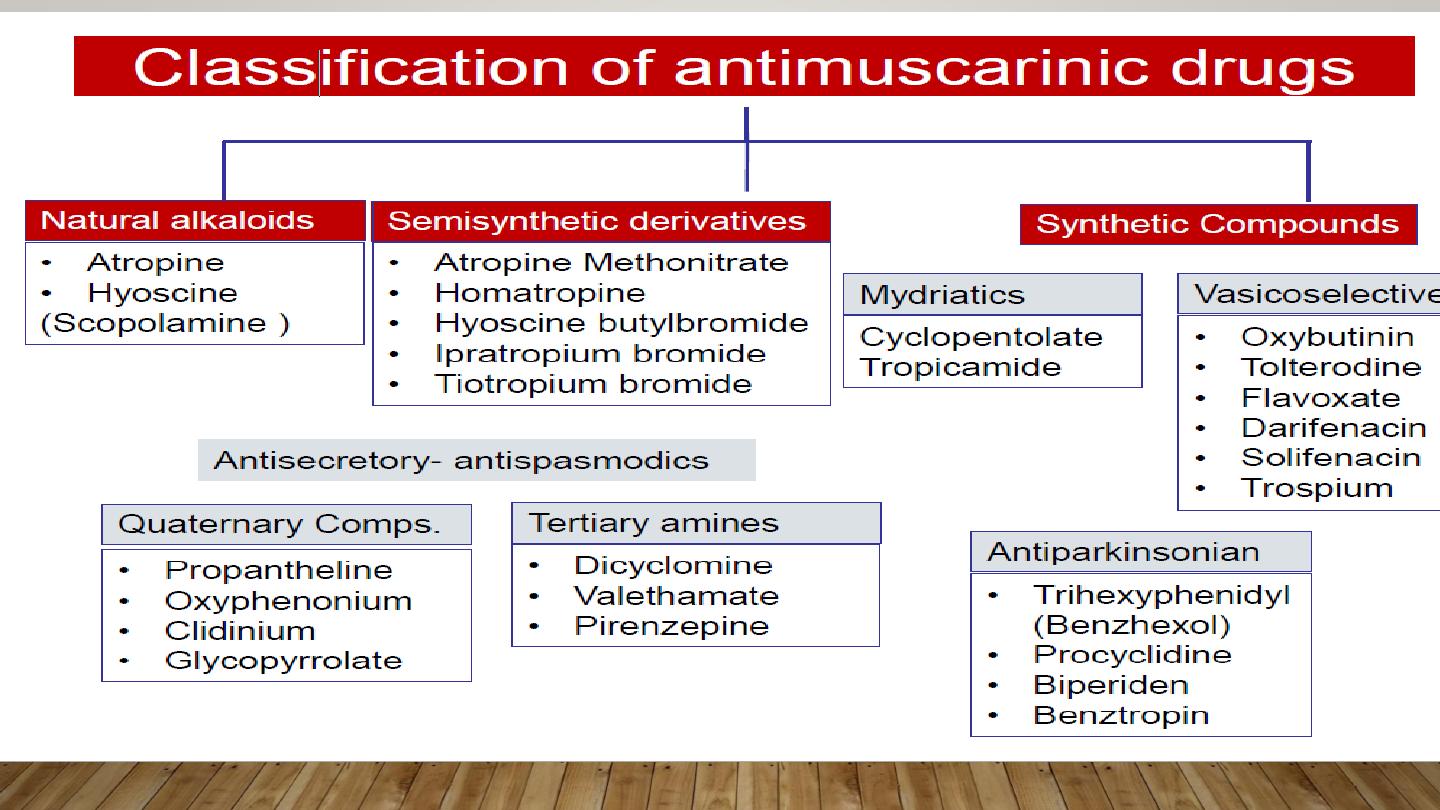
NATURAL ALKALOIDS
•
Atropine
•
Scopolamine
•
Atropine prototype drug
•
Source---Atropa belladona
•
(deadly night shade)
•
Datura stramoni
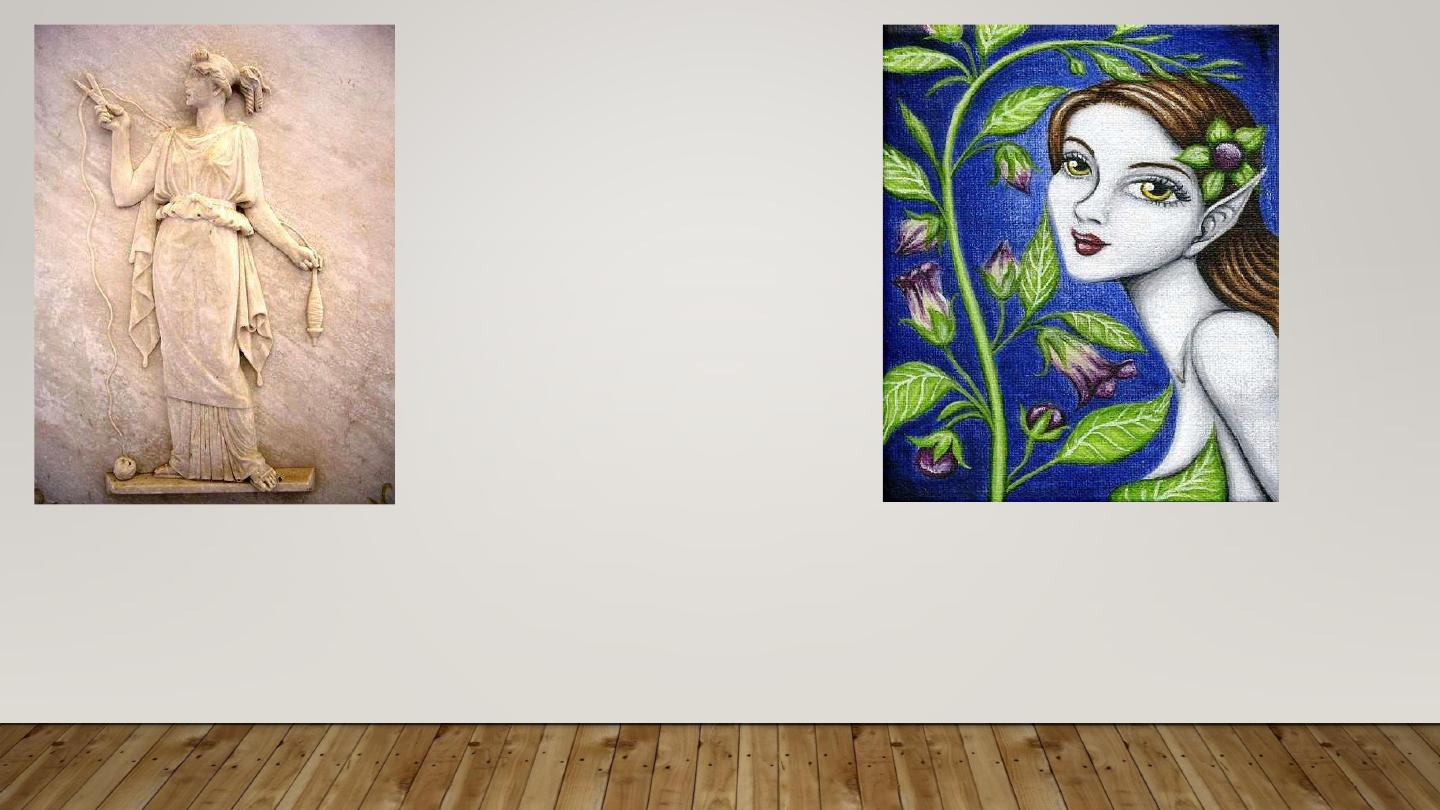
ATROPOS
BELLADONNA
Linnaeus – Atropa belladona

SOLANACEAE
FAMILY
Atropa belladona
Hyocyamus niger
PHARMACOLOGICAL ACTIONS OF ATROPINE
CNS:
– Mild CNS stimulant action in therapeutic doses
– Large doses- excitement, restlessness, hallucinations
– Antiparkinsonian effect by reducing cholinergic overactivity in basal ganglia
– Antimotion sickness effect by suppressing vestibular disturbances
CVS :
– Low doses of atropine cause bradycardia due to blockade of presynaptic M1 receptors on
vagal nerve endings (Inhibit release of Ach)
– Moderate to high doses cause tachycardiadue to blockade of M2 receptors in heart
– ↑ SA and AV nodal conduction ↓ PR interval
Glands
– All secretions under cholinergic influence
reduced (Due to M3 receptor block)
– Except Milk and Bile secretion
– Skin and mucus membrane become dry
Smooth muscles
– GIT:
• ↓Tone and motility
• ↑ Sphincter tone may cause constipation
• Relaxes smooth muscle of gall bladder
– Genitourinary tract
• Relaxes detrusor muscle of bladder & ↑ tone of trigone
and sphincter (Retention of urine)
– Bronchi
• Relaxes bronchial smooth muscle
• ↓ secretion & muco-ciliary clearance (mucus plug may
form)
EYE
Mydriasis
Paralysis of ciliary muscle (cycloplegia):
Loss of accommodation
Adjustment of eye for far vision
Photophobia
Blurred vision
Lasts for 7-10 days
Acute glaucoma attack in patient with narrow iridocorneal angle due
to impairment of drainage
Reduction of lacrimal secretion leading dry sandy eye
PHARMACOKINETICS OF ANTICHOLINERGIC
DRUGS
•
Absorption :
– Atropine, scopolamine other tertiary amines well absorbed
• Distribution:
– except quaternary compounds rest drugs are widely
distributed.
