Physiology Of blood
WBCs” Leucocyte”Lect. 6
Objectives:
• What are the WBC cells in our body?• Define their role in blood .
• Determine its type and function .
• Describe the pathological states of Leukocytosis & Leucopenia
The leukocytes, also called white blood cells, are the mobile units of the body’s protective system. They are formed partially in the bone marrow (granulocyte and monocytes ) and partially in the lymph tissue (lymphocytes and plasma cells).
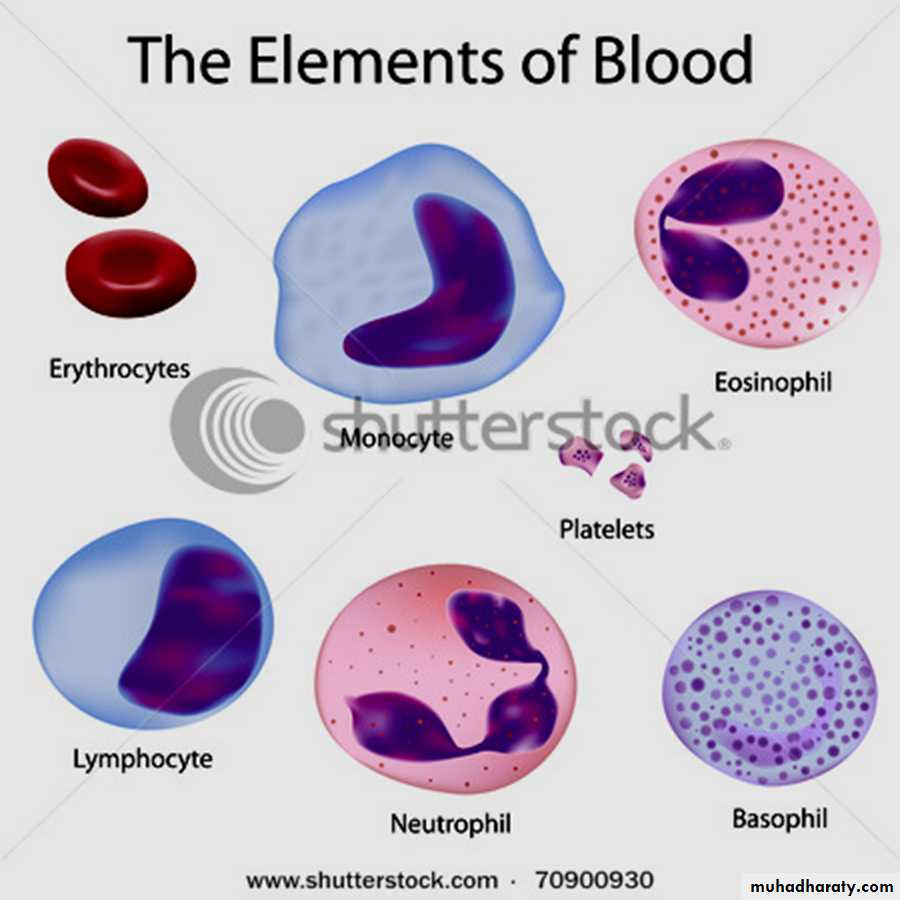
Six types of WBCs are normally present in the blood.
1.Polymorphonuclear Neutrophils they have granular cytoplasm2. Polymorphonuclear Eosinophils,
3.Polymorphonuclear Basophils,
4.Monocytes,
5.Lymphocytes, with the immune system..
6.Plasma cells.
***The granulocytes and monocytes protect the body against invading organisms mainly by ingesting them— phagocytosis.
WBCs are the colorless and nucleated formed elements of blood
Compared to RBCs, the WBCs are larger in size and lesser in number, have a role in defense mechanism of body and protect the body from invading organisms .The differences between WBCs and RBCs are:
• Larger in size.
• 2. Irregular in shape.
• 3. Nucleated.
• 4. Many types.
• 5. Granules are present in some type of WBCs.
• 6. Lifespan is shorter.
