THE LARYNX Larynx is a specialized organ responsible for production of voice. It houses the vocal cords. The wall of the larynx has a complex structure made up of a number of cartilages, membranes and muscles.
1-Mucous Membrane The epithelium lining the mucous membrane of the larynx is predominantly pseudo-stratified ciliated columnar. However, over some parts that come in contact with swallowed food the epithelium is stratified squamous. These parts include the epiglottis (anterior surface and upper part of the posterior surface), and the upper parts of the aryepiglottic folds. The vocal folds do not come in contact with swallowed food, but their lining epithelium is exposed to considerable stress during vibration of the folds. These folds are also covered with stratified squamous epithelium. Serous glands and lymphoid tissue are also present.
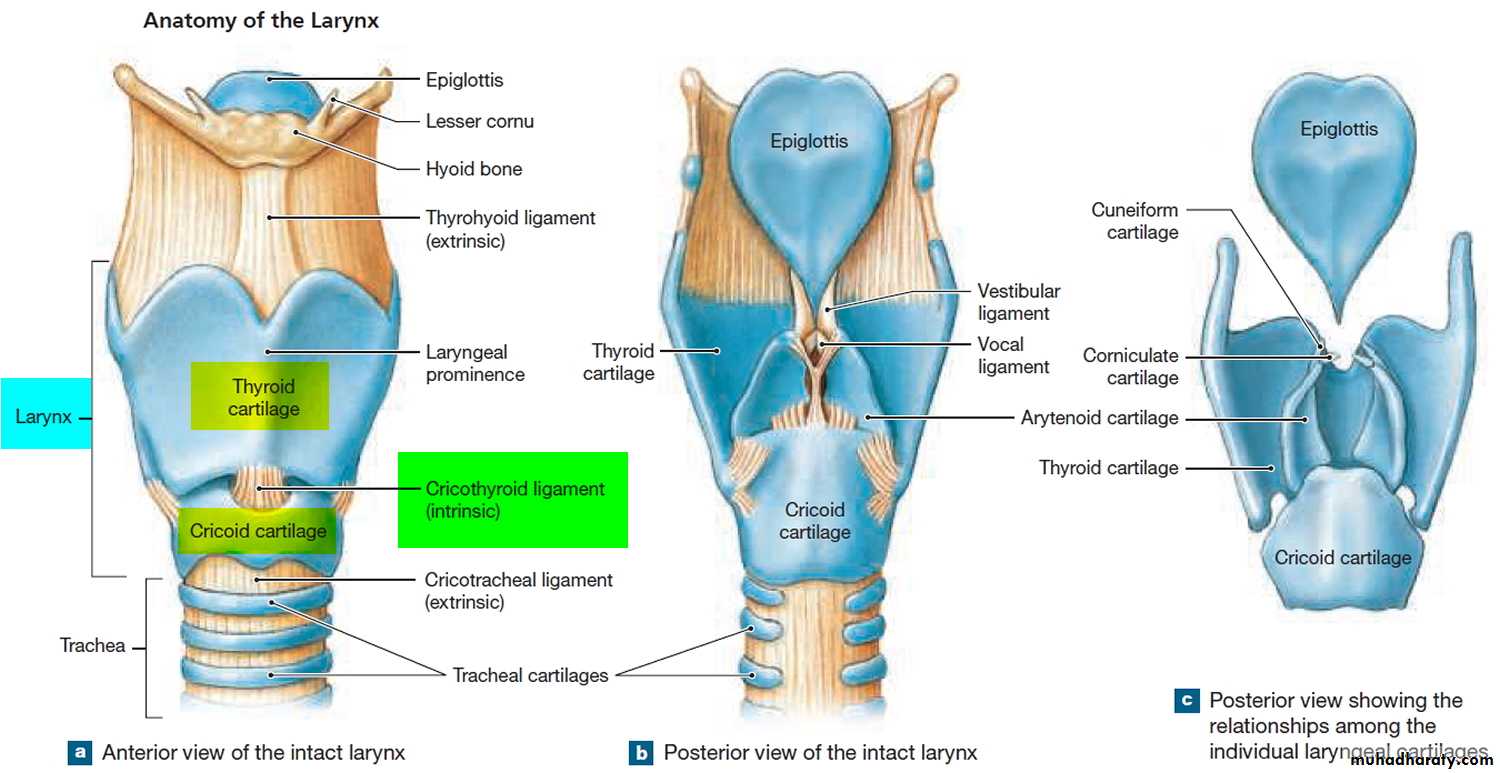
2- Cartilages of the Larynx The larynx has a cartilaginous framework which is made of nine cartilages (3 paired and 3 unpaired) that are connected to each other by membranes and ligaments. The cartilages are either hyaline or elastic in nature. These are: 1- Hyaline cartilages a- Thyroid (unpaired) b- Cricoid (unpaired) c- Arytenoid (paired)
2- Elastic cartilages a- Epiglottis (unpaired) b- Cuneiform (paired) c- Corniculate (paired) With advancing age, calcification may occur in hyaline cartilage, but not in elastic cartilage.
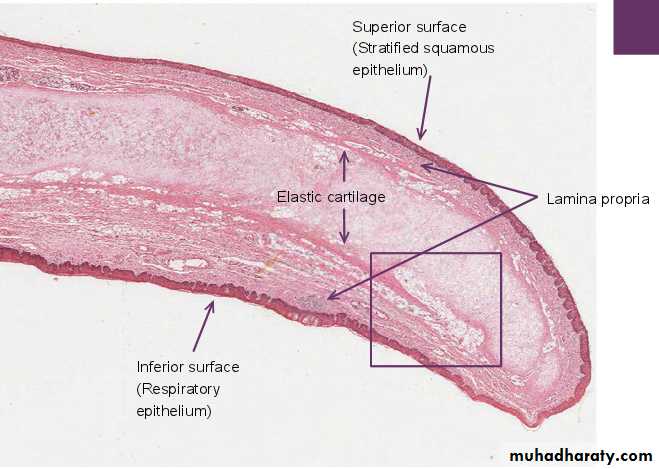
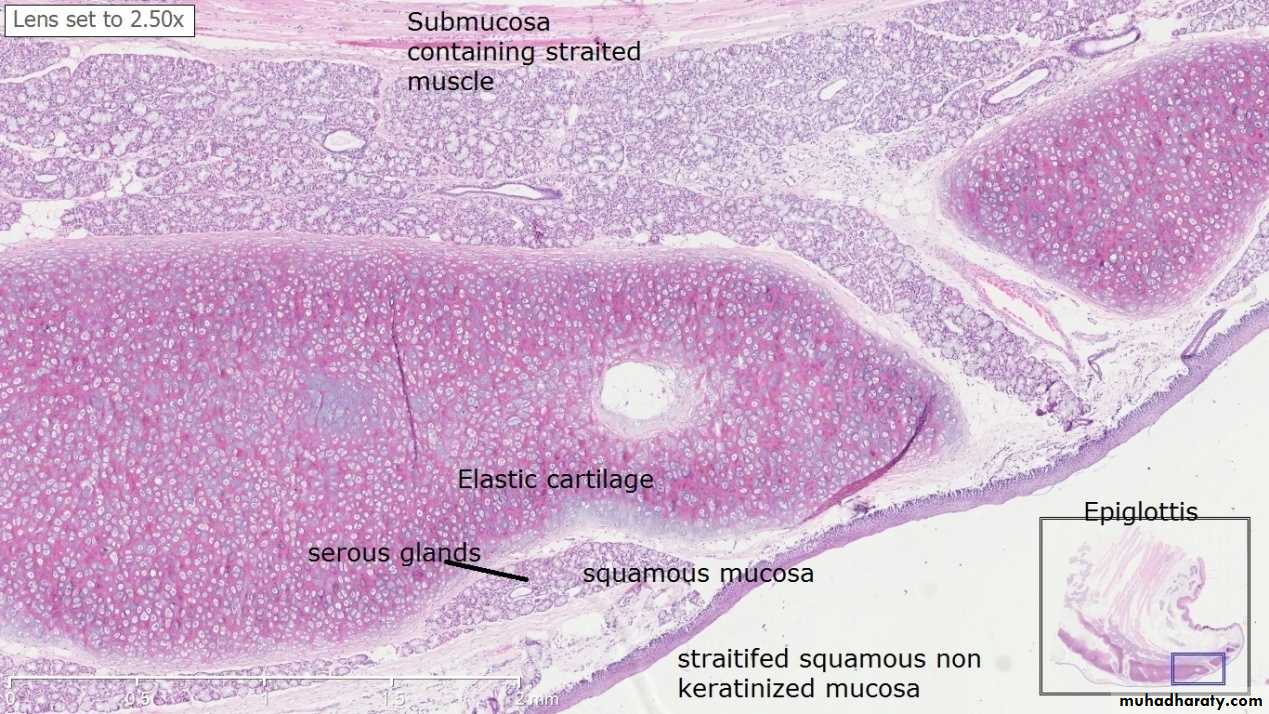
