Lec : 8
Flap Surgery (2)UNIVERSITY OF MOSUL
COLLEGE OF DENTISTRY
By:
Dr.Ghayath Aljawady
B.D.S, M.Sc., Ph.D in periodontics
2020-2021
Department of:
Oral and Maxillofacial surgery / Periodontics unit
Department of:
Flap Surgery (2)
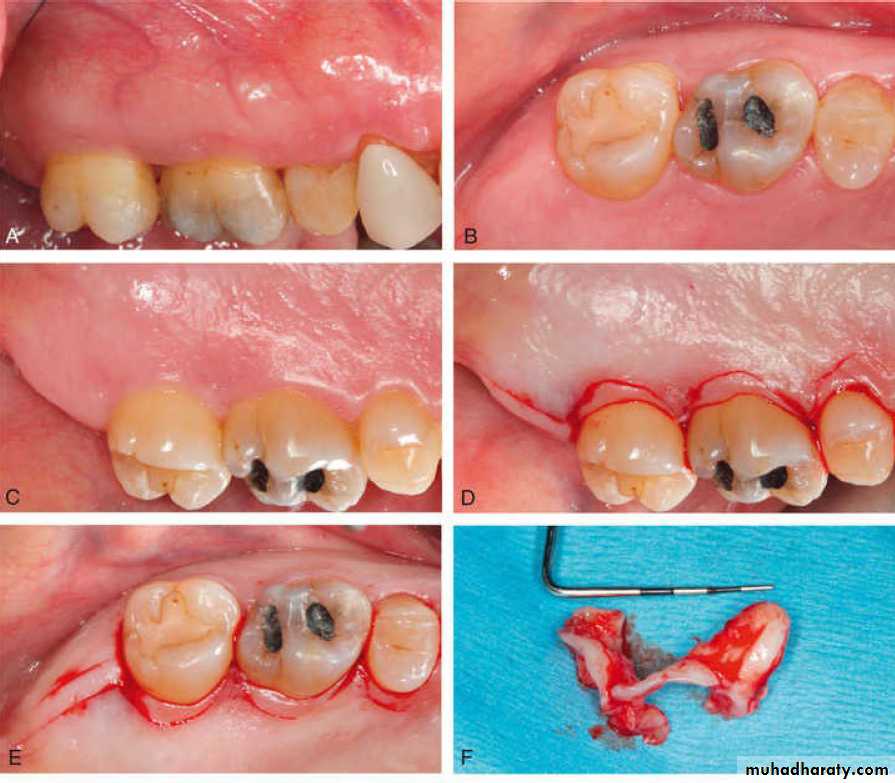
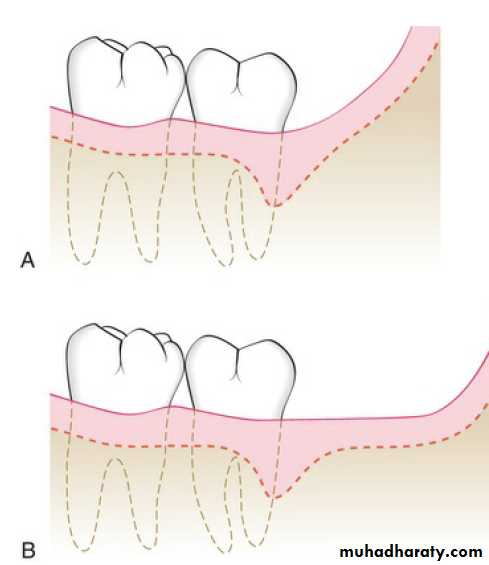
The treatment of periodontal pockets on the distal surface of terminal molars is often complicated by the presence of bulbous fibrous tissue over the maxillary tuberosity or prominent retromolar pads in the mandible.
Distal Terminal Molar Flap
Some of these osseous lesions may result from incomplete repair after the extraction of impacted third molars.
