
Achalasia:-
1. What is the meaning of achalasia?
2. How can you diagnose a patient with achalasia?
3. An old patient with long history of GERD present with dysphagia,
what do you think the cause of his condition?
4. How could you manage a patient with CA esophagus?
It is functional obstruction at the level of lower esophageal sphincter due
to:-
1.
Hypertonic lower oesophageal sphincter which fail to relax in
response to the swallowing wave.
2.
Failure of propagated oesophageal contraction, leading to
progressive dilatation of the gullet.
3.
Degeneration of ganglion cell in the muscles of the mid and
lower oesophageal. This abnormal non adrenergic non
cholinergic (NANC) innervations related to abnormal nitric
oxides synthesis with in the lower oesophageal sphincter and the
body of esophagus
4.
Loss of the dorsal vagal nuclei with in the brain stem in the later
stages.

5.
Chagas dis.:-is endemic in South America due to parasite
trypanosome cruzy leads to myocarditis and arrange of motility
disorders of the GIT at various level.
Clinical picture
:-
It is usually developed in middle life but can occur at any age.
Dysphagia develops slowly; it is initially intermittent, worse for solid and
is eased by drinking liquid and by standing and moving around post
eating.
Heart burn doesn’t occur because no GERD can occur. As disease
progress, nocturnal aspiration and severe dysphagia for both solid and
liquid (vigorous achalasia) .
Achalasia is a predisposing factor for CA esophagus rarely as
squamous cell carcinoma.
Investigations:-
1.
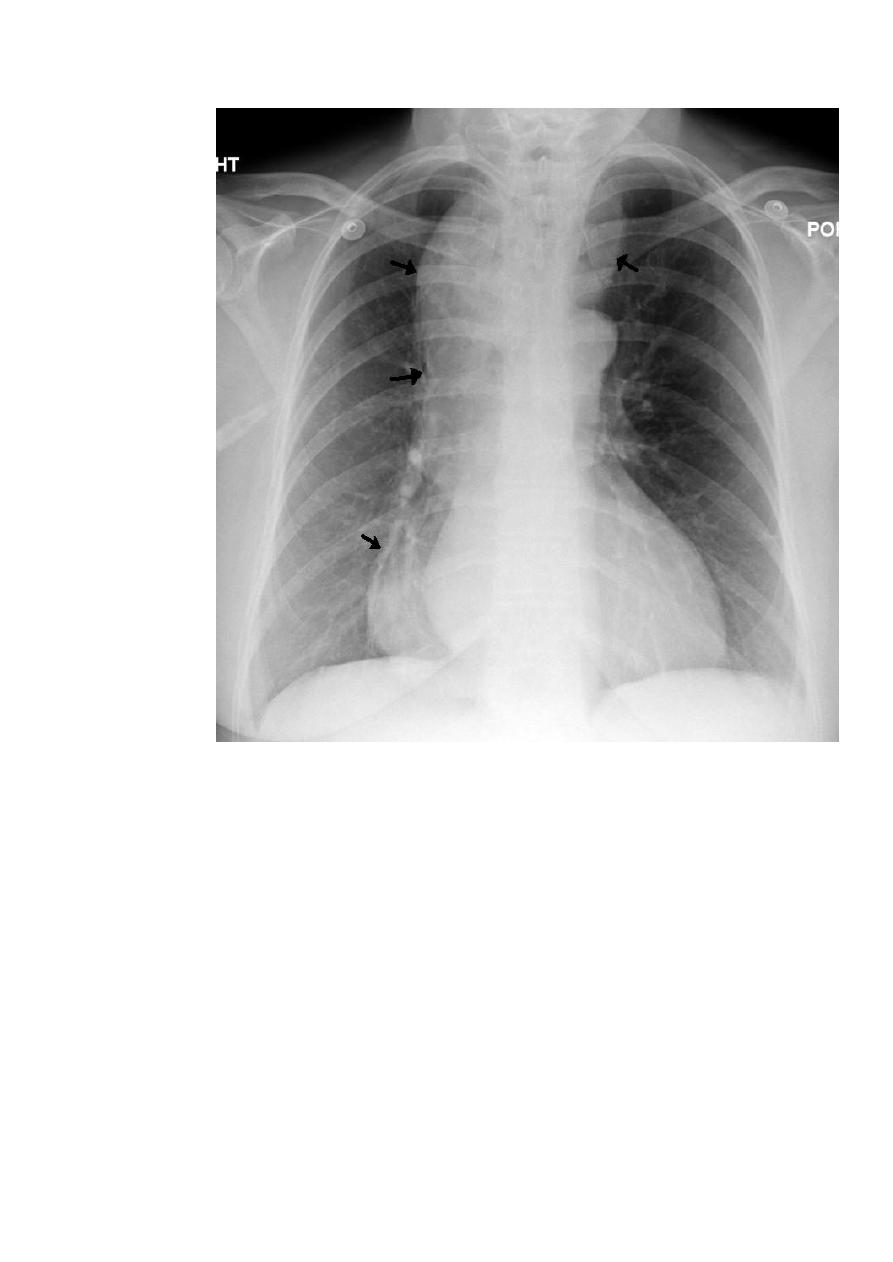
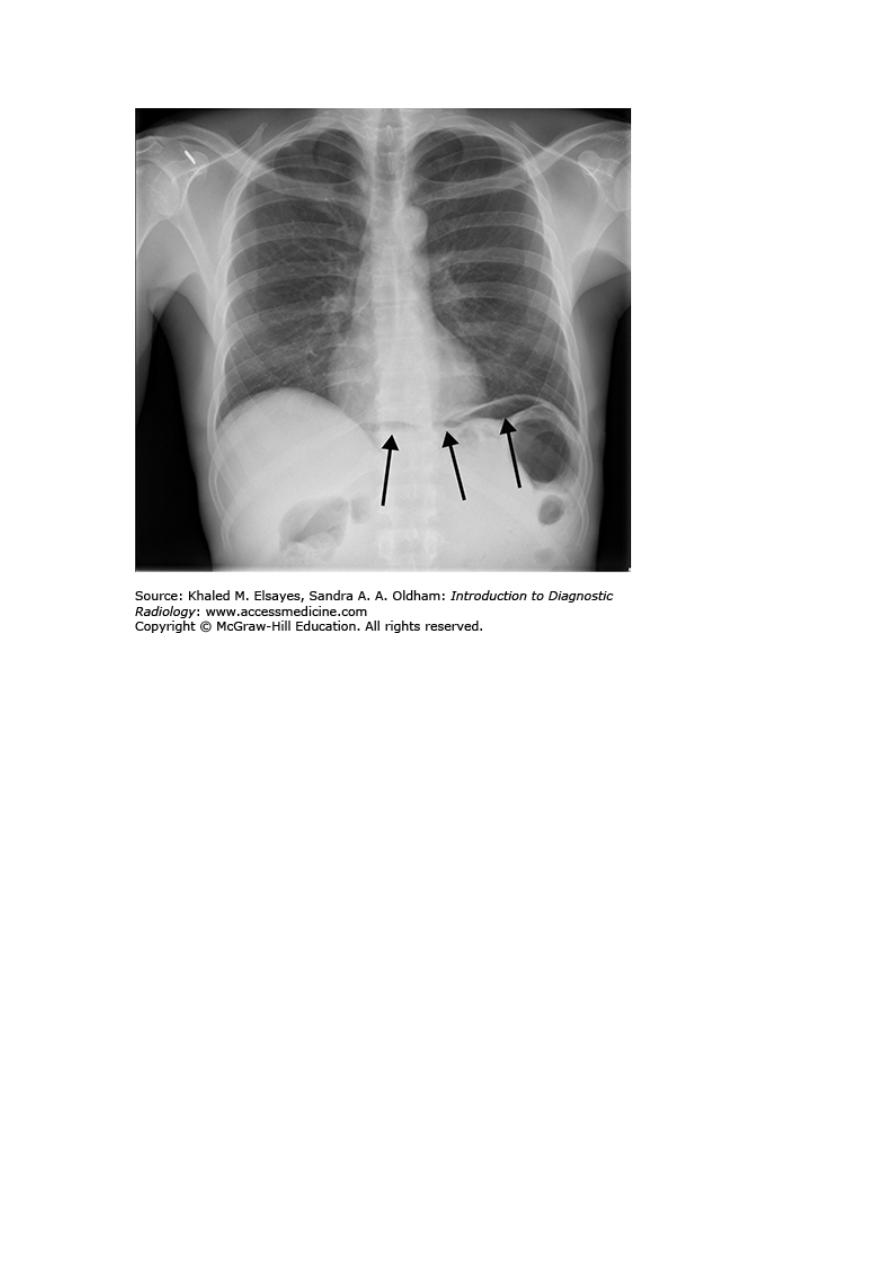
Chest x-ray may be abnormal in late dis., with widening of
mediastinum (oesophageal dilatation) and presence of aspiration
pneumonitis.
2.
