Platelet & HemostasisPhysiology Dr. Suroor Mohamed
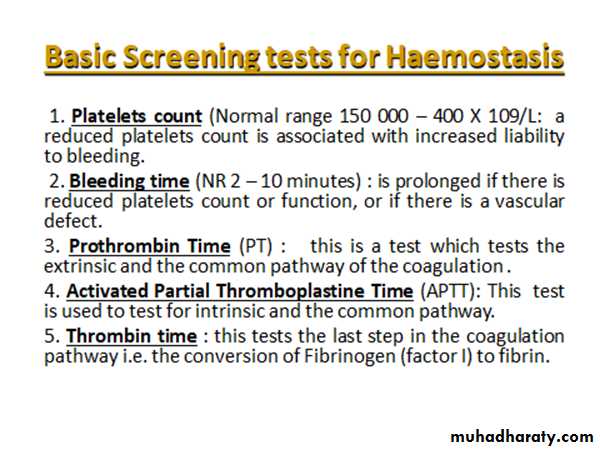
Objectives1-To know the physiological basis about platelets functions.2- What's mean by bleeding & thrombocytopenia terms.3- Describe the mechanism of platelets plug .4- To understand the screening test in bleeding disorder.Platelets (thrombocytes - "clotting")
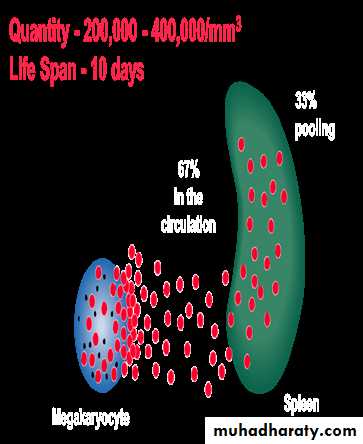
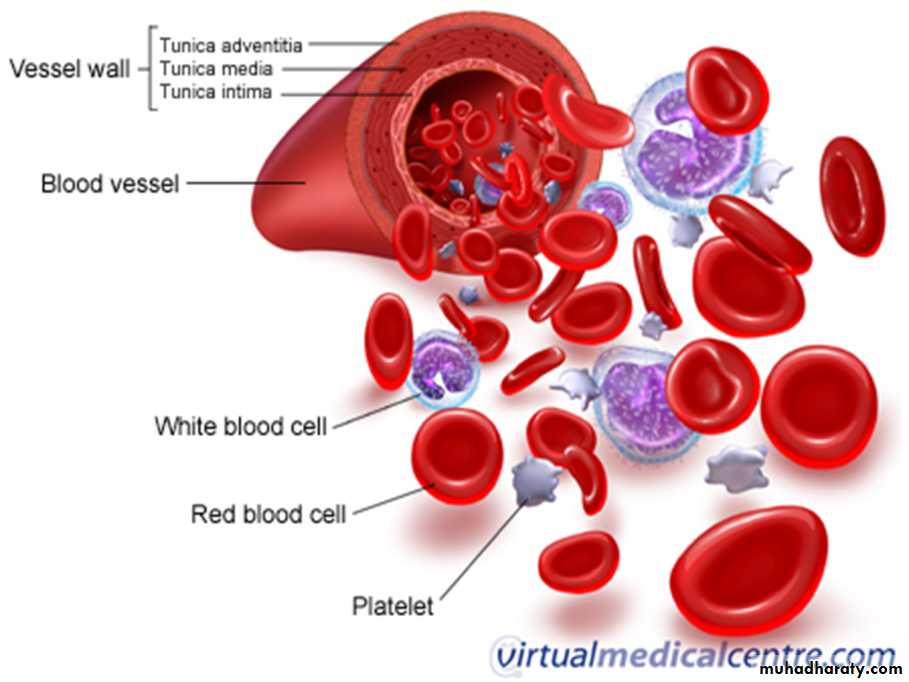
The platelets are small, granulated bodies that aggregate at sites of vascular injury. They lack nuclei and are 2-4 um in diameter . There are about( 150,000- 300,000/uL) of circulating blood, and they normally have a half-life of about 10 days.( 8-12 days).The megakaryocytes, giant cells in the bone marrow, form platelets by pinching off bits of cytoplasm and extruding them into the circulation. Between 60% and 75% of the platelets that have been extruded from the bone marrow are in the circulating blood, and the remainder are mostly in the spleen(1\3).
Splenectomy causes an increase in the platelet count (thrombocytosis).
