Internal medicine UA_NSTEMI Dr.tahsin
Acute Coronary Syndrome (ACS):
Unstable Angina/ Non-ST Elevation Myocardial Infarction UA/NSTEMI
Objectives
• ACS can present as unstable angina, NSTEMI, and STEMI
• The above division is based on the ECG and s.troponin
• The difference in clinical presentation between STEMI and NSTEMI depends on whether the
obstruction is complete or partial.
• Life-long medication is essential to improve long term outcomes
UA/NSTEMI
Definition:
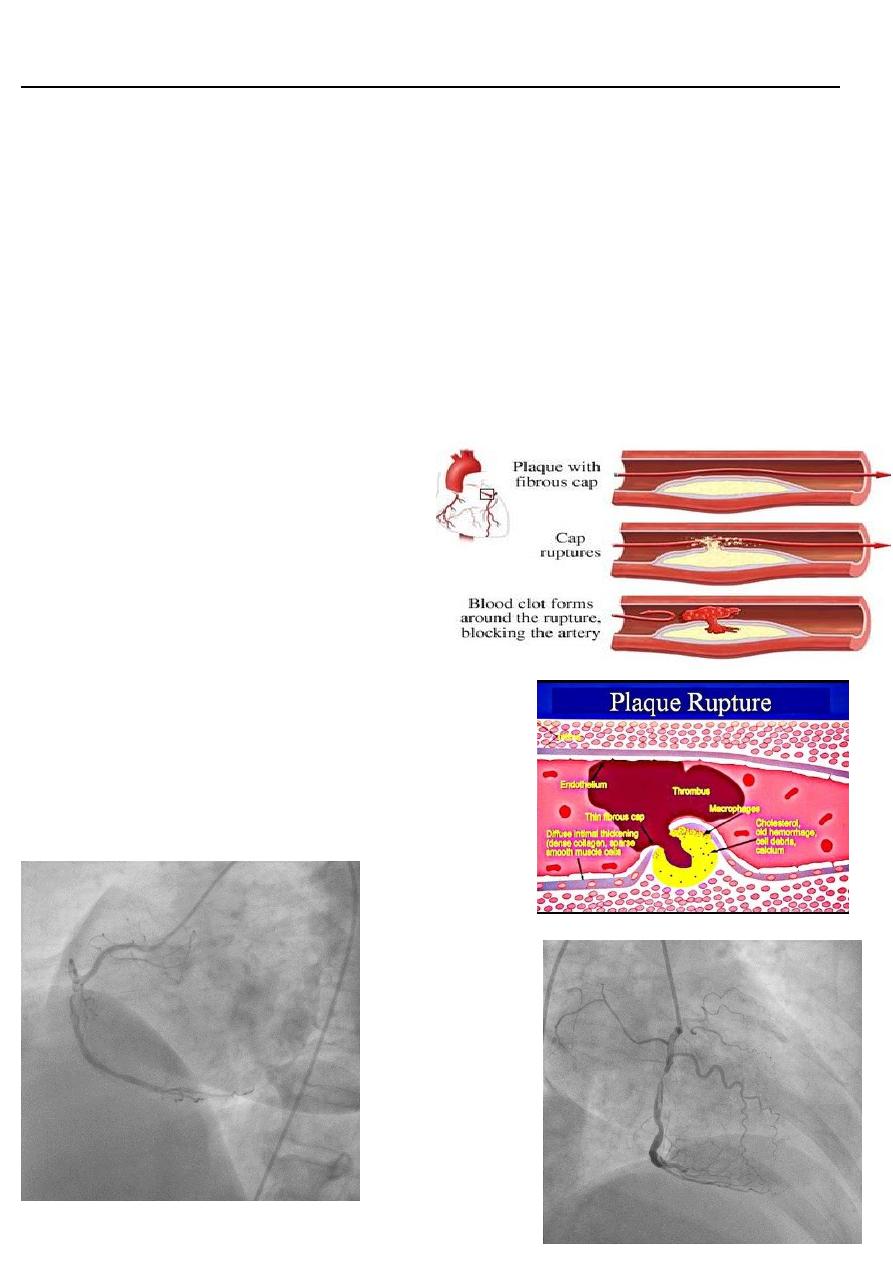
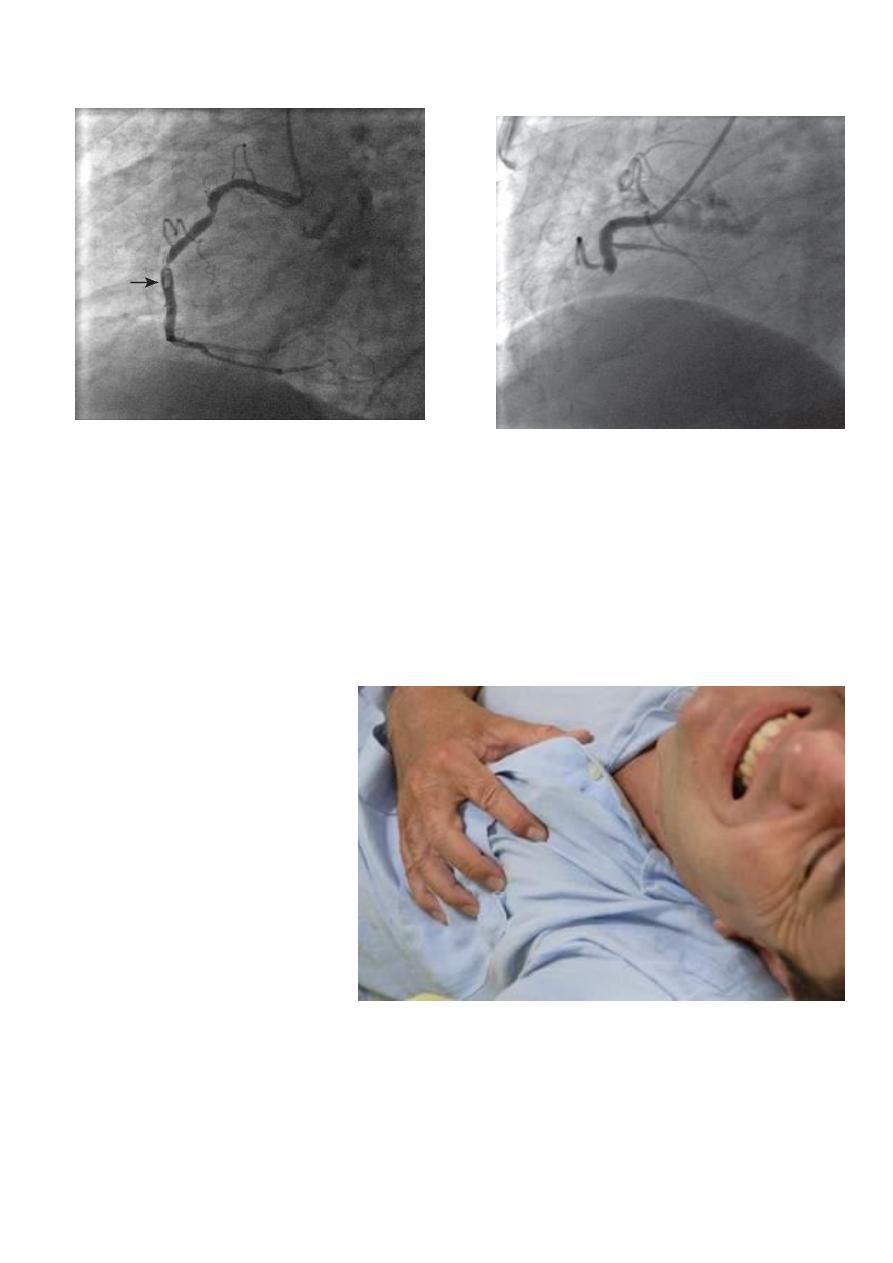
unstable angina is ischemia caused by
dynamic obstruction of a coronary artery