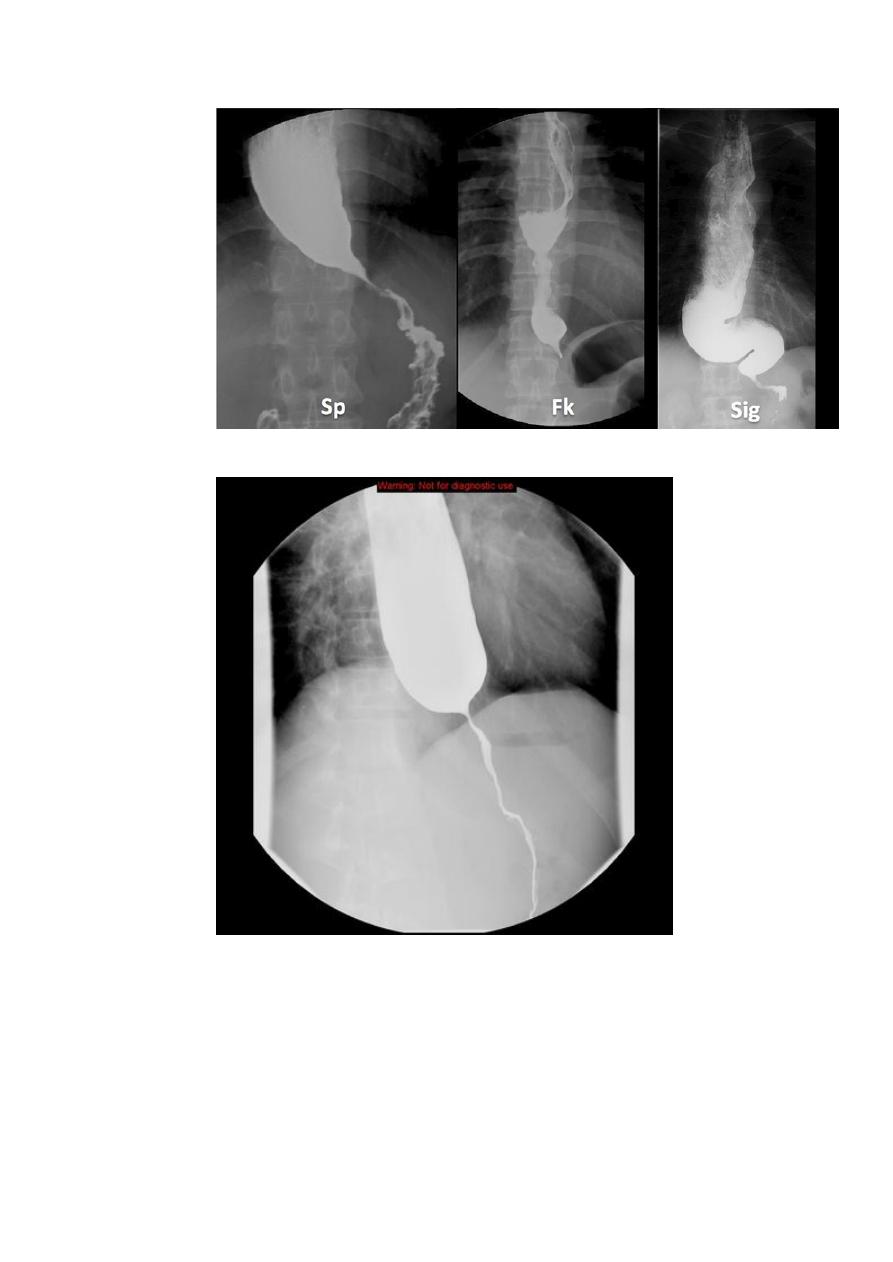
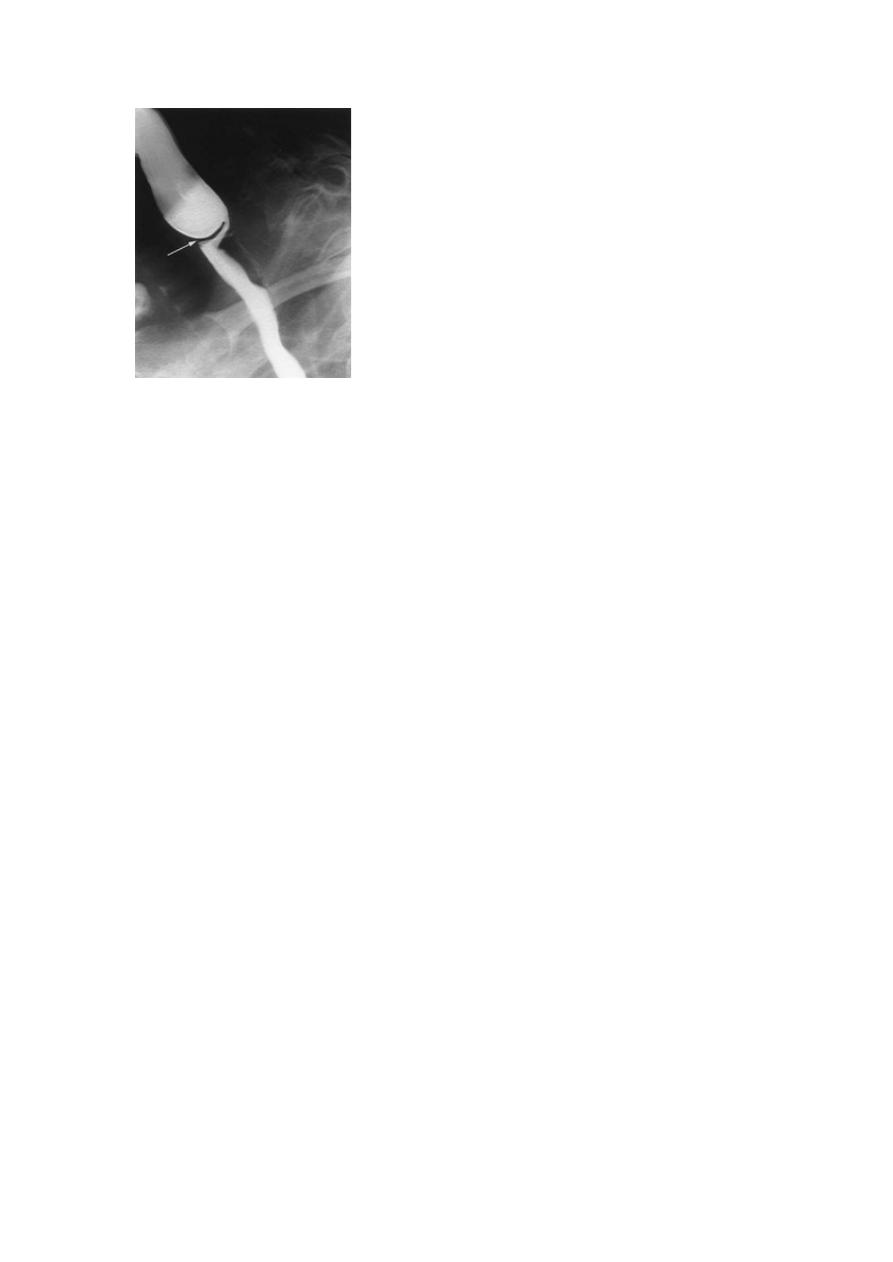
Barium swallows . Tapered narrowing (bird beak) of the lower
oesophagus and dilating body of oesophagus, a peristaltic and
food filled (sigmoid oesophagus).
