UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRYBy :Dr Ali Moayid
2020-2021
Department of
Conservative Dentistry
5th YEARs
Pulpal AND PERIAPICAL pathosisNormal Pulp
This is a clinical diagnostic category in which the pulp is symptom-free and normally responsive to pulp testing.
Teeth with normal pulp do not usually exhibit any spontaneous symptoms. The symptoms produced from pulp tests are mild, do not cause the patient distress, and result in a transient sensation that resolves in seconds.
Radiographically, there may be varying degrees of pulpal calcification but no evidence of resorption, caries, or mechanical pulp exposure. No endodontic treatment is indicated for these teeth.
Pulpitis
This is a clinical and histologic term denoting inflammation of the dental pulp.• clinically described as reversible or irreversible
• and histologically described as acute, chronic, or hyperplasticReversible Pulpitis
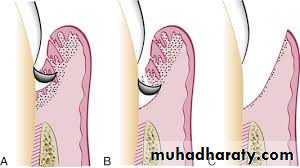
By definition, reversible pulpitis is a clinical condition associated with subjective and objective findings indicating presence of mild inflammation in the pulp tissueInflamed pulp
Normal pulp
Irreversible Pulpitis
Causes: Causative factors include caries, exposed dentin, recent dental treatment, and defective restorations.
incipient caries.
cervical erosion and occlusal (incisal)attrition
most operative procedures
deep periodontal curettagetrauma or orthodontic movement
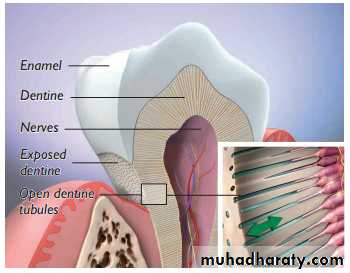
enamel fractures resulting in exposure of dentinal tubules can cause reversible pulpitis.Symptoms
Reversible pulpitis is usually asymptomatic
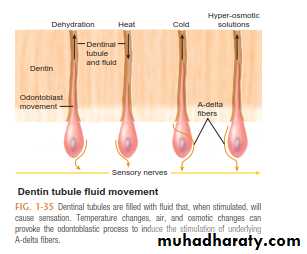
Application of stimuli, such as cold or hot liquids, as well as air, may produce sharp, transient pain. Removal of these stimuli, which do not normally produce pain or discomfort, results in immediate relief.
When heat is applied to teeth with uninflamed pulp, the initial response is delayed; the intensity of pain increases as the temperature rises. In contrast, pain in response to cold in normal pulp is immediate; the intensity tends to decrease if the cold stimulus is maintained. Based on these observations, pulpal responses in both health and disease apparently result largely from changes in intrapulpal pressures.
Treatment
The removal of irritants and sealing and insulating the exposed dentin or vital pulp usually results in diminished symptoms and reversal of the inflammatory process in the pulp tissue.
Irreversible Pulpitis
As the disease state of the pulp progresses, the inflammatory condition of the pulp can change to irreversible pulpitis. At this stage, treatment to remove the diseased pulp will be necessary. This condition can be divided into the subcategories of symptomatic and asymptomatic irreversible pulpitis.Symptomatic Irreversible Pulpitis
This is a clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing
Teeth that are classified as having symptomatic irreversible pulpitis exhibit intermittent or spontaneous pain.
