Hypertension
Epidemiology of Hypertension
By 2001, CVD had become the leading cause of death in the developing world, as it has been in the developed world since the mid 1900s (WHO).It is estimated world-wide that 45% of adults have mean SBP equal to or greater than 140 mmHg.
Leading CVD Risk Factors
HTNCigarette Smoking
Hyperlipidemia
Obesity
Inactivity
Diabetes
Lifestyle Modifications to Prevent and/or Manage HTN
• Modification• Recommendations
• Approximate Systolic
• Blood Pressure Reduction
• 1- Weight Reduction
• Maintain normal body weight (BMI 18.5-24.9)
• 5-20 mm Hg for each 10 kg weight loss
• 2- Adapt healthy eating plan
• Consume diets rich in fruits, vegetables, low fat dairy and low saturated fat
• 8-14 mm Hg
• 3- Dietary sodium reduction
• Reduce sodium to no more than 2.4 g/day sodium or 5 g/day NaCl
• 2-8 mm Hg
• 4- Increase physical activity
• Engage in regular aerobic activity such as brisk walking (30 min/day on most days)
• 4-9 mm Hg
• 5- Stop alcohol consumption
• >4 mm Hg
Source: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure JNCVII. JAMA. 2003;289:2560-2572.
Diagnostic Workup
• Initial Drug Therapy
• BP Classification• SBP* (mm Hg)
• DBP* (mm Hg)
• Lifestyle Modification
• Without Compelling Indications
• With Compelling Indications
• Normal
• <120• and <80
• Encourage
• No antihypertensive drug indicated.
• Drug(s) for compelling indications.
• Prehypertension
• 120–139
• or 80–89
• Yes
• Stage 1 hypertension
• 140–159• or 90–99
• Yes
• Thiazide-type diuretic for most. May consider ACEI, ARB, BB, CCB, or combination.
• Drug(s) for compelling indications.
• Other antihypertensive drugs (diuretic, ACEI, ARB, BB, CCB) as needed.• Stage 2 hypertension
• ³160
• or ³100
• Yes
• Two-drug combination for most (usuallythiazide-type diuretic and ACEI or ARB or BB or CCB).
Classification and Management of Blood Pressure for Adults
JNC 7. 2003. NIH publication 03-5233.
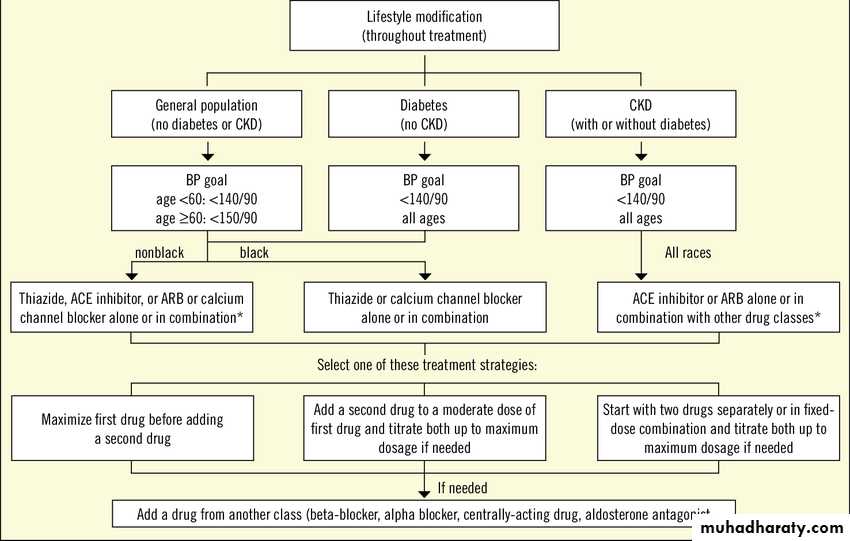
Treatment algorithm adopted from JNC 8 hypertension guideline 2014
Compelling Indications
Heart FailurePost- Myocardial Infarction
High CVD risk
DM
Chronic Renal Failure
Stroke
Failure of Patient Education
50% of patients discontinue their anti-hypertensive within 1 year of initiating treatment.
Healthy diet for hypertension:
limit sodium
Increase fruits and vegetables (8-10/d)
Increase low fat dairy (3-4/d)
Need to focus on diet history and advice for hypertensive patients
Key Diet History Questions for Patients with HTN
Do you use a salt shaker?Do you taste your food before you add salt?
How often do you eat salty foods, such as chips, pretzels, salted nuts, canned and smoked foods?
Do you read labels for sodium content?
How many servings of fruits and vegetables do you eat everyday?
How often do you eat or drink dairy products? What kind?
How often do you eat out? What kinds of restaurants?
Do you drink alcohol?
How often do you exercise, including walking?
Special Populations
Women:Aged:
Estrogen containing oral contraceptives elevate BP. Aldomet, BB, and vasodilators OK in pregnancyHigher prevalence, more frequent complications from ACE, CCB
Stroke
What is stroke?
