1
Impacted Canine in Orthodontics
Tooth impaction can be defined as the infra-osseous position of the tooth after the
expected time of eruption, whereas the anomalous infra-osseous position of the canine
before the expected time of eruption can be defined as a displacement.
Theories regarding the causes of palatal displacement
1. Long path of eruption
2. Crowding
3. Non-resorption of the root of the deciduous canine
4. Trauma
5. Soft tissue pathology
6. Heredity
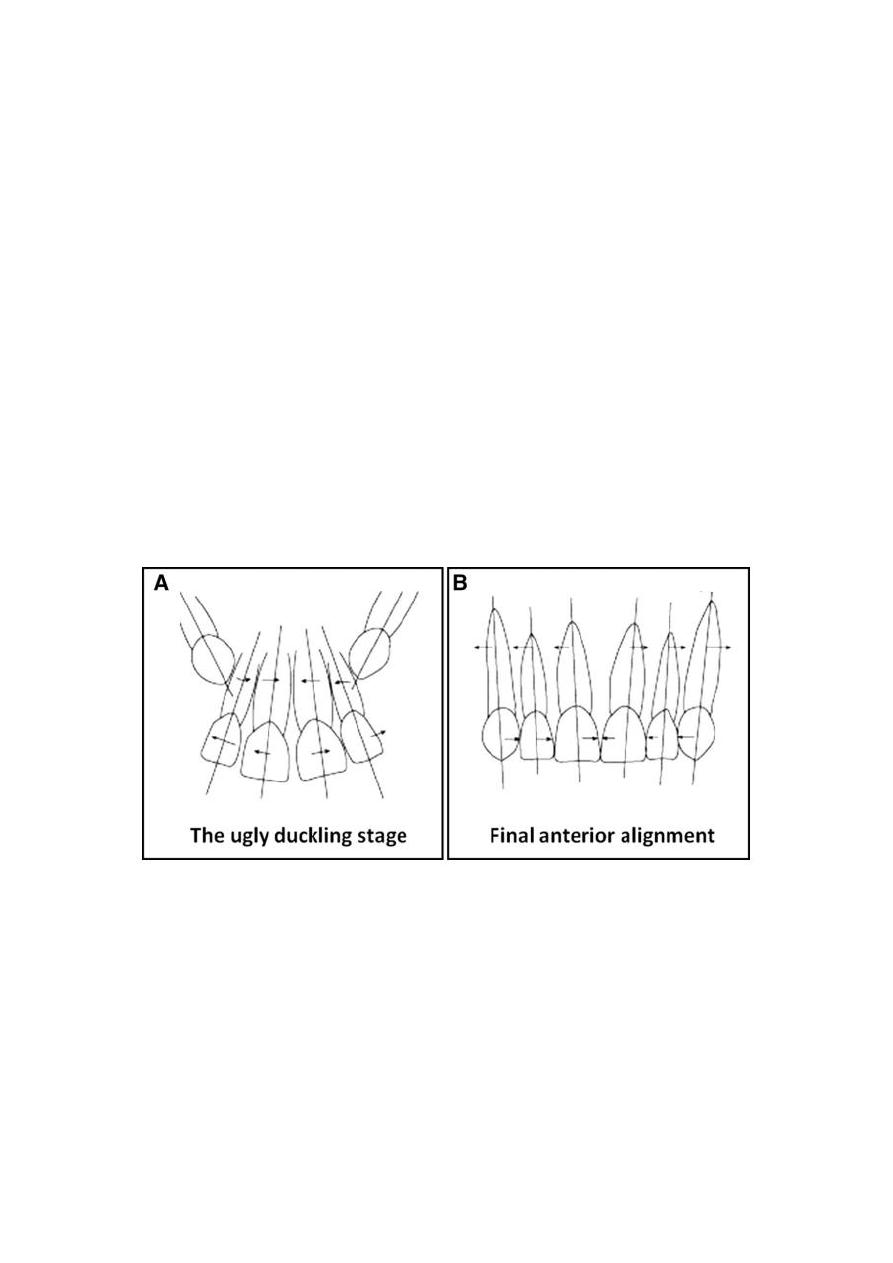
Diagrammatic representation of the relationships between the maxillary incisors, and between them and
the unerupted canines in normal development in a 9- to 10-year-old patient. The canines restricted the
roots into a narrowed apical area, causing lateral flaring of the incisor crowns. B, Diagrammatic
representation of the final alignment and long axis reorientation after eruption of the canines.
Causes of canine impaction
The causes can be classified into 4 distinct groupings: local hard tissue obstruction,
local pathology, departure from or disturbance of the normal development of the
incisors, and hereditary or genetic factors.