Rapid exposure to dramatic temperature changes (especially to cold stimuli) will elicit heightened and prolonged episodes of pain even after the thermal stimulus has been removed
The pain in these cases may be sharp or dull, localized, diffuse or referred
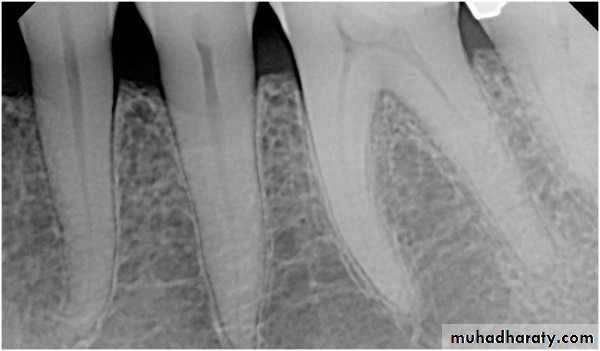
Typically, there are minimal or no changes in the radiographic appearance of the periradicular bone.With advanced irreversible pulpitis, a thickening of the periodontal ligament may become apparent on the radiograph, and there may be some evidence of pulpal irritation by virtue of extensive pulp chamber or root canal space calcification or even internal resorption
Deep restorations, caries, pulp exposure, or any other direct or indirect insult to the pulp, recently or historically, may be present
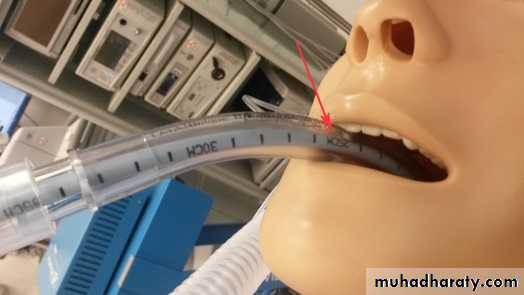
Patients who present with symptomatic anterior teeth for which there are no obvious etiologic factors should be also questioned regarding past general anesthesia or endotracheal intubation procedures.
In addition, patients should be questioned about a history of orthodontic treatment.
Typically, when symptomatic irreversible pulpitis remains untreated, the pulp will eventually become necroticAsymptomatic Irreversible Pulpitis
This is a clinical diagnosis based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing. The patient, however, does not complain of any symptoms. On occasion, deep caries will not produce any symptoms, even though clinically or radiographically the caries may extend well into the pulp.Left untreated, the tooth may become symptomatic or the pulp will become necrotic. In cases of asymptomatic irreversible pulpitis, endodontic treatment should be performed as soon as possible so that symptomatic irreversible pulpitis or necrosis does not develop and cause the patient severe pain and distress
Asymptomatic Irreversible Pulpitis
Symptomatic Irreversible Pulpitis
Necrosis
Endodontic
Pulp Necrosis
This is a clinical diagnostic category indicating death of the dental pulp. This condition is subsequent to symptomatic or asymptomatic irreversible pulpitisWhen pulpal necrosis (or nonvital pulp ) occurs, the pulpal blood supply is nonexistent and the pulpal nerves are nonfunctional
After the pulp becomes completely necrotic, the tooth will typically become asymptomatic until such time when there is an extension of the disease process into the periradicular tissues.
With pulp necrosis, the tooth will usually not respond to electric pulp tests or to cold stimulation. However, if heat is applied for an extended period of time, the tooth may respond to this stimulus. This response could possibly be related to remnants of fluid or gases in the pulp canal space expanding and extending into the periapical tissues.
Pulpal necrosis may be partial or complete and it may not involve all of the canals in a multirooted tooth
.
Pulp necrosis, in the absence of restorations, caries, or luxation injuries, is likely caused by a longitudinal fracture extending from the occlusal surface and into the pulp
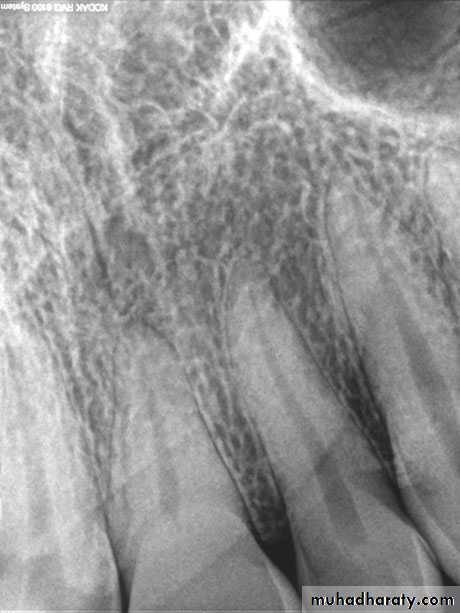
Radiographic changes may occur, ranging from a thickening of the periodontal ligament space to the appear-
ance of a periapical radiolucent lesion
Previously Treated
This is a clinical diagnostic category indicating that the tooth has been endodontically treated and the canals are obturated with various filling materials other than intracanal medicaments. In this situation, the tooth may or may not present with signs or symptoms but will require additional nonsurgical or surgical endodontic procedures to retain the toothPreviously Initiated Therapy
This is a clinical diagnostic category indicating that the tooth has been previously treated by partial endodontic therapy (e.g.,pulpotomy, pulpectomy). In most instances, the partial endodontic therapy was performed as an emergency procedure for symptomatic or asymptomatic irreversible pulpitis cases. In other situations, these procedures may have been performed as part of vital pulp therapy procedures, traumatic tooth injuries, apexification, or apexogenesis therapyAt the time these cases present for root canal therapy it would not be possible to make an accurate pulpal diagnosis because all, or part, of the pulp tissue has already been removed.