• Metabolism:
– 50% atropine & 80 % scopolamine metabolized by liver as
conjugates
• Excretion
– 50% atropine excreted unchanged in urine
– t ½ = 3 hours
THERAPEUTIC USES OF ANTICHOLINERGIC
DRUGS
1.
Parkinsonism
2. Motion sickness
3. Bronchial Asthma & COPD
4. Vagolytic to treat sinus bradycardia, partial
heart block
5. Antispasmodic in dysmennorhoea
6. Intestinal, renal, biliary colic
7. Relieve bladder spasm after uro-surgery, Urinary incontinence
8. Ophthalmic uses
– Mydriatic and cycloplegic for refraction testing
– Mydriatic for fundoscopy
– Iridocyclitis used alternatingly with miotics to break the adhesions between iris and lens
9. Preanaesthetic medication
– Atropine or glycopyrrolate used to prevent vagal bradycardia and laryngospasm
10. Sialorrhoea (also known as drooling)
11. Organo-phosporus Poisoning
12. some type of mushroom poisoning
13. Along with neostigmine to counter its muscarinic effects
ADVERSE EFFECTS
•
Dry mouth, difficulty swallowing
• Photophobia, blurred vision
• May precipitate acute congestive glaucoma
• Retention of urine
• Constipation
• Restlessness, excitement
• Tachycardia, palpitations
ATROPINE TOXICITY
•
Hot as a hare: hyperpyrexia
• Red as beetroot: cutaneous vasodilation
• Dry as a bone: dry skin
• Blind as a bat: mydriasis and cycloplegia
• Mad as hatter: restlessness, excitement