2
According to that aetiology for impacted canines could be due to:
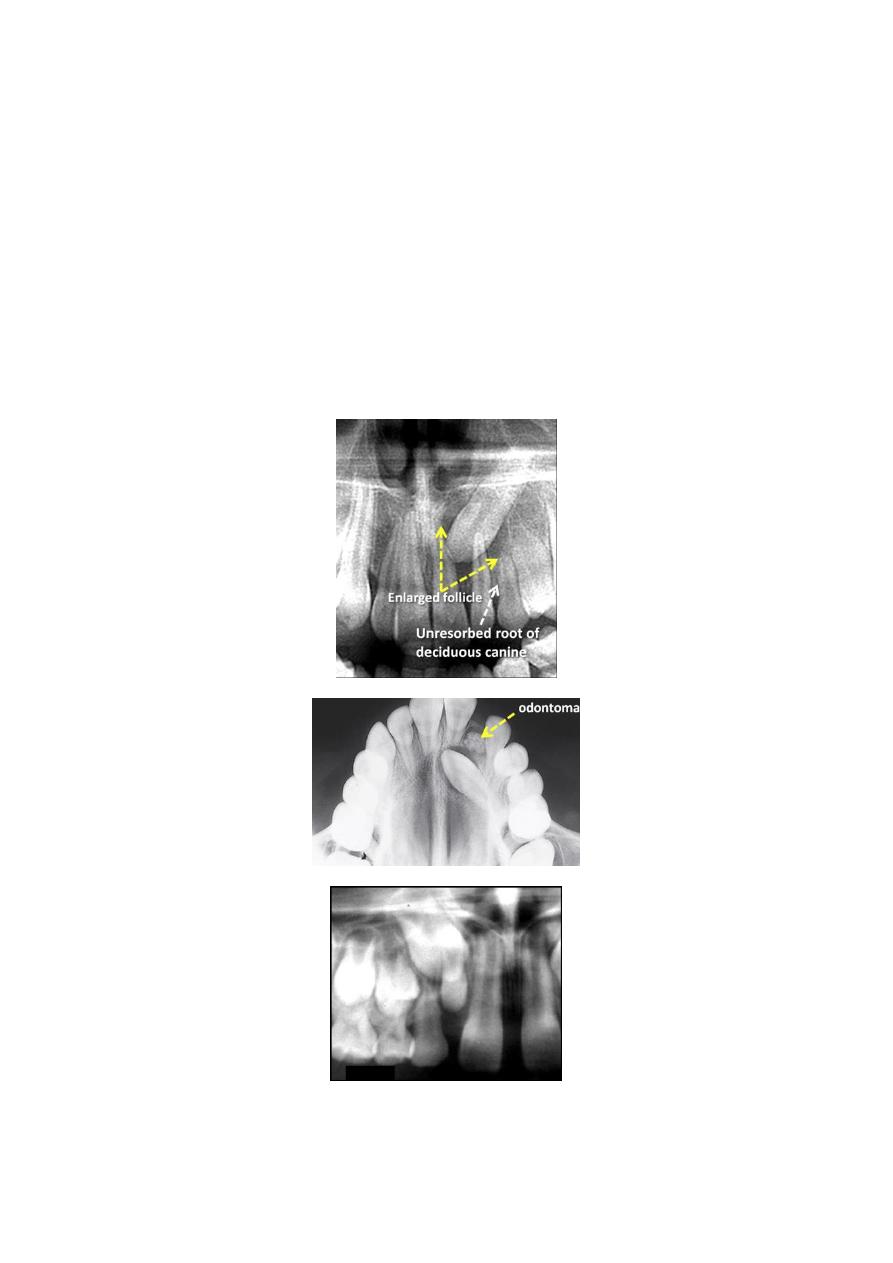
1. Presence of supernumeraries
2. Odontomes
3. Pathological lesions, eg cysts
4. Delayed exfoliation of the deciduous canine (although this is thought to be an
indicator rather than a cause of displacement)
5. Early trauma to the maxilla
6. Cleft lip and palate