3.
Endoscope. is a must ,to exclude carcinoma of oesophagus,
which can give (pseudo achalasia) due to the same radiological
4.
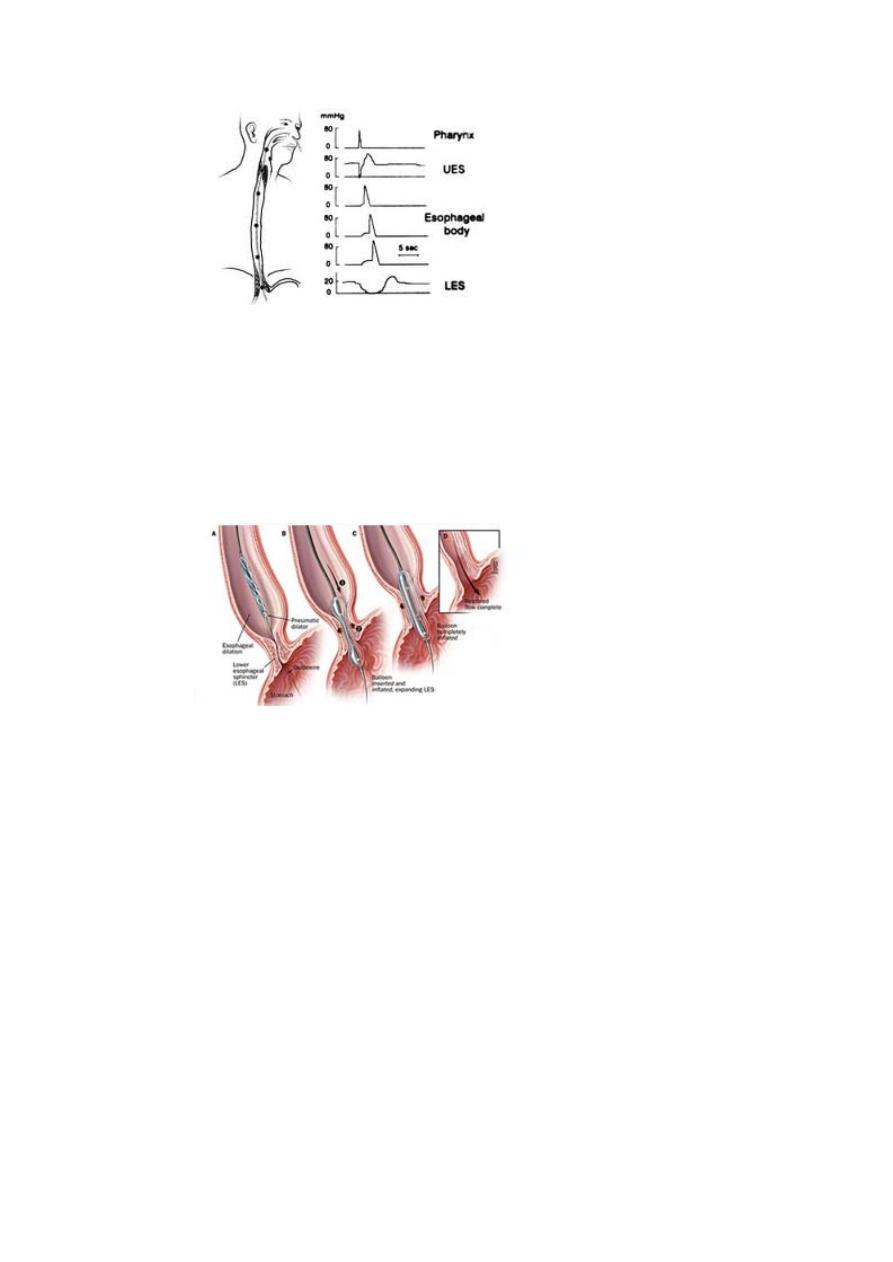
Manometer:-
confirms high pressure , non-relaxing lower
esophageal sphincter ,with poor contractility of the oesophageal
body. The intraoesophageal pressure is higher than the gastric
pressure due to a fluid and food filled oesophagus.