PULPAL CALCIFICATIONS
Calcification of pulp tissue is a common occurrenceIn the coronal pulp, calcification usually takes the form of discrete, concentric pulp stones.
Pulp stones (denticles) range in size from small, microscopic particles often seen in association with the wall of arterioles to accretions that occupy almost the entire pulp chamber.
The cause of pulpal calcification is largely unknown. Calcification may occur around a nidus of degenerating cells, blood thrombi, or collagen fibers. Many authors believe that this represents a form of dystrophic calcification
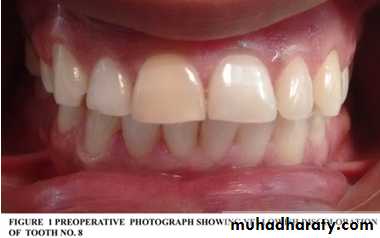
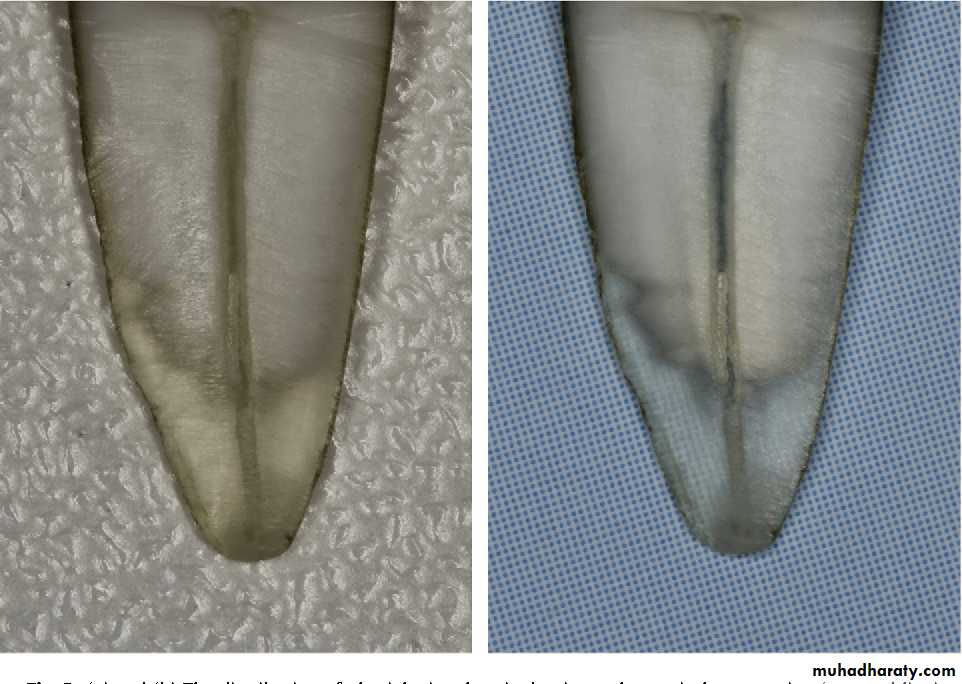
Luxation of teeth as a result of trauma may result in calcific metamorphosis, a condition that can, in a matter of
months or years, lead to partial or complete radiographic obliteration of the pulp chamber. The cause of radiographic obliteration is excessive deposition of mineralized tissue resembling cementum or, occasionally, bone on the dentin walls, also referred to as internal ankylosis
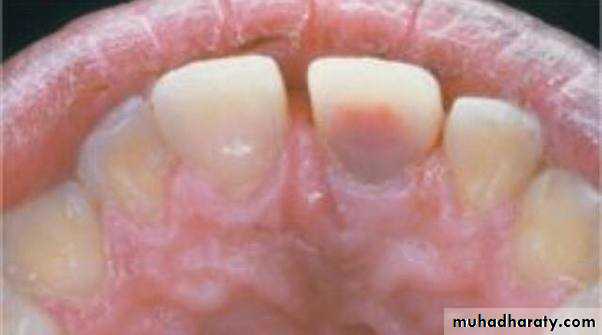
Clinically, the crowns of teeth affected by calcific metamorphosis may show a yellowish hue compared with adjacent normal teeth.
