بسم الله الرحمن الرحيم
24/01/2021 a.c.
RESPIRATORY MEDICINE
Pulmonary TuberculosisObjectives
To know the followingEpidemiology
Etiology
Pathogenesis
Clinical presentation
Diagnosis
Treatment
Complication and prognosis
Case 1
Twenty five years old female presented with 2 months fever ,night sweating,weight loss.Dry cough
Tem 38 c R.Rate 20
Chest clear.
What is d dx will include.
Case 2
Seventeen years student present with heamoptysis ,fever ,weight loss
What investigation?
What D dx ?
Case 3
Sixty five years old male present with weight loss fatigue, enlargment of liver and spleen.What is next ?
Introduction
Tuberculosis (TB) is one of the oldest diseases known to affected humans.Caused by bactria of mycobacterium complex, and usually affects the lungs.
Transmitted by airborne droplet nuclei from infected persons.
Curable if properly treated .
May be fatal within 5 years in 50-60%of cases if not treated
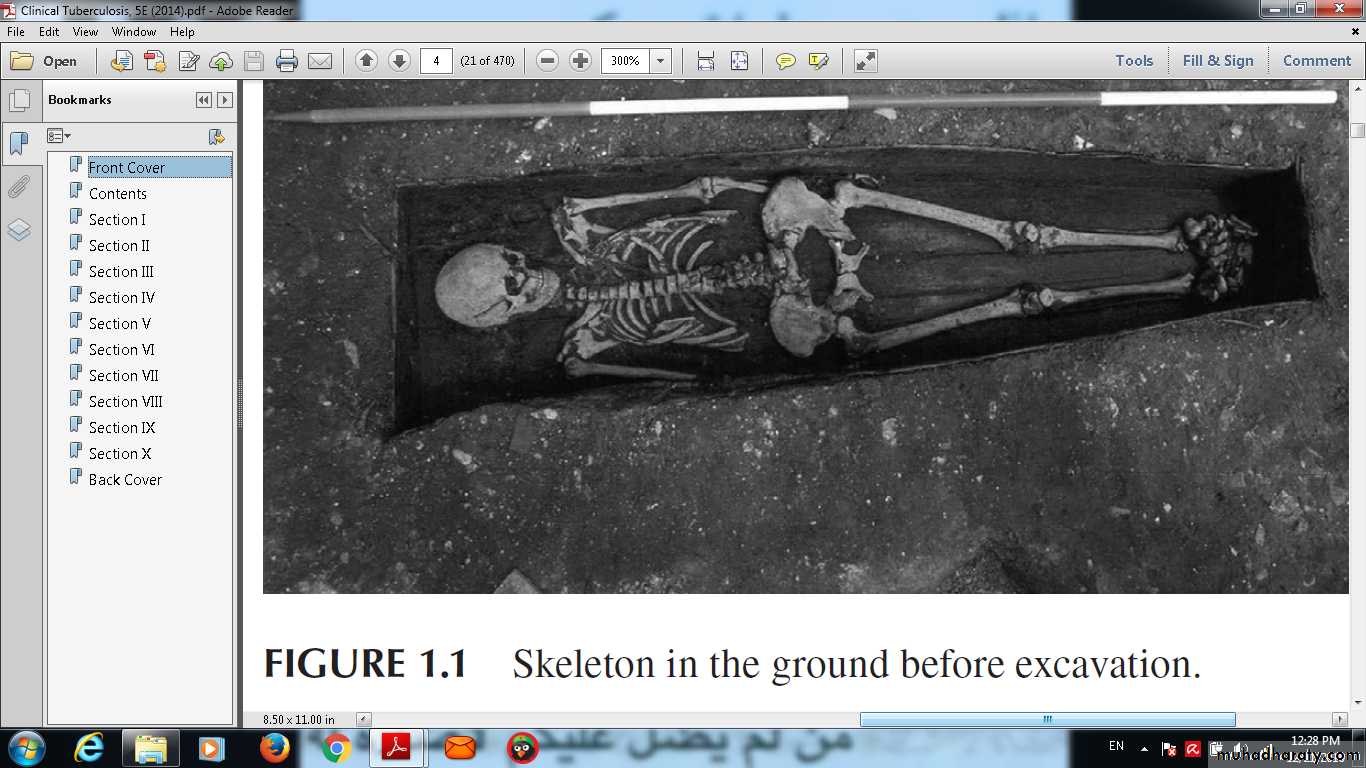
Old Disease
Oldest cases of T B
Epidemiology
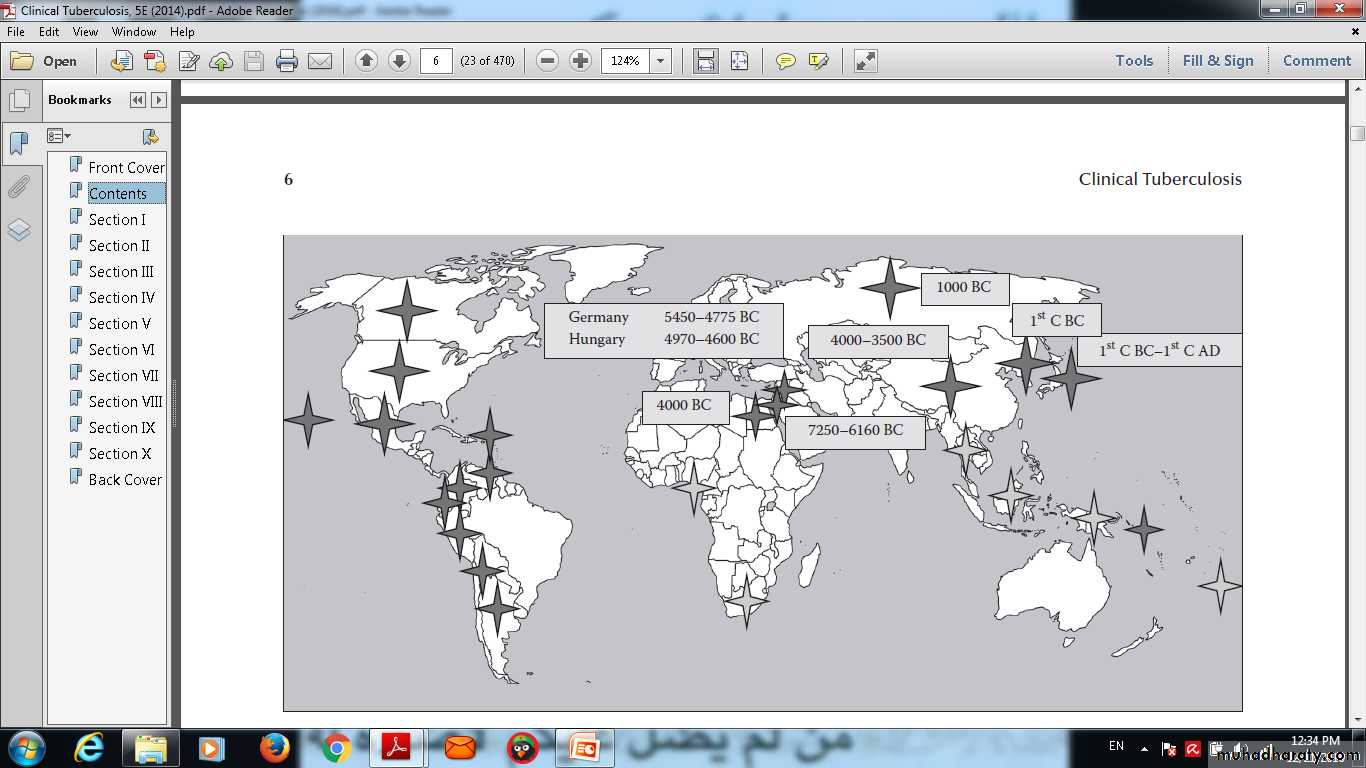
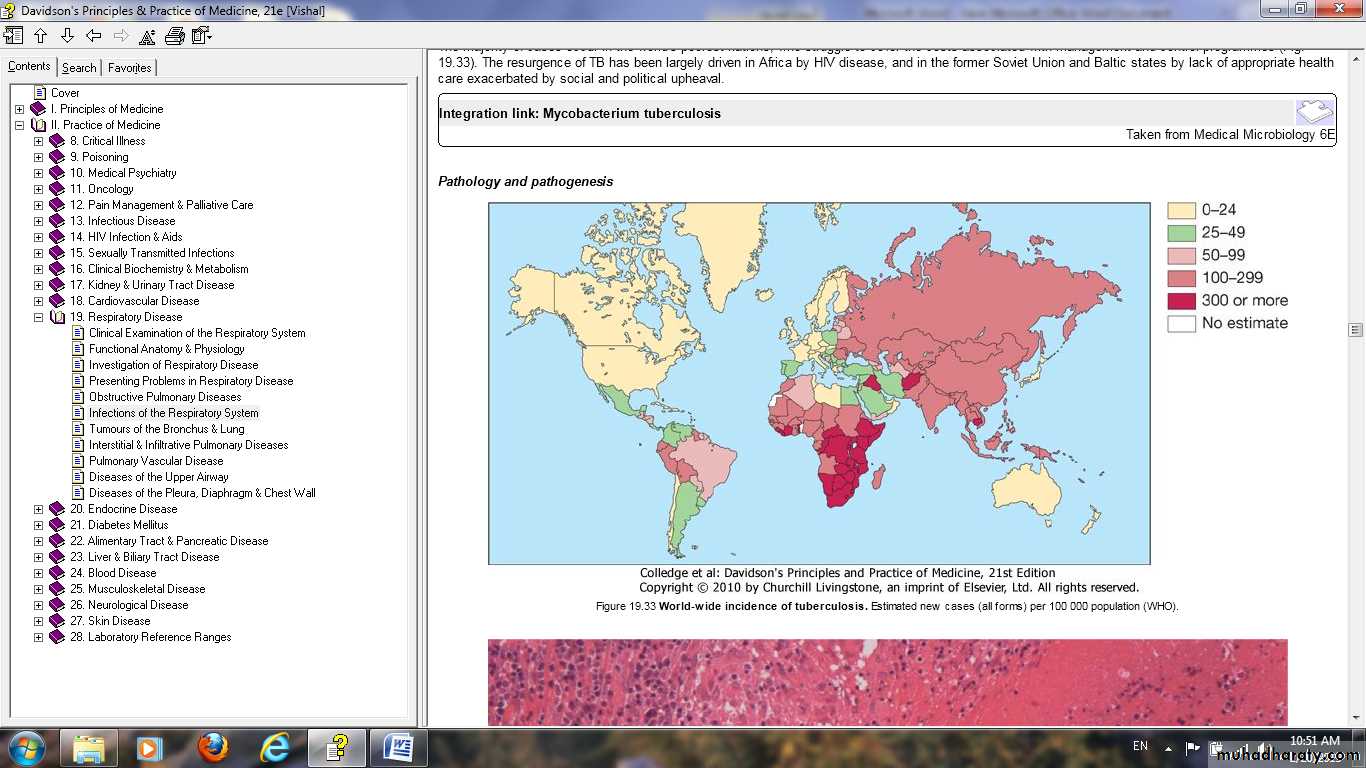
Tuberculosis (TB) is caused by infection with Mycobacterium tuberculosis (MTB).In 2006
There were an estimated 9.2 million new cases, 14.4 million prevalent cases and 1.5 million deaths attributable to TB.
Around one-third of the world's population has latent TB.
The majority of cases occur in the world's poorest nations.
The resurgence of TB has been largely driven by HIV disease and by lack of appropriate health care.
Iraq has a
high burden of TB, the estimated incidencewas 45 per 100,000.
Prevalence is 74 per 1 00 000.
Mortality is 3 per 1 00 000.