Differential diagnosis:-
1. Chagas dis.
2. pseudo achalasia
3. diffuse oesophageal spasm
4. Scleroderma oesophagus with peptic stricture.
Management:-
1. endoscopically:-
a.
forceful pneumatic dilatation using 30-35 mm diameter
fluoroscopically positioned balloon across the gastro esophageal
junction. It improves the symptoms in 80% of pt. we face two
problems:-
- Perforation of oesophagus in less than 3% may need surgical repair.
- Recurrent achalasia need frequent dilatation may improve with
surgery.
b.
botulinum toxin injection: under endoscope guided procedure to
the lower oesophageal sphincter.
Advantage:
- improvement of symptoms in 85%of pt.
Disadvantage:-
1. Symptoms relapse occur over 50% in 6-9 months although repeated
injections give some improvement.
2. It is not appropriate for elderly with multiple medical problems.
3. it is inferior for pneumatic dilatation and surgery.
Surgery
Hurler’s operation:-either open operation or laparascopically.
a. it improve the symptoms in 85 % of the patients
b. Complicated by GERD in 20%, therefore; partial fundoplication
(antireflux surgery) is done.
c. We need proton pump inhibitor drugs post operatively.
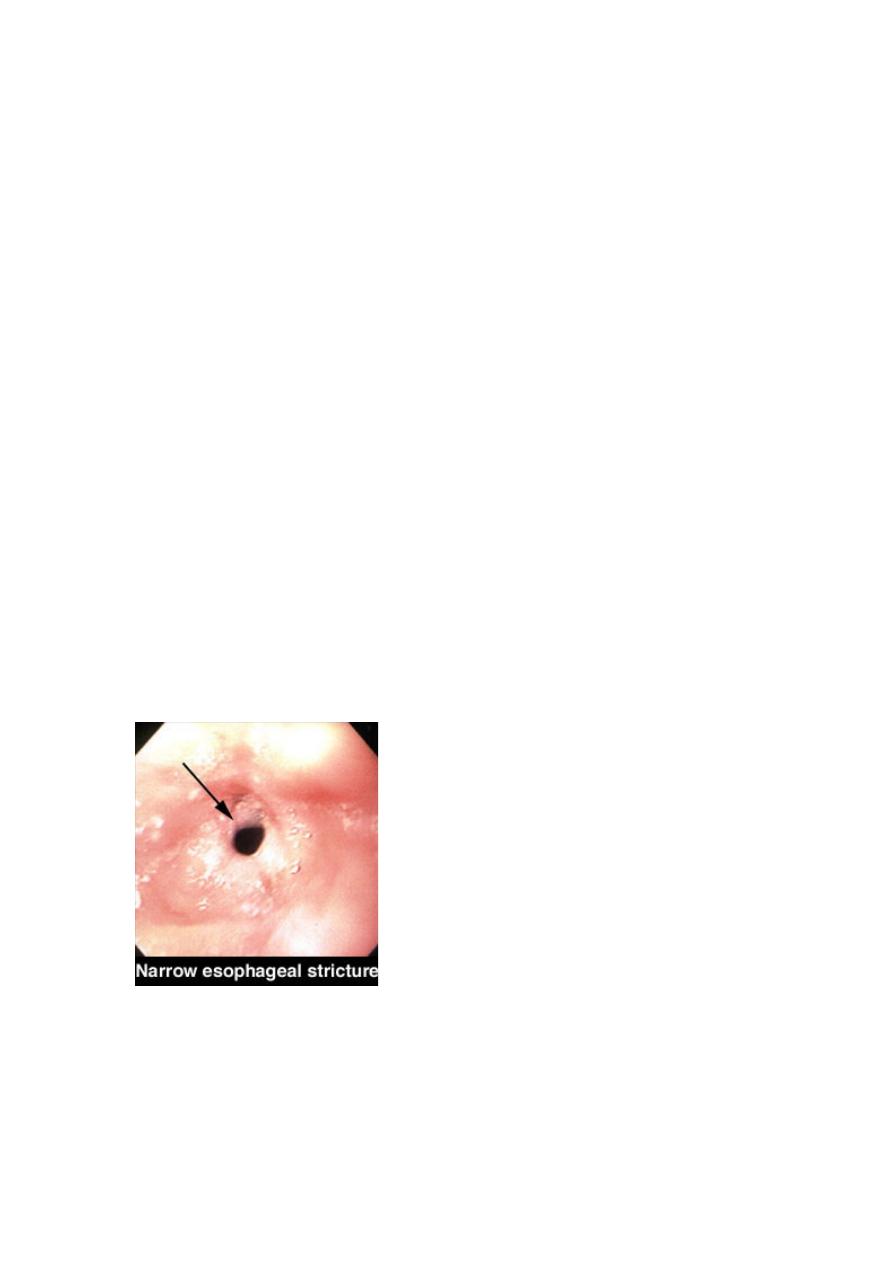
Causes of oesophageal stricture:-
1. GERD
2. webs and ring
3. CA oesophagus and or cardia.
4. Extrinsic compression from CA bronchus.
5. corrosive ingestion
6. post-operative scarring from oesophageal resection
7. post radiotherapy
8. Following long term nasogastric intubations.
Other causes of benign stricture
- GERD, occur in elderly with poor oesophageal clearance.