prophylactic intervention does not seem to be warranted.
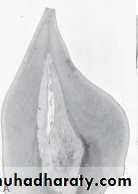
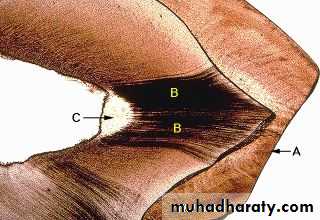
Internal (Intracanal) Resorption
The pulp is transformed into a vascularized inflammatory tissue with dentinoclastic activity; this condition leads to the resorption of the dentinal walls, advancing from its center to the peripheryMost cases of intracanal resorption are asymptomatic. Advanced internal resorption involving the pulp chamber is often associated with pink spots in the crown.
Teeth with intracanal resorptive lesions usually respond within normal limits to pulpal and periapical tests.
Radiographs reveal presence of radiolucency with irregular enlargement of the root canal compartment
Immediate removal of the inflamed tissue and completion of root canal treatment are recommended; these lesions tend to be progressive and eventually perforate to the lateral periodontium.
AGE CHANGES IN THE PULP
Continued formation of secondary dentin throughout life gradually reduces the size of the pulp chamber and root canals.There is a gradual decrease in the cellularity and a concomitant increase in the number and thickness of collagen fibers
The odontoblasts decrease in size and number and they may disappear altogether in certain areas of the pulp,
particularly on the pulpal floor over the bifurcation or trifurction areas of multirooted teeth
With age there is a progressive reduction in the number of nerves and blood vessels
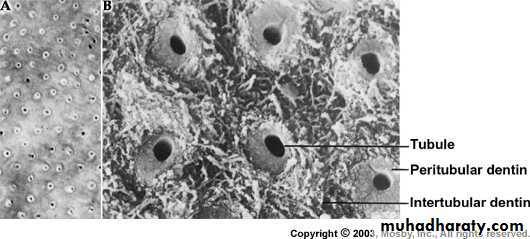
The main changes in dentin associated with aging are an increase in peritubular dentin, dentinal sclerosis, and the number of dead tracts. * Dentinal sclerosis produces a gradual decrease in dentinal permeability as the dentinal tubules become progressively reduced in diameter
Apical (Periapical) Disease
Normal Apical TissuesIn this category the patient is asymptomatic and the tooth responds normally to percussion and palpation testing. The radiograph reveals an intact lamina dura and periodontal ligament space around all the root apices.
