Peptic ulcer disease (PUD):
1. Causes of PUD.2. Role of H. pylori bacteria in gastric, duodenal ulcers and CA stomach.
3. How could you diagnose H. pylori bacteria?
4. How could a patient with peptic ulcer present to you?
5. Management of PUD.
6. complications of PUD.
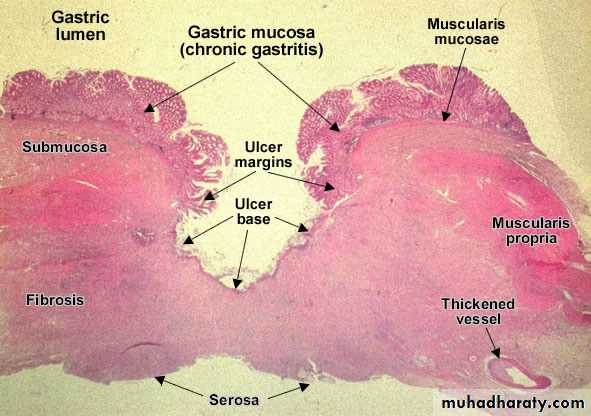
It refers to an ulcer in the lower esophagus stomach or duodenum, in the jejunum after surgical anastomosis to the stomach or rarely in the ileum adjacent to a Mickel’s diverticulum’s is divided into acute or chronic as acute shows no signs of fibrosis although both of them penetrate muscularis mucosa.
Epidemiology:-
The life time prevalence is about 10%.
In duodenal ulcer male: female =5:1 to 2:1
In gastric ulcer male: female =2:1 or less
Etiology:-
The incidence of ulcer dis increases with age which may be explained by increased use of NSAID and decrease prostaglandin level with age.Genetic factors: - increase incidence with first degree relative, others increase incidence in relatives with high levels of serum pepsinogen1 which is inherited as a dominant trait.
Ethnic black group:- black has PU in early life.
Certain disease association: - chronic lung disease, cirrhosis, hyper parathyroidism, chronic renal failure and PRV.
Association with drug ingestion
NSAIDS, it seems to increase the incidence of gastric erosion and gastric ulcer more than DU.it doesn’t appear to depend on type of NSAIDs.
Corticosteroids:-it is controversial, increase incidence of recurrent ulcer rather than induction of ulcer.
Psychological factors:-emotional stress may increase gastric secretion.
Environmental factors and eating especially spices.helicobacter pylori :-
This is the most important factor now a day and most commonly discussed.
This infection increases with age and in UK about 50% are infected in pt more than 50 years old. In other countries more than 90% of people infected and only minority of them develop the symptoms.
Around 90% of pt with DU have the infection and 70% of pt with ‘GU infected, the other 30% due to NSAIDs
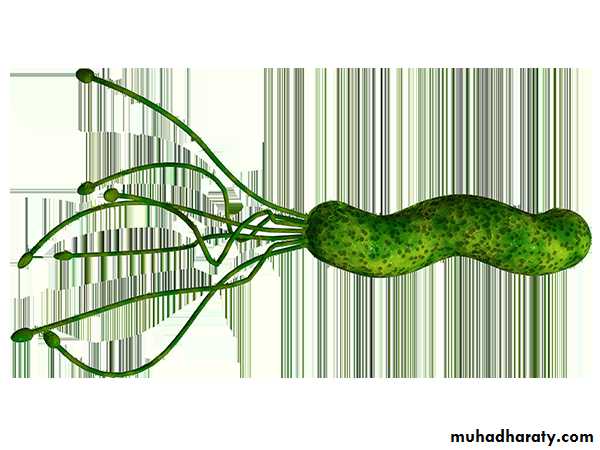
H pylori this is a gram negative micro aerophilic, spiral and has multiple flagella at one end which make it motile, allowing it to burrow and live deep beneath the mucus layer closely adherent to surface epithelium .it infect the stomach mainly but may be found in duodenal mucosa where there is gastric metaplasia.
The bacterium try to make neutral environment of pH 7 around it by effect of urease enzyme, this produces ammonia from urea and raises pH around bacteria.
It uses adhesive molecules (Bab A) to bind to the Lewis b antigen on epithelial cells
The bacteria express two antigens
Bacterial cag A gene 2. bacterial vac A gene
Segment of genome that carry the pathogenicity island (cag) which is gene for secretion system, this will be injecting into epithelial cells.
interaction with several cell-signaling pathway
Cell replication, apoptosis.
H pylori strain express cag A in either:
Cag A +ve strain
Or Cag A –ve strain
Cag A + more than Cag A - strain in association with the dis. Most strain secretes a large pore –forming protein called vac A. This vac A protein leads to:-
Causes large vacuoles in the cells in vitro.