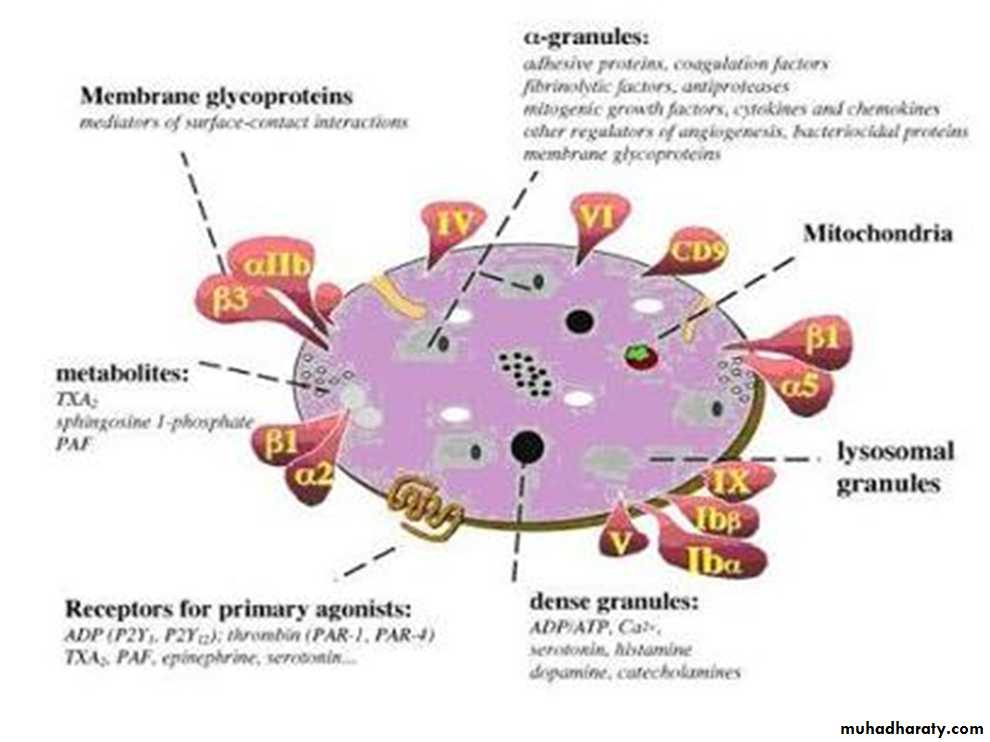
In their cytoplasm are
(1) actin and myosin molecules, which are contractile proteins, thrombosthenin, that can cause the platelets to contract(2) residuals of both the endoplasmic reticulum and the Golgi apparatus that synthesize various enzymes and especially store large quantities of calcium ions
(3) mitochondria and enzyme systems that are capable of forming (ATP) and adenosine diphosphate (ADP)
(4) enzyme systems that synthesize prostaglandins, which are local hormones that cause many vascular and other local tissue reactions
(5) an important protein called fibrin-stabilizing factor
(6) a growth factor that causes vascular endothelial cells, vascular smooth muscle cells, and fibroblasts to multiply and grow, thus causing cellular growth that eventually helps repair damaged vascular walls.
Their membranes contain receptors for collagen, ADP, vessel wall von Willebrand factor . and fibrinogen. Their cytoplasm contains actin, myosin, glycogen, lysosomes, and two types of granules:
Platelet Granules :
** Alpha granules contain:• Clotting factors – fibrinogen, V and XIII
• 2. Platelet-derived growth factor PDGF
• 3. Vascular endothelial growth factor (VEGF)
• 4. Basic fibroblast growth factor (FGF)
• 5. Endostatin
• 6. Thrombospondin.
** Dense granules contain: Adenine
1. Nucleotides “ADP “
2. Serotonin
3. Phospholipid
4. Calcium
5. Lysosomes.
150,000 to 300,000 per microliter
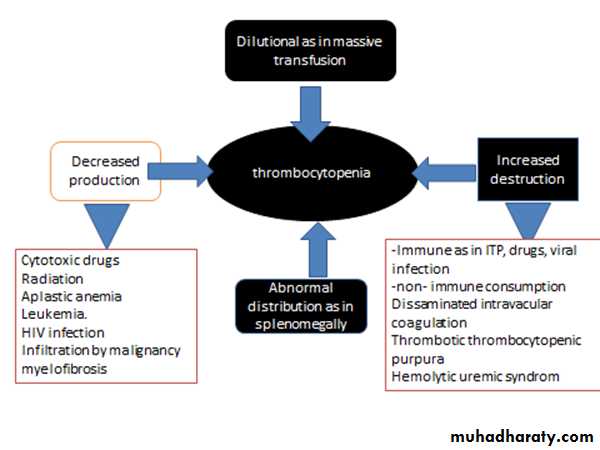
Thrombocytopenia: abnormally low platelet countThrombocytosis: abnormally high platelet count
Low count due to :
Decreased Production
Decreased Survival – Immune (ITP) immune thrombocytopenia
Increased utilization – DIC disseminated intravascular coagulopathy
Defective Platelet function:
Acquired – Drugs – Aspirin, MDS Myelodysplastic syndrome
Congenital – Eg. Thrombasthenia.