7. Ankylosis
8. Displacement of crypt
9. Long path of eruption
10. Syndromes, eg cleidocranial dysplasia.
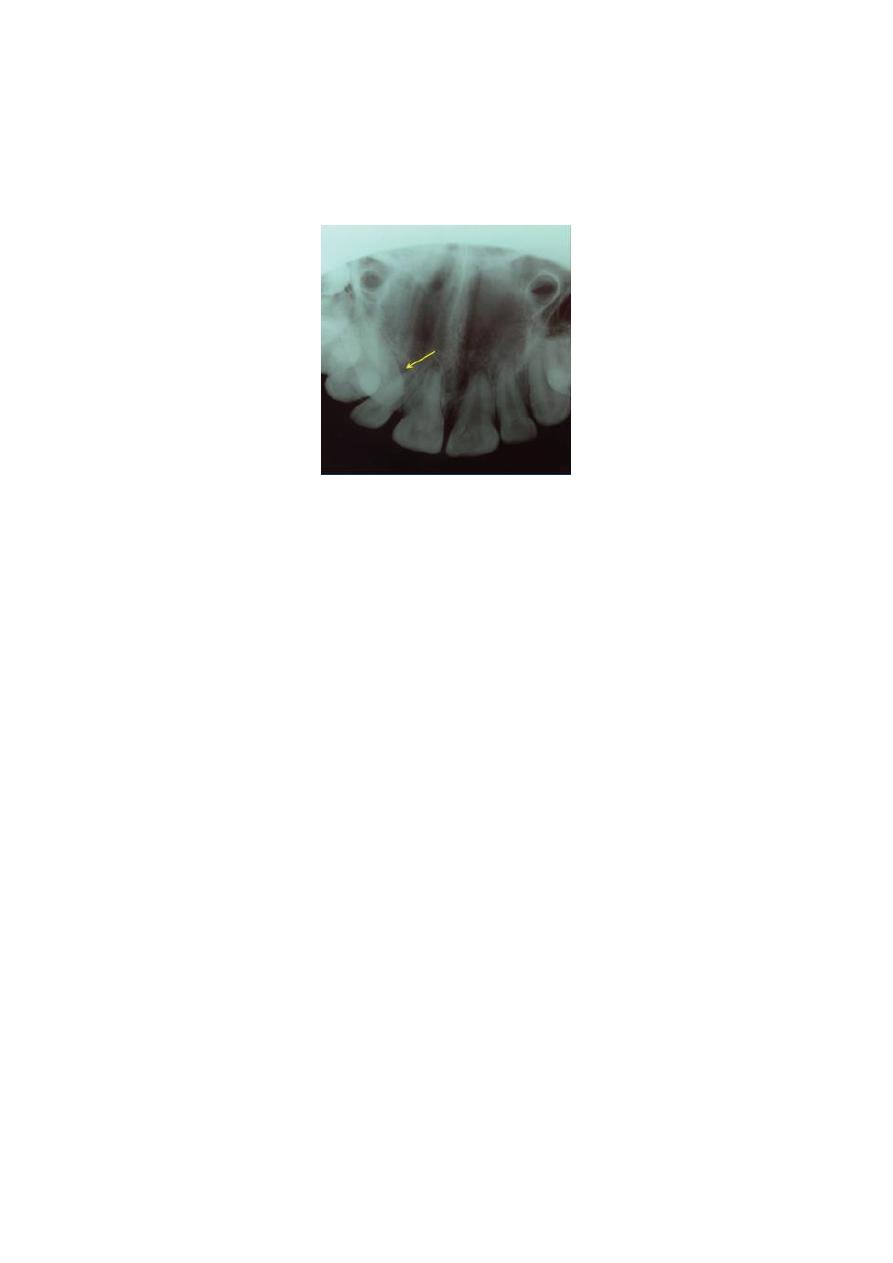
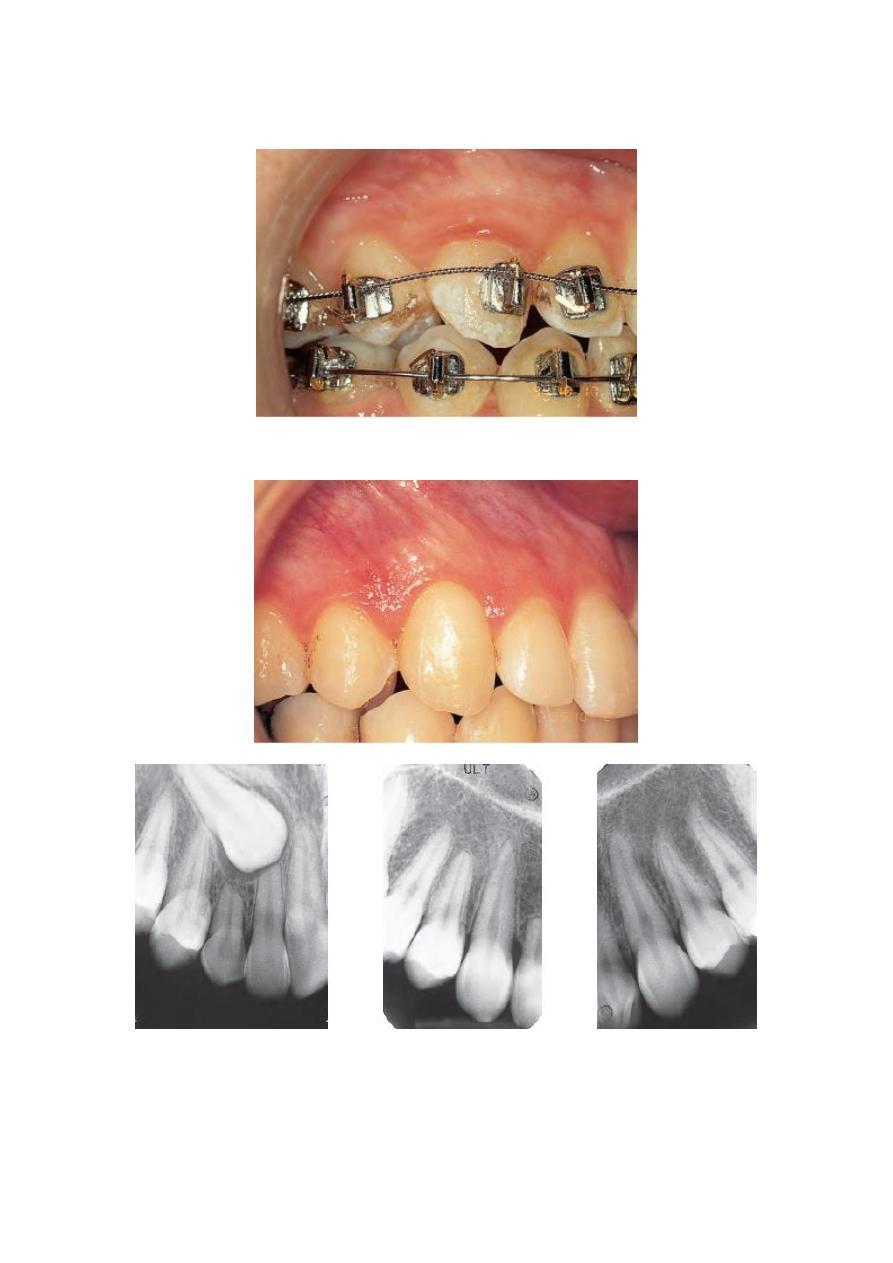
The crown of the unerupted lateral incisor is reduced in size and mildly peg shaped, whereas its
developing root has a length normally seen at age 4 to 5 years ( for image No.3).