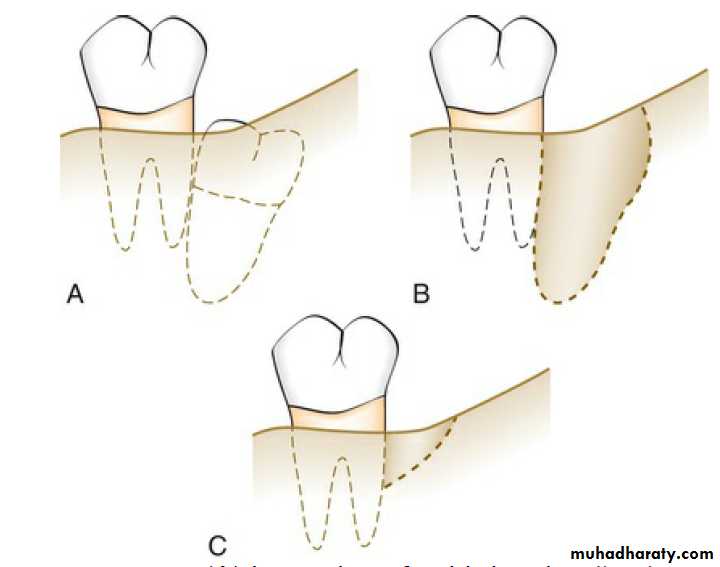
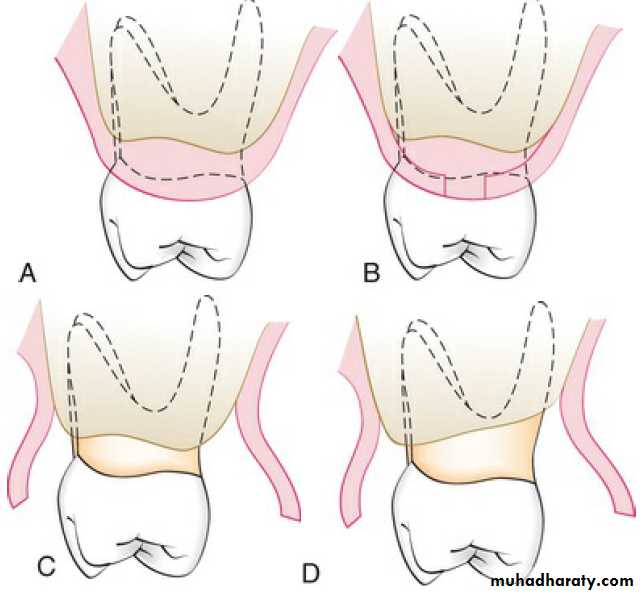
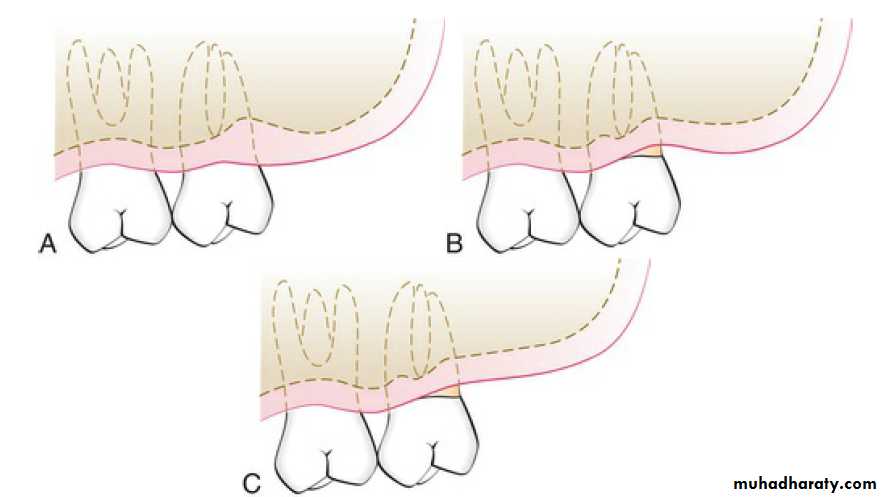
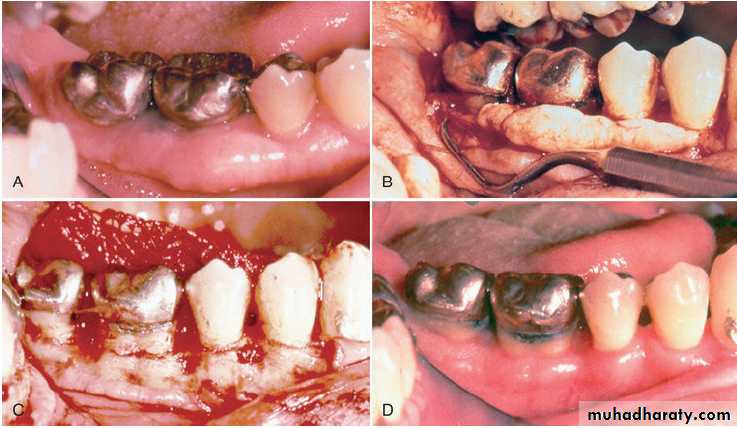
The two incisions distal to the molar should follow the area with the greatest amount of attached gingiva. Therefore the incisions could be directed distolingually or distobuccally, depending on which area has more attached gingiva. Before the flap is completely reflected, it is thinned with a #15 blade. After the reflection of the flap and the removal of the redundant fibrous tissue, any necessary osseous surgery is performed
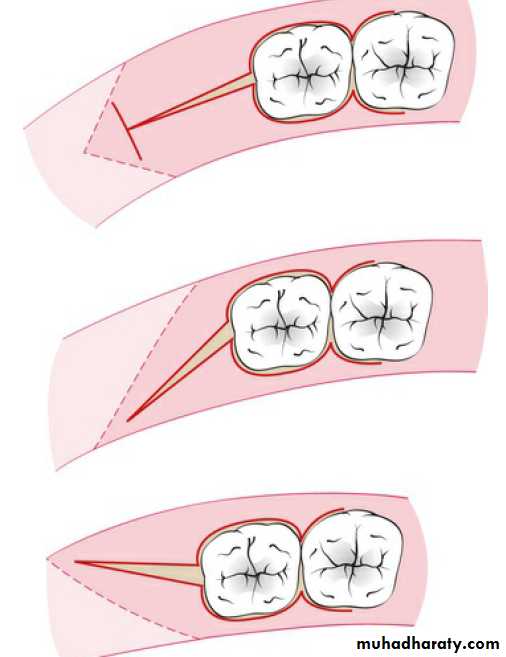
Access to these distal areas may be obtained by:
a single horizontal incision,two converging horizontal incisions,
or two parallel incisions extending distally from the distal surface of the terminal molar to the Mucogingival junction distal to the tuberosity or the retromolar pad.
The distal horizontal incision is connected with the crevicular incision on the distal surface of the terminal molar, which merges mesially with the buccal and lingual or palatal scalloped incisions.
If the secondary objective of surgery is regenerative or the buccolingual width of the distal keratinized tissue is limited, a single horizontal incision in keratinized tissue is used.
If the secondary objective of surgery is resective and adequate keratinized tissue is present buccolingually, two distal horizontal incisions are placed in keratinized tissue.
The two horizontal incisions technique were described by Robinson and Braden and modified by several other investigators.
These techniques are called the distal wedge and the modified distal wedge.
The buccolingual distance between the two horizontal incisions in both techniques depends on the transgingival probing depth and the amount of fibrous tissue involved.
When the flaps are thinned and the tissue between the two incisions is removed, the two flap edges must approximate each other at a new apical position without overlapping.
Upper
Lower
Flap design
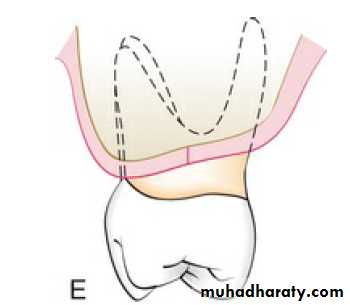
The treatment of distal pockets in the maxilla is usually less challenging than that in the mandible.
