
The Oral Cavity
Firas Al-Hameed
Thi-Qara Medical School
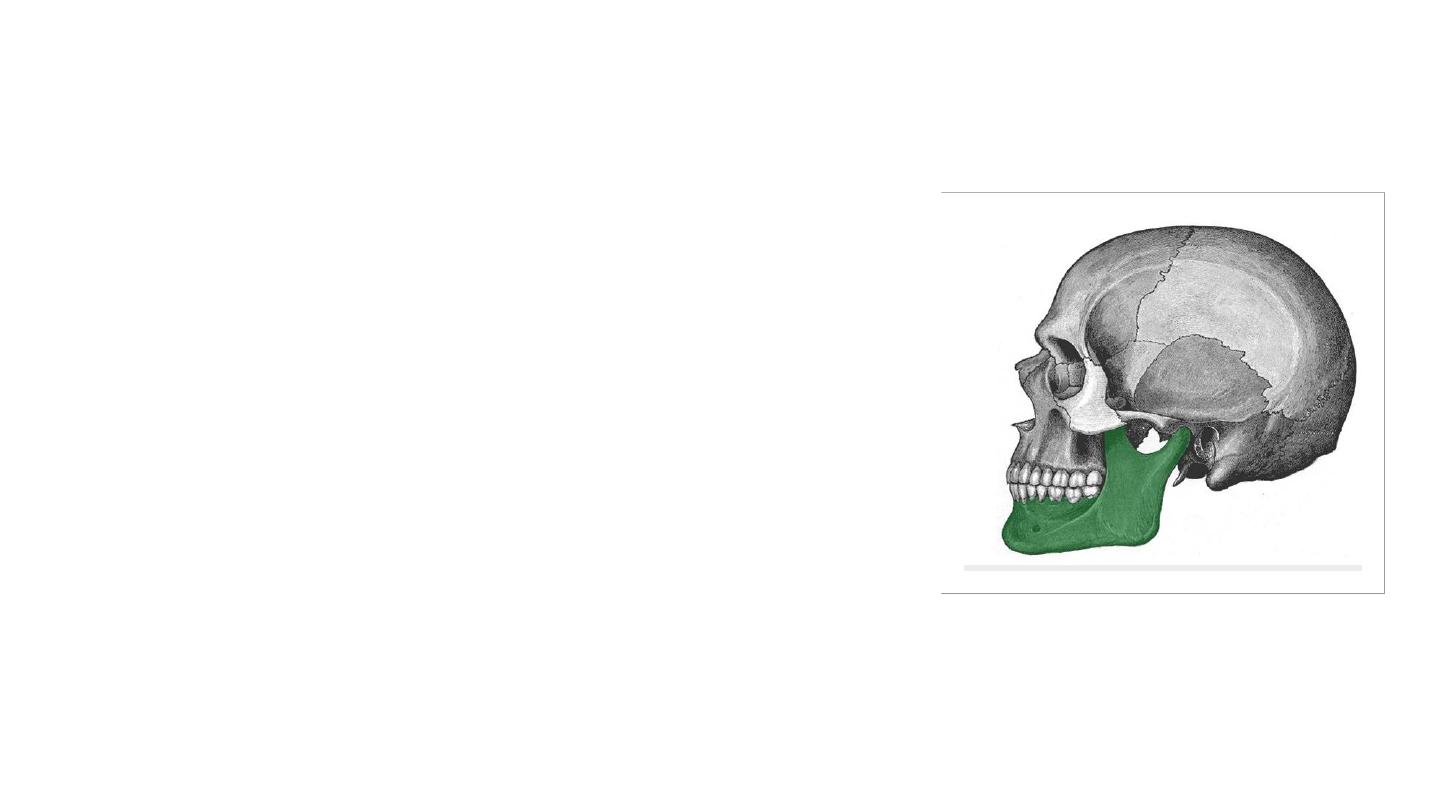
The Mandible
• Is the largest and strongest bone of the face.
• It also articulates on either side with the
temporal bone, forming the
temporomandibular joint.
• Consists of:
• Horizontal body (anteriorly) and two vertical rami
(posteriorly).
• The body and the rami meet on each side at the
angle of the mandible.