by vessel spasm or plaque rupture and
superimposed thrombus
Pathophysiology
• Similar to that of acute myocardial infarction (AMI)
• Thrombus developing on top of an ulcerated,
fissured, or ruptured atherosclerotic plaque
• In UA/NSTEMI, thrombus is mainly
composed of platelets
• In STEMI, the thrombus is composed
mainly of fibrin
• The condition is no longer an imbalance
between myocardial blood supply and
demand, since chest pain is present
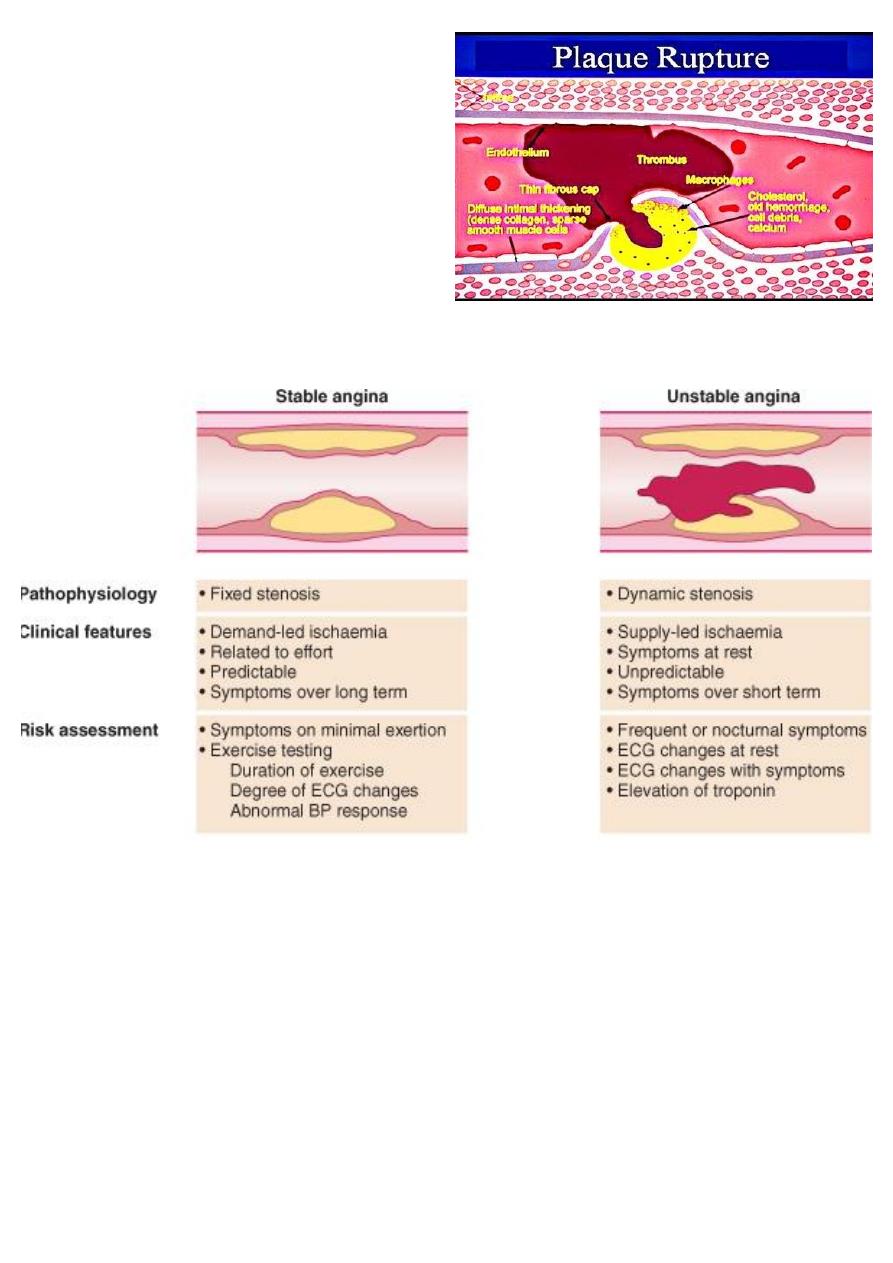
Acute Coronary syndrome Vs Stable Angina
Components of ACS: Clinical Differentiation
• Unstable angina
• Non-ST segment myocardial infarction (NSTEMI)
• ST-elevation MI (STEMI)