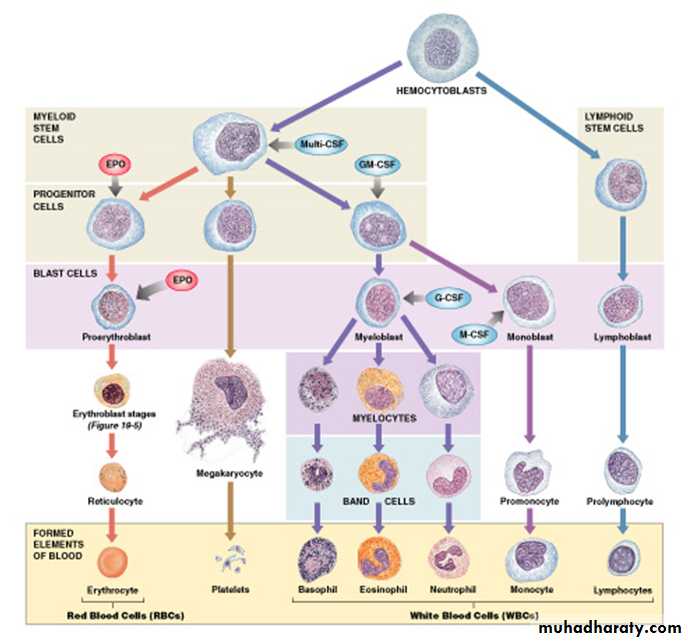
Origins and Differentiation of Formed Elements
All blood cells originate from hemocytoblasts:which produce myeloid stem cells and lymphoid stem cells
Myeloid Stem Cells
Differentiate into progenitor cells:
which produce all WBCs except lymphocytes
Lymphocytes
Are produced by lymphoid stem cells
Lymphopoiesis: the production of lymphocytes.
WBCs, except monocytes: develop fully in bone marrow i. e develop into macrophages in peripheral tissues
Hormones that regulate blood cell populations:
Colony-Stimulating Factors (CSFs)1. M-CSF: stimulates monocyte production
2. G-CSF: stimulates granulocyte production neutrophils, eosinophils, and basophils
3. GM-CSF: stimulates granulocyte and monocyte production
4. Multi-CSF: accelerates production of granulocytes, monocytes, platelets, and RBC
CLASSIFICATION
Based on the presence or absence of granules in the cytoplasm, the leukocytes are classified into two groups:
• Granulocytes which have granules.
• Agranulocytes which do not have granules
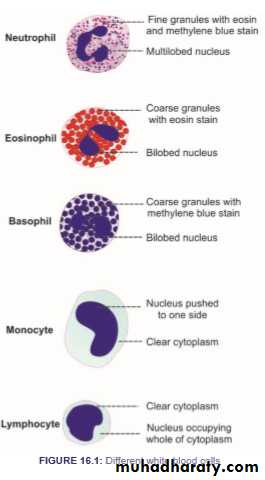
**Granulocytes
Depending upon the staining property of granules, the granulocytes are classified into three types:
i. Neutrophils with granules taking both acidic and basic stains.
ii. Eosinophils with granules taking acidic stain.
iii. Basophils with granules taking basic stain.
** Agranulocytes have plain cytoplasm without granules are of two types:
• Monocytes.
• ii. Lymphocytes
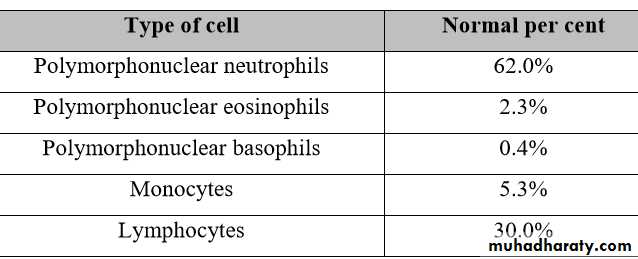
Concentrations of the Different White Blood Cells in the Blood.