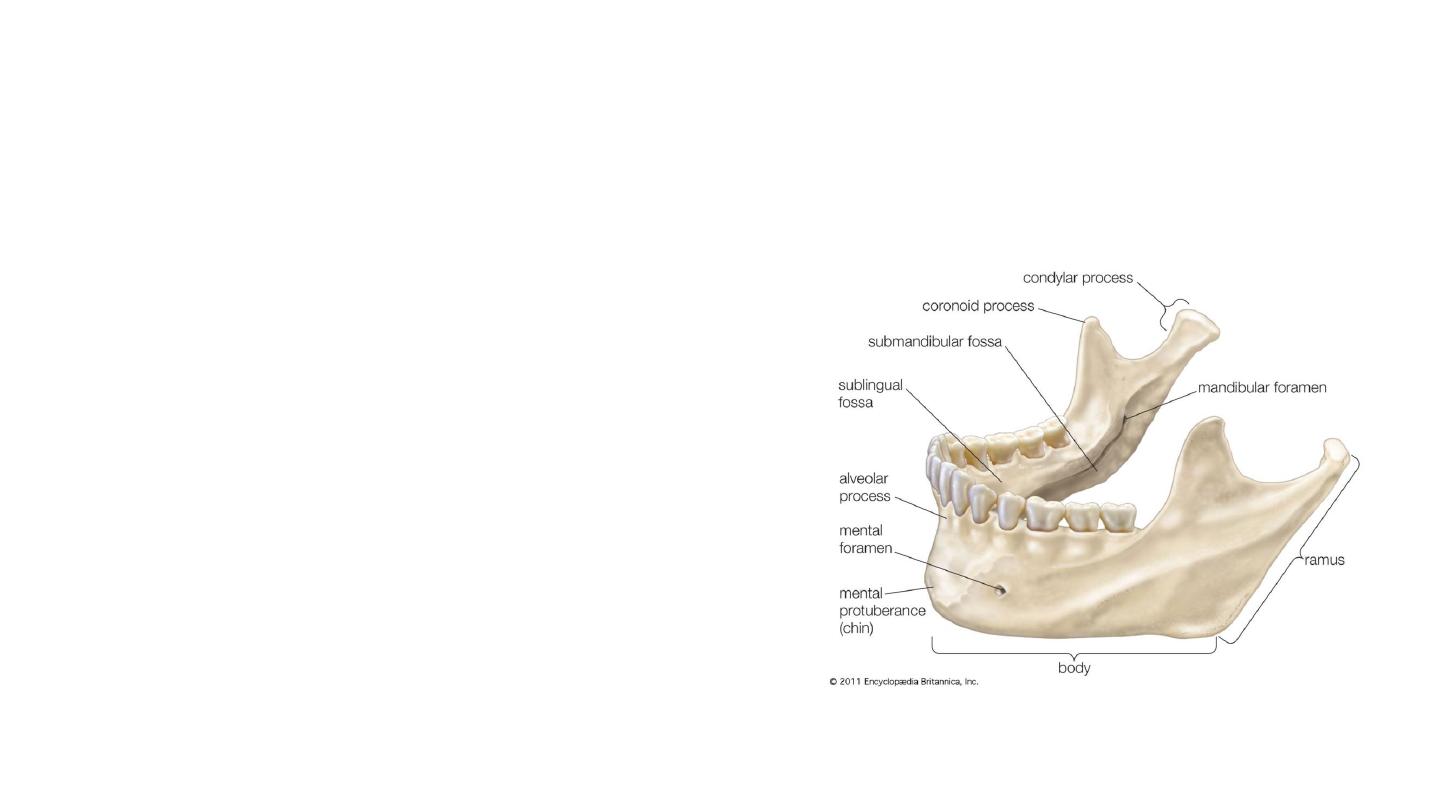
• The body has two borders:
• Alveolar border (superior) – contains 16 sockets
to hold the lower teeth.
• Base (inferior) – site of attachment for the
digastric muscle medially
• The body is marked in the midline by the
mandibular symphysis. This is a small ridge of
bone that represents the fusion of the two halves
during development
• Rami (2)
• Head (ccondyle) – situated posteriorly, and
articulates with the temporal bone to form the
temporomandibular joint.
• Neck – supports the head of the ramus, and site
of attachment of the lateral pterygoid muscle.
• Coronoid process – site of attachment of the
temporalis muscle

Foramina of the mandible
• The mandibular foramen is located on the internal surface of the
ramus of the mandible. It serves as a conduit for the inferior alveolar
nerve and inferior alveolar artery.
• The mental foramen is positioned on the external surface of the
mandibular body, below the second premolar tooth. It allows the
inferior alveolar nerve and artery to exit the mandibular canal. When
the inferior alveolar nerve passes through the mental foramen, it