TREATMENT OF ATROPINE POISONING
• Hospitalization
• Gastric lavage
• Tepid sponging
• Diazepam to control convulsions
• Antidote for atropine poisoning is
physostigmine 1-4 mg injected slowly
CONTRAINDICATIONS OF ATROPINE
• Acute congestive glaucoma
• Elderly patients (More prone for urinary
retention)
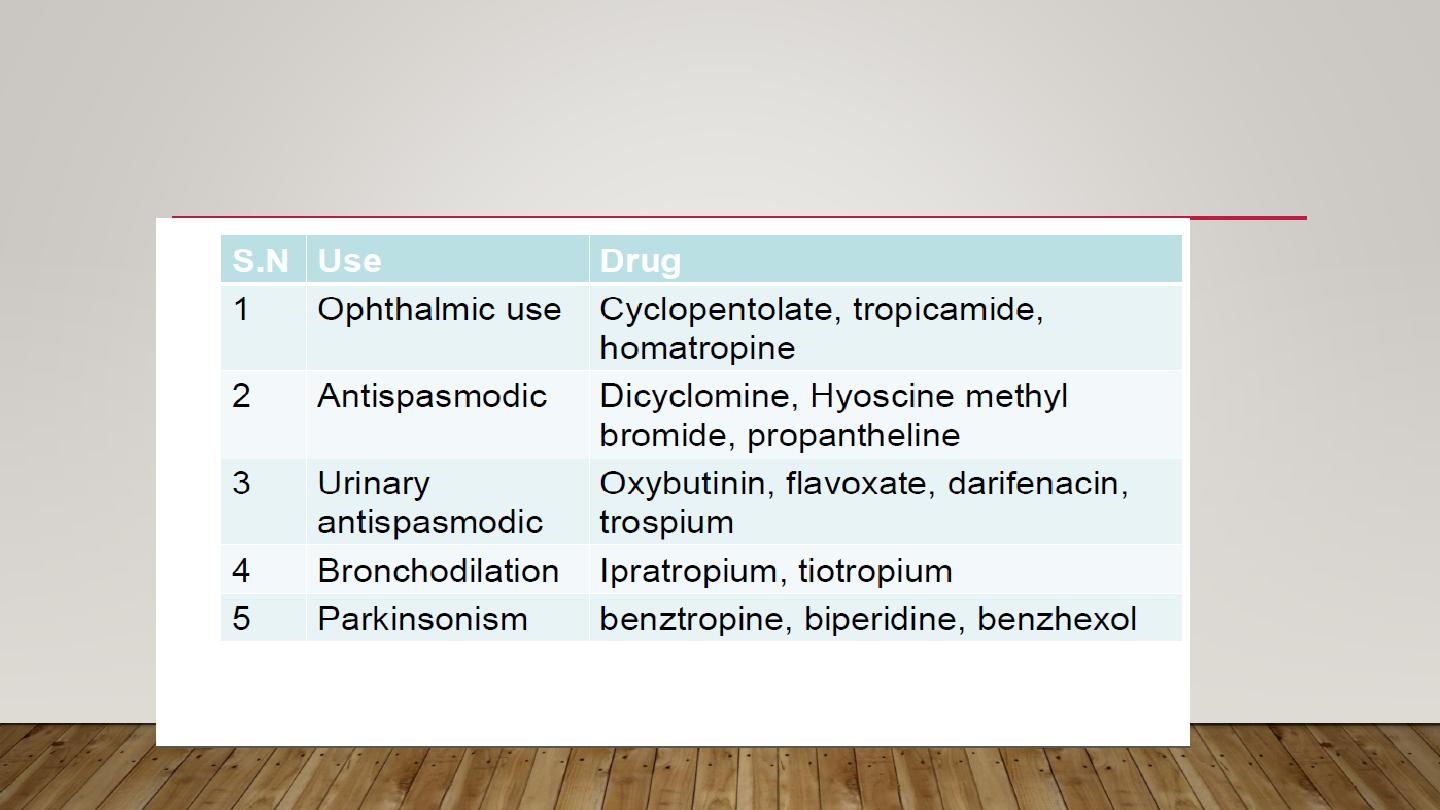
CLASSIFICATION OF ANTICHOLINERGICS ACCORDING
TO CLINICAL USE
GANGLIONIC BLOCKERS
Hexamethonium : acts mainly by channel blocker
Decamethonium
Quaternary -Tetraethyl ammonium:
short acting
-Pentolinium
-Chlorizondamine
-Trimetaphan:
very short acting
-Mecamylamine
Secondary -Pempidine
MECHANISM OF GANGLIONIC BLOCK
:
1) Depolarizing block, eg. by sustained
depolarization: Ach, nicotine, carbamoylcholine
2) Nondepolarizing competitive antagonism of Ni
receptors
3) Channel block: Hexamethonium
RESULTS OF GANGLION BLOCKADE
CNS:
- Quaternary group is devoid of such effects
- Secondary group readily enters CNS: sedation, tremor,
choreiform movements, mental disturbances
EYE:
- Moderate mydriasis (since p.sympathetic influence on
iris is dominant)
- Cycloplegia with loss of accommodation
CVS:
- Sympathetic CV reflexes are depressed
- Sympathetic influence on arteriols and veins are
diminished, PVR and venous return are reduced,
vasodilatation, hypotension (orthostatic), tachycardia