The adult human being has about 7000 white blood cells per microliter of blood (in comparison with 5 million red blood cells). Of the total white blood cells, the normal percentages of the different types are approximately the following:Circulating WBCs
Migrate out of bloodstreamHave amoeboid movement
Attracted to chemical stimuli (positive chemotaxis)
Some are phagocytic: as neutrophils, eosinophils, and monocytes
Life Span of the White Blood Cells
The life of the granulocytes after being released from the bone marrow is normally 4 to 8 hours circulating in the blood and another 4 to 5 days in tissues where they are needed.The monocytes have a short time, 10 to 20 hours in the blood. Once in the tissues, they swell to much larger sizes to become tissue macrophages, can live for months unless destroyed while performing phagocytic functions.
• It is mainly the neutrophils and tissue macrophages that attack and destroy invading bacteria, viruses, and other injurious agents by a phagocytosis, which means cellular ingestion of the offending agent. The neutrophile has a lysosomal enzymes & bactericides (hydrogen peroxide and superoxide)
The macrophage are much more powerful phagocytes than neutrophils, often capable of phagocytizing as many as 100 bacteria with the ability to engulf much larger particles, even whole RBCs or, occasionally, malarial parasites, whereas neutrophils are not capable of phagocytizing particles much larger than bacteria.
• Eosinophils are weak phagocytes, they are produced in large numbers in people with parasitic infections, and they migrate in large numbers into tissues diseased by parasites , and allergic reactions as in bronchial tissues of the lungs in people with asthma
• The basophils play an important role in some types of allergic reactions that its release histamine, bradykinin and serotonin . basophils liberate heparin into the blood, a substance that can prevent blood coagulation
• The mast cells and basophils play an important role in some types of allergic reaction because the type of antibody that causes allergic reactions, the immunoglobulin E (IgE) type, has a special propensity to become attached to mast cells and basophils.
Lymphocytes enter the circulatory system continually, the lymphocytes have life spans of weeks or months; this depends on the body’s need for these cells. 3 Types :
1-T cells Cell-mediated immunity ( Attack foreign cells directly)
2- B cells Humoral immunity (Differentiate into plasma cells (activated B cells that secrete antibodies)
3-Natural killer (NK) cells Detect and destroy abnormal tissue cells (cancers)
PHYSIOLOGICAL VARIATIONS
1. Age:WBC count is about 20,000 per cu mm in infants and about 10,000 to 15,000 per cu mm of blood in children. In adults, it ranges between 4,000 and 11,000 per cu mm of blood.
2. Sex: Slightly more in males than in females.
3. Diurnal variation: Minimum in early morning and maximum in the afternoon.
4. Exercise: Increases slightly.
5. Sleep: Decreases.
6. Emotional conditions like anxiety: Increases.
7. Pregnancy: Increases.
8. Menstruation: Increases.
• NORMAL WHITE BLOOD CELL COUNT
• Total WBC count : 4,000 to 11,000/cu mm of blood. PATHOLOGICAL VARIATIONS
All types of leukocytes do not share equally in the increase or decrease of total leukocyte count. In general, the neutrophils and lymphocytes vary in opposite directions.
Leukocytosis occurs in conditions such as:
1.Infections 2. Allergy 3. Common cold 4. Tuberculosis 5. Glandular fever.
• Leukopenia is the decrease in the total WBC count , occurs in :
• 1. Anaphylactic shock 2. Cirrhosis of liver 3. Disorders of spleen 4. Pernicious anemia 5. Typhoid and paratyphoid 6. Viral infections
Granulocytosis
Granulocytosis is the abnormal increase in the number of granulocytes.
Granulocytopenia
Granulocytopenia is the abnormal reduction in the number of granulocytes.
Leukemia is the condition which is characterized by abnormal and uncontrolled increase in leukocyte count more than 1,000,000/cu mm. It is also called blood cancer.