becomes the mental nerve (innervates the skin of the lower lip and
the front of the chin).
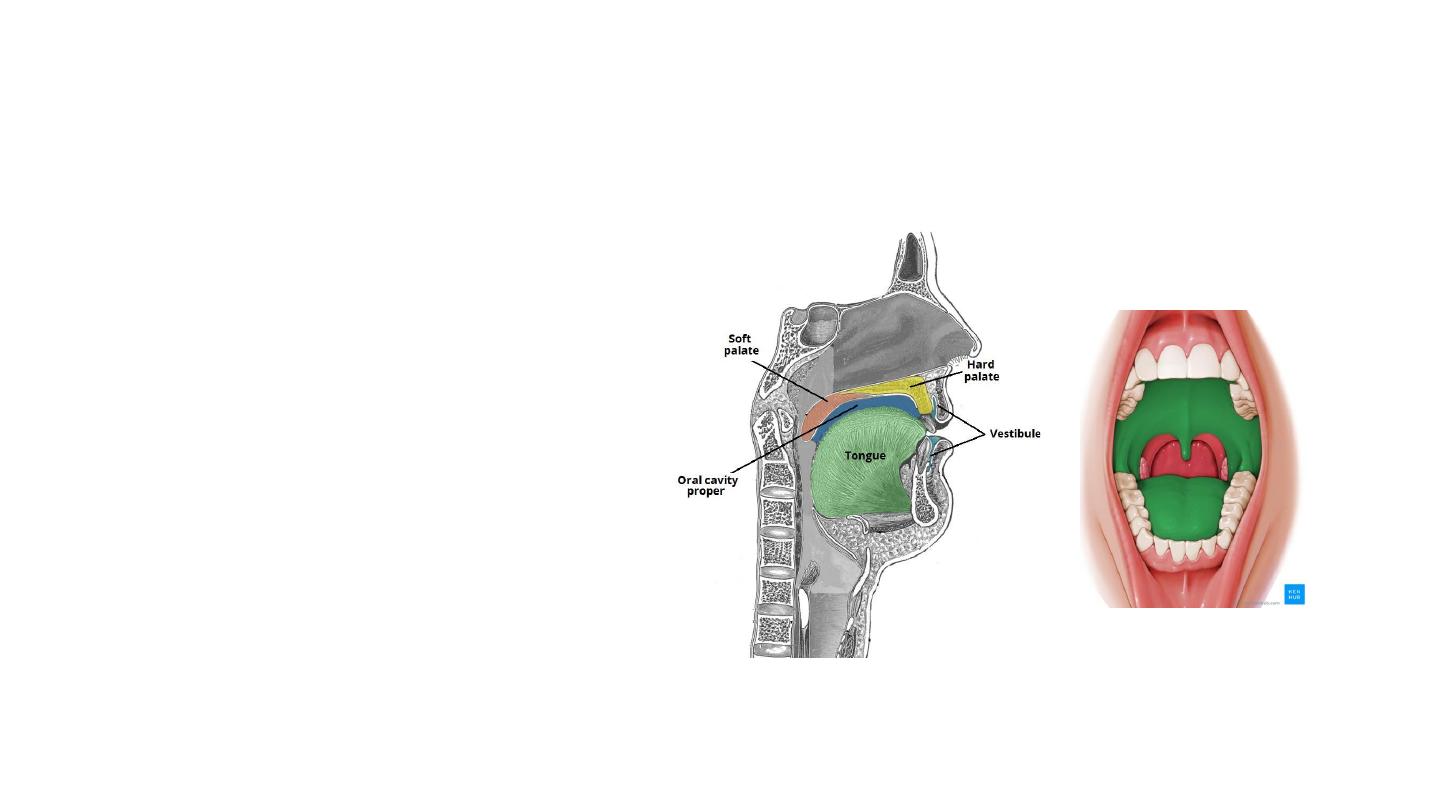
Divisions of the Oral Cavity
• The oral cavity spans between
the oral fissure (anteriorly –
the opening between the lips),
and the oropharyngeal isthmus
(posteriorly – the opening of
the oropharynx).
• The vestibule
• The mouth cavity proper.

Vestibule
• Situated anteriorly.
• It is the space between the lips/cheeks, and the gums/teeth.
• The vestibule communicates with the mouth proper via the space
behind the third molar tooth, and with the exterior through the oral
fissure.
• Opposite the upper second molar tooth, the duct of the parotid
gland opens out into the vestibule, secreting salivatory juices.
Mouth Proper
• lies posteriorly to the vestibule.
• The tongue fills a large proportion of the cavity of the mouth proper.

Boundaries
Roof
• Hard and soft palates.
Cheeks
• Formed by the buccinator muscle, which is lined internally by the oral
mucous membrane.
• Buccal branches of the facial nerve (CN VII).
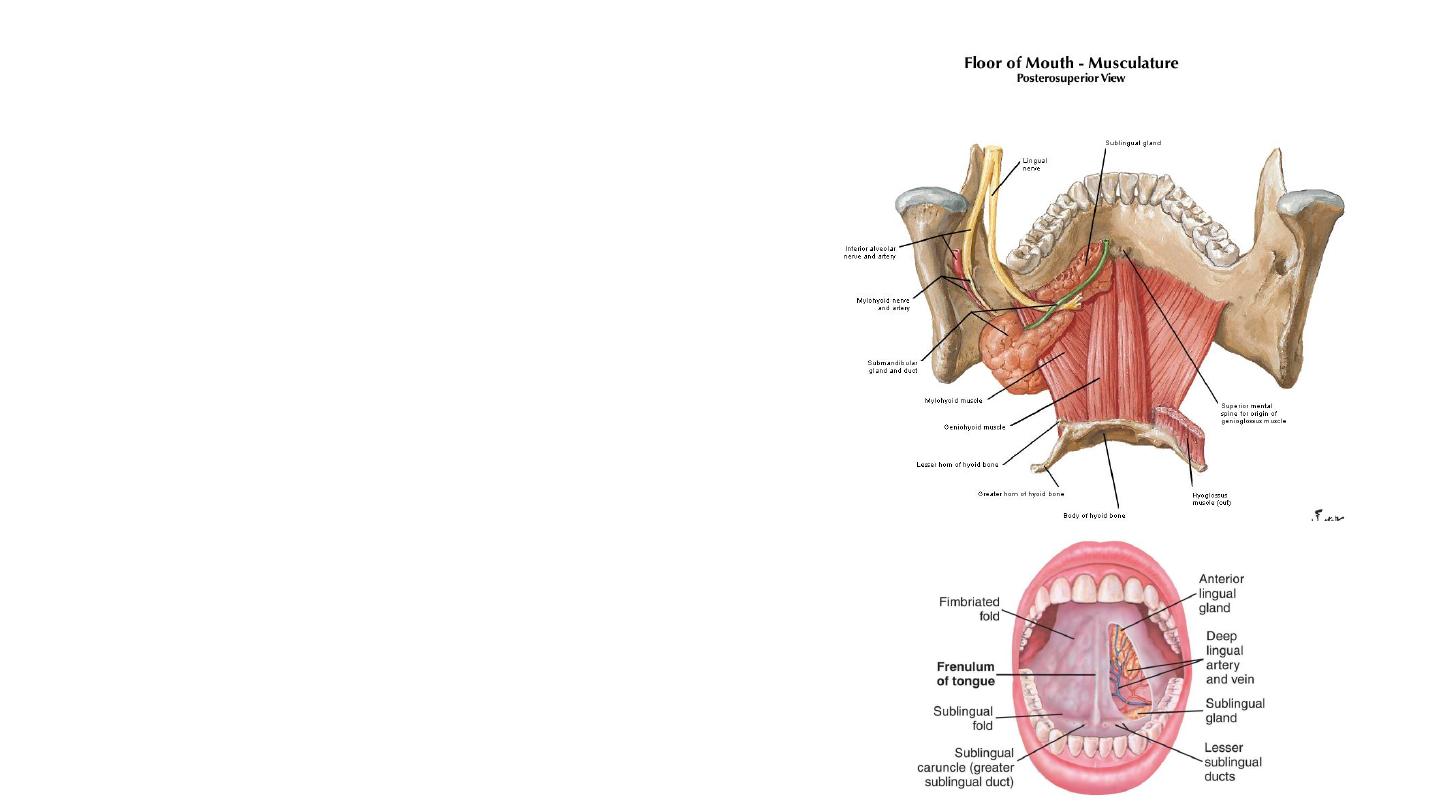
Floor
• Muscular diaphragm –
• Bilateral mylohyoid muscles.