Unstable angina: pain at rest, NO ECG changes, troponin normal
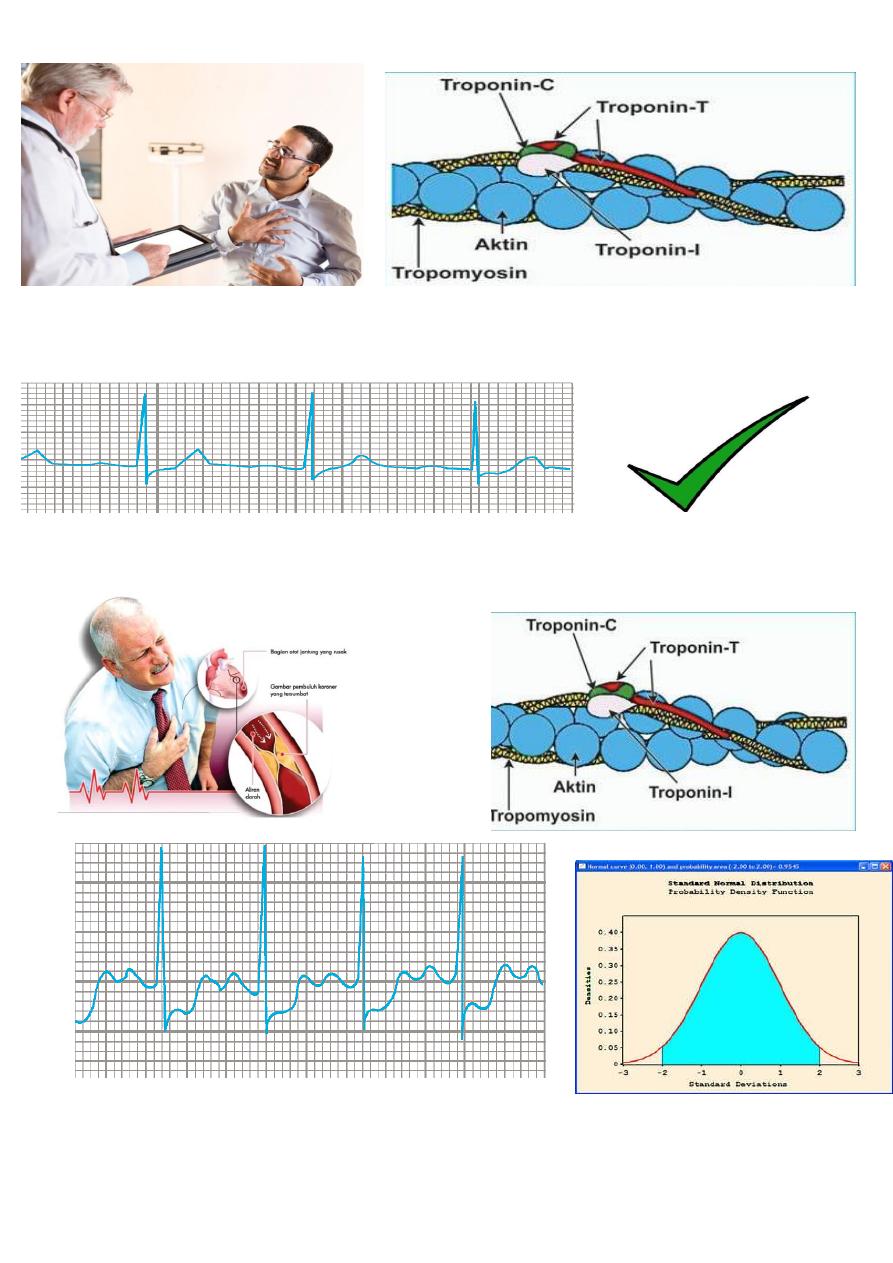
NSTEMI: chest pain, ECG normal or shows ST-Depression, troponin increased
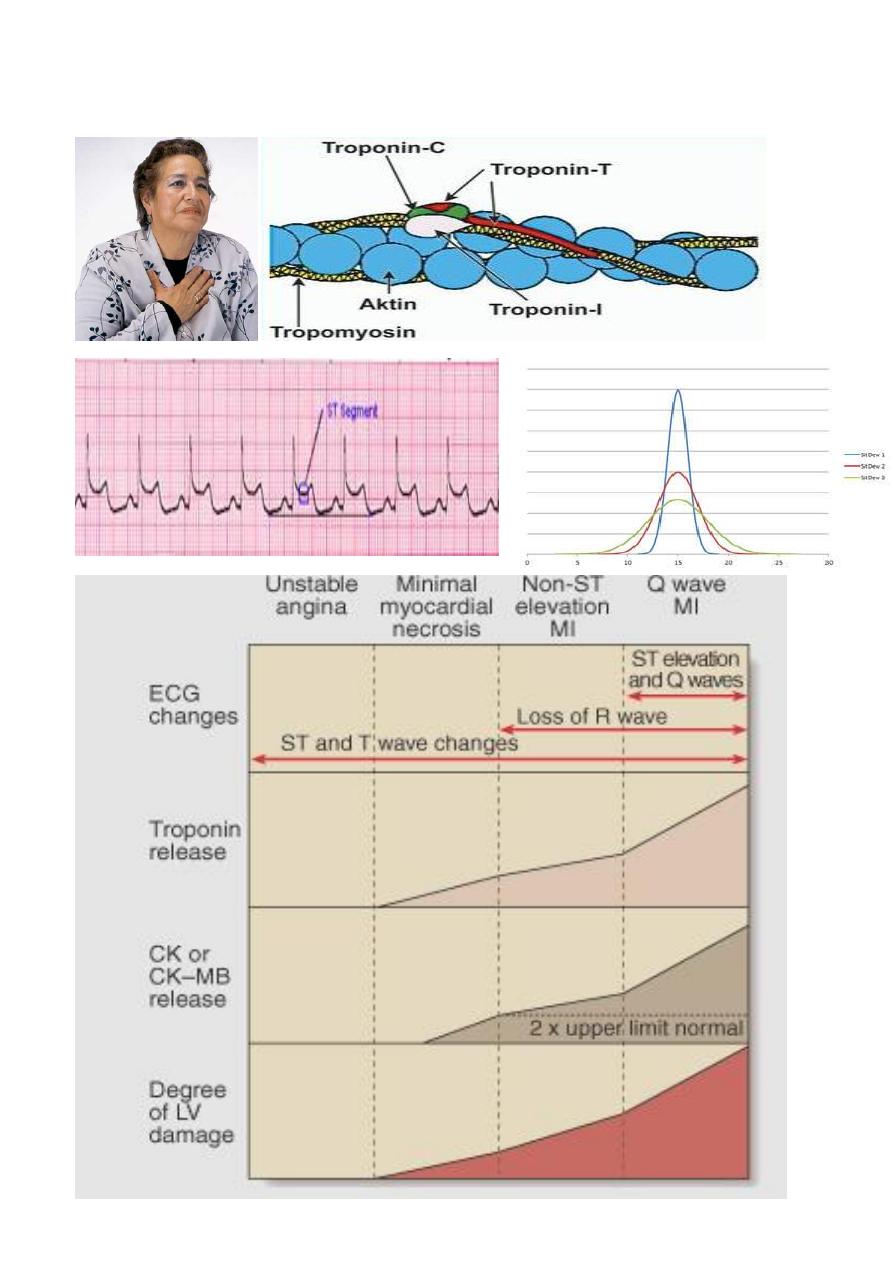
STEMI: chest pain, ECG shows ST elevation, troponin high
NSTEMI STEMI
Definition
• Prolonged angina (> 20 minutes)
• New onset (de novo) severe angina (within 3 months)
• Recent destabilization of previously stable angina: angina at rest
• Post MI angina
Clinical Features: Symptoms
• Anginal pain
– Rest pain
– Nocturnal angina
– Minimal exertion
• Sweating
• Nausea
• Abdominal pain
• Syncope
Clinical Features: Signs