3
Sequelae of Canine Impaction
1. Labial or lingual mal-positioning of the impacted tooth,
2. Migration of the neighboring teeth and loss of arch length,
3. Internal resorption,
4. Dentigerous cyst formation,
5. External root resorption of the impacted tooth, as well as the neighboring teeth,
6. Infection particularly with partial eruption, and
7. Referred pain and combinations of the above sequelae.
Diagnosis of Canine Impaction
The diagnosis of canine impaction is based on both clinical and radiographic
examinations.
Clinical assessment
Clinical investigation involves the following:
Visual inspection of the canine bulge, whether it is buccal or palatal which should be
seen between the lateral incisor and first premolar roots, and inspection of the
angulation of the lateral incisor, eg a distally inclined lateral incisor may infer palatal
impaction and a mesially inclined lateral incisor may indicate buccal impaction). In
addition, the colour and mobility of the deciduous canine should be inspected as this
might indicate resorption of the root.

4
Palpation of the buccal surface of the alveolar process distal to the lateral incisor from
8 years of age may reveal the position of the maxillary canine and has been
recommended as a diagnostic tool.
It has been suggested that the following clinical signs might be indicative of canine
impaction:
1. Delayed eruption of the permanent canine or prolonged retention of the deciduous
canine beyond 14–15 years of age,
2. Absence of a normal labial canine bulge,
3. Presence of a palatal bulge, and
4. Delayed eruption, distal tipping, or migration (splaying) of the lateral incisor.
Radiographic assessment
Although various radiographic exposures including occlusal films, panoramic views,
and lateral cephalograms can help in evaluating the position of the canines, in most
cases, periapical films are uniquely reliable for that purpose.
Periapical films
A single periapical film provides the clinician with a two-dimensional representation
of the dentition. In other words, it would relate the canine to the neighboring teeth
both mesio-distally and supero-inferiorly. To evaluate the position of the canine
bucco-lingually, a second periapical film should be obtained by one of the following
methods.
Tube-shift technique or Clark's rule or (SLOB) rule
Two periapical films are taken of the same area, with the horizontal angulation of the