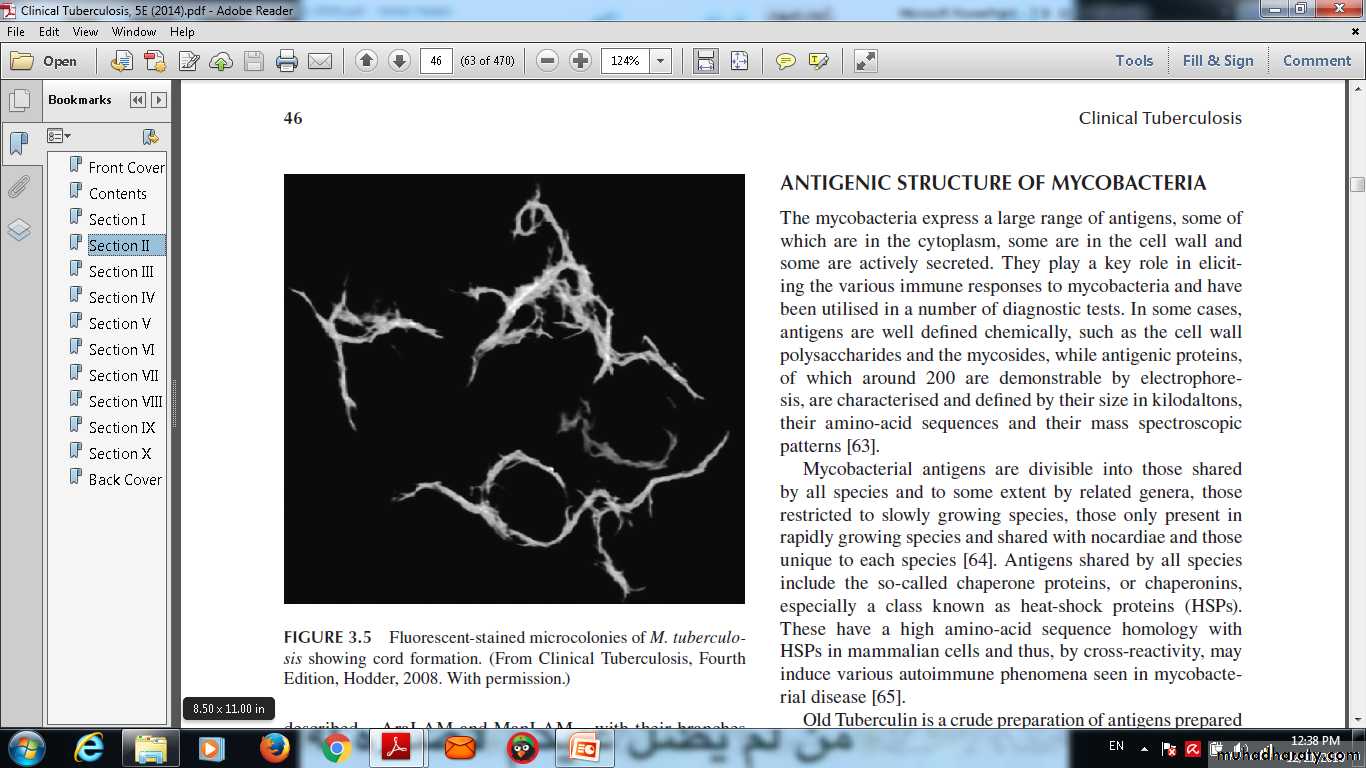
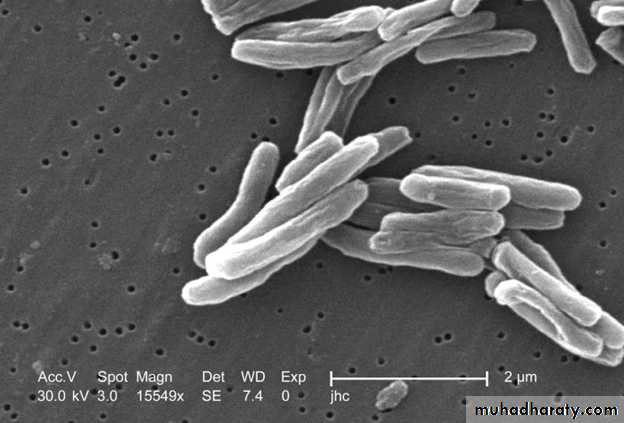
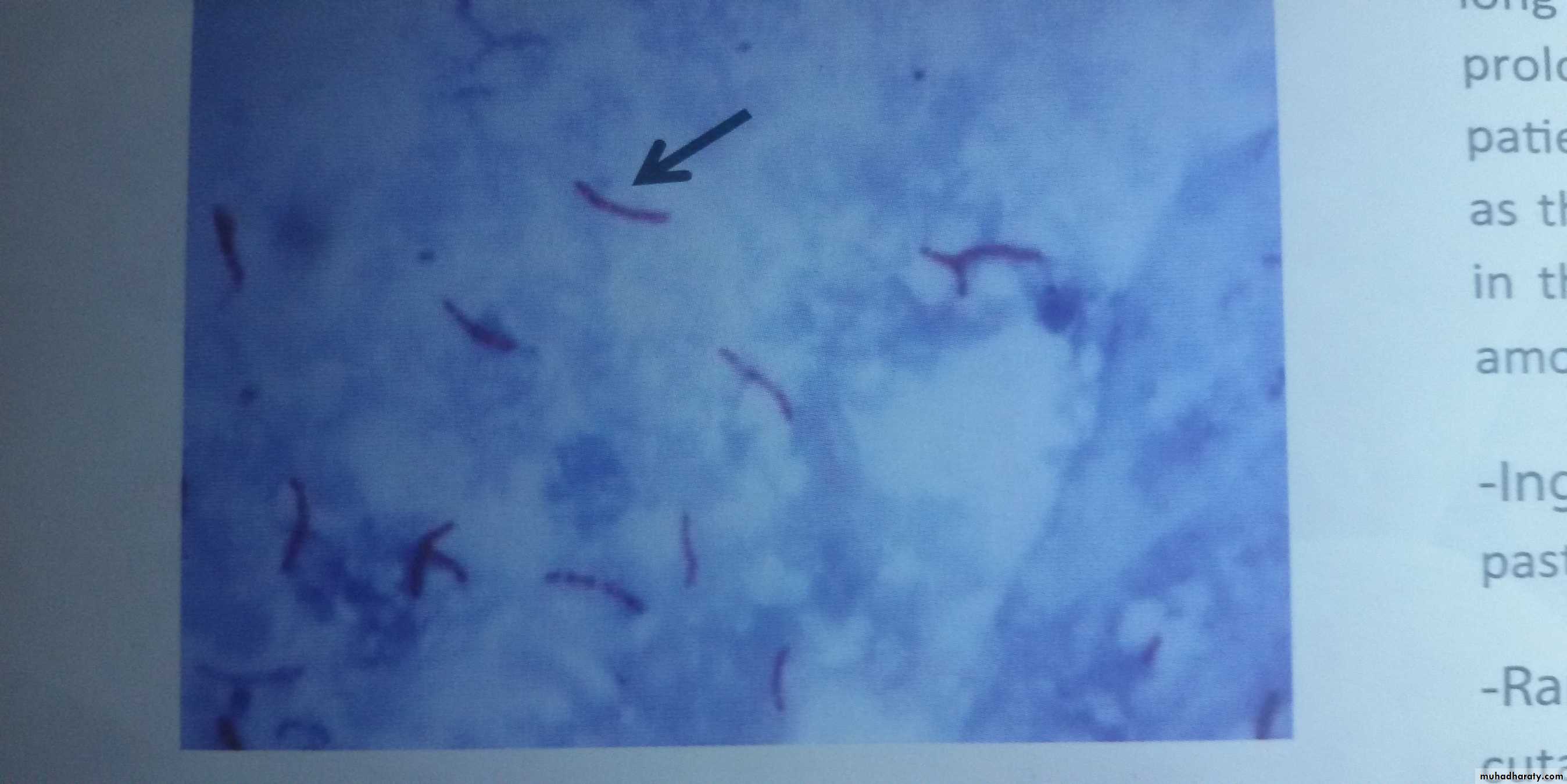
Flourescent stained microcolonies of M.tuberclonies .
Pathology and pathgenesis
M. bovis infection arises from drinking non-sterilized milk from infected cows.M. tuberculosis is spread by the inhalation of aerosolised droplet nuclei from other infected patients.
Once inhaled, the organisms lodge in the alveoli and initiate the recruitment of macrophages and lymphocytes.