GUT:
- Secretions and motility are inhibited
- Some degree of constipation
Urinary system:
- Urination is blocked
- Urine retention in a man with prostate hypertrophy
Thermoregulatory sweating is blocked
T
HERAPEUTIC USES
:
1) Hypertension:
- rapid tolerance development and orthostatic
hypotension
-now more effective agents are available
2) Acute hypertensive crisis in a patient with
dissecting aortic aneurism.
Trimetaphan: 0.5-3mg/min by iv infusion
Disadvantage: tolerance development within 48h
3) Production of controlled hypotension to minimize
haemorrhage at the operative field.
Trimetaphan: 1-4mg/min by iv infusion
4) Autonomic hyperreflexia (or reflex sympathetic
dystrophy)
Side effects:
The most serious one is orthostatic
hypotension
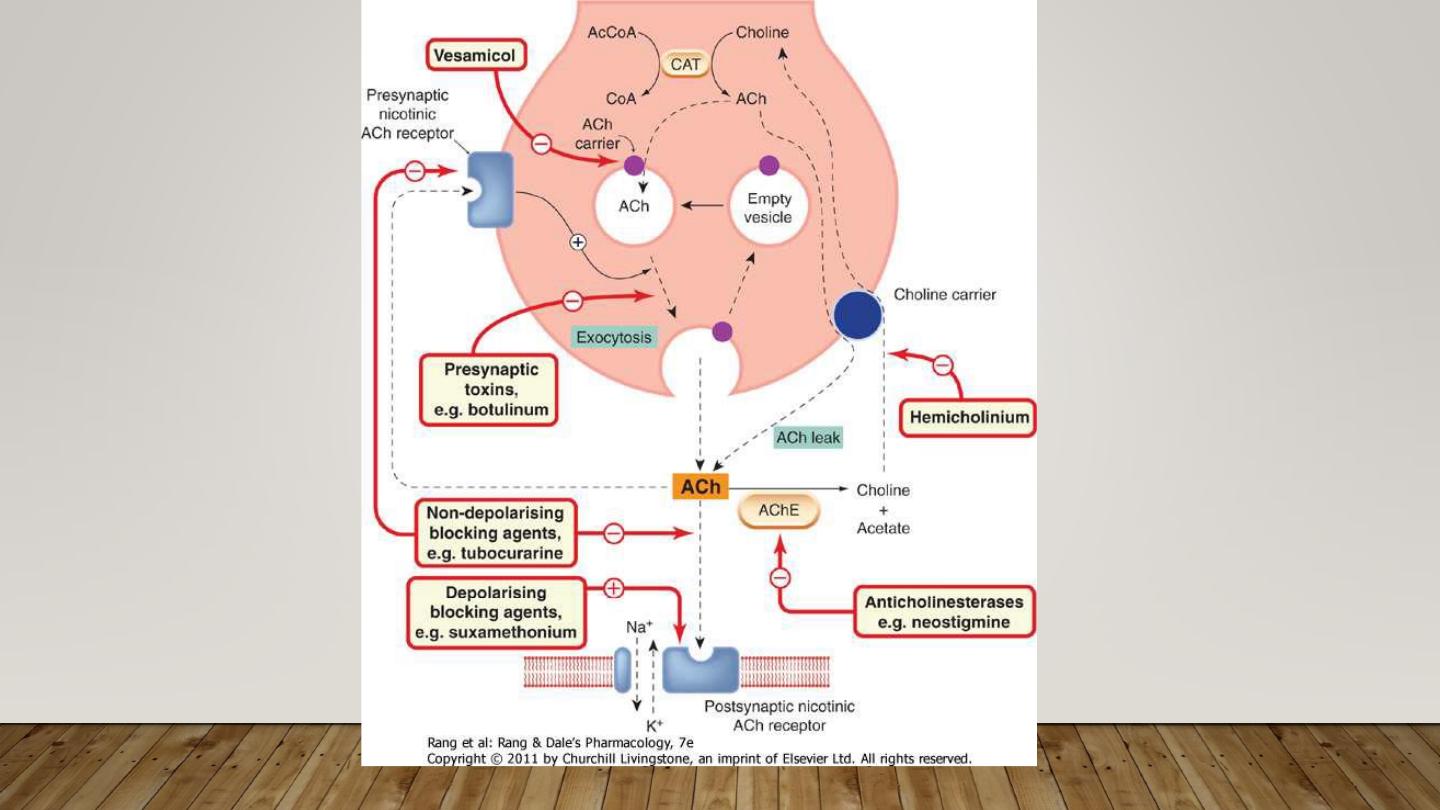
NEUROMUSCULAR BLOCKERS
Block synaptic transmission at the neuromuscular
junction
Affect synaptic transmission only at skeletal muscle
Does not affect nerve transmission, action potential
generation
Act at nicotinic acetylcholine receptor NM
•
Classification:
•
Neuromuscular blocking agents:-
1) Depolarizing muscle relaxants.
2) Non-depolarizing muscle relaxants
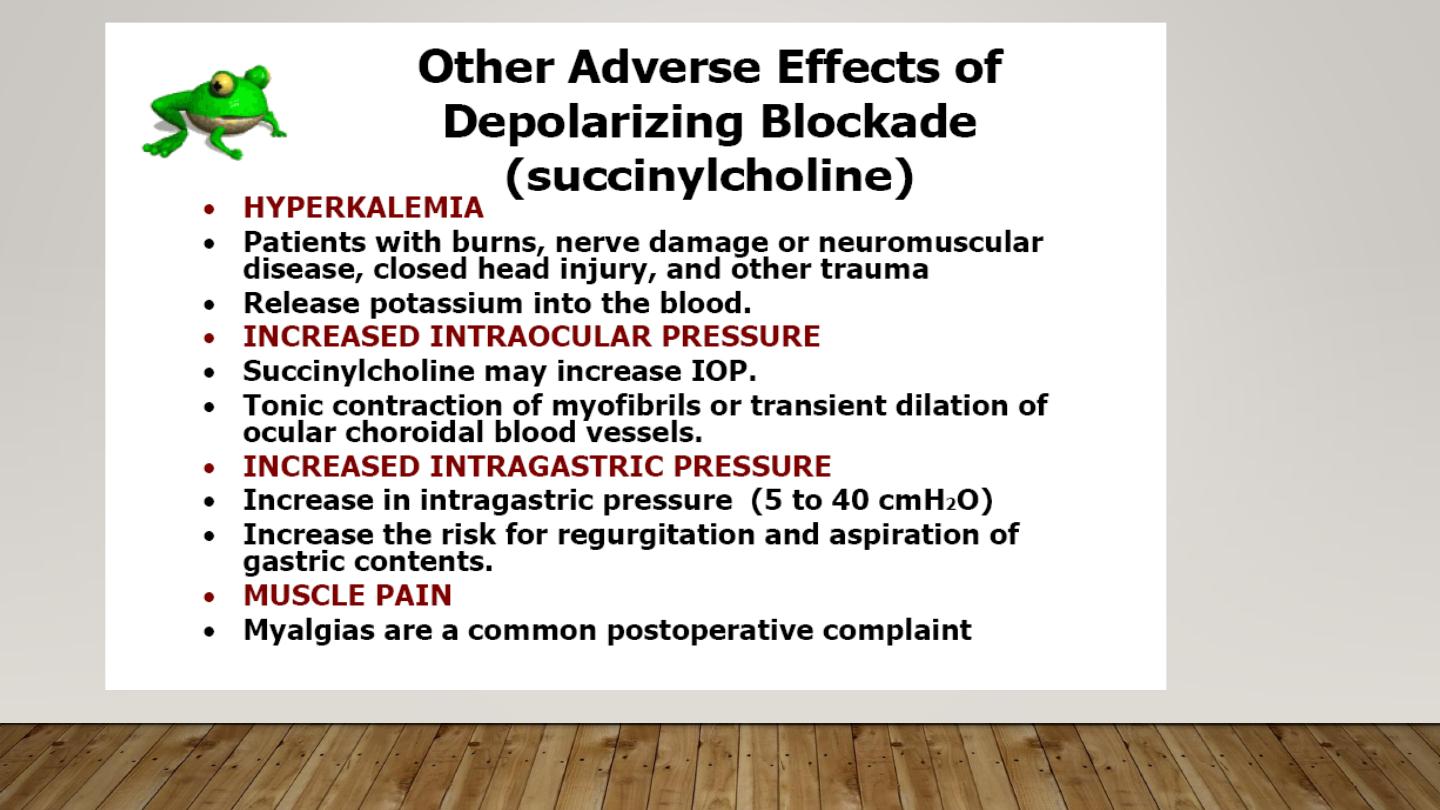
Depolarizing Muscle relaxants:
Succinylcholine (short acting)
Non-depolarizing Muscle relaxants
:
Short acting:
Mivacurium
Intermediate