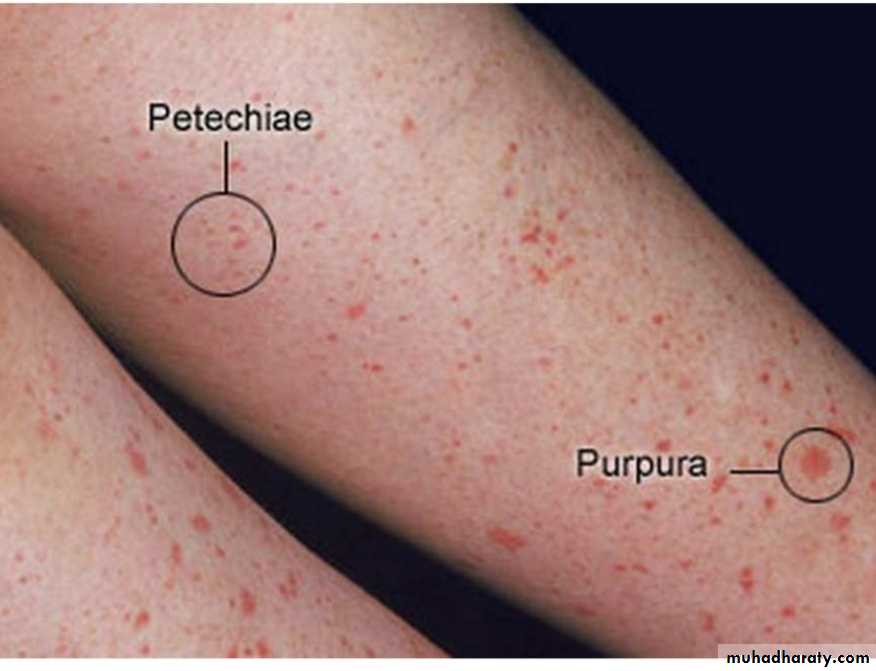
Thrombocytopenic purpura
When the platelet count is low, clot retraction is deficient and there is poor constriction of ruptured vessels. The resulting clinical syndrome (thrombocytopenic purpura) is characterized by easy bruisability and multiple subcutaneous hemorrhages. Purpura may also occur when the platelet count is normal & in state of , the circulating platelets are abnormal (thrombasthenic purpura). Individuals with thrombocytosis (increased number of platelets) are predisposed to thrombotic events.
Petechiae Tiny red spots resulting from blood extravasated from normally healthy blood vessels which have become abnormally permeable (due to a vascular or platelet disorder)
Epistaxis "Nose bleeding" This is usually caused by a mild trauma to the blood vessels of the anterior nares, but occasionally is a manifestation of a platelet or vascular abnormality
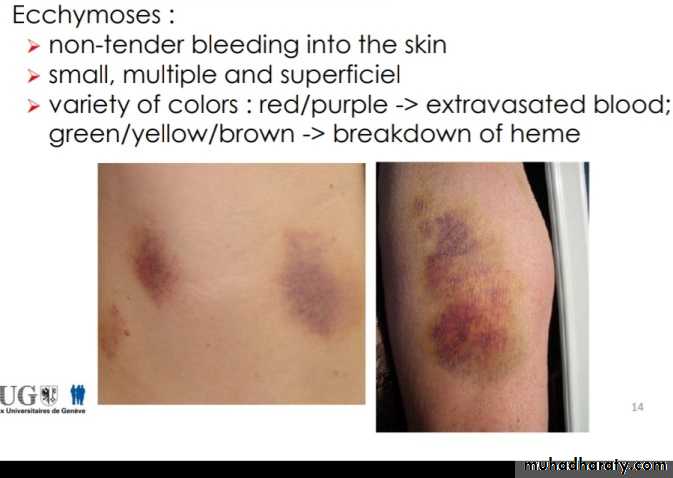
Ecchymosis An area of extravasated blood arising from trauma to the blood vessels of that area. This can also arise in patients with vascular or platelet disorders.