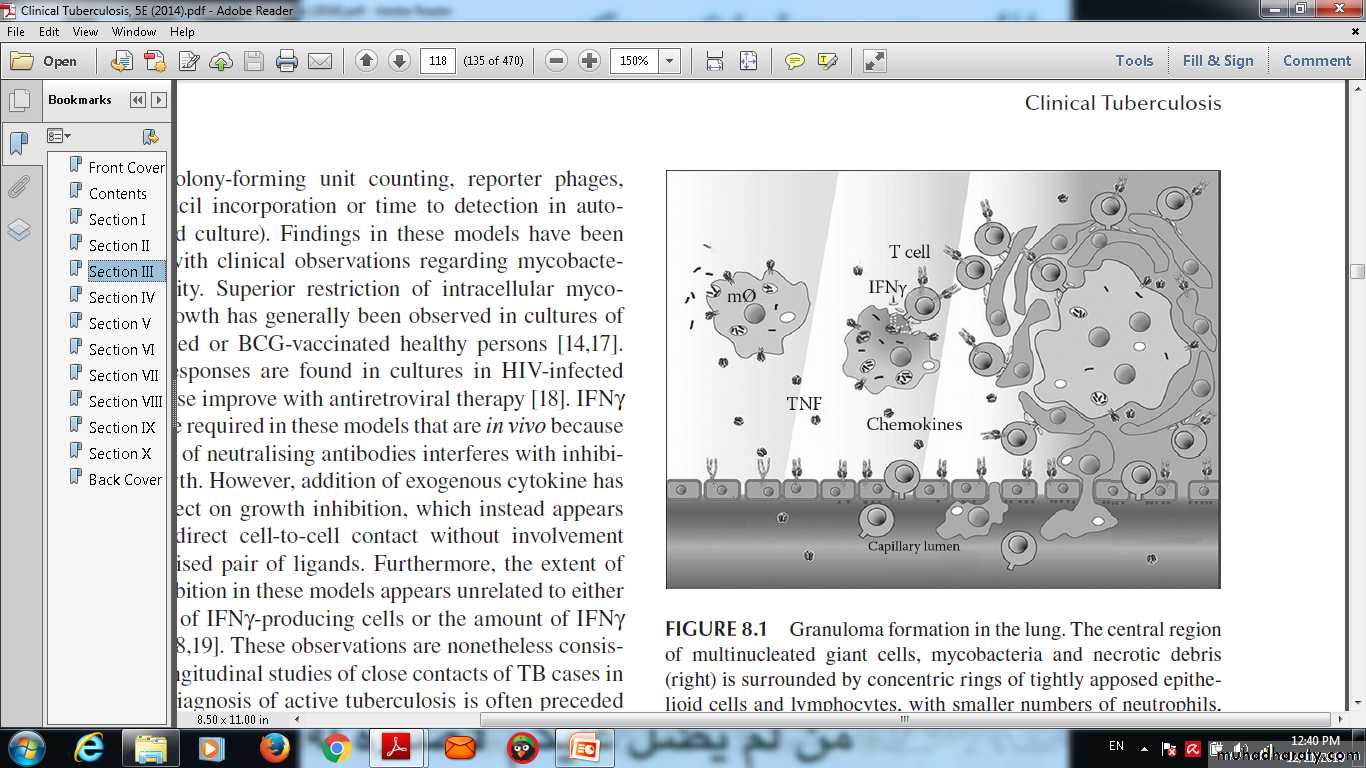
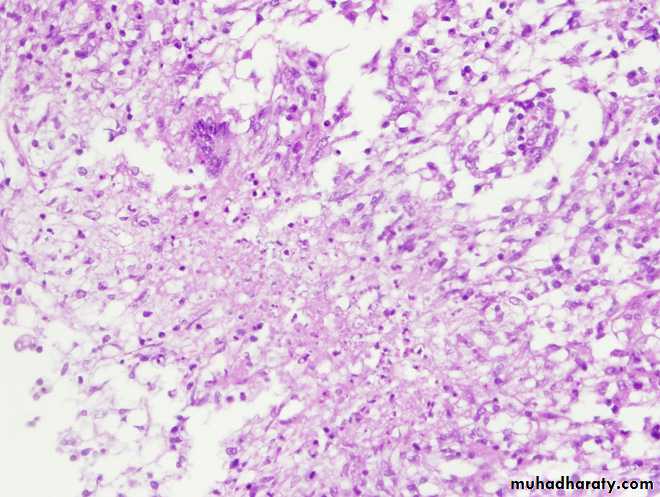
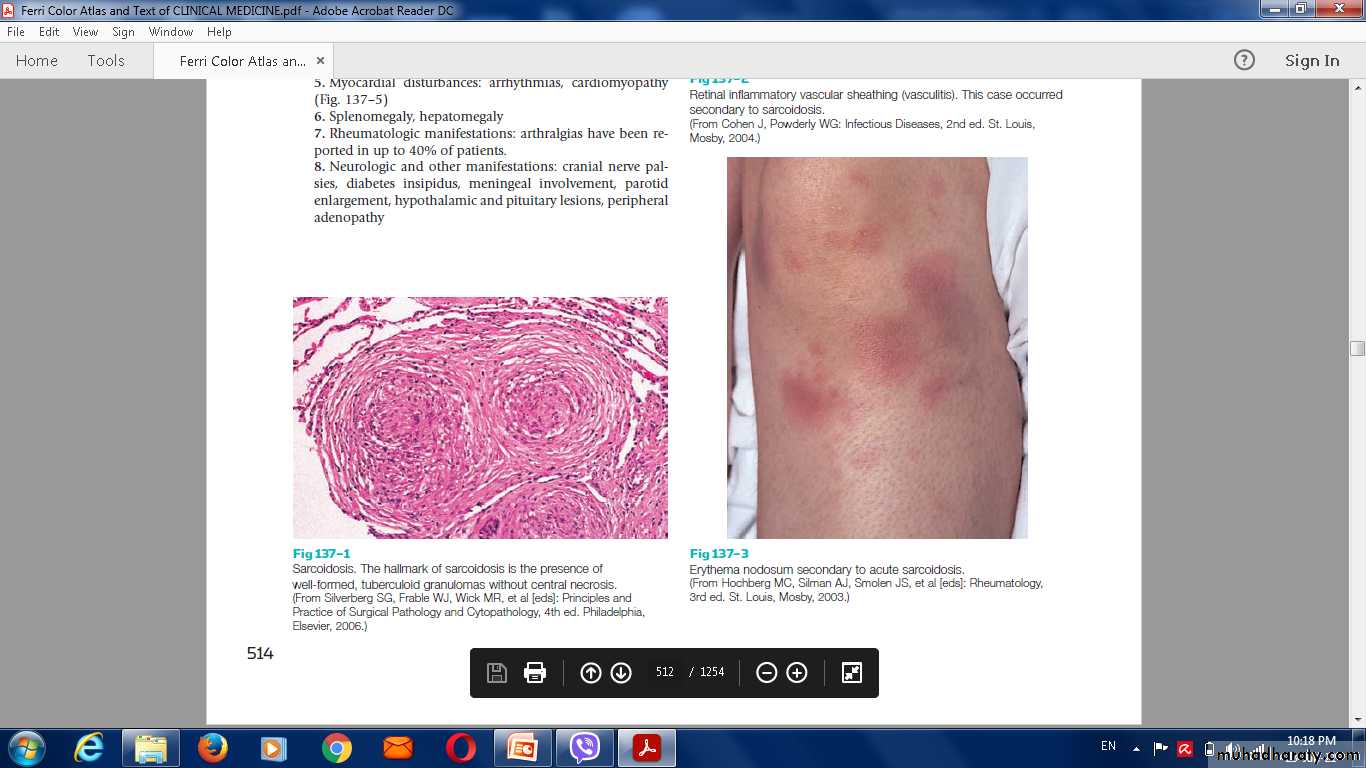
Macrophages undergo transformation into epithelioid and Langhans cells which aggregate with the lymphocytes to form the classical tuberculous granuloma .
Granuloma formation in the lung. The central region of multinucleated giant cells, mycobacteria and necrotic debris (right) is surrounded by concentric rings of tightly apposed epithelioid cells and lymphocytes, with smaller numbers of neutrophils, plasma cells and fibroblasts.
Primary lesion or 'Ghon focus
Form from aggregation of numerous granulomas which is situated in the periphery of the lung.‘Primary complex of Ranke
The combination of a primary lesion and regional lymph nodes ( the hilar lymph nodes) which has similar pathological reaction .Latent TB
the primary complex in a fibrous capsule limiting the spread of bacilli WHICH calcifies and is seen on a chest X-ray.
Spread
1-lymphatic 2- or haematogenous
before immunity>>> seeding secondary foci in other organs including lymph nodes, serous membranes, meninges, bones, liver, kidneys and lungs, which may lie dormant for years.
What Tuberculin skin test ?
The appearance of a cell-mediated, delayed-type hypersensitivity reaction to tuberculin in skin test.Electron microscopy show T.B bacilli
Granuloma