• Provides structural support to the floor of
the mouth, and pulls the larynx forward
during swallowing.
• Geniohyoid muscles – pull the larynx
forward during swallowing.
• Tongue – connected to the floor by the
frenulum of the tongue, a fold of oral
mucosa.
• Salivary glands and ducts.
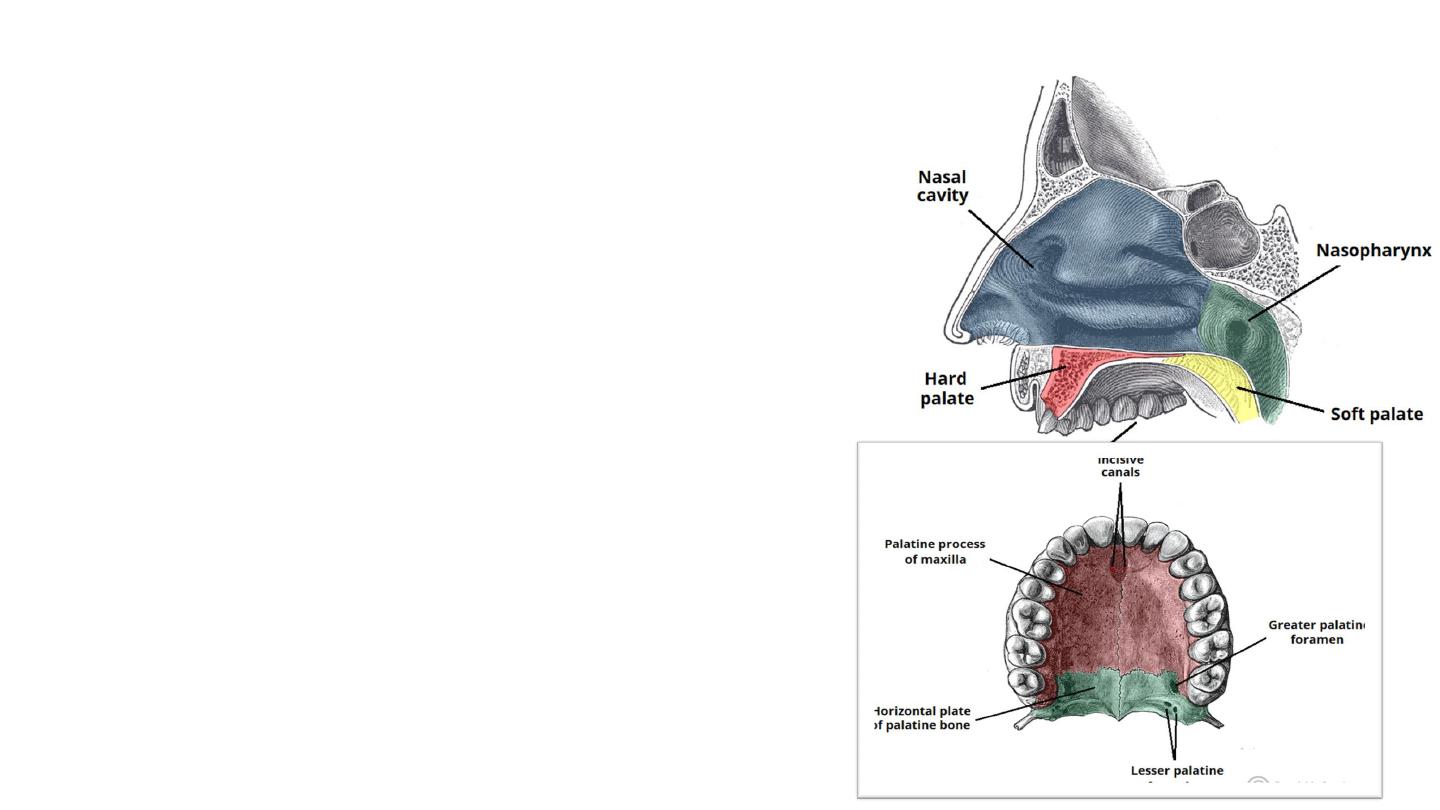
The Palate
• Also known as the ‘roof of the mouth’).
• It is separated into two distinct parts:
• Hard palate – comprised of bone. It is immobile.
• Soft palate – comprised of muscle fibres covered by
a mucous membrane.
• The hard palate positioned anteriorly and the soft
palate posteriorly.
• Forms a division between the nasal and oral
cavities.
• Reflecting this, the superior and inferior palatal
surfaces have different mucosal linings:
• Superior aspect of palate (nasal cavity) – respiratory
epithelium.
