PROF.DR.MAHA SHAKIR (Lec.1)
Hemodynamic Disorders,Thromboembolism, and Shock
The health of cells and tissues depends on the circulation of blood, which delivers oxygen and nutrients and removes wastes generated by cellular metabolism.
In this system we will discuss the following:
Hyperemia and Congestion
Hemorrhage
Edema
Thrombosis
Disseminated Intravascular Coagulation
Embolism
Infarction
Shock
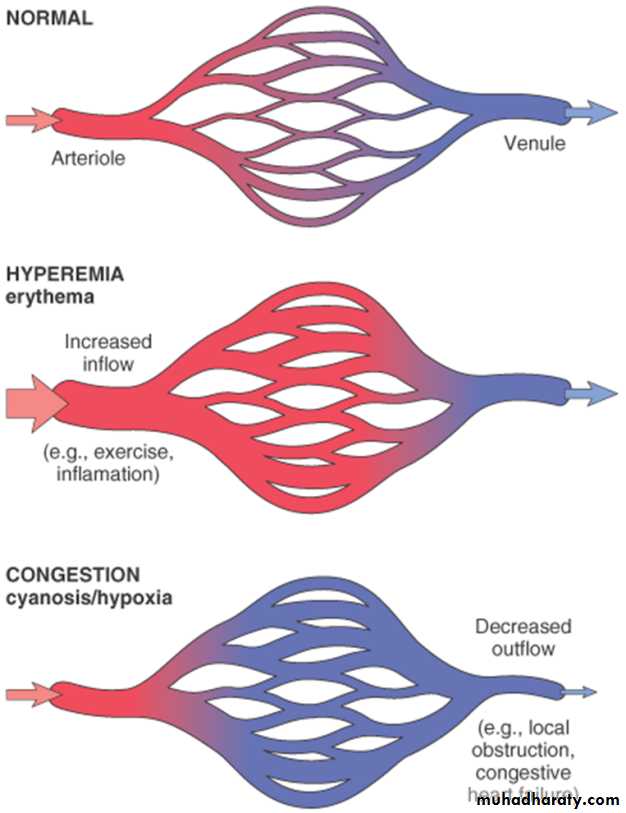
Hypermia and Congestion
Definition: Both of them can be defined as a local increase in volume of blood in a particular tissue.
Hypermia
It is an active process resulting from arteriolar dilation and increased blood inflow, as occurs at sites of:
exercising skeletal muscle
or acute inflammation
Hyperemic tissues are redder than normal because of engorgement with oxygenated blood.
Congestion
Congestion is a passive process resulting from impaired outflow of venous blood from a tissue. It can occur:
systemically, as in cardiac failure,
or locally as a consequence of an isolated venous obstruction.
Congested tissues have an abnormal blue-red color (cyanosis) that stems from the accumulation of deoxygenated hemoglobin in the affected area.
In long-standing chronic congestion, inadequate tissue perfusion and persistent hypoxia may lead to:
parenchymal cell death.
secondary tissue fibrosis.
the elevated intravascular pressures may cause edema or sometimes rupture capillaries forming focal hemorrhage.
Fig.HYPEREMIA/(CONGESTION)
MORPHOLOGYCut surfaces of hyperemic or congested tissues feel wet and
typically ooze blood.
a) Pulmonary congestion
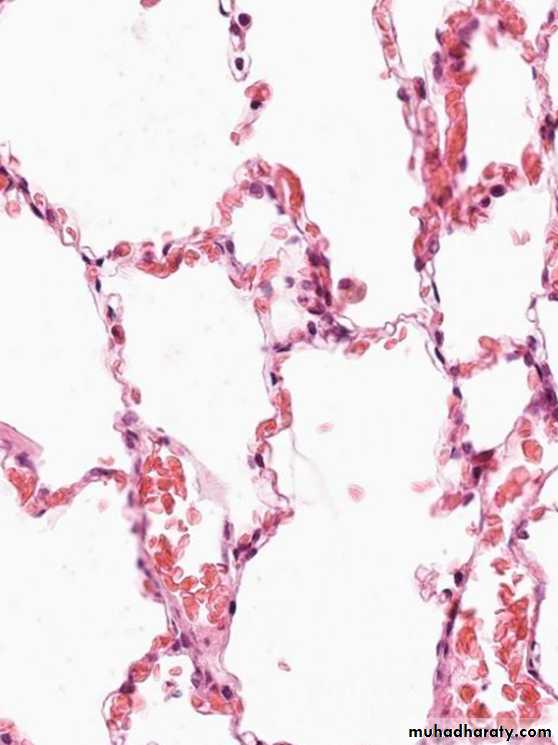
Acute pulmonary congestion:
Alveolar capillaries engorged with blood
variable degrees of alveolar septal edema and intraalveolar hemorrhage.