Depend on the severity of the condition and the state of LV function
• Can be unremarkable
• Severe anxiety

• Pallor
• Sweating
• S3 & S4 gallop
• Crepitations
UA/NSTEMI: Risk Stratification
Depends on
• Clinical
• ECG
• & Biochemical criteria
Clinical Criteria of Poor Px
• Old age * Diabetes mellitus
Clinical Criteria of Poor Px
• Recurrent, prolonged chest pain at rest
• Post MI angina
• Congestive heart failure
• Mitral regurgitation
ECG Criteria of Serious Disease
• Arrhythmias
• Widespread ST depression
• Transient ST elevation (< 30 min)

Biochemical Criteria for Px
Plasma troponin level:
• > 0.1 µg/l correlates with serious disease and poor prognosis (extensive myocardial damage)
• < 0.1 µg/l correlates with low risk
UA/NSTEMI: Management
• Urgent admission to hospital
• IV line
• Bed rest
• Oxygen if O2 saturation < 90%
• Detect and treat any precipitating condition:
– Hypertension
– Tachycardia
– Anemia, thyrotoxicosis
UA/NSTEMI: Management
• Aspirin: 300 mg initially followed by 100 mg daily
• Clopidogrel
• Anticoagulation:
– Unfractionated heparin
– Low molecular weight heparin
– Bivaluridin
UA/NSTEMI: Management
• Oral beta blockers: especially if tachycardia or hypertension without signs of heart failure
• Nitrates: oral or intravenous, according to severity.