A neurological event following an interruption in blood flow due toThrombus/embolus (70%)
Hemorrhage (27%)
Hypotension, other unknown causes (3%)
Epidemiology of stroke
Stroke is one of the leading causes of mortality and morbidity, as well as long-term disability and hospital admission._ 15% of strokes are immediately fatal
_ 50% result in long-term patient care
_ 35% recover completely or with minor impairments.
Morbidity:
Prevalence 100 –600 per 100 000 adult population
At early ages more males are affected than females.
Mortality:
10– 90 per 100 000 adult population
Third leading cause of death in the developed countries.
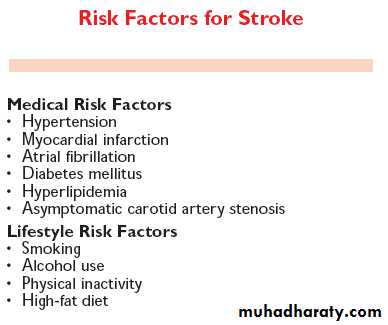
Risk factors modifiable by primary prevention
Non-modifiable risks ?
Medical risk factors modifiable by primary prevention I
HTN: RR (Relative Risk)of stroke in untreated hypertensive (>140/90) is 1.2 – 4.0MI: Risk of stroke increases 30% in the first month post-MI, then 1-2% each year after that.
AF: strong independent risk for ischemic stroke (RR = 5). 70% are cardioembolic, 30% are ‘other-embolic’. Stroke risk in untreated AF is 6% per year. AF double the risk of death after stroke.
Note that only high-risk strategy or 20 prevention can deal with MI or AF.
Increased RBCs
Medical risk factors modifiable by primary prevention II
DMIncreased RR of 1.4-1.7
Glycemic control may not help
Hypercholesterolemia: those with TC>240, when treated, had decreased RR of 0.7
Carotid artery stenosis: isolated risk factor
Only 33% of significant stenosis = bruit
Only 60% of bruits = significant stenosis
Risk of same-side stroke is 2% after CEA
Lifestyle risk factors modifiable by primary prevention I
SmokingRisk of stroke doubles with each pack
Risk of stroke returns to baseline 2-5 yrs after quitting
Alcohol drinking
Increase risk of stroke and risk of death after strokeLifestyle risk factors modifiable by primary prevention II
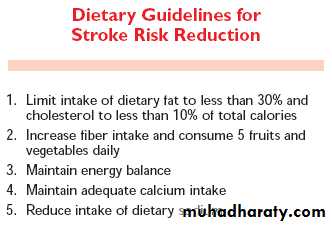
DietSpecial populations
WomenAfter 65 years, more women than men have stroke
Why? Under-treatment, increased risk of HTN
Use of OCs esp. in conjunction with smoking and HTN is a risk factor
OCs + HTN = RR 10.7
OCs + smoking=7.2
Newer OCs + <35y.o. + no HTN = no increased risk.
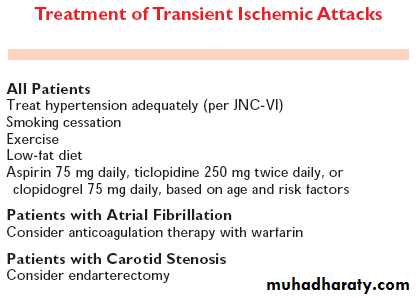
Secondary prevention for special populations: TIA
Focal neurologic deficit (e.g., hemiparesis, slurred speech, diplopia, ataxia) resolving in 24 hours (60-70% within 1 hour)Usual cause: temporary ischemia from emboli, vasospasm, hypotension.
Stroke Units
• Early admission of most patients to a unit that has a specialized interest in the treatment of stroke is strongly recommended• A team of physicians, nurses, and technicians devoted to the early care of patients with stroke should be assembled
• Rapid transfer of a patient to a hospital that has a specialized stroke care unit is strongly recommended.
•
Stroke and TPA (Tissue Plasminogen Activator)
Hospital treatment of thrombotic strokeTPA within 3 hours minimizes stroke size and decreases disability at 3 months
TPA May cause bleeding (carefully consider contraindication)
Later on, heparin or heparinoids may be considered for non-hemorrhagic stroke.
Post-stroke care I
Post-stroke concerns frequently managed by family physicians:Secondary prevention including modification of risk factors
Dealing with organic brain syndromes, e.g., depression, mania, dementia
Risk factor: family history of psychiatric disorder
Depression associated with 3-year mortality increase of 350%.
Post-stroke care II: Rehabilitation
Rehab. should begin soon after the patient is stable (ideally, within 48hrs). Early mobilization and measures to prevent the sub-acute complications of stroke (aspiration, malnutrition, pneumonia, deep vein thrombosis, pulmonary embolism, bed ulcers, contractures, and joint abnormalities) are strongly recommendedEarly rehab. aids early return to normal daily life.
A Prehospital Stroke Scale
Accurate in identifying patients with stroke
An abnormal finding in ANY of the three tests strongly suggests a stroke
• Test• Normal
• Abnormal
• facial droop
• both sides of the face move equally
• one side of the face does not move as well as the other
• arm drift
• both arms move the same or both arms do not move at all (palms up, eyes closed)
• one arm drifts down compared to the other or one arm does not move
• speech
• patient says correct words with no slurring of words
• patient slurs words, says the wrong words, or is unable to speak