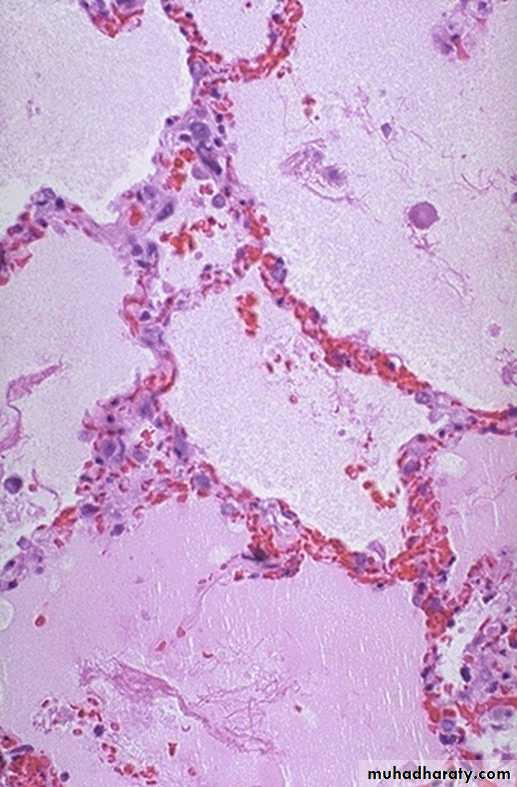
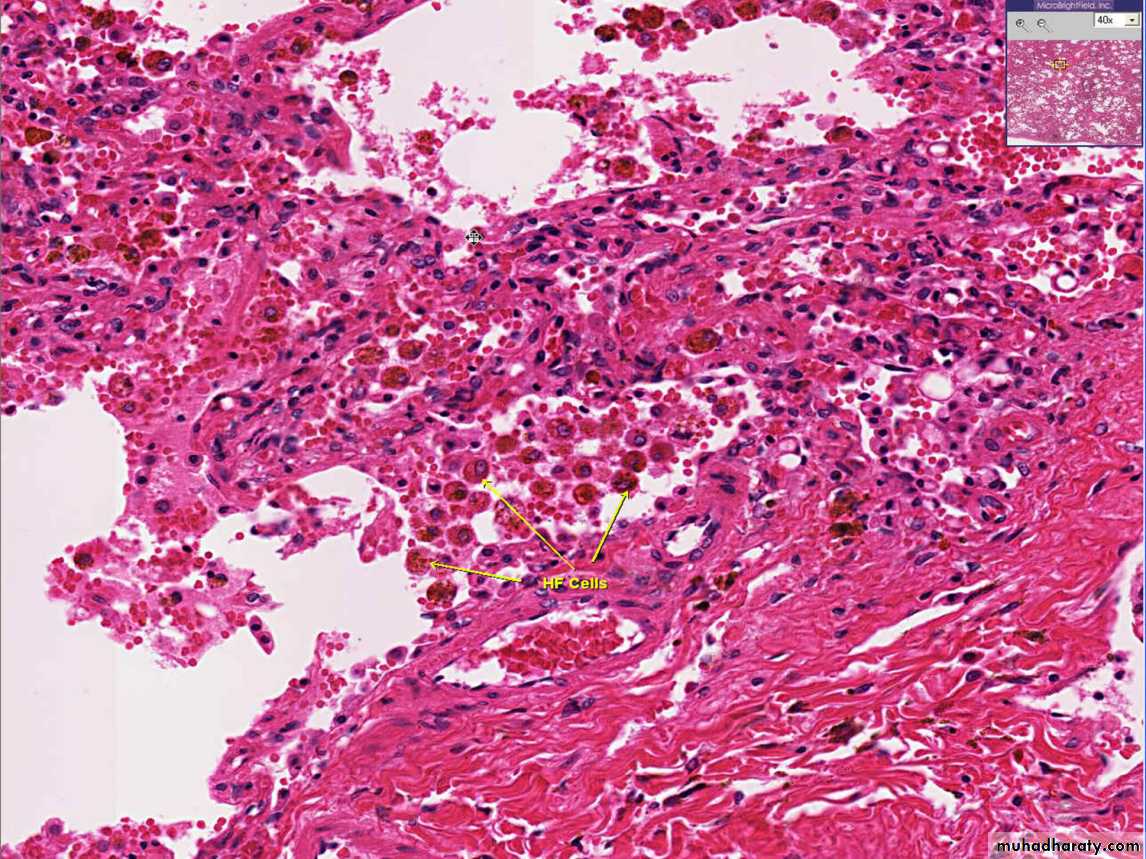
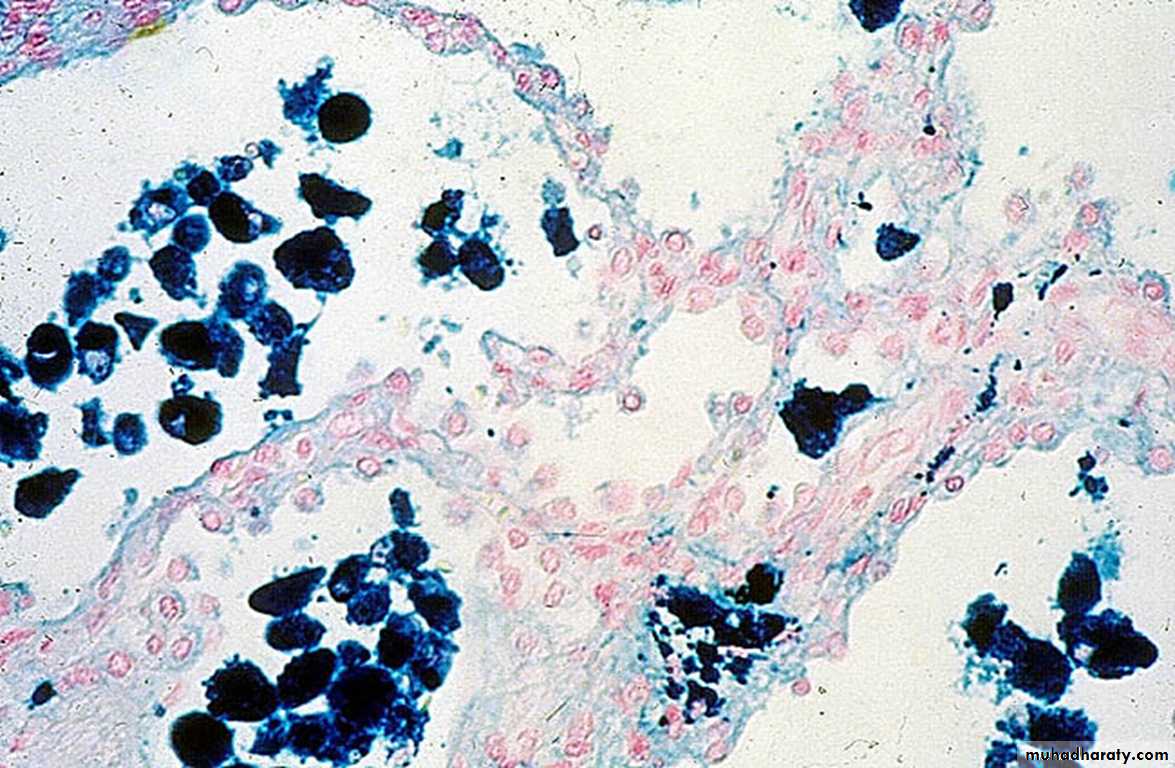
-2Chronic pulmonary congestion
Thickened & fibrotic septa
Alveolar spaces contain hemosiderin-laden macrophages (“heart failure cells”) derived from phagocytosed red cells.
Fig; Lung, acute pulmonary congestion.