cone changed when the second film is taken. If the object in question moves in the
same direction as the cone, it is lingually positioned. If the object moves in the
opposite direction, it is situated closer to the source of radiation and is therefore
buccally located.
Buccal-object rule
If the vertical angulation of the cone is changed by approximately 20° in two
successive periapical films, the buccal object will move in the direction opposite to
the source of radiation. On the other hand, the lingual object will move in the same
direction as the source of radiation. The basic principle of this technique deals with
the foreshortening and elongation of the images of the films.
5
Occlusal films
Also help to determine the bucco-lingual position of the impacted canine in
conjunction with the periapical films, provided that the image of the impacted canine
is not superimposed on the other teeth.
Extra-oral films
Frontal and lateral cephalograms
These can sometimes aid in the determination of the position of the impacted canine,
particularly its relationship to other facial structures (e.g., the maxillary sinus and the
floor of the nose).
Panoramic films
These are also used to localize impacted teeth in all three planes of space, as much the
same as with two periapical films in the tube-shift method, with the understanding
that the source of radiation comes from behind the patient; thus, the movements are
reversed for position.
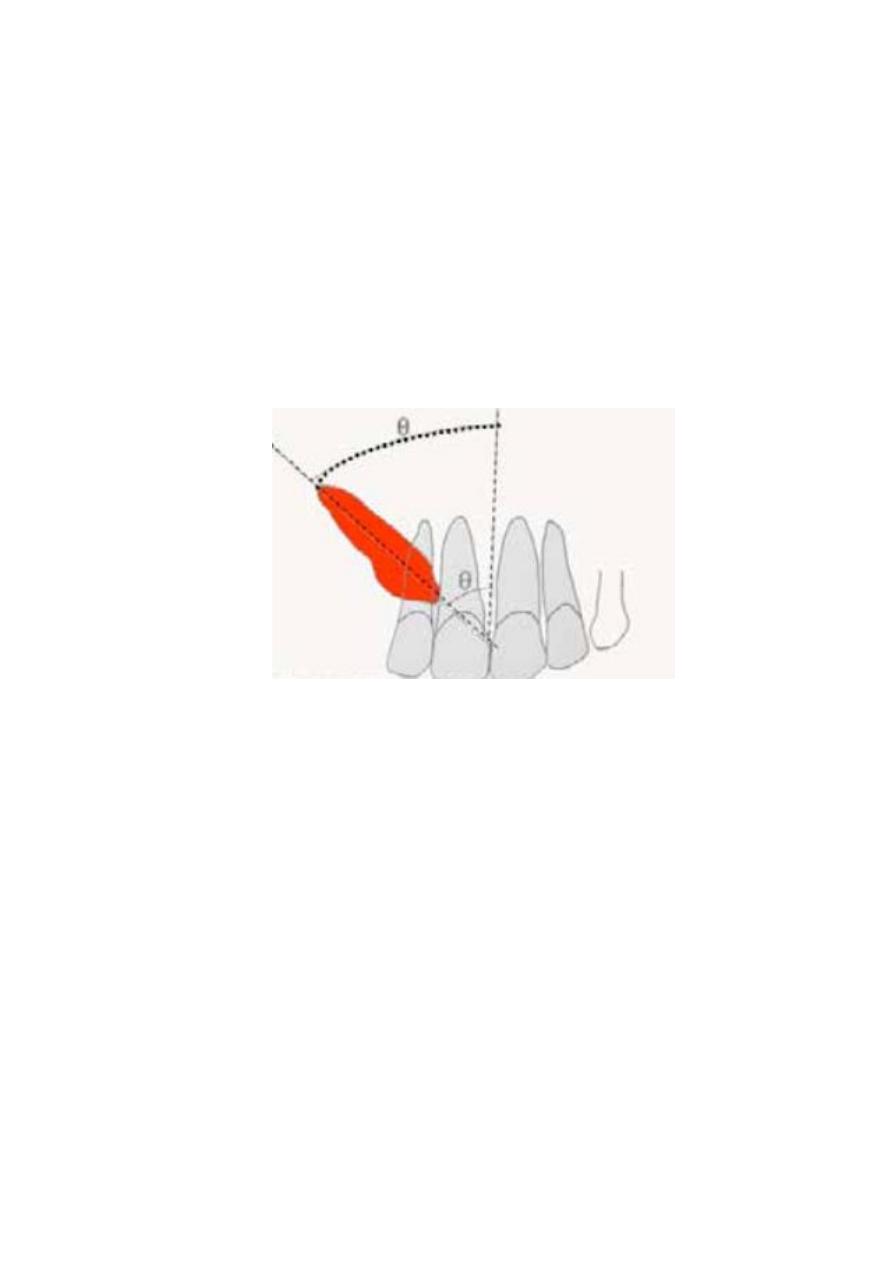
A method based on the location of the impacted canine
cusp tip and its relationship to
the adjacent lateral incisor was developed. Dividing impacted
canines into four
groups—sectors I through IV, with sector IV representing the
most severe
impaction—as many as 78% of the canines with
cusp tips in sectors II through IV
were destined to become impacted.
Sector I: cusp tip distal to a line tangent to the distal heights of
contour of the lateral
incisor crown and root.
Sector II: mesial to sector I, with the cusp tip distal to a line
bisecting the mesiodistal
dimension of the lateral incisor along the long
axis.
Sector III: mesial to sector II, with the cusp tip distal to a line tangent to
the mesial heights of contour of the lateral incisor crown and root.
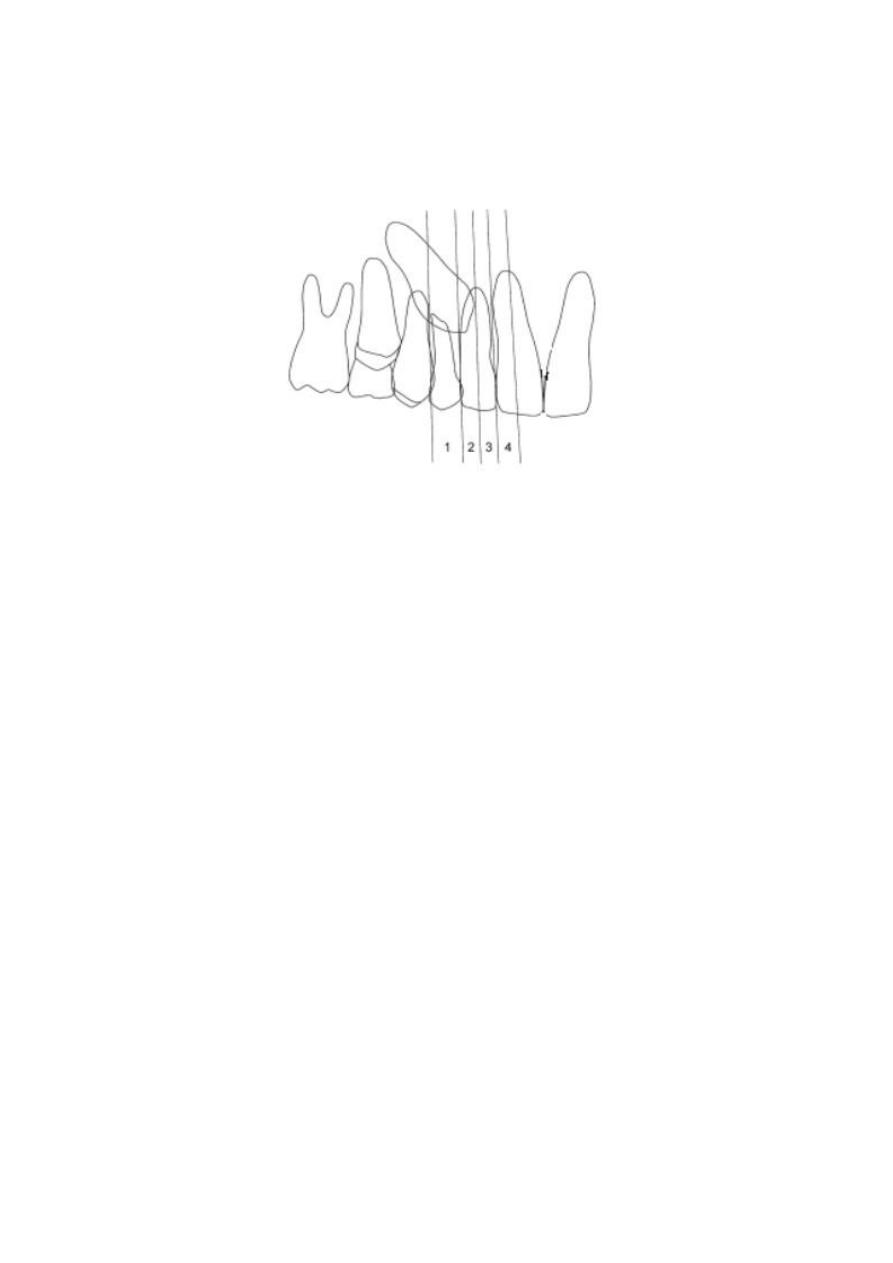
6
Sector IV: any position mesial to sector III.