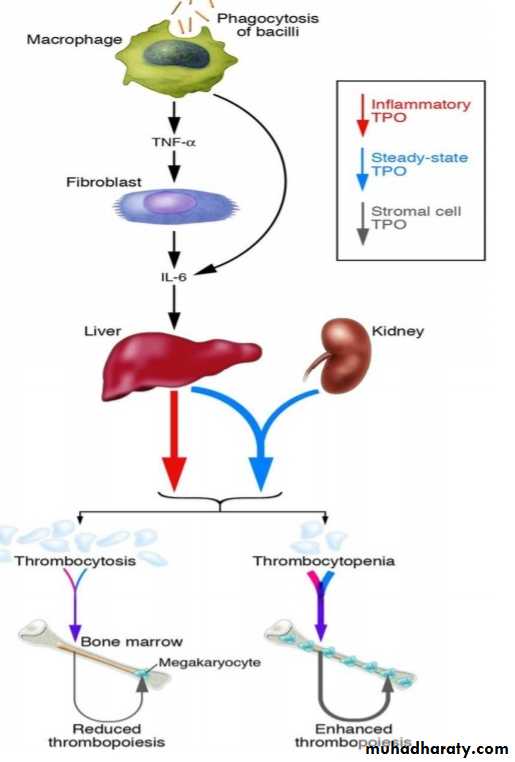
Platelet production is regulated by (Thrombopioesis):
1. colony- stimulating factors that control the production of megakaryocytes.2. Thrombopoietin, a circulating protein
factor which facilitates megakaryocyte
maturation.(TPO)
From the pluripotent stem cells in the bone marrow.
CFU-M “Colony forming megakaryocyte”
Megakaryoblast→→Promegakaryoctye
→Megakaryocytes →PlateletsPlatelets are eliminated from the circulation
mainly by the tissue macrophage system in thespleen( splenomegaly reduced the platelet count).
Normal blood vessel wall Injured vessel
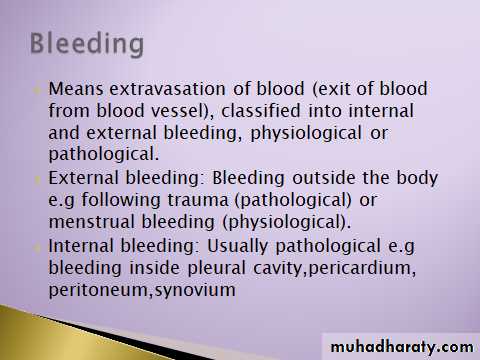
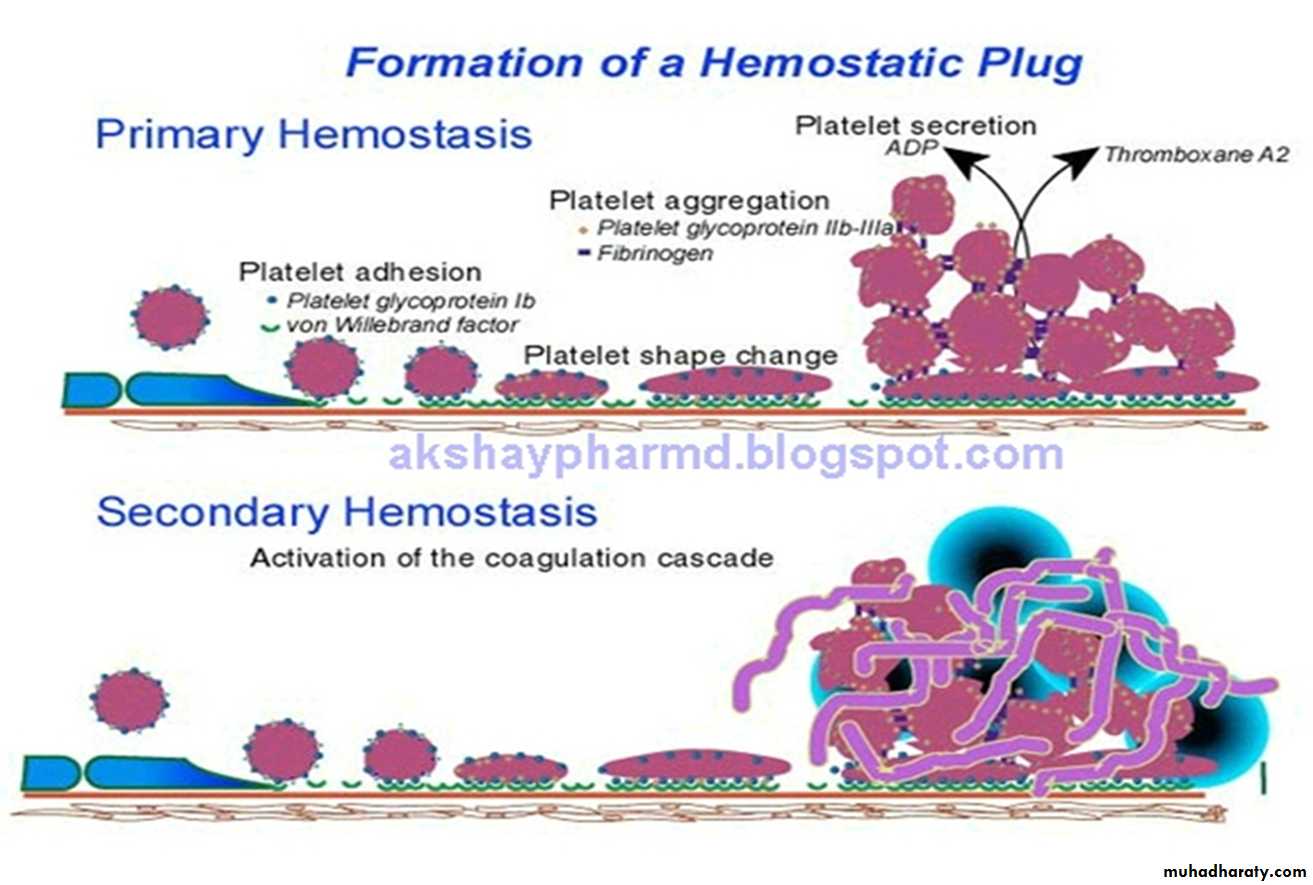
Hemostasis means prevention of blood loss( stoppage of blood flow after damage) .
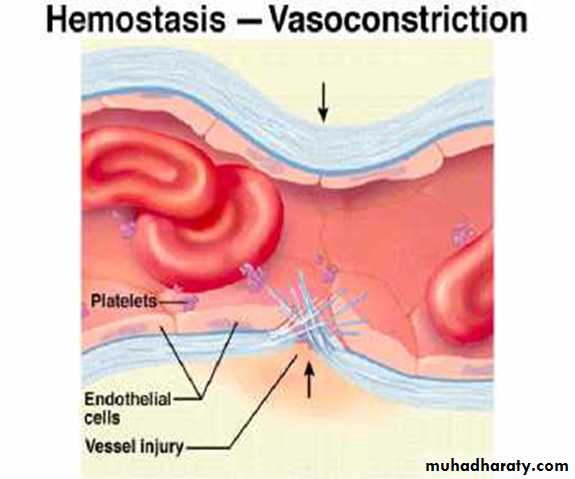
Whenever a vessel is severed or ruptured, hemostasis is achieved by several mechanisms:(1) vascular constriction
(2) formation of a platelet plug
(3) formation of a blood clot as a result of blood coagulation
(4) eventual growth of fibrous tissue into the blood clot to close the hole in the vessel permanently
In ruptured blood vessel
1. Pain impulses from the site of trauma as well as from the surrounding nervous tissue originate and reach the spinal cord.From the spinal cord order signal arise.
The order signals pass through the sympathetic nerves
Lead to spasm of the vessel.
2. Local muscle also contribute to the vascular vasospasm.
3. local autacoid factors from the traumatized tissues and blood platelets.
**Vasoconstriction resulting from local myogenic contraction of the blood vessels is initiated by direct damage to the vascular wall.In the smaller vessels, the platelets are responsible for much of the vasoconstriction by releasing a vasoconstrictor substance, thromboxane A2.