- Upper oesophageal ring (Plummer –Vinson syndrome) post
cricoids web it is a rare complication of iron deficiency anemia,
may be complicated by squamous cell CA.
- Lower oesophageal web (schatzki ring) causes intermittent
dysphagia often starting in middle age.
- Endoscope and dilatation is treatment of choice +treatment of
original dis.
Oesophageal tumor
Basic classification of esophageal tumor:-
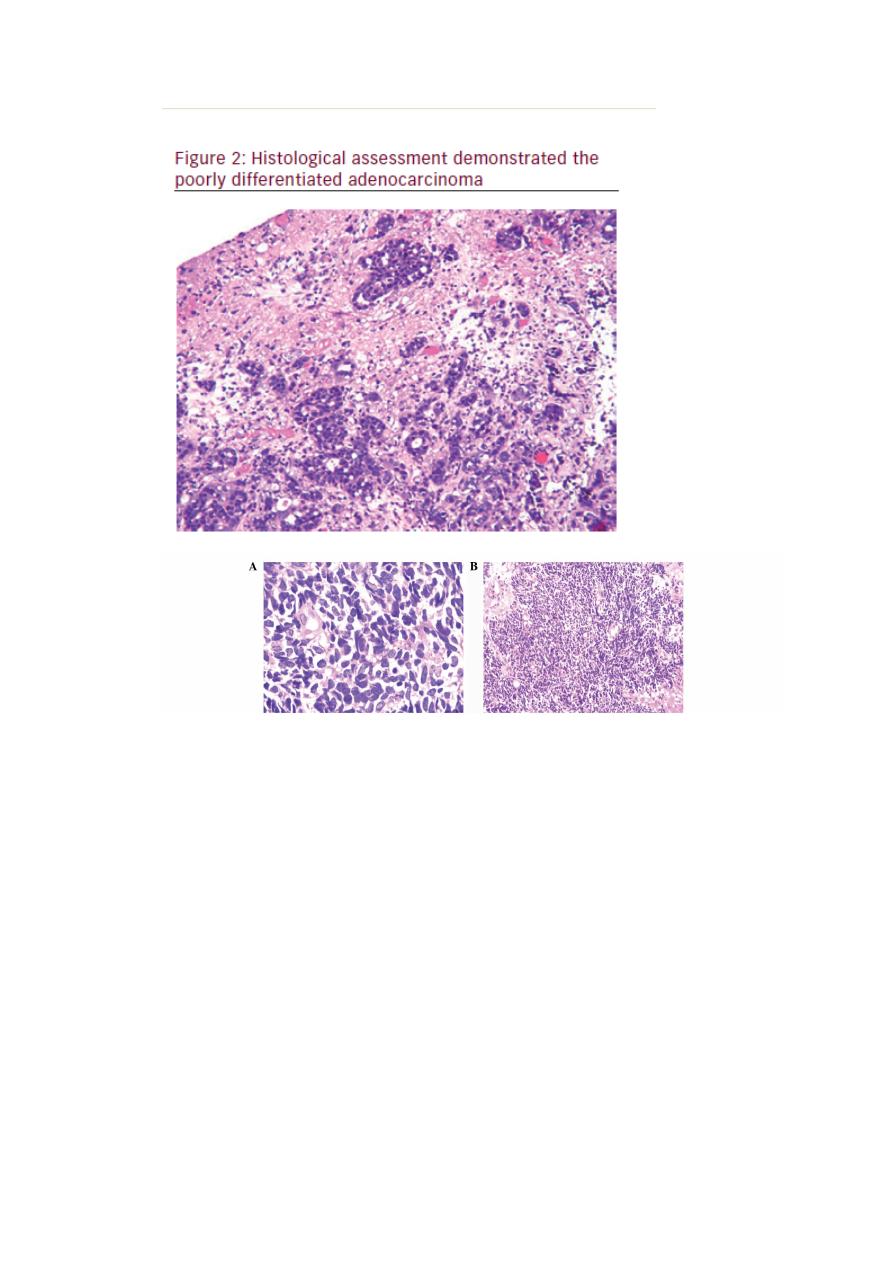
Malignant - squamous cell carcinoma
-adenocarcinoma
- Melanoma
- Sarcoma (rarely leiomyosarcoma)
Benign
Leiomyoma
Adenoma
Cysts
Other said:- almost all are adenocarcinoma or squamous cell
carcinoma ,small cell CA is rare third type.
Squamous cell carcinoma:-
It can occur from the cricoid cartilage to the cardia of the stomach.
Almost all tumors above the lower third of the oesophagus are
squamous cell CA.