• Inferiorly aspect of palate (oral cavity) – oral
mucosa, populated by secretory salivary glands.
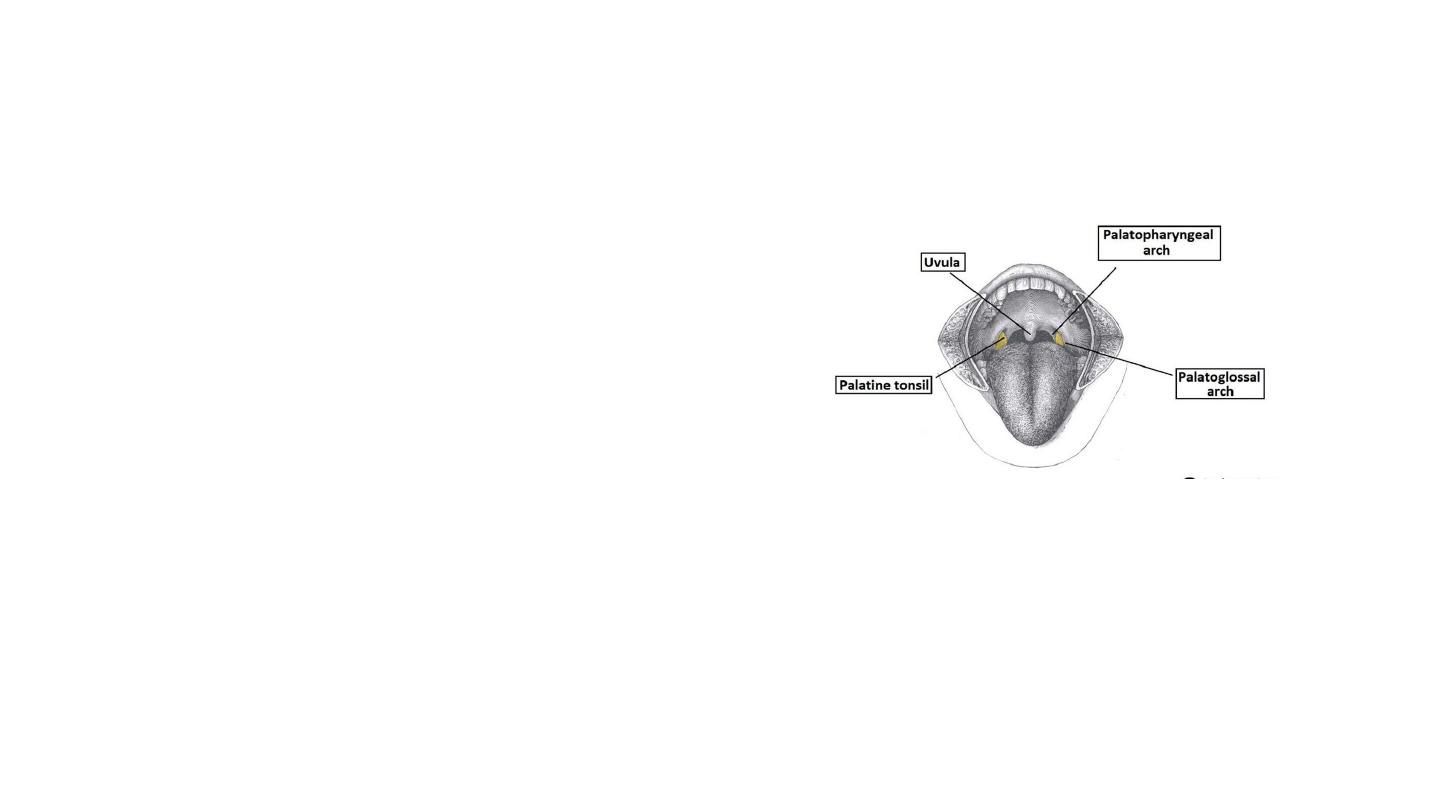
Soft palate
• The soft palate is a posterior
continuation of the hard palate. In
contrast to the hard palate, it is a
muscular structure. It acts as a
valve that can lower to close the
oropharyngeal isthmus, and
elevate to separate the
nasopharynx from the oropharynx.