Periodontitis
This classification refers to an inflammation of the periodontium. When located in the periapical tissues it is referred to as apical periodontitis. Apical periodontitis can be subclassified to symptomatic apical periodontitis and asymptomatic apical periodontitis
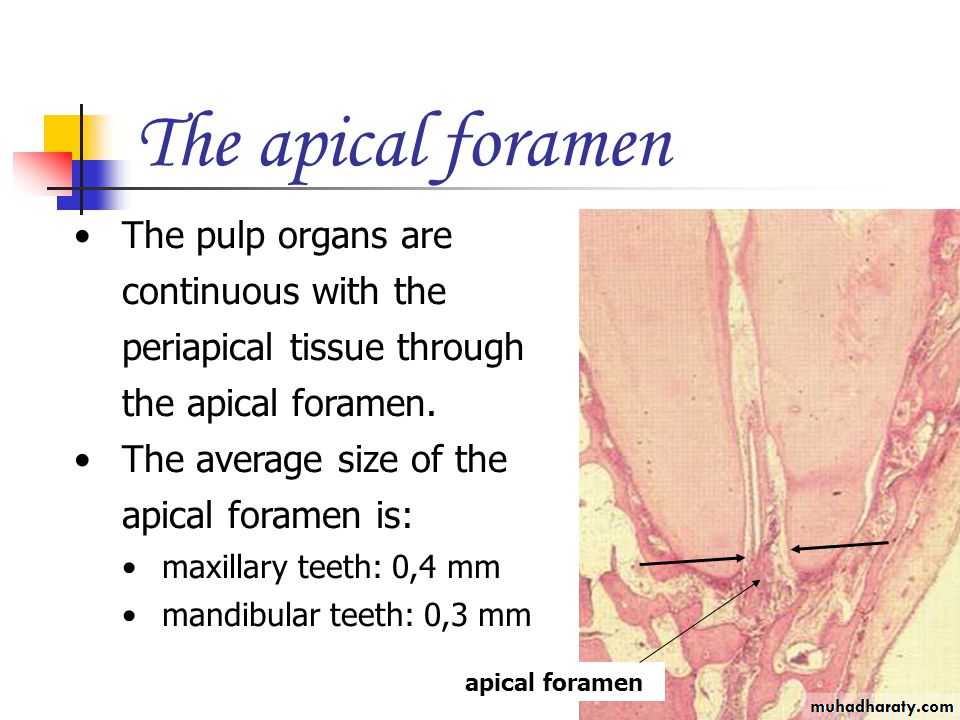
Apical Tissues Anatomical and Histological Background
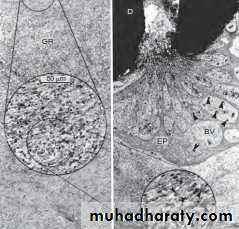
Periradicular tissues consist of cementum, periodontal ligament, and alveolar boneCementum is a mineralized, avascular connective tissue and consists of three different types. Many growth factors, such as insulin-like growth factor-1 (IGF-1), fibroblast growth factors (FGFs), epidermal growth factor (EGF), bone morphogenetic proteins (BMPs), transforming growth factor- β (TGF- β ), and platelet-derived growth factor (PDGF), are contained in the cementum matrix released under certain conditions and associated with cementoblast proliferation, migration, and differentiation during cementum wound healing
The periodontal ligament is a soft, specialized connective tissue that connects the cementum to the alveolar bone. Periodontal ligament contains heterogeneous cell populations and extracellular matrix (ECM). The cells of the periodontal ligament include osteoblasts, osteoclasts, fibroblasts, epithelial cell rests of Malassez, macrophages, cementoblasts, and undifferentiated mesenchymal cells (stem cells). The ECM of the periodontal ligament consists of collagen fibers, fibronectin, elastin, other noncollagenous proteins, and proteoglycans.
Alveolar bone or alveolar process is that part of bone of the jaws housing the sockets for the teeth. It consists of outer cortical plate, a central spongy or cancellous bone, and bone lining the sockets. Bone matrix contains IGFs, TGF- β , BMPs, FGF, and PDGF.