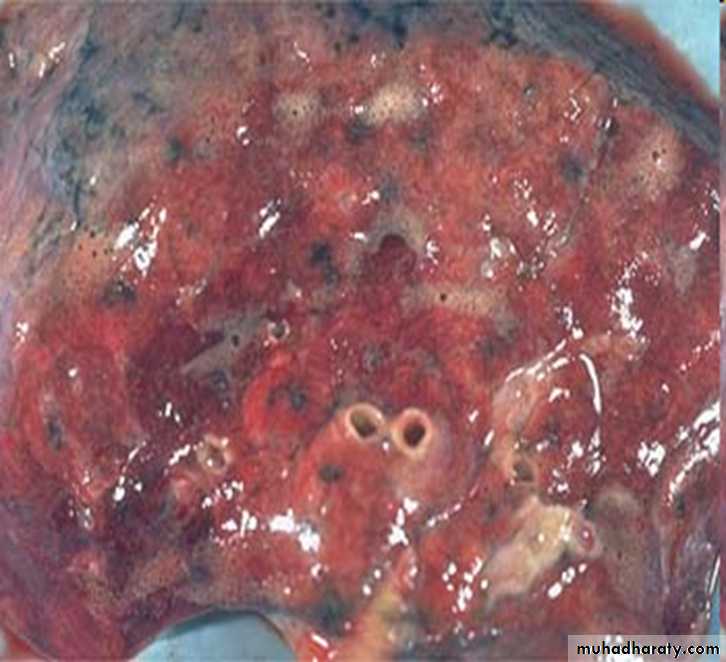
fig:Lung, chronic passive congestions: surface The lung has a red-brown color due to accumulation of hemosiderin from extravasated erythrocytes. Fibrosis causes the cut edges to stand up rather than collapse.
Fig: left :normal lung. Right:ACUTE PASSIVE HYPEREMIA/CONGESTION, LUNG
Fig:CHRONIC PASSIVE HYPEREMIA/CONGESTION, LUNG: heart failure cells
Fig:Special stain for haemosiderin (prusian blue) for heart failure cells
b) Hepatic congestion
1-Acute hepatic congestion:
the central vein and sinusoids are distended with blood,
and there may even be necrosis of centrally located hepatocytes.
The periportal hepatocytes, better oxygenated,???
because of their proximity to hepatic arterioles, experience
less severe hypoxia and may develop only reversible fatty change.
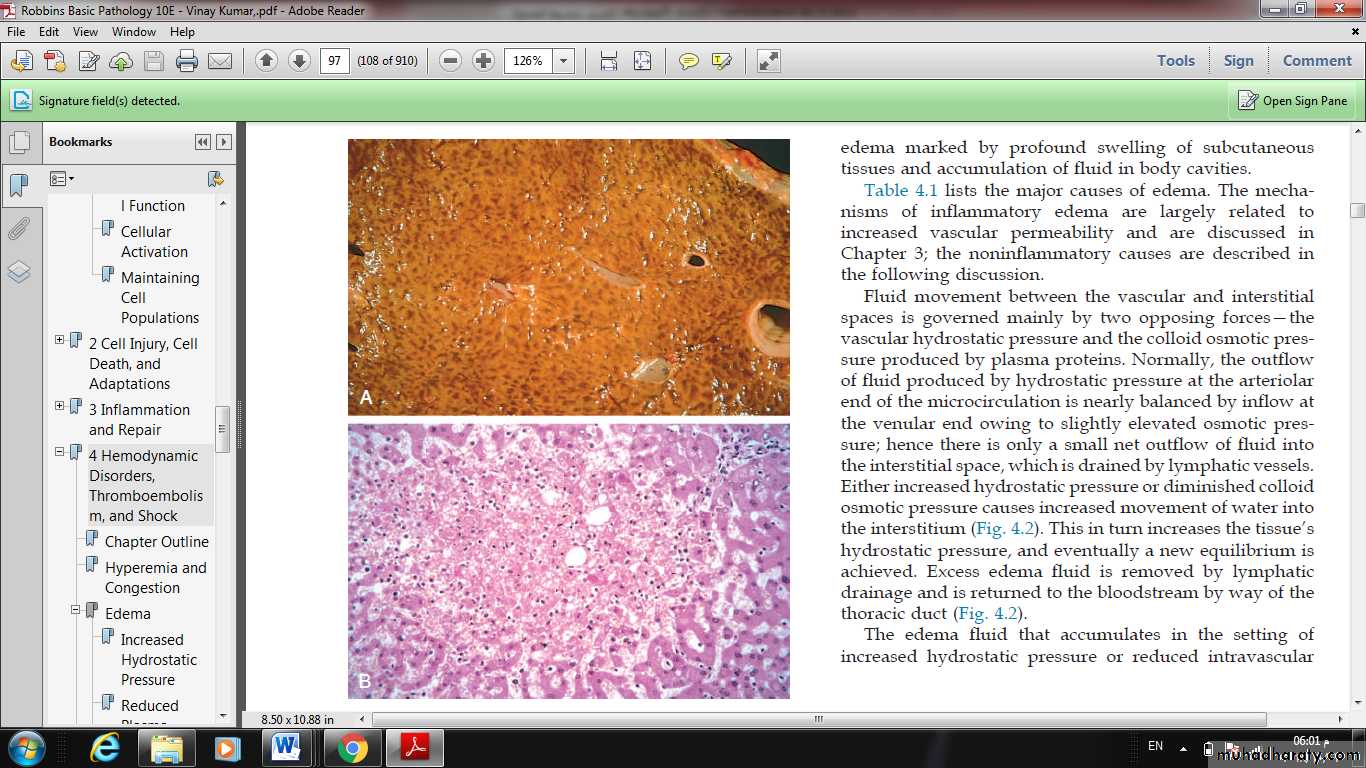
2-Chronic passive congestion of liver:
Gross examination the central regions of the hepatic lobules, viewed, are red-brown and slightly depressed (owing to cell loss) and are accentuated against the surrounding zones of uncongested tan, sometimes fatty, liver (nutmeg liver)
Microscopic findings include centrilobular hepatocyte necrosis, hemorrhage, and hemosiderin-laden macrophages.
Fig. Liver with chronic passive congestion and hemorrhagic necrosis.(A) In this autopsy specimen, central areas are red and slightly depressed compared with the surrounding tan viable parenchyma, creating “nutmeg liver” (so called because it resembles the cut surface of a nutmeg). (B) Microscopic preparation shows centrilobular hepatic necrosis with hemorrhage and scattered inflammatory cells.
Hemorrhage
Hemorrhage, defined as the extravasation of blood from vessels, is most often the result of damage to blood vessels or defective clot formation.capillary bleeding can occur in chronically congested tissues. Trauma, atherosclerosis, or inflammatory or neoplastic erosion of a vessel wall also may lead to hemorrhage, which may be extensive if the affected vessel is a large vein or artery.