–acting:
Atracurium,
Cisatracurium,
Vecuronium,
Rocuronium
Long acting :
Doxacurium
Pancuronium
Pipecuronium
MECHANISM OF ACTION
Depolarizing Muscle relaxants
•
Block transmission by causing prolonged depolarization of endplate
at neuromuscular junction.
•
Manifestation by initial series of muscle twitches (fasciculation)
followed by flaccid paralysis.
•
It immediately metabolize in plasma by Pseudocholinesterase
which is synthesized by liver so to prevent its metabolism in plasma it
should be given at faster rate.
S
YSTEMIC EFFECTS
Cardiovascular: Produces muscarinic effects as
acetylcholine , therefore causes bradycardia ( but when
given high doses causes tachycardia because of
stimulation of nicotinic receptors at sympathetic
ganglions.)
Hyperkalemia: Occurs due to excessive muscle
fasciculations. Ventricular fibrillation can occur due to
hyperkalemia.
CNS: Increases intracranial tension ( due to contraction
of neck vessels)
Eye: Increases intraocular pressure
GIT: Increases intra-gastric pressure , salivation, peristalsis.
Muscle pains ( myalgia): This is a very common problem in
post operative period. These are due to excessive muscle
contractions.
Malignant hyperthermia
Severe Anaphylaxis
Masseter Spasm : Sch can cause masseter spasm
especially in children & patients susceptible for malignant
hyperthermia.