The Epiglottis The epiglottis is considered separately because sections through it are usually included in sets of class slides. The epiglottis has a central core of elastic cartilage. Overlying the cartilage there is mucous membrane. The greater part of the mucous membrane is lined by stratified squamous epithelium (non-keratinizing). The mucous membrane over the lower part of the posterior surface of the epiglottis is lined by pseudo-stratified ciliated columnar epithelium . This part of the epiglottis does not come in contact with swallowed food as it is overlapped by the aryepiglottic folds. Numerous glands, predominantly mucous, are present in the mucosa deep to the epithelium. Some of them lie in depressions present on the epiglottic cartilage.
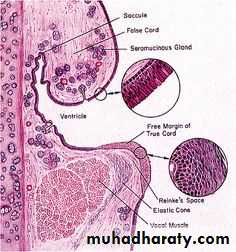
Below the epiglottis and laryngeal vestibule, the mucosa projects into the lumen bilaterally with two pairs of folds separated by a narrow space or ventricle. The upper pair, the immovable vestibular folds, is partly covered with typical respiratory epithelium overlying numerous seromucous glands and occasional lymphoid nodules. The lower pair of folds, the vocal folds (or cords), have features important for phonation or sound production is lined by non keratinizing squamous epithelium .
THE TRACHEA AND PRINCIPAL BRONCHI The trachea is a fibro-elastic cartilaginous tube. It extends from the lower border of cricoid cartilage to its level of bifurcation into right and left bronchi. The trachea consists of four layers :