The tuberosity presents a greater amount of fibrous attached gingiva than does the retromolar pad.
Healing of a distal wedge in the maxilla results in an acute angle between the distal tooth surface and the tuberosity that is biofilm retentive and difficult to clean.
Maxillary Molars
In contrast, the use of the modified distal wedge with two parallel distal incisions allows the soft tissue along the whole length of the distal flap to be evenly displaced apically.
This is advantageous in the maxilla in maintaining a wide angle between the tooth and the tuberosity that is much easier to clean. Therefore, the modified distal wedge is preferred in the maxilla.
Incisions in the distal mandible differ from those in the tuberosity due to differences in the anatomy of the area. The retromolar pad usually has limited attached gingiva and vestibular depth. The attached gingiva, if present, may not be found directly distal to the molar.
Mandibular Molars
The ascending ramus of the
mandible may also create a short or completely eliminate thehorizontal area distal to the terminal molar .
The shorter this area, the more difficult it is to treat any deep distal lesion
around the terminal molar.
The mandibular retromolar tissue ascends distally to merge with the ascending ramus. This anatomy favors the distal wedge technique in the mandible, although the parallel distal incisions and the single horizontal incision may be used. The two distal incisions should follow the area with the greatest amount of attached gingiva and must be made over bone
the incisions could be directed distally or distobuccally, depending on which area has more attached gingiva. Incisions directing distolingually should be avoided due to the potential presence of the lingual nerve.
FLAPS FOR RECONSTRUCTIVE SURGERY
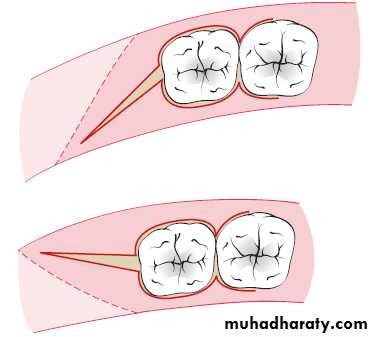
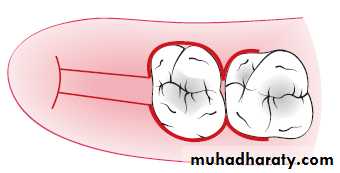
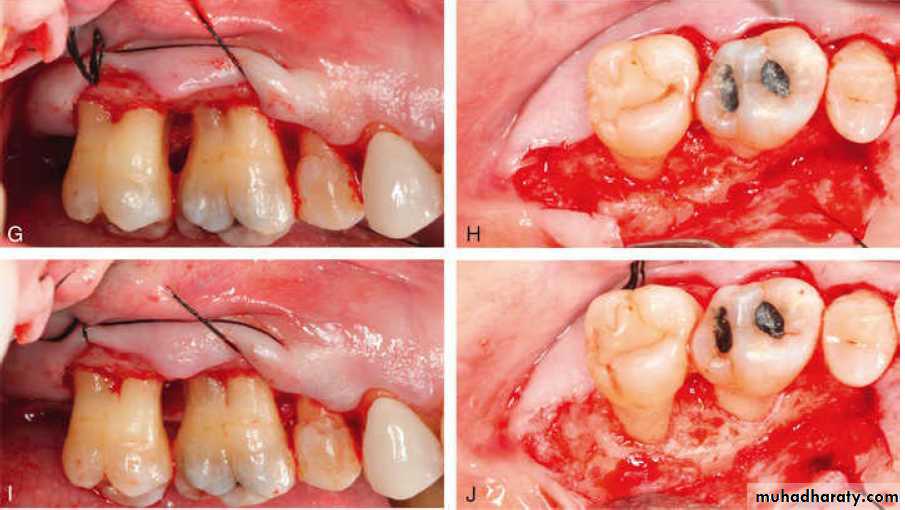
In current reconstructive therapy, bone grafts, membranes, or a combination of these, with or without other agents, are used for a successful outcome. The flap design should therefore be set up so that the maximum amount of gingival tissue and papilla are retained to cover the material(s) placed in the pocket.Two flap designs are available for reconstructive surgery: the
papilla preservation flap and
conventional flap with only crevicular incisions.