The risk of hemorrhage is increased in a wide variety of clinical disorders collectively called hemorrhagic diatheses. These have diverse causes, including inherited or acquired defects in vessel walls, platelets, or coagulation factors, all of which must function properly to ensure homeostasis.
Hemorrhage may be manifested by different appearances and clinical consequences.
Hemorrhage may be external or accumulate within a tissue as a hematoma, which ranges in significance from trivial to fatal. Large bleeds into body cavities are described variously according to location—hemothorax, hemopericardium, hemoperitoneum, or hemarthrosis (in joints).
Petechiae are minute (1 to 2 mm in diameter) hemorrhages into skin, mucous membranes, or serosal surfaces ; causes include low platelet counts (thrombocytopenia), defective platelet function, and loss of vascular wall support, as in vitamin C deficiency.
Purpura are slightly larger (3 to 5 mm) hemorrhages.
Purpura can result from the same disorders that cause petechiae, as well as trauma, vascular inflammation (vasculitis), and increased vascular fragility.
Ecchymoses are larger (1 to 2 cm) subcutaneous hematomas (colloquially called bruises).
Extravasated red cells are phagocytosed and degraded by macrophages; the characteristic color changes of a bruise result from the enzymatic conversion of hemoglobin (red-blue color) to bilirubin (blue-green color) and eventually hemosiderin (golden-brown).The clinical significance of any particular hemorrhage
depends on:
the volume of blood that is lost
and the rate of bleeding. Rapid loss of up to 20% of the blood volume, or slow losses of even larger amounts, may have little impact in healthy adults; greater losses, however, can cause hemorrhagic (hypovolemic) shock
The site of hemorrhage also is important; bleeding that would be trivial in the subcutaneous tissues can cause death if located in the brain .
chronic or recurrent external blood loss (e.g., due to peptic ulcer or menstrual bleeding) frequently culminates in iron deficiency anemia as a consequence of a loss of iron in hemoglobin.
By contrast, iron is efficiently recycled from phagocytosed red cells, so internal bleeding (e.g., a hematoma) does not lead to iron deficiency.