CT/CBCT
Clinicians can localize canines by using advanced three-dimensional imaging
techniques.
Because of superimposition of structure on the film it become difficult to
distinguish the details which makes the diagnosis and treatment planning difficult
with conventional radiographic methods. To be in a position to recommend best line
of treatment and to plan appropriate mechanotherapy strategy the orthodontist
requires following information:
1. The exact position of the crown and root apex of the impacted tooth and orientation
of the long axis.
2. The proximity of the impacted tooth to the roots of the adjacent teeth.
3. The presence of pathology, such as supernumerary teeth, apical granulomas, or
cysts, and their relationship with the impacted tooth.
4. The presence of adverse conditions affecting adjacent teeth, including root
resorption.
5. The anatomy and position of crown and root
Treatment
In normal circumstances, by the age of 9–10, it is usually possible to palpate a
normally developing maxillary permanent canine tooth on the buccal side of the
alveolus, high above its deciduous predecessor. In the presence of crowding, and
particularly after the eruption of the first premolar, the bulging of the unerupted
canine is emphasized. The greater the degree of crowding the greater will be this
displacement and the more palpable will the canine become, as its eruptive process
brings it further and further down on the facial side of the dental arch. It follows, too,
that the greater the buccal displacement the greater the risk that it will erupt through
oral mucosa, higher up the alveolar process, rather than through attached gingiva.

7
In the event that the tooth is not palpable at this age, radiographs should be taken to
assist in locating the tooth accurately and to secure other information regarding the
presence, size, shape, position and state of development of individual unerupted teeth
and any pathology. In a patient younger than 9 years, the radiographs will not usually
show abnormality in the position of the unerupted canine teeth, even if the canines are
not palpable and even if they are destined subsequently to become palatally displaced.
Many of these non-palpable canines will finally erupt into good positions in the dental
arch in their due time, provided that there is little or no mesial and palatal
displacement of the crown of the unerupted tooth. It may be argued that even canines
with an initial mild palatal displacement will achieve spontaneous eruption and
alignment despite a first-stage displacement. Other canines, however, will not erupt,
and their positions may worsen in time, as may be seen in follow-up radiographs. If it
were possible to distinguish between the two early enough, a line of preventive
treatment might be advised
Interceptive Treatment
When the clinician detects early signs of ectopic eruption of the canines, an attempt
should be made to prevent their impaction and its potential sequelae. Selective
extraction of the deciduous canines as early as 8 or 9 years of age has been suggested
as an interceptive approach to canine impaction in Class I
un crowded cases
.
removal of the deciduous canine before the age of 11 years will normalize the position
of the ectopically erupting permanent canines in 91% of the cases if the canine crown
is distal to the midline of the lateral incisor. On the other hand, the success rate is only
64% if the canine crown is mesial to the midline of the lateral incisor
Schematic illustration showing the normalization rates of the maxillary canine after extraction
of the primary canine when the permanent maxillary canine is located mesially and distally to
the midline of the lateral incisor.
8
The extraction of a maxillary deciduous canine may be a useful measure in the
prevention of incipient canine impaction. To achieve maximum reliability, the
following conditions should be met before extraction is advised:
1. The diagnosis of palatal displacement must be made as early as possible.
2. The patient must be in the 10–13-year age range, preferably with a delayed
dental age.
3. Accurate identification of the position of the apex should be made and
confirmed to be in the line of the arch.
4. Medial overlap of the unerupted canine cusp tip should be less than half-way
across the root of the lateral incisor, on the panoramic view.
5.
The angulation of the long axis should be less than 55° to the mid-sagittal
plane.
Treatment alternatives
Each patient with an impacted canine must undergo a comprehensive evaluation of
the malocclusion. The clinician should then consider the various treatment options
available for the patient, including the following:
1. No treatment if the patient does not desire it. In such a case, the clinician should
periodically evaluate the impacted tooth for any pathologic changes. It should be
remembered that the long-term prognosis for retaining the deciduous canine is poor,
regardless of its present root length and the esthetic acceptability of its crown. This is
because, in most cases, the root will eventually resorb and the deciduous canine will
have to be extracted.
2. Auto transplantation of the canine.
3. Extraction of the impacted canine and movement of a first premolar in its position.
4. Extraction of the canine and posterior segmental osteotomy to move the buccal
segment mesially to close the residual space.