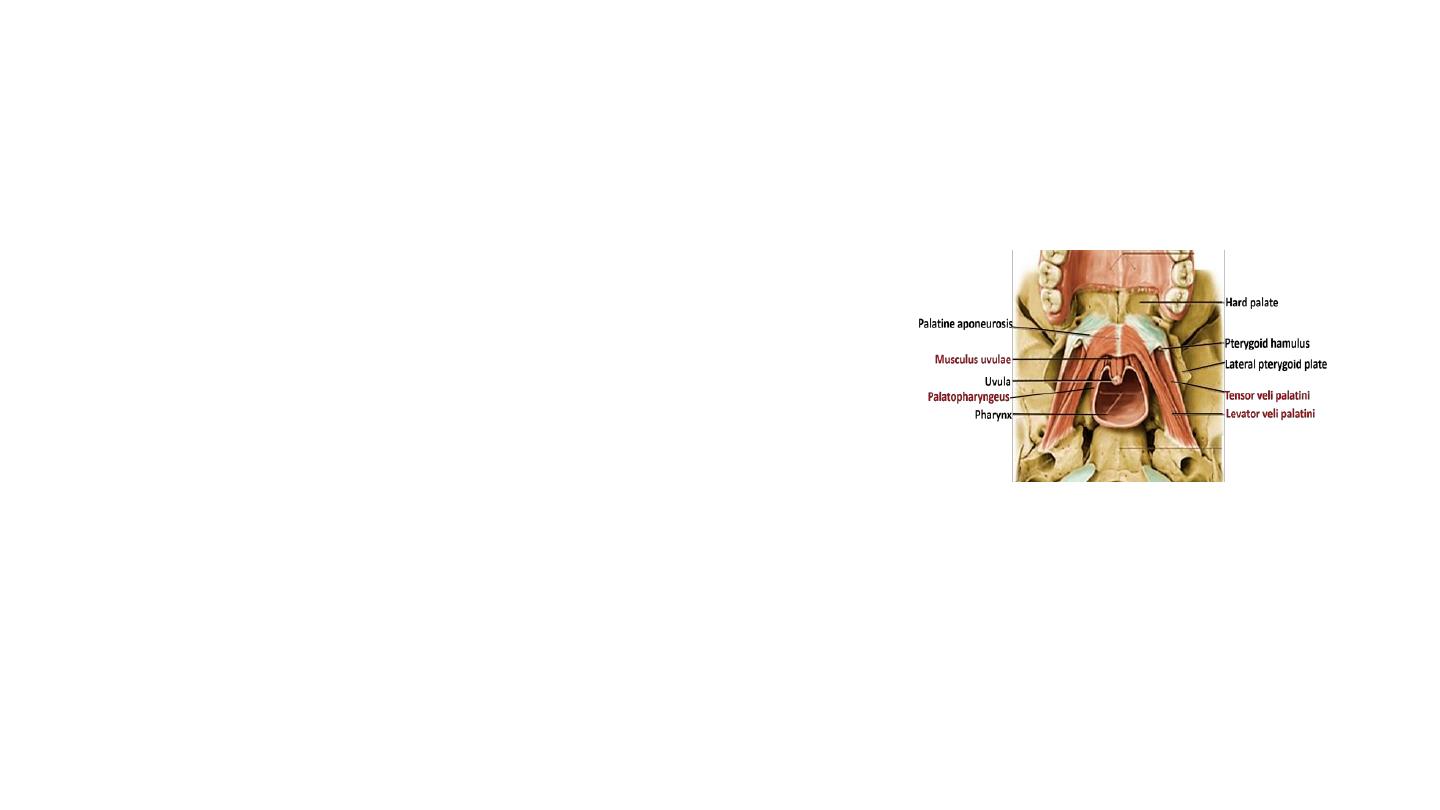
Muscles of the Soft Palate
• Tensor Veli Palatini
Function: Tenses the soft palate.
• Levator Veli Palatini
Function: Elevation of the soft palate.
• Palatoglossus
Function: Pulls the soft palate towards the
tongue.
• Palatopharyngeus
• Function: Tenses soft palate and draws the
pharynx anteriorly on swallowing.
• Musculus Uvulae
• Function: Shortens the uvula.
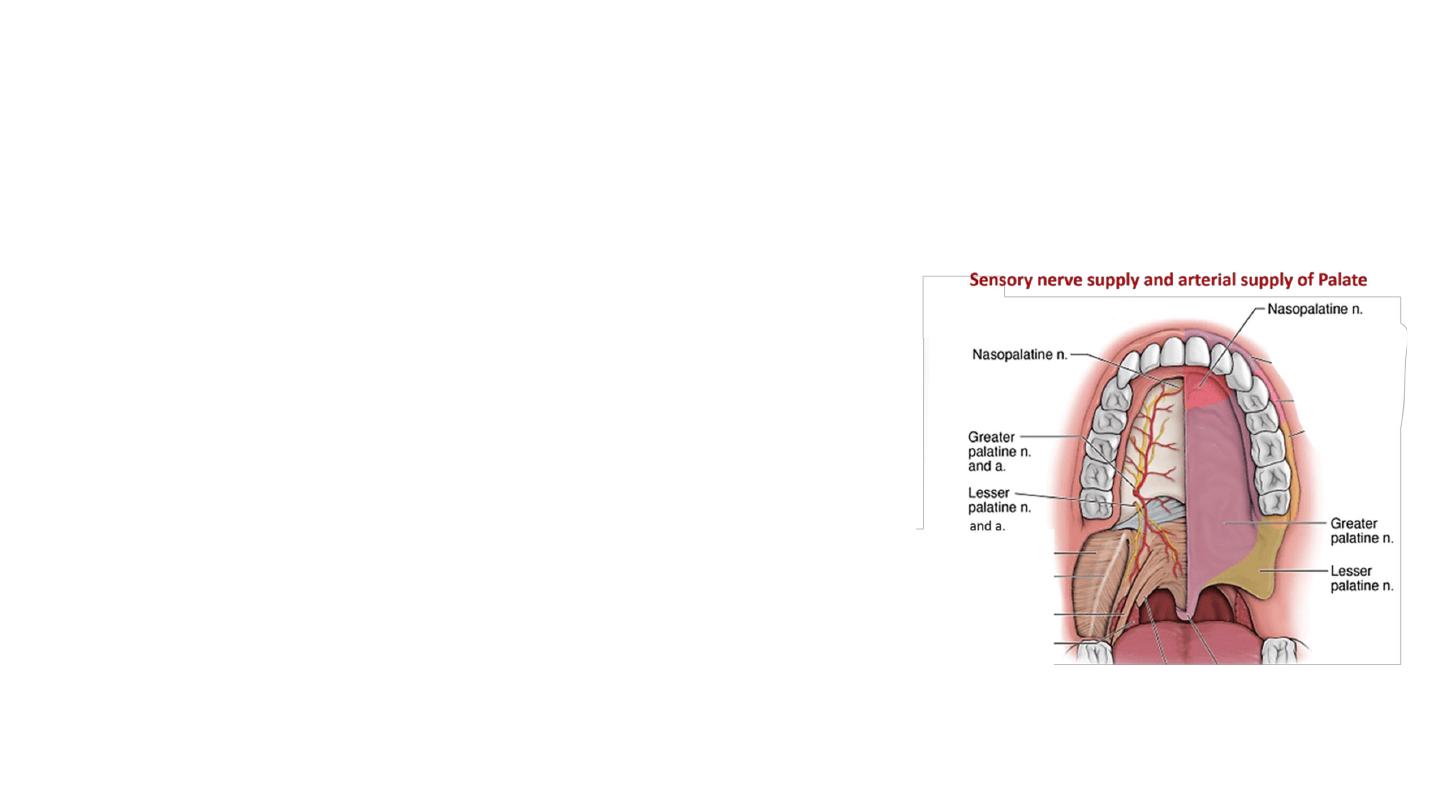
• Vasculature
• Greater palatine arteries, which run anteriorly
from the greater palatine foramen.