Etiology:-
Cigarette smoking, high alcohol intake, celiac dis, radiation, achalasia,
ingestion of strong acids or alkali, environmental carcinogen, and
possible reflux oesophagitis, Plummer-Vinson disease and palmer
hyperkeratosis (tylosis palmaris).
Adenocarcinoma:-
This arises in the lower third of the oesophagus from barrette’s
oesophagus or from the cardia of the stomach.
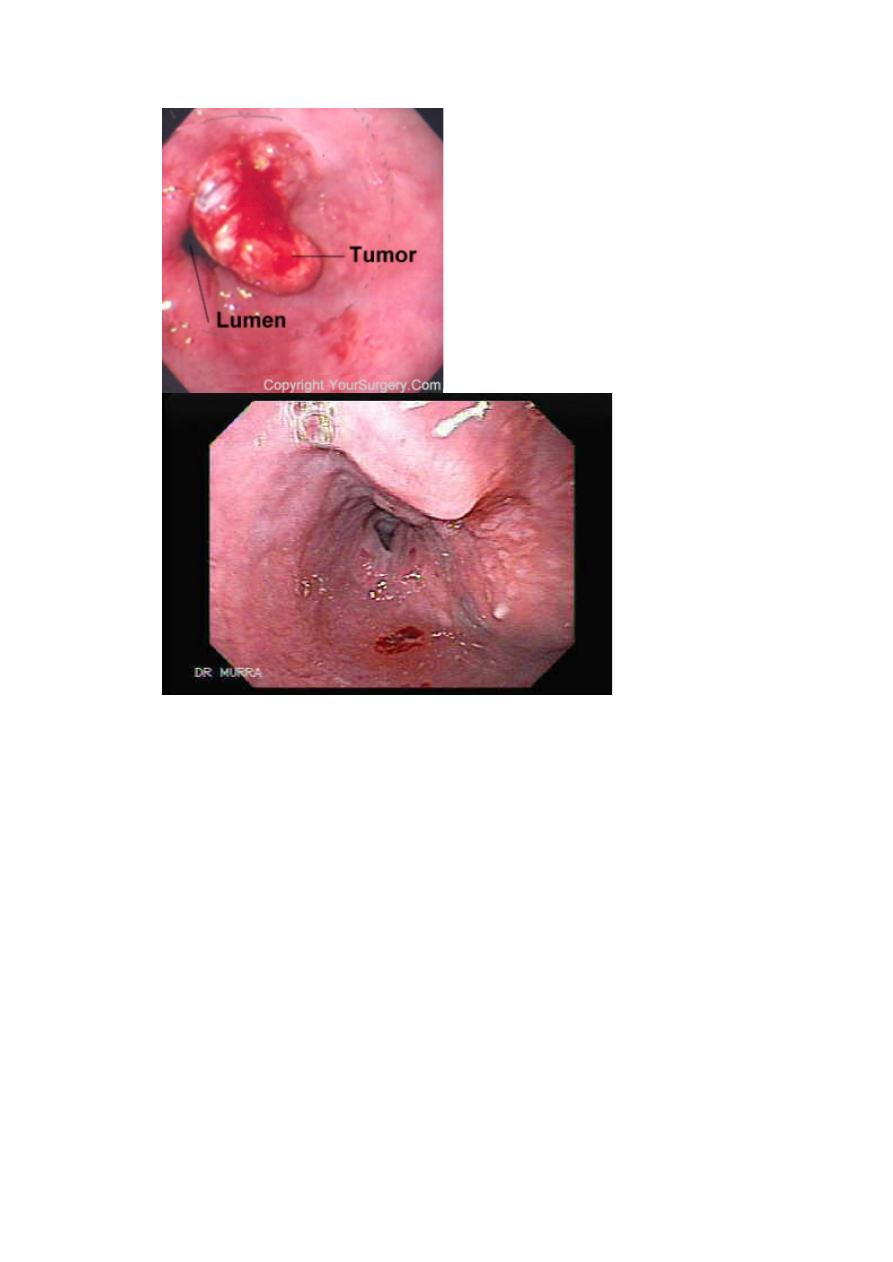
Clinical feature in all types :-
Most patients have a history of painless, progressive dysphagia for
solid food or acutely because of food bolus obstruction. Dysphagia is
usually rapidly progressive. Pain is usually retrosternal and is due to
invasion into the mediastinum (hoarseness is also a symptom).
Productive cough may reflex aspiration pneumonia or Broncho
esophageal fistula (cough after swallowing)
Weight loss is also obvious, anemia usually reflect bleeding or
appetite depression, cervical LAP & hepatomegaly (metastasis) are a
late symptoms.