1-Mucosa : The lumen of the trachea is lined by mucous membrane that consists of a lining epithelium and an underlying layer of connective tissue. The lining epithelium is pseudo stratified ciliated columnar. It contains numerous goblet cells, and basal cells that lie next to the basement membrane. Numerous lymphocytes are seen in deeper parts of the epithelium.
2- Submucosa The sub-epithelial connective tissue contains numerous elastic fibers. It contains serous glands that keep the epithelium moist; and mucous glands that provide a covering of mucous in which dust particles get caught. The mucous is continuously moved towards the larynx by ciliary action. Numerous aggregations of lymphoid tissue are present in the sub-epithelial connective tissue. Eosinophil leucocytes are also present.
3- Cartilage and Smooth Muscle Layer The skeletal basis of the trachea is made up of 16 to 20 tracheal cartilages. Each of these is a C-shaped mass of hyaline cartilage. The open end of the ‘C’ is directed posteriorly. Occasionally, adjoining cartilages may partly fuse with each other or may have Y-shaped ends. The intervals between the cartilages are filled by fibrous tissue that becomes continuous with the perichondrium covering the cartilages. The gaps between the cartilage ends, present on the posterior aspect, are filled in by smooth muscle and fibrous tissue. The connective tissue in the wall of the trachea contains many elastic fibers.