• In addition, the anastomosis between the lesser
palatine artery and ascending palatine artery
provide collateral supply to the palate.
• Innervation
• Sensory innervation : branches of the
trigeminal nerve (CN V).
• Muscles are all innervated by the pharyngeal
branch of the vagus nerve (CN X) – apart from
Tensor veli palatini – which is innervated by a
branch of CN V3.
Tongue
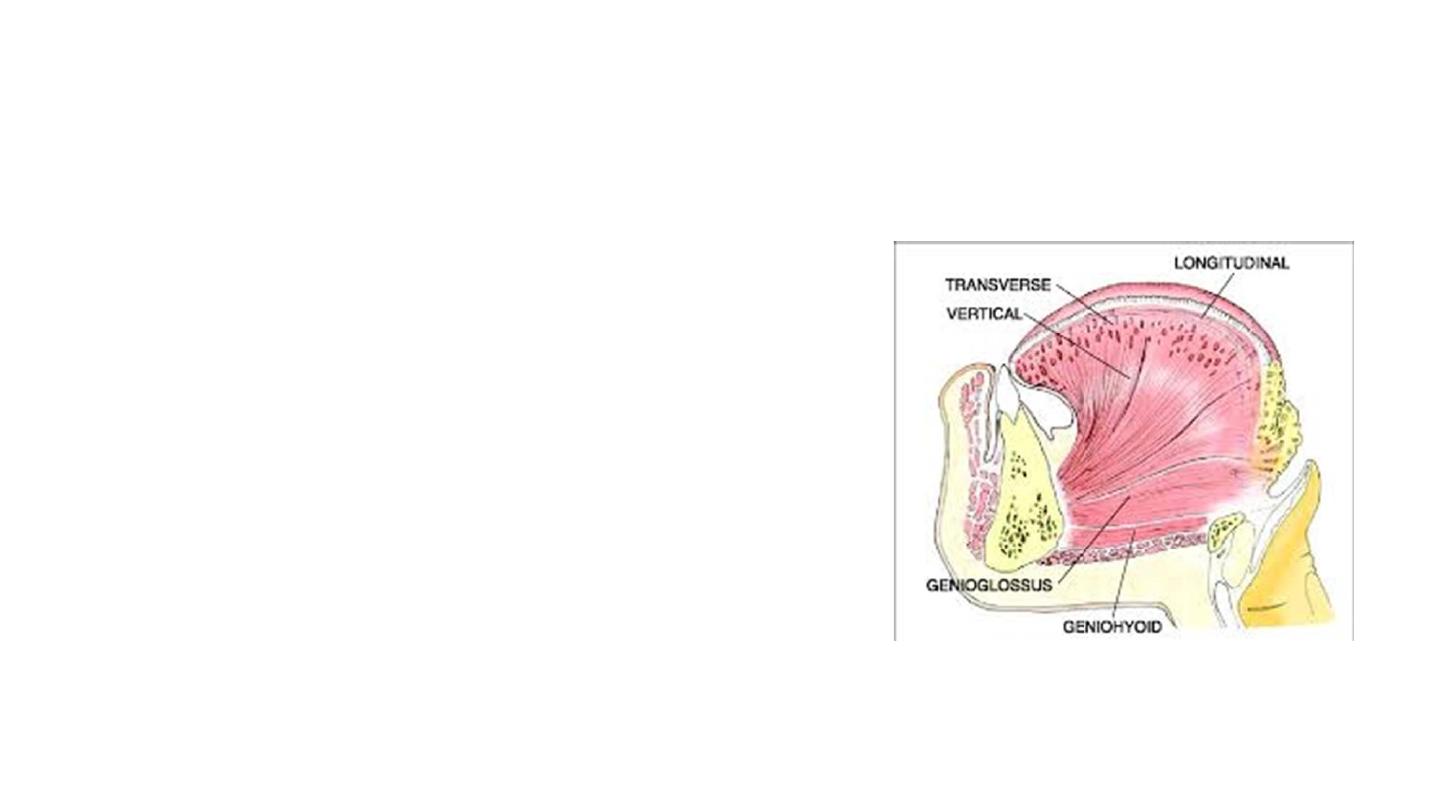
Intrinsic Muscles
• There are four paired intrinsic muscles of
the tongue and they are named by the
direction in which they travel
• Longitudinal ( superior and inferior) ,
transverse and vertical muscles of the
tongue.