9
5. Prosthetic replacement of the canine.
6. Surgical exposure of the canine and orthodontic treatment to bring the tooth into the
line of occlusion. This is obviously the most desirable approach.
When to Extract an Impacted Canine
It should be emphasized that extraction of the labially erupting and crowded canine,
unsightly as this tooth may look, is contraindicated. Such an extraction might
temporarily improve the esthetics, but may complicate and compromise the
orthodontic treatment results, including the ability to provide the patient with a
functional occlusion. The extraction of the canine, although seldom considered, might
be a workable option in the following situations:
1. If it is ankylosed and cannot be transplanted,
2. If it is undergoing external or internal root resorption,
3. If its root is severely dilacerated,
4. If the impaction is severe (e.g., the canine is lodged between the roots of the central
and lateral incisors and orthodontic movement will jeopardize these teeth),
5. If the occlusion is acceptable, with the first premolar in the position of the canine and
with an otherwise functional occlusion with well-aligned teeth,
6. If there are pathologic changes (e.g., cystic formation, infection), and
7. If the patient does not desire orthodontic treatment.
Management of Impacted Canines
The most desirable approach for managing impacted maxillary canines is early
diagnosis and interception of potential impaction. However, in the absence of
prevention, clinicians should consider orthodontic treatment followed by surgical
exposure of the canine to bring it into occlusion. In such a case, open communication
between the orthodontist and oral surgeon is essential, as it will allow for the
appropriate surgical and orthodontic techniques to be used. The most common
methods used to bring palatally impacted canines into occlusion are surgically
exposing the teeth and allowing them to erupt naturally during early or late mixed
dentition and surgically exposing the teeth and placing a bonded attachment to and
using orthodontic forces to move the tooth. Three methods for uncovering a labially