4- Adventitia It is made of fibroelastic connective tissue containing blood vessels and nerves.
Principal Bronchi The trachea divides at the level of T4 into right and left principal bronchi (primary or main bronchi). They have a structure similar to that of the trachea.
THE LUNGS The lungs are the principal respiratory organs that are situated one on either side of mediastinum in the thoracic cavity, they are covered by visceral pleura.
The structure of the lungs has to be understood keeping in mind their function of oxygenation of blood. The following features are essential for this purpose.
A surface at which air (containing oxygen) can be brought into close contact with circulating blood. The barrier between air and blood has to be very thin to allow oxygen (and carbon dioxide) to pass through it, the surface has to be extensive enough to meet the oxygen requirements of the body.
A system of tubes to convey air to and away from the surface at which exchanges take place.
A rich network of blood capillaries present in intimate relationship to the surface at which exchanges take place.
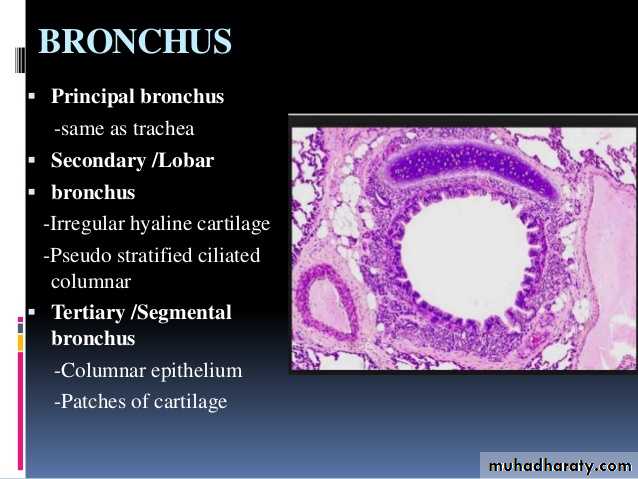
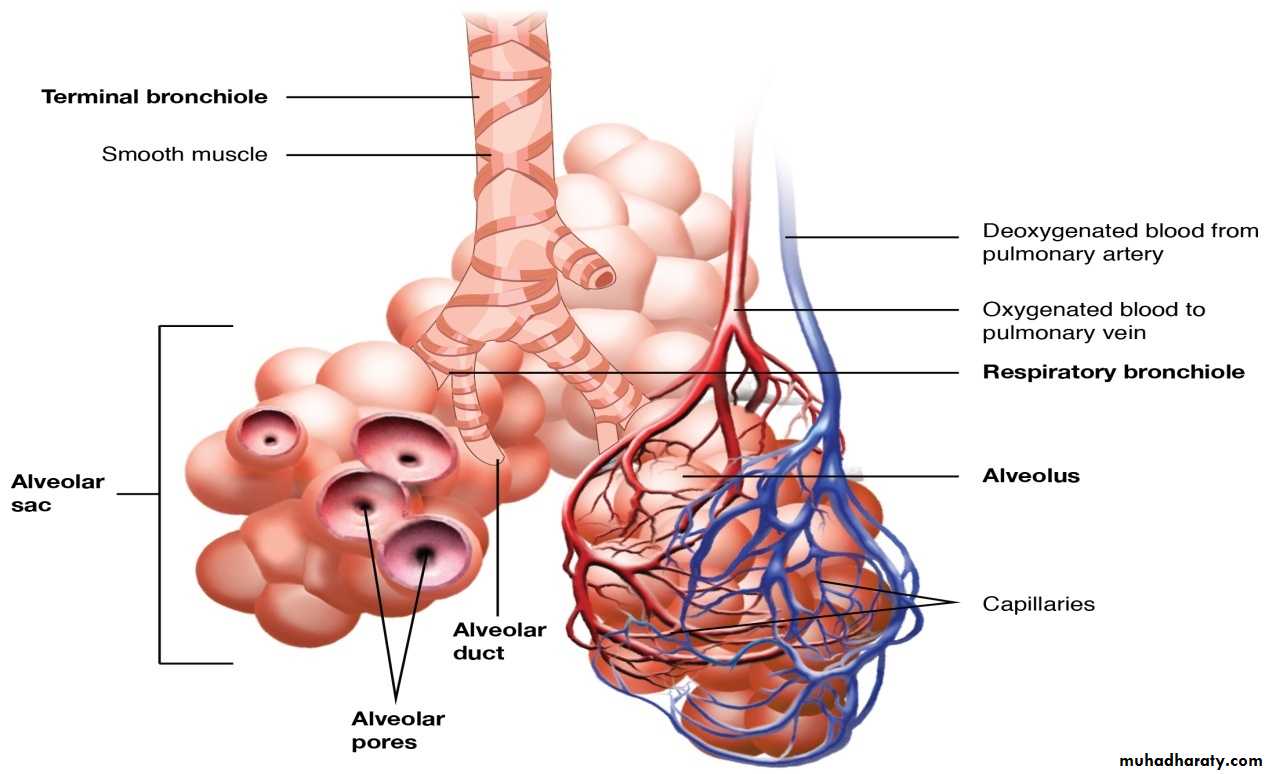
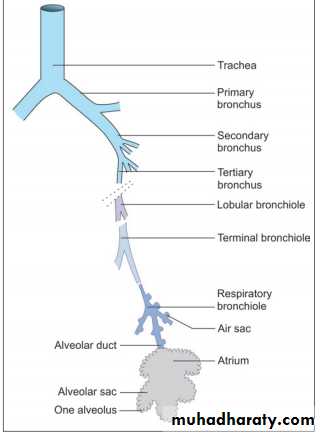
Intrapulmonary Passages On entering the lung the principal bronchus divides into secondary, or lobar bronchi (one for each lobe). Each lobar bronchus divides into tertiary, or segmental bronchi (one for each segment of the lobe). The segmental bronchi divide into smaller and smaller bronchi, which ultimately end in bronchioles. The lung substance is divided into numerous lobules each of which receives a lobular bronchiole. The lobular bronchiole gives off a number of terminal bronchioles