Investigations
:-
1. OGD
2. barium swallow
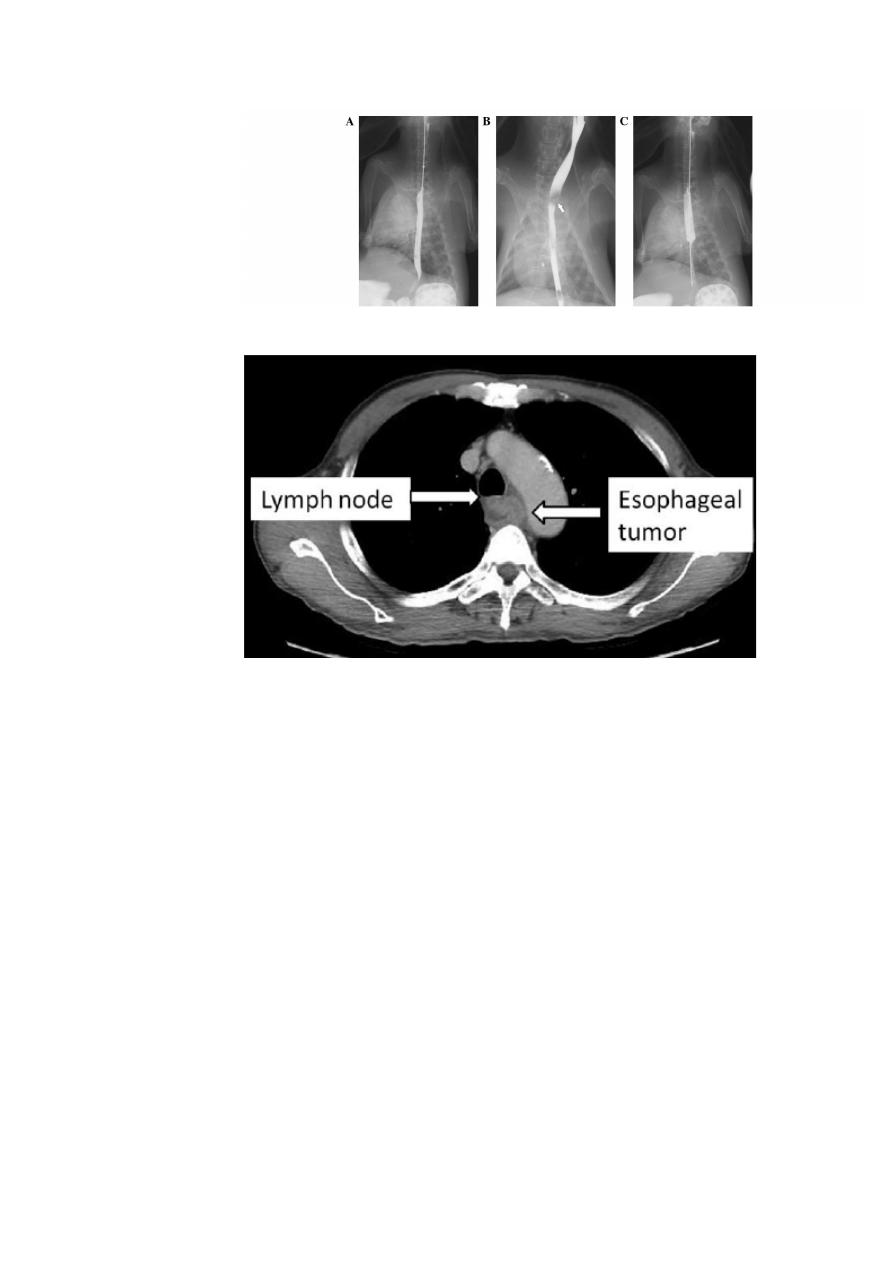
3. Chest x-ray and abdominal u\s to exclude metastatic lesion.
4. CT scan or MRI
5. Endoscope is the most sensitive investigation.
Management:-
Approximately 70% of pt. has extensive dis. At presentation and
treatment only to relief dysphagia and pain (palliative therapy) by:-
1. laser therapy
2. insertion of stent
3. palliative
radiotherapy
to
induce
shrinkage
of
both
adeno :&squamous CA
4. Nutritional support & analgesia.
The over all survival rate is less than 10% 5 years .survival rate depend
on stage of tumor and type of CA. The overall survival following
potential curative surgery (all microscopic tumor removed )is 30%at 5
years. But this can be improved by chemotherapy as cisplatinum and
5flurouracil.
The management of sq. cell CA is controversial because sq.CA is
radiosensitive. Surgery or radical radiotherapy may be effective in
patients who are fit, with no LN involvement or metastasis.
In the upper third, radiotherapy may be the preferred treatment as surgery
is technically difficult procedure.
In the middle and lower third, surgery is preferred to radiotherapy if the
patient is fit enough.
Surgery:-
1. the stomach is mobilized to the chest and anatomized to the
oesophagus in the chest or
2. Colonic mobilization.
Radiation is complicated by oesophagitis and stricture.
- Surgery is complicated by stricture, mediastinitis and anastomotic
leaks.
Perforation of oesophagus
Causes:
- iatrogenic by endoscope OGD either dilatation or intubations
post malignant, corrosive or post radiotherapy stricture which need
surgical therapy.
- Perforated peptic stricture is managed usually conservatively by
antibiotics.
- Spontaneous esophageal perforation (Boerhaave’s syndrome).
Result from forced vomiting.
Clinical picture
:-
Chest pain, shocked subcutaneous emphysema, pleural effusion, and
pneumothorax.
Diagnosis:-
Water soluble contrast swallows CT or OGD under GA.
Treatment:-
Surgery is a must as early as possible.