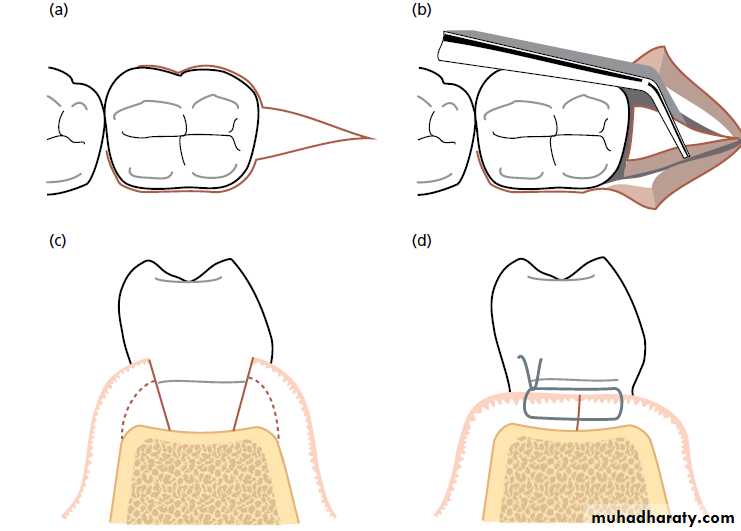
The flap design of choice is the papilla preservation flap, which retains the entire papilla covering the lesion. However, to use this flap, there must be adequate interdental space to allow the intact papilla to be reflected with the facial or lingual/palatal flap.
When the interdental space is very narrow, making it impossible to perform a papilla preservation flap, a conventional flap with only crevicular incisions is made.
In current regenerative therapy, bone grafts, membranes, or a combination of these are used with or without other biologics. The flap design should maximize the amount of gingival tissue and papilla retained to cover the material placed in the osseous defect.
Papilla Preservation Flap
the crevicular incision is the incision of choice for the anterior aesthetic area and regenerative therapy. The interdental papilla is retained with the papilla preservation technique when the interdental space is adequate for reflection of the intact papilla; otherwise, it is split beneath the contact point of the two approximating teeth. The flap is elevated in full thickness without thinning of the flap or the papilla.
The step-by-step technique for the papilla preservation flap is as follows:
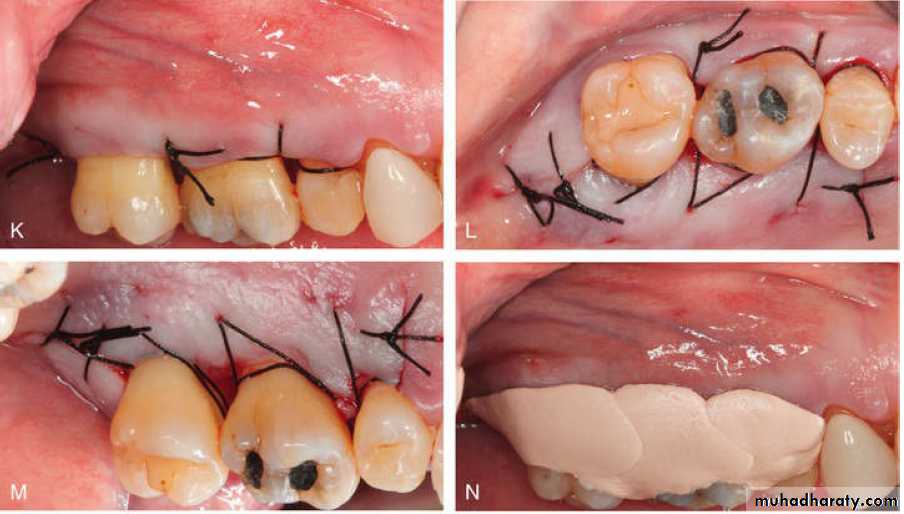
Step 1: A crevicular incision is made around each tooth, with no incisions across the interdental papilla.Step 2: The preserved papilla can be incorporated into the facial-buccal flap (original papilla preservation technique) or lingual-palatal flap (modified papilla preservation technique).