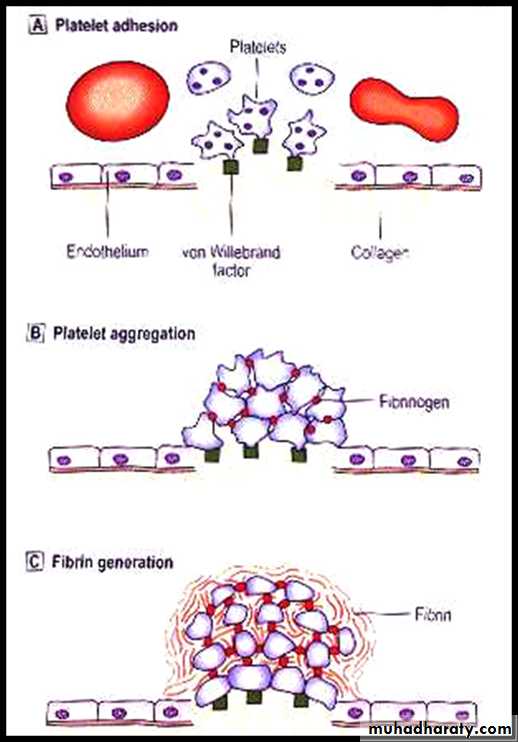
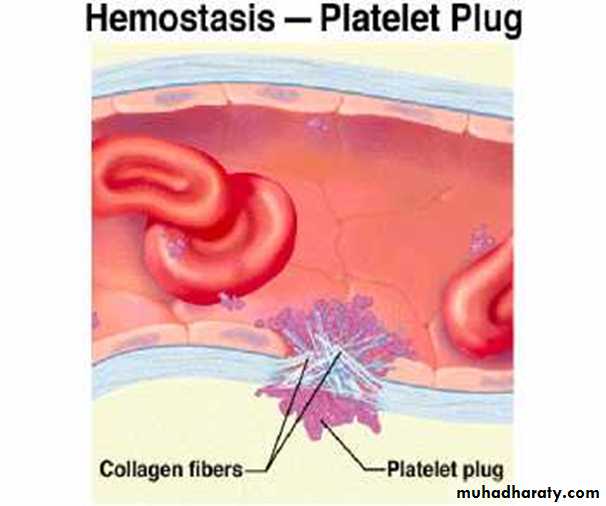
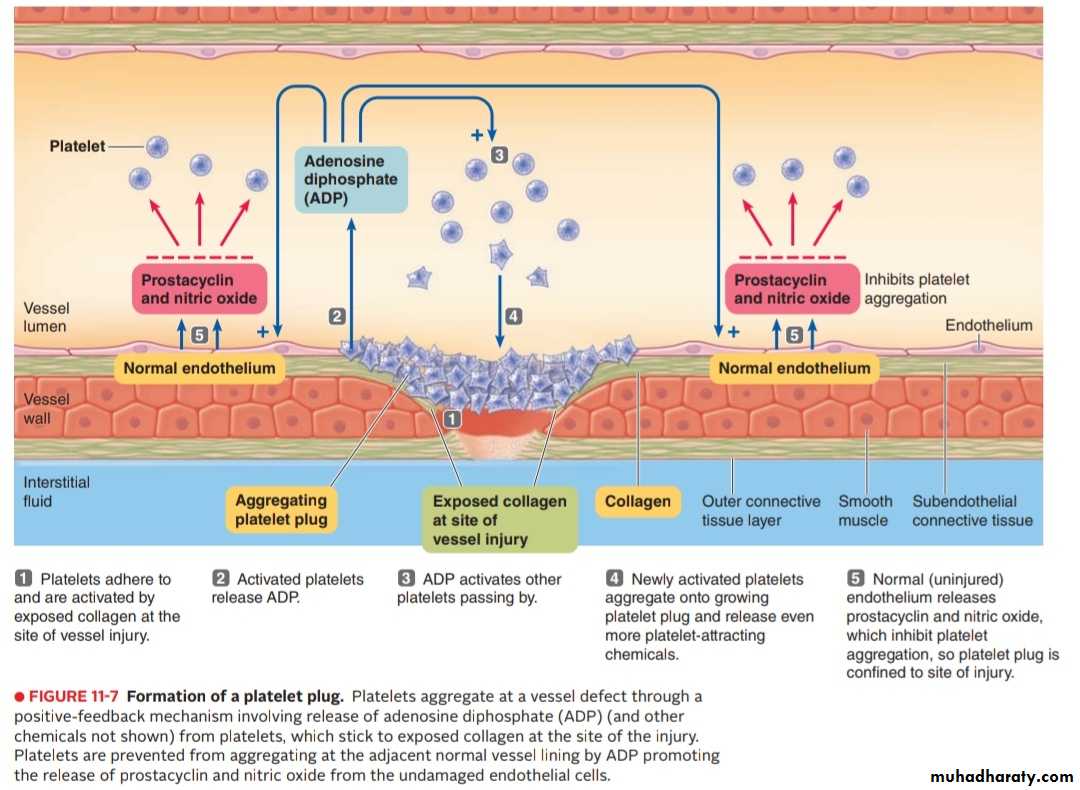
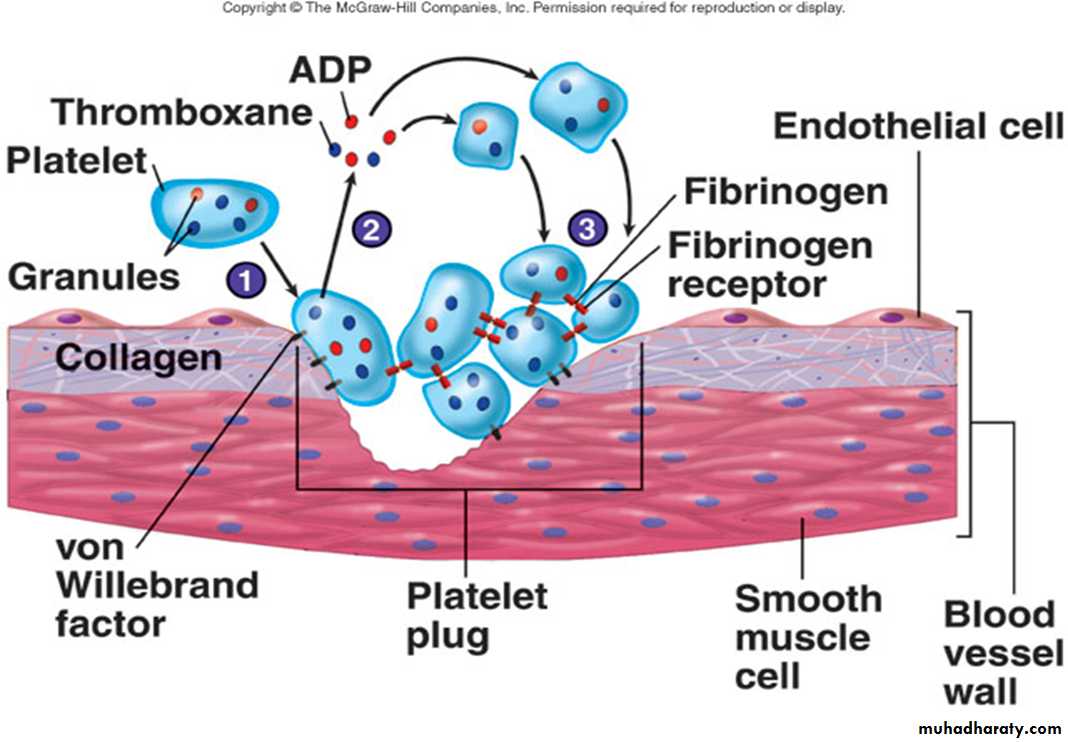
When platelets come in contact with a damaged vascular surface, platelets attach to the exposed collagen fibers in the vascular wall.
Platelets immediately change their own characteristics.
Platelets begin to swell and assume irregular forms with numerous irradiating pseudopods protruding from their surfaces.
Contractile proteins in the platelets contract forcefully and cause the release of granules that contain multiple active factors , Adenosine diphosphate (ADP) is released which causes surface of nearby circulating platelets to become sticky and it adheres to the first layer of aggregated platelets
The aggregated platelets adhere to the von Willebrand factor that leaks into the traumatized tissue from the plasma
It leads to the release of more ADP , which cause more platelets to pile up at the injured site. The aggregating process is reinforced by the formation of Thromboxane A2. It directly promotes platelet aggregation and further enhances it indirectly by triggering the release of even more ADP from the platelet granules, then Formation of platelet plug takes place.