Increase cell permeability.
Efflux of micronutrients from the epithelium.
Induction of apoptosis.
Suppression of local immune cells activity.
May stimulate secretion of s1\m1 toxin.
Pathophysiological effect of H pylori in DU:-
cause antral gastritis and depletion of D-cellsIncrease gastrin release from G –cells.
Increase acid production by parietal cells.
Increase acid load in duodenum leads to gastric metaplasia.
Further inflammation and eventual ulceration.
Pathophysiological effect of H pylori in gastric ulcer
Acts by reducing gastric mucosal resistance to attack from acid and pepsin.
In 1% of infected person, H pylori may cause pangastritis leading to gastric atrophy and hypochlorhydria, this in turn leads to proliferation of bacteria within the stomach, and these bacteria will split dietary nitrates to produce mutagenic nitrate and gastric CA.Another thing, this process leads to expression of proinflammatory cytokine interleukin-1 B (IL1 –B) which associated with risk of CA stomach and atrophic gastritis.
Diagnosis of H pylori
non invasiveSerology by using kits in out pt, it lacks specificity and sensitivity, can’t differentiate chronic from acute.
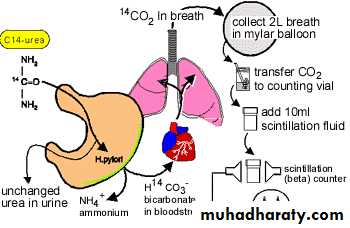
Urea breath test: - high sensitivity and specificity by using C14 (with high radioactivity and C13 (expensive method).
Fecal antigen test: - cheap, accurate, but un accepted.
invasive
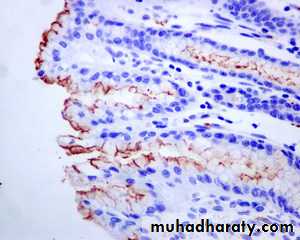
Histology: - highly specific and sensitive but it takes along time to be processed and may give false (-ve).
Rapid urease test:-cheap quick and specific but lack sensitivity.
Microbiology:-gold standard but slow and laborious.
Culture: - it helps to define antibiotics sensitivity but it lacks sensitivity by it self.
Incidence of peptic ulcer:-
Chronic gastric ulcer is single.90% are situated on lesser curvature with in the antrum or at the junction between body and antrum.
Chronic DU usually occurs in the first part of the duodenum 50% on the anterior wall.
Pathology of Peptic ulcer
It shows four layers, surface debris, and an infiltrate of neutrophil, granulation tissue, and collagen.Clinical feature:-
Chronic condition with spontaneous relapse and remission lasting for years or life.
recurrent abdominal pain that :
Localization: - finger-pointing pain in the epigastrum but it may extend from xiphisternum down to the umbilicus.
Episodic occurrence and periodicity, remission and relapse and the pain may subside although incomplete healing of the ulcer.
Relationship to food, the pain typically comes 1 -3 hours after eating, it is a hunger pain may a wake the pt at night (empty stomach).
The eating may relief pain as well as antacids, this is more true for duodenal ulcer than gastric ulcer; therefore, the pt may gain weight.
Sometime the vomiting may occur either by itself or induce by the pt himself, the persistent daily vomiting suggest gastric outlet obstruction.
The pt. may have a symptomatic peptic ulcer, this may occur in one third of the pt. or the pt. may have only vague sense of dyspepsia , or anorexia and nausea or completely silent presenting for the first time with anemia from blood loss hematemesis ,or acute perforation or may be recurrent acute bleeding without ulcer pain between the attacks.
Investigations:-
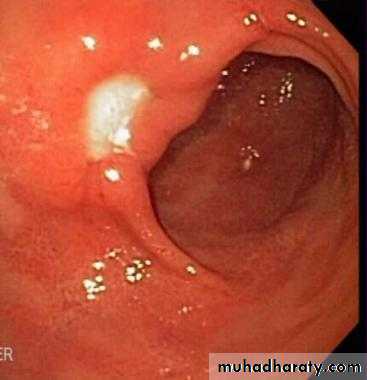
Endoscope is the mean investigation.a biopsy is a must in gastric ulcer to exclude malignancy.
Management:-
The aims of management are to-Relieve symptoms.
induce healing
prevent recurrence
Eradication of H pylori is necessary to-
prevent relapseEliminate the need for long-term therapy in the majority of the pt .