Step 3: The papilla is then elevated with an Orban knife or curettes and is reflected intact with the flap.
Step 4: The flap is reflected without thinning the tissue.
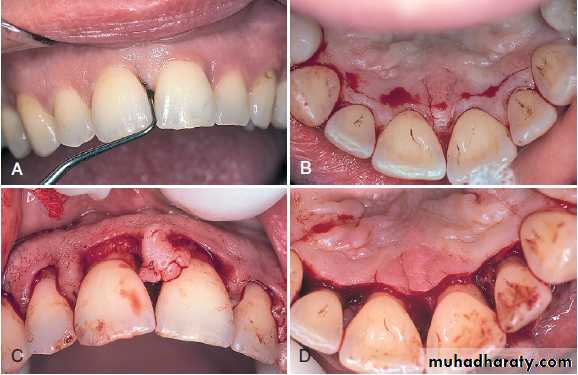
Papilla preservation flap. A, Facial view after sulcular incisions have been made. B, Straight-line incision in the palatal area about 3 mm from gingival margins. This incision is then connected to the margins with vertical incisions in the midpart of each tooth. C, Papillae are reflected with the facial flap. D, Lingual view after reflection of the flap.
Immediately after suturing (≤24 hours), a connection between the flap and the tooth or bone surface is established by a blood clot, which consists of a fibrin reticulum with many polymorphonuclear leukocytes, erythrocytes, debris of injured cells, and capillaries at the edge of the wound. Bacteria and an exudate or transudate also result from tissue injury.
Healing After Flap Surgery
One to 3 days after flap surgery, the space between the flap and the tooth or bone is thinner. Epithelial cells migrate over the border of the flap, and they usually contact the tooth at this time. When the flap is closely adapted to the alveolar process, the inflammatory response is minimal.
One week after surgery, an epithelial attachment to the root has been established by means of hemidesmosomes and a basal lamina. The blood clot is replaced by granulation tissue derived from the gingival connective tissue, the bone marrow, and the periodontal ligament.
Two weeks after surgery, collagen fibers begin to appear parallel to the tooth surface. Union of the flap to the tooth is still weak because of the presence of immature collagen fibers, although the clinical aspect may be almost normal.
One month after surgery, a fully epithelialized gingival crevice with a well-defined epithelial attachment is present. A functional arrangement of the supracrestal fibers is beginning.
Full-thickness flaps, which denude the bone, result in superficial bone necrosis after 1 to 3 days. Osteoclastic resorption follows and reaches a peak at 4 to 6 days and then declines thereafter. This results in a loss of bone of about 1 mm; the bone loss is greater if the bone is thin.
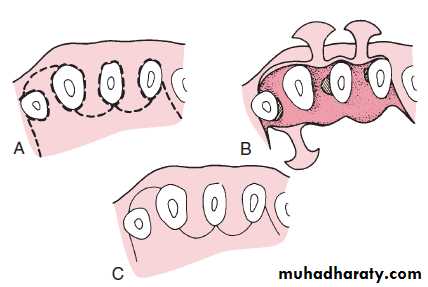
Osseous surgery may be defined as the procedure by which changes in the alveolar bone can be accomplished to rid it of deformities induced by the periodontal disease process or other related factors such as exostosis and tooth supraeruption
Osseous Surgery
Osseous surgery can be either additive or subtractive.
Additive osseous surgery includes procedures directed at restoring the alveolar bone to its original level, whereassubtractive osseous surgery is designed to restore the form of preexisting alveolar bone to the level present at the time of surgery or slightly more apical to this level
Procedures used to correct osseous defects have been classified in two groups: osteoplasty and ostectomy. Osteoplasty refers to reshaping the bone without removing tooth-supporting bone.