Mechanism of Defense of Neutrophils & Monocytes Against Infection
Neutrophils & monocytes attack & destroy invading organisms like bacteria, virus or other foreign agents.The mechanism of destruction of bacteria include:
1. Margination: Sticking of leukocytes to endothelial cells in the capillary wall.
2. Diapedesis: Squeezing of leukocytes through capillary wall.
3. Amoeboid motion: Movement of leukocytes in the tissue with speed up to 40 μ/min
4.Chemotaxis: Movement of the leukocytes to the site of infection by the effect of different substances like: bacterial toxins, degenerative substances of tissue,
reactive products of complement (C5a) & clotting system, leukotrienes & polypeptide for lymph.
Chemotaxis depends on concentration gradient of chemical substance which is effective up to 100 μm away from site of inflammation.
Movement of neutrophils by diapedesis through capillary pores and by chemotaxis toward an area of tissue damage
• البلعمة 5.Phagocytosis:
• (ingestion of the offending agent) cell to be phagocytized:
• a) Devoted from protective protein (Dead cell & foreign particles).
• b) Some cells are recognized by Antibody adhere to bacteria with complement proteins
• الهاضمة(Opsonization )
• Mechanism of phagocytosis
• ➢the neutrophil first attaches itself to the particle (attachment of bacteria on Ab-Ag complex to cell).
• ➢Project of pseudopodia around particles then fused to form phagosome (vesicle).
• ➢Enzymatic digestion of phagocytized particles
• ❖Lysosome fuse to vesicle to release digestive enzymes like proteolytic enzymes with sharp rise in
• O2 uptake with respiratory burst.
• ❖ Macrophages also contain lipases to digest lipid membrane of TB.
• ❖If bacteria cannot be digested so it will be killed by oxidizing agent as superoxide (O2), hydrogen
• peroxide (H2O2) & hydroxyl on (OH
• Neutrophils are mature WBC can start phagocytosis of bacteria immediately, up to 20 bacteria can be phagocytized before inactivation & death.
• ➢Monocytes are immature, then as they go to tissue swollen to 5x its diameter (80 μ) & develop lysosomes & mitochondria in cytoplasm to be macrophage,➢as activated by immune system they become powerful > than neutrophil (up to 100 bacteria), dead neutrophil, necrotic tissue, malarial parasite & even RBC can be engulfed and then can extrude the residual products
Monocyte – macrophage system (Reticuloendothelial system):
➢It represented by combination of monocytes, mobile macrophages, fixed tissue macrophages and a few specialized endothelial cells in B.M., spleen, and lymph nodes.Tissue macrophages
➢in skin called Histiocytes.
➢in spleen, lymph node & Bone.Marrow called Tissue macrophages.
➢in liver called Kupffer cells.
➢in Lung called Alveolar cells.
➢in Brain called Microglial cells
Inflammation
➢Local changes in the tissues due to the release of chemical substances like (histamine, bradykinin, serotonin, prostoglandin, blood clotting products, complement system products, lymphokines & others), which strongly activate the macrophage system.
➢These substances released as a result of tissue damage by injury, trauma, bacterial or viral infection, heat & chemical substance.
Response of neutrophils & monocytes to inflammation:
1. Tissue Macrophage is the first line of defense against infection : within minutes after inflammation begins; Tissue macrophages start their phagocytic effect). Their numbers are not great, but they are life saving.
2. Neutrophil invasion of the inflamed area is a second line of defense: within the first hour or so after inflammation begins, large numbers of neutrophils begin to invade the inflamed area from the blood. This is caused by inflammatory
cytokines (e.g., TNF, IL-1) and other biochemicalsubstance produced by the inflamed
tissues.
3.Second Macrophage Invasion into the Inflamed Tissue Is a Third Line of Defense:
•Migration of (immature) monocytes to inflammatory area to become (mature) macrophages. Its maturation needs 8-12 hours.
4. Great increase in production of both granulocytes and monocytes by the Bone Marrow.
This results from stimulation of the granulocytic and monocytic progenitor cells of the marrow by factors released mainly by macrophages. It takes 3 to 4 days before newly formed granulocytes and monocytes reach the stage of leaving the Bone Marrow.
Cardinal Signs & Symptoms of Inflammation (clinically)
➢Hot
➢Redness
➢Swelling
➢Pain
➢Loss of Function