impacted maxillary canine:
1. Gingivectomy,
2. Creating an apically positioned flap,
3. Using closed eruption techniques.
11
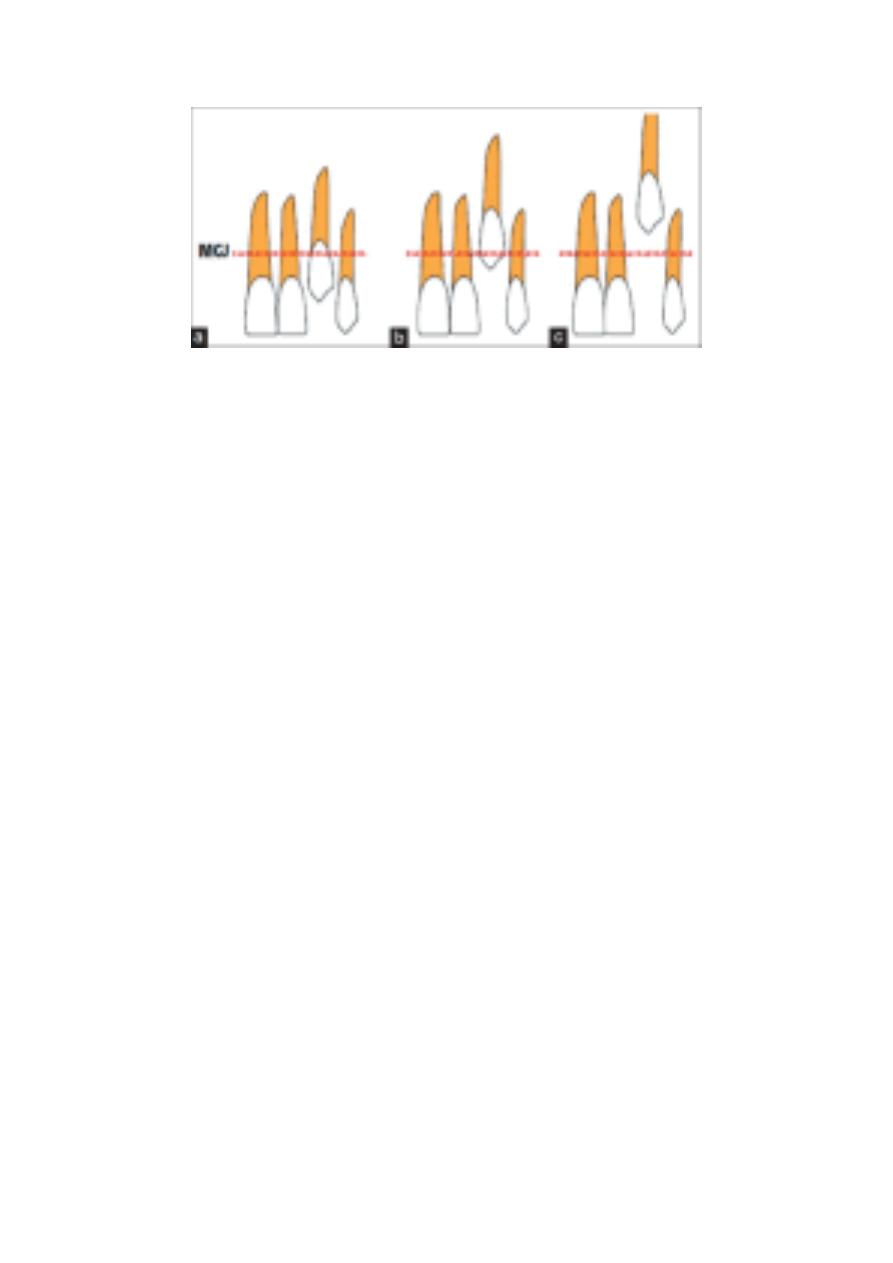
Recommended surgical techniques relative to the mucogingival junction (MGJ) when
the canine cusp is (a) coronal to the MGJ: gingivectomy; (b) apical to the MGJ:
creating an apically positioned flap; and (c) significantly apical to the MGJ: using a
closed
eruption techniques
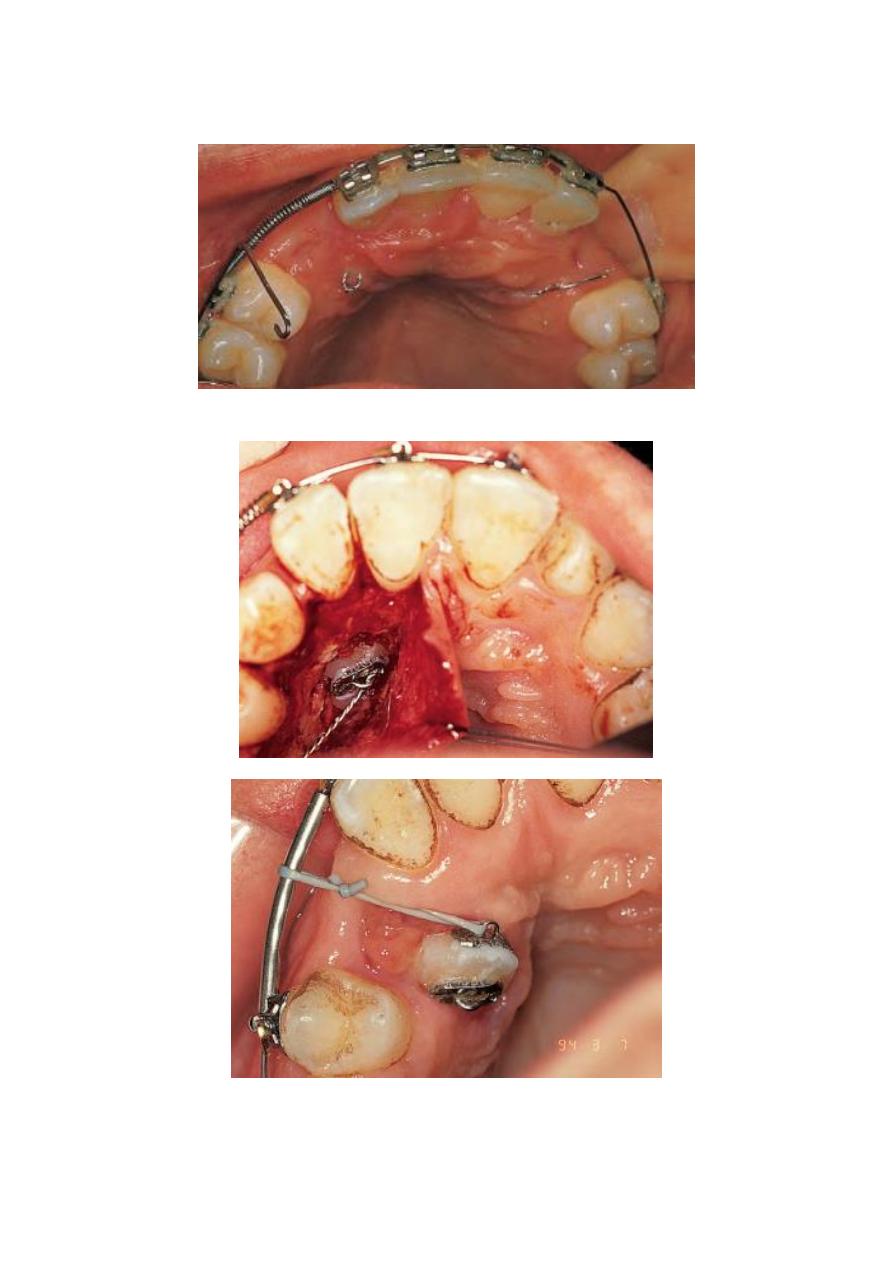
Orthodontists have recommended that other clinicians first create adequate space in
the dental arch to accommodate the impacted canine and then surgically expose the
tooth to give them access so that they can apply mechanical force to erupt the tooth.
Although various methods work, an efficient way to make impacted canines erupt is
to use closed-coil springs with eyelets, as long as no obstacles impede the path of the
canine.
If the canine is in close proximity to the incisor roots and a buccally directed force is
applied, it will contact the roots and may cause damage. In addition, the canine
position may not improve due to the root obstacle. Consequently, various techniques
have been proposed that involve moving the impacted tooth in an occlusal and
posterior direction first and then moving it buccally into the desired position. When
using a bonded attachment and orthodontic forces to bring the impacted canines into
occlusion, it is important to remember that first premolars should not be extracted
until a successful attempt is made to move the canines. If the attempt is unsuccessful,
the permanent canines should be extracted.
In such cases, the orthodontist has to decide if the premolar should be moved into the
canine position. Orthodontists should consider treatment alternatives, such as
autotransplantation or restoration, in collaboration with other specialists, including
oral surgeons, periodontists, and prosthodontists. The patient should be informed
about all of the potential complications before surgical and orthodontic interventions
take place.
11
12