• These muscles affect the shape and size of
the tongue and have a role in facilitating
speech, eating and swallowing.
• Motor innervation : Hypoglossal nerve
(CNXII).

Extrinsic Muscles
Genioglossus
• Attachments:
• Arises from the mandibular symphysis.
• Inserts into the body of the hyoid bone and the entire length of the
tongue.
Hyoglossus
• Attachments:
• Arises from the hyoid bone and inserts into the side of the tongue
Styloglossus
Attachments:
• Originates at the styloid process of the temporal bone and inserts into the
side of the tongue
Innervation
: Motor innervation via the hypoglossal nerve (CNXII).
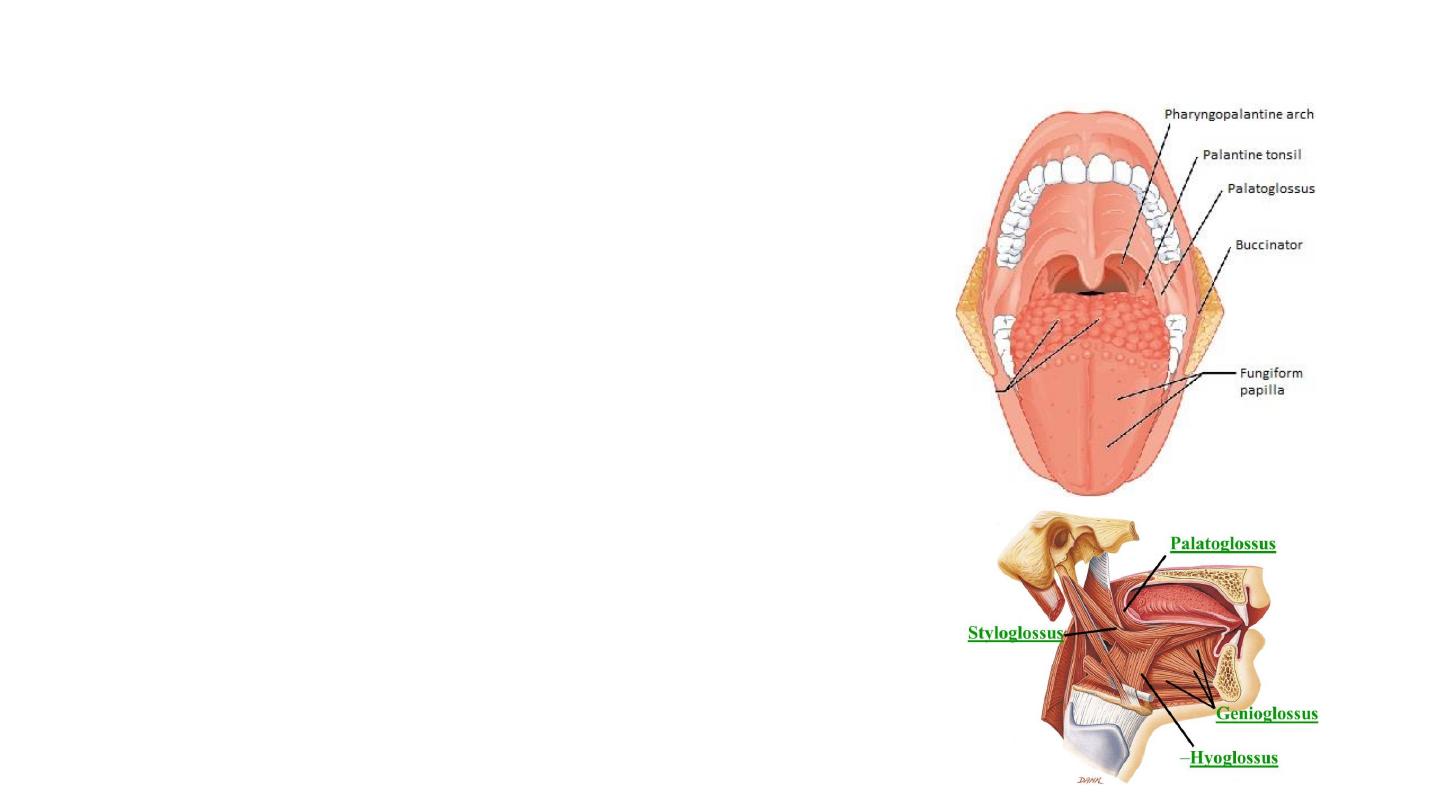
Palatoglossus
• Attachments:
• Arises from the palatine aponeurosis and inserts broadly across
the tongue
• Innervation: Motor innervation via the vagus nerve
(CNX).
Function
: altering the tongue's position allowing for
protrusion, retraction, and side-to-side movement.

Sensory innervation
• Anterior 2/3
• General sensation: lingual nerve- mandibular nerve (CN V3)- trigeminal nerve
(CNV).
• Taste: chorda tympani- the facial nerve (CNVII).. This travels through the
middle ear, and continues on to the tongue.
• The posterior 1/3 :
• Both touch and taste are supplied by the glossopharyngeal nerve (CNIX).

Vasculature
• The lingual artery (main)
• A branch from the facial artery, called the tonsillar artery, which can
provide some collateral circulation.
• Drainage is by the lingual vein.
• Lymphatic Drainage
• Anterior two thirds – initially into the submental and submandibular nodes,
which empty into the deep cervical lymph nodes
• Posterior third – directly into the deep cervical lymph nodes