Mechanism of platelet plug
The aggregated platelet plug not only physically seal the break in the vessel but, also perform three other important roles:
1. Actin and myosin which were the contractile proteins in the platelets contract , This compacts and strengthens the plug which was initially, a loose plug.
2. Various chemicals released from the platelet plug include several vasoconstrictors (serotonin, epinephrine and Thromboxane A2 ) cause vascular vasospasm
3. The platelet plug release other chemical substances that play a role in blood clotting.
Platelet plugging mechanism alone is sufficient to seal tears in the capillaries and small vessels but, large holes require formation of blood clot to stop bleeding.
**Normal endothelium of the vessel release Prostacyclin which prevents platelet aggregation. So, platelet plug is limited to the defected part of the vessel and does not spread to the normal vascular tissue.
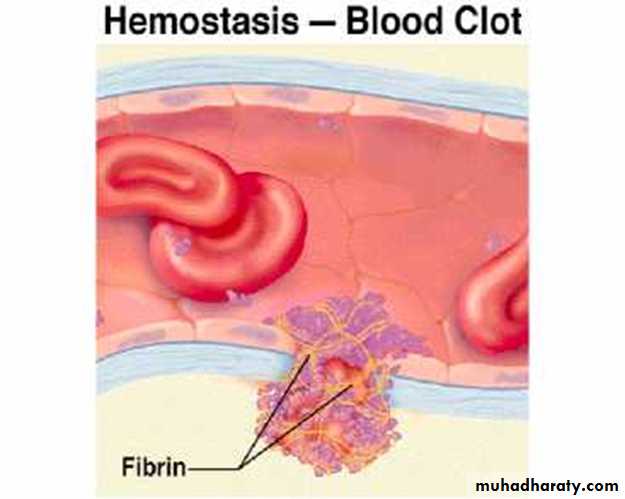
Blood clot in ruptured vessels
If there is a large defect in the vessel then blood clot + platelet plug are required to stop bleeding. As clot on the top of platelet plug , supports it and reinforces the seal over the break in the vessel.