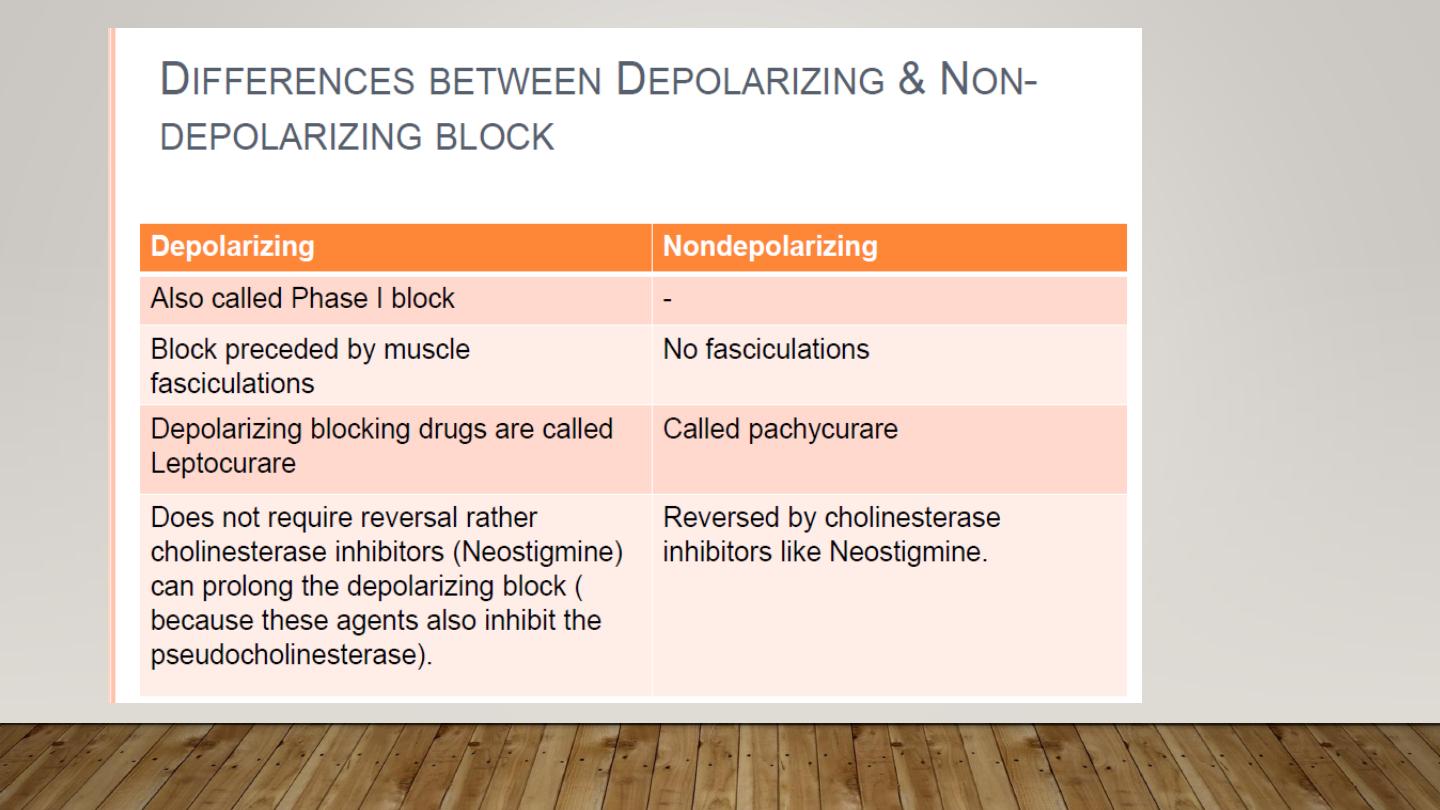
Doesnot require reversal rather cholinesterase inhibitors
(neostigmine) can prolong the depolarizing block (because
these agents also inhibits the pseudocholinesterase)
N
ON
-
DEPOLARIZING
M
USCLE
RELAXANTS
:
Mechanism of action:
•
It blocks nicotinic receptors competitively resulting
in inhibition of sodium channels and excitatory postsynaptic
potential.
•
It binds at the same site at which acetylcholine
binds.
•
All NDMR are quarternary ammonium compounds
& highly water soluble i.e. hydrophilic. So, they do
not cross blood brain barrier & placenta except
Gallamine.
BROAD CLASSIFICATION
These are broadly divided into steroidal
compounds and benzylisoquinoline (BZIQ) compunds.
STEROIDAL COMPOUNS: (vagolytic properties)
It includes PANCURONIUM,VECURONIUM ,
PIPECURONIUM,ROCURONIUM,
RAPACURONIUM,DOXACURIUM
BZIQ(Benzylisoquinoline): (hystamine realease)
It includes d-Tubocurare, Metocurine, Doxacurium,
Atracurium, Mivacurium, Cisatracurium
OTHERS includes Gallamine, Alcuronium
NDMR
ARE USED IN ANAESTHESIA FOR
:
Maintenance of anaesthesia.
For intubation where succinylcholine is contraindicated (
Rocuronium is of choice)
For precurarization to prevent postoperative myalgias by
succinylcholine.
STEROIDAL COMPOUNDS
Pancuronium
Very commonly used as it is inexpensive.
It releases noradrenaline & can cause tachycardia & hypertension.
Because of this there are increased chances of arrhythmia with
halothane
Pipercuronium
It is a pancuronium derivative with no vagolytic activity, so cardiovascular
stable, slightly more potent
Vercuronium
It is very commonly used now a days. It is cardiovascular stable. Shorter
duration of action.
It is the muscle relaxant of choice in cardiac patient.
Rocuronium
8 times more potent than vecuronium and it also has earlier onset of
action
Because of onset comparable to succinylcholine it is suitable for rapid
sequence intubation as an alternative to succinylcholine.
B
ENZYLISOQUINOLINE COMPOUNDS
D- Tubocurare
It is named so because it was carried in bamboo
tubes &
used as arrow poison for hunting by Amazon people.