These growth factors are essential for osteoblast progenitor cell proliferation, migration, and differentiation during bone wound healing
The response of the periradicular tissues to various injuries is similar to that of other connective tissues elsewhere in the body. The response is manifested as an inflammatory reaction regulated by both innate and adaptive immune mechanisms.
the pathologic changes of the periapical tissues in apical periodontitis are usually not directly caused by microbes themselves, but rather by their toxins, noxious metabolic by-products, and disintegrated pulp tissue in the root canal system
Apical inflammation is the periapical tissue reaction to irritants emerging from the root canal system that manifests as vasodilation, increased vascular permeability, and exudation
In contrast, apical infection is due to the physical presence of pathogenic microorganisms in the periapical
tissues that subsequently produce tissue damage
SYMPTOMATIC APICAL PERIODONTITIS
Teeth with acute apical periodontitis are usually symptomatic and painful to bite and percussion which results from mechanical allodynia and hyperalgesia.Radiographic examination usually does not show periapical bone destruction of the involved tooth in acute apical periodontitis, although occasional slight widening of the apical periodontal ligament space and loss of the apical lamina dura of the involved tooth may be present.
Treatment:
If vital, removal of the causative agent(s)
If non vital, Root canal therapy
Outcomes
Depending on the dynamic interaction between host defenses and microbial insults, acute apical periodontitis can result in:(1) restitution of normal periapical tissues if irritants are immediately eliminated by root canal Therapy
, (2) abscess formation if massive invasion of periapical tissues by highly pyogenic bacteria occurs
(3) progression to chronic apical inflammation if irritants continue to persist
Abscess is a focal localized collection of purulent exudate in a tissue or an organ
Abscess begins as a great battle between highly virulent pathogens and an army of neutrophilic leukocytes.The pathogens produce massive toxins to kill neutrophils. As neutrophils attack the pathogens, they secrete lysosomal enzymes that digest not only the dead cells but also some live ones. Many neutrophils die fighting against
pathogens. The resulting purulent fluid is poorly oxygenated and has a low pH.
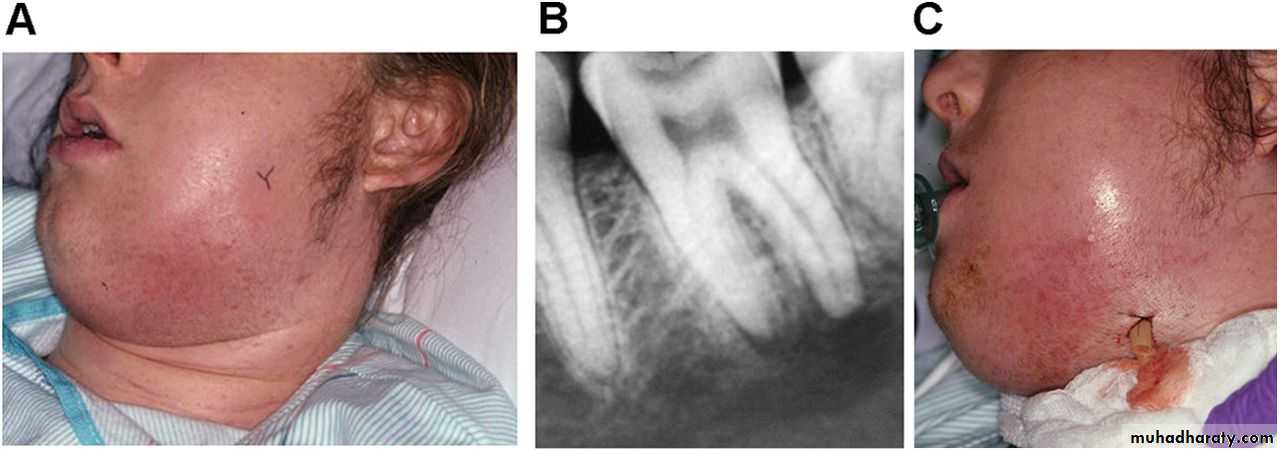
Acute Apical Abscess
Acute apical abscess (AAA) is a localized or diffuse liquefaction lesion of pulpal origin that destroys periradicular tissues and a severe inflammatory response to microbial and nonbacterial irritants from a necrotic pulp.The development of an abscess in apical periodontitis lesions is probably caused by invasion of a combination of specific pyogenic bacteria in the inflamed periapical tissues.