indicated by their name the terminal bronchioles represent the most distal parts of the conducting passage. Each terminal bronchiole ends by dividing into respiratory bronchioles. These are so called because they are partly respiratory in function as some air sacs arise from them. Each respiratory bronchiole ends by dividing into a few alveolar ducts. Each alveolar duct ends in a passage, the atrium, which leads into a number of rounded alveolar sacs. Each alveolar sac is studded with a number of air sacs or alveoli.
The alveoli are blind sacs having very thin walls through which oxygen passes from air into blood, and carbon dioxide passes from blood into air. The structure of the larger intrapulmonary bronchi is similar to that of the trachea. As these bronchi divide into smaller ones the following changes in structure are observed.
The cartilages in the walls of the bronchi become irregular in shape, and are progressively smaller. Cartilage is absent in the walls of bronchioles: this is the criterion that distinguishes a bronchiole from a bronchus.
The amount of muscle in the bronchial wall increases as the bronchi become smaller. The presence of muscle in the walls of bronchi is of considerable clinical significance. Spasm of this muscle constricts the bronchi and can cause difficulty in breathing.
Sub-epithelial lymphoid tissue increases in quantity as bronchi become smaller. Glands become fewer, and are absent in the walls of bronchioles.
The trachea and larger bronchi are lined by pseudostratified ciliated columnar epithelium. As the bronchi become smaller the epithelium first becomes simple ciliated columnar, then non-ciliated columnar, and finally cuboidal (in respiratory bronchioles) .