H pylori eradication is indicated in PU pt if :-
1. Acute or chronic duodenal ulcer.2. Gastric ulcer with proven H pylori +ve
The basic therapy included-
first line therapy:-For 7 days with success 90 %
Proton pump inhibitor twice daily +
Amoxicillin 1 gm bid or clarithromycin 500 mg bid +metronodazole 400 mg bid
Factor influence success
1. Compliance
side effect
metronidazole resistance
second line therapy:- for 7 days
PPI bid +Bismuth 120 mg four-time daily +metronidazole 400 mg +tetracycline 500mg four times daily
Or long term maintenance therapy with acid suppression.If the pt H pylori and need to receive NSAID, it is not clear whether to eradicate H pylori before NSAIDs or not ,but now a day it shows that this is not necessary in:-
young
Fit pt with no history of PU or dyspepsia.
If the pt has a low risk of PU and need to receive aspirin, it is not always to receive PPI with it.
Indication for H pylori eradication:-
Definite indication:-
PU
malt oma
H pylori + ve dyspepsia.
Not indicated:-
Asymptomatic H pylori.GERD.
UN certain:-
family history of gastric CAnon ulcer dyspepsia
long term NSAIDs
Surgery:-
rarely used because :-. Eradication of H pylori
. Presence of PPI.
In chronic non –healing gastric ulcer, the surgery required is partial gastrectomy (Billroth 1) because of high suspicion of gastric CA.
Pyloroplasty.
gastroenterostomy.Highly selective vagotomy.
Under running the ulcer. ( patch ) for perforated DU
Billroth 11(polya) for giant DU.
Complications of gastric resection and vagotomy:-
Dumping syndrome: small size with rapid gastric emptying leads to distention of the proximal small intestine as the hypertonic contents draw fluid into the lumen, this leads to abdominal discomfort and diarrhea after eating.postural drop after eating :- autonomic reflexes release arrange of gastrointestinal hormones which leads to vasomotor features such as flushing , palpitation , sweating tachycardia and hypotension , so pt need to avoid large meals with high CHO content .
biliary reflex gastritis:- usually asymptomatic or dyspepsia with it , treatment with aluminum ( antacid ) or sucralfate or Roux en Y loop .
Diarrhea: - one to two hours after eating .it is treated by eating small dry meals & decrease refined CHO.
malabsorption :- because
Poor mixing of food in the stomach.
Rapid empting.
Inadequate mixing with pancreatic and biliary secretion.
Reduced small intestinal transit time.
Bacterial over growth.
Weights lose: - due to low intake diarrhea and mild steatorrhea.
Anemia: - due to a. iron deficiency anemia most commonly
Folic acid and B12 deficiency anemia.
Due to
1. Decrease intake
2. Intrinsic factor and lack of acid
3. Mild chronic low-grade blood loss.
4. Recurrent ulcer.
8. Metabolic bone disease:- a. Osteoporosis
b. osteomalacia
Due to malabsorption of Ca and Vit D.
Gastric cancer.
Due to:-hypochlorhydria /
Duodenogastric reflux of bile.
smoking
H. pylori infection.
No indication of endoscope post gastric surgery seeking for tumor .
blind loop syndrome
Drug used in PU disantacid and alginate
a. aluminum hydroxide =leads to constipationb. magnesium trisalicate = leads to diarrhea
c. alginate leads to = may be used as an assistance
The combination of the first two drugs or three may be present, they form a barrier for the ulcer from acids, may exacerbate heart failure due to 1. Decrease digoxin absorption
2 . High Na content with in the drug
H2 antagonist
Ranitidine 150 mg bid
Cimitidine 400 mg bid
Famotidine 20 mg bid
Mesotidine
Good safety profile, cimitidine may interact with warfarin and phanytoin, metabolized via live cytochrome P450.
3. Proton pump inhibitor (PPI)
Omeprazole
Lansoprazole, esmoprazole , pontoprazole , rabiprazole
Work on parietal cell surface leads to irreversible inhibitors of H\k ATPase , they are potent acid suppression and rapid healing , more effective than other drugs in healing of PU.
4, chelator (tripotassium dicitratobismuthate)
Ammoniacal suspension of complex bismuth salt. anti H pylori activity and enhances mucosal protection , it may darken the tooth and tongue.Complex salt sucralfate (aluminum salt of sucrose octasulfate) :- little effect on acid may protect ulcer bases from peptic activity and enhance epithelial cells turn over.
Side effect: used in caution in renal impairment & Bezoars formation
prostaglandin analogue (mesoprostol )200 microgram
enhance mucosal blood flowstimulate mucus and bicarbonate secretion
stimulate epithelial proliferation
side effect diarrhea and abortification in female so contra indicated in child barring female
Indications for surgery in PU
Emergency indication
Perforation & hemorrhage