Ostectomy, or osteoectomy, includes the removal of tooth-supporting bone.
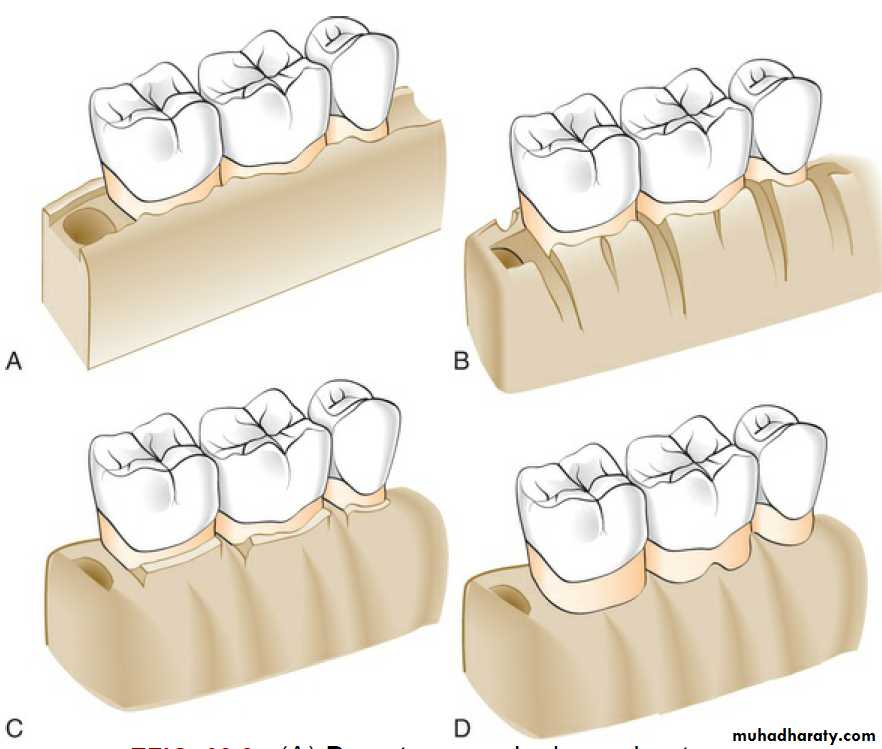
Bony lesions have been classified according to their configuration and number of bony walls:
one wall bone defect
two walls bone defect (Two-walled defects, or craters). Two-walled defects (craters) are the most common bony defects found in patients with periodontitis.
Three wall bone defect
Peaks of bone typically remain at the facial and lingual-palatal line angles of the teeth (widow's peaks).
Examples of morphologically descriptive terms include negative, positive, flat, and ideal. These terms all relate to a preconceived standard of ideal osseous form.
Positive architecture and negative architecture refer to the relative position of interdental bone to radicular bone. The architecture is “positive” if the radicular bone is apical to the interdental bone. The bone has “negative” architecture if the interdental bone is more apical than the radicular bone.
Flat architecture is the reduction of the interdental bone to the same height as the radicular bone.
the following sequential steps are suggested for resective osseous surgery:
1. Vertical grooving2. Radicular blending
3. Flattening interproximal bone
4. Gradualizing marginal bone.
Critical probing depth
Initial P.depth value below which LA likely to occur & above which CAL gain often result following therapySo above CPD more gain following surgery than RP
Below CPD more LA with surgery than RP
Value of CPD smaller for S.& RP than for surgery
Critical probing depth
For RP 2.9-+o.3mm while for MWF 4.2 -+0.2mmP. less than 2.9mm;
no treatment
P. more than 2.9mm & less than 4.2mm ;
RP
P. deeper than 4.2mm;
MWF
Critical probing depth
Large no. of shallow p.;no surgical approach
Large no. of deep p.;
surgical approach (more gain)
More gain of CAL occur in B.,L.,incisors & premolars because of better access & visibility
so RP alone is successful in such area