– Used cautiously if BP< 90mmHg
UA/NSTEMI: Management
• ACE inhibitors
• Statins
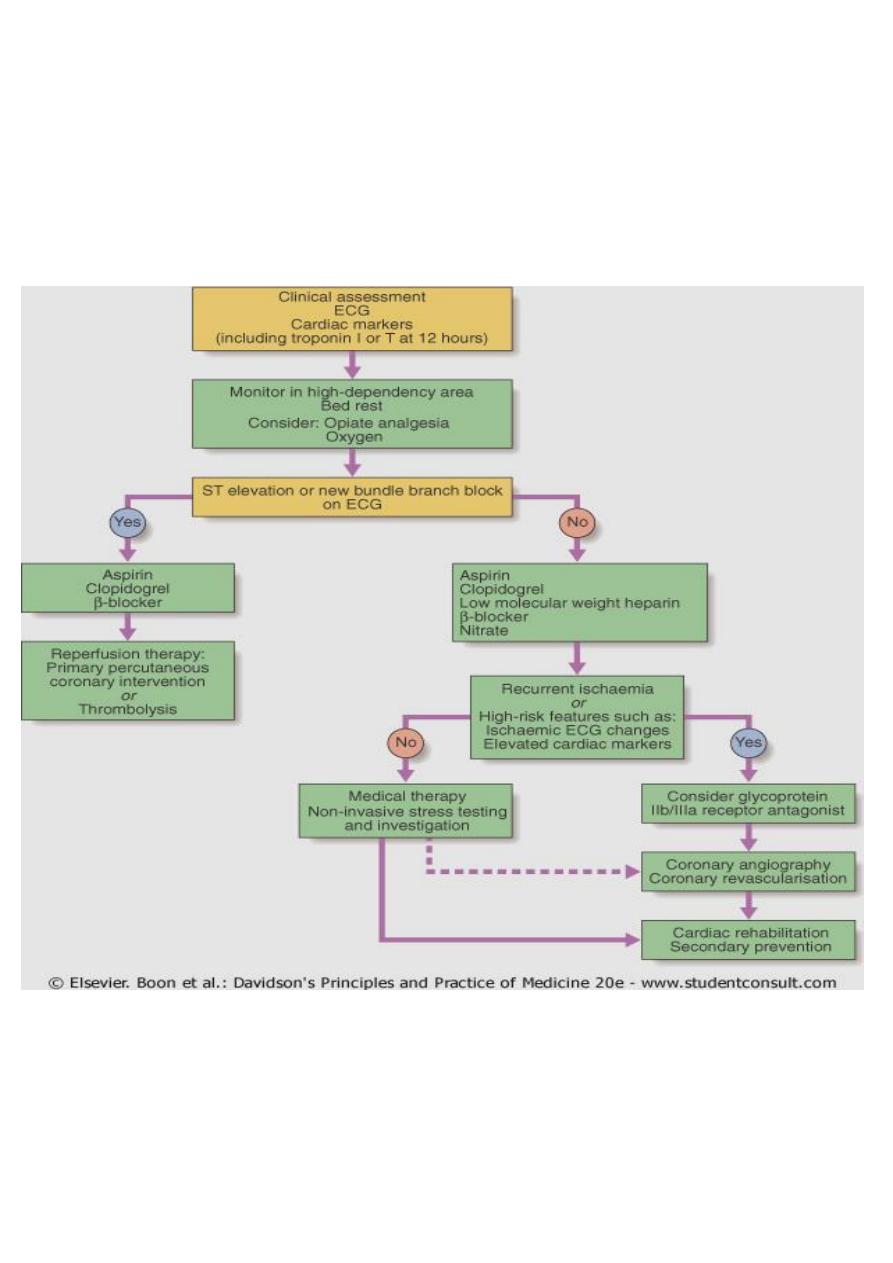
Management of the High Risk Patient
• Early invasive strategy: PCI or CABG
• Thrombolytic therapy?
– Not useful (why?)
– May be harmful
Steps in Managements
• Optimized medical treatment
• If patient is still unstable: invtervention
• If chest pain resolves: kept in hospital for 3-5 days, then before discharge ETT done at
modified workload

• If predischarge ETT positive; intervention
• If predischarge ETT negative: patient sent home on treatment, then ETT repeated at full
workload after 6 weeks
• If full workload ETT positive: intervention
• If negative: medical therapy, with regular check ups
• LIFELONG treatment with:
• Aspirin
• Beta blockers
• Statin
• ACE inhibitor or ARB
• In addition to one-year treatment with clopidogrel
" مع الشكر تدوم النعم"