Onset Of Formation Of Blood Clot:
15 – 20 sec…… in severe trauma.1 – 2 min…… in minor trauma.
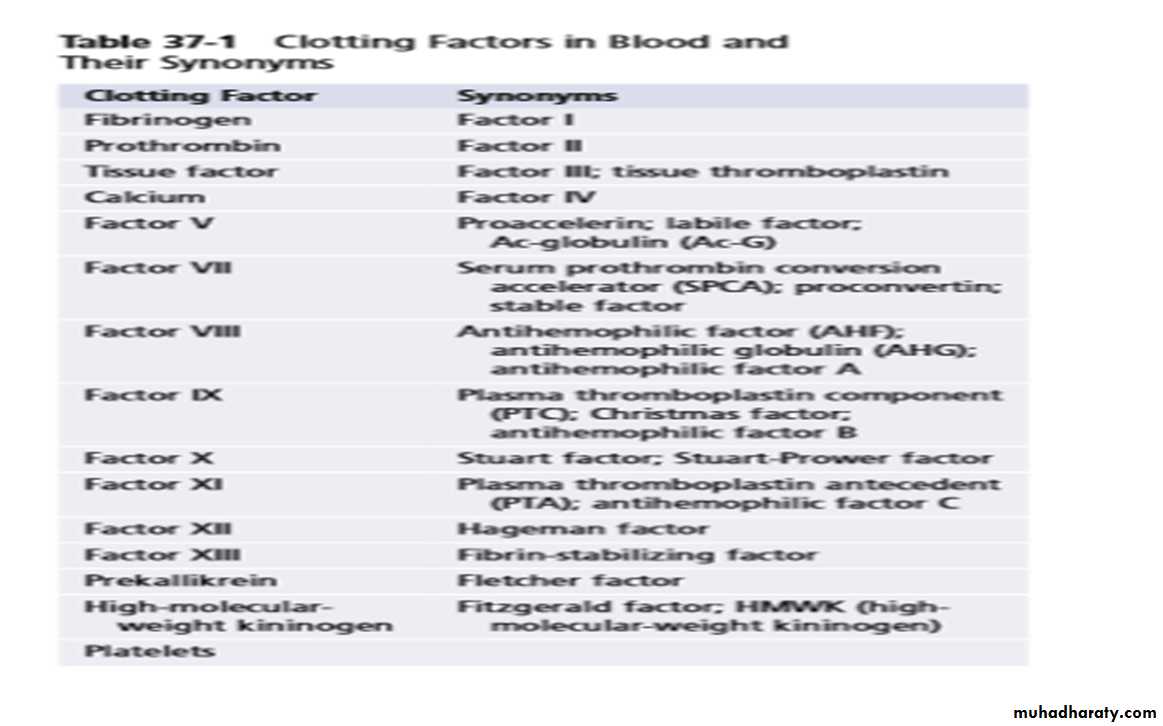
Ultimate step in clot formation is the conversion of fibrinogen which is a (soluble protein that is produced by the liver and is normally always present in the plasma) to fibrin which is( insoluble thread like molecule).
Fibrinogen ( thrombin) Fibrin
Fibrin molecules adhere to the damaged vessel surface forming a loose netlike meshwork that traps the cellular elements of blood. The clot appears red because of abundance of RBC that are trapped in it.
The original fibrin web is weak because the fibrin threads are loosely interlaced, then various chemical linkages are formed between adjacent strands to strengthen and stabilize the clot mesh work.
The cross linkage process which is catalyzed by a clotting factor known as factor XIII (Fibrin stabilizing factor).
Fibrous organization or Dissolution of blood clot
Once a blood clot has formed, it can follow one of two courses:
It can become invaded by fibroblasts, which subsequently form connective tissue all through the clot.
It can dissolve
The usual course for a clot that forms in a small hole of a vessel wall is invasion by fibroblasts, beginning within a few hours after the clot is formed. This event is promoted by growth factor secreted by platelets.
Complete organization of the clot into fibrous tissue takes place within 1 to 2 weeks.