It has highest propensity to release histamine
It causes maximum ganglion blockade. Because
of
ganglion blocking & histamine releasing property it
can
produce severe hypotension.
Due to histamine release it can produce severe
bronchospasm.
REVERSAL OF BLOCK
Drugs used for reversal of block are cholinesterase inhibitors
(anticholinesterases).
Reversal should be given only after some evidence of
spontaneous recovery appear.
Mechanism of Action
It inactivate the enzyme acetylcholinesterase which is
responsible for break down of actetylcholine, thus increasing
the amount of acetylcholine available for competition with non
depolarizing agent thereby re-establishing neuromuscular
transmission.
Anticholinesterases used for reversal are:
Neostigmine
Pyridostigmine
Edrophonium
Physostigmine
F
ACTORS
P
ROLONGING THE NEUROMUSCULAR
BLOCAKDE
Neonates
Old age
Obesity
Hepatic disease (both depolarizer & NMDR)
Renal disease ( only NDMR)
Inhalational agents : Prolong the block by both
depolarizers & NDMR. Inhalational agents decrease the
requirement of relaxant .The maximum relaxation is by
ether followed by desflurane
Antibiotics: Both depolarizers & NMDR
Aminoglycosides.
Tetracyclines.
Local Anaesthetics : Except procaine local anaesthetics
prolong the action by stabilizing post synaptic membrane.
Hypothermia : Decreases metabolism of muscle relaxants.
Hypocalcemia: Calcium is required for producing action
potential. Action of NDMR is enhanced.
Hypokalemia : NMDR block is enhanced.
Acid base imbalances especially acidosis.
Calcium channel blockers
Dantrolene
Neuromuscular disease
Hypermagnesemia.
D
RUGS WHICH ANTAGONISE
N
EUROMUSCULAR
B
LOCKADE
They reverse the block by NDMR only
Phenytoin
Carbamazepine
Calcium
Cholinesterase inhibitors
Azathioprine
Steroids.
D
RUGS WITH ANTICHOLNERGIC ACTION
ANTIHISTAMINES (H-1 BLOCKERS)
Chlorpheniramine
Cyproheptadine
Diphenhydramine
Hydroxyzine
CARDIOVASCULAR MEDICATIONS
Furosemide
Digoxin
Nifedipine
Disopyramide
ANTIDEPRESSANTS
Amoxapine
Amitriptyline
Clomipramine
Desipramine
Doxepin
Imipramine
Nortriptyline
Protriptyline
Paroxetine
GASTROINTESTINAL
MEDICATIONS
Antidiarrheal Medications
Diphenoxylate
Atropine
Antispasmodic
Medications
Belladonna
Clidinium
Chlordiazepoxide
Dicyclomine
Hyoscyamine
Propantheline
Antiulcer Medications
Cimetidine
Ranitidine
ANTIPSYCHOTIC
MEDICATIONS
Chlorpromazine
Clozapine
Olanzapine
Thioridazine
MUSCLE RELAXANTS
Cyclobenzaprine
Dantrolene
Orphenadrine
URINARY
INCONTINENCE
Oxybutynin
Probantheline
Solifenacin
Tolterodine
Trospium
ANTIVERTIGO
MEDICATIONS
Meclizine
Scopolamine
PHENOTHIAZINE
ANTIEMETICS
Prochlorperazine
Promethazine
N
EWER ANTICHOLINERGICS
Umeclinidium bromide:
An anticholinergic drug approved for use in
combination with vilanterol (as umeclidinium
bromide/vilanterol) for the treatment of COPD
Aclinidium
An anticholinergic for the long-term management
of
chronic obstructive pulmonary disease (COPD). It
has a much higher propensity to bind to muscarinic
receptors than nicotinic receptors.
FDA approved on July 24, 201
DARIFENACIN
Darifenacin is a medication used to treat urinary
incontinence.
Darifenacin works by blocking the M3 muscarinic
acetylcholine receptor, which is primarily
responsible for bladder muscle contractions.
It thereby decreases the urgency to urinate. It
should not be used in people with urinary retention.
98% bound to plasma proteins
Hepatic metabolism. Primarily mediated by the
cytochrome P450 enzymes CYP2D6 and
SOLIFENACIN
Solifenacin is a competitive cholinergic
receptor antagonist.
The binding of acetylcholine to these receptors,
particularly the M
3
receptor subtype, plays a critical role
in the contraction of smooth muscle.
By preventing the binding of acetylcholine to these
receptors, solifenacin reduces smooth muscle tone in
the bladder, allowing the bladder to retain larger
volumes of urine and reducing the number of micturition,
urgency and incontinence episodes.
Because of a long elimination half life, a once-a-day
dose can offer 24 hour control of the urinary
bladder smooth muscle tone
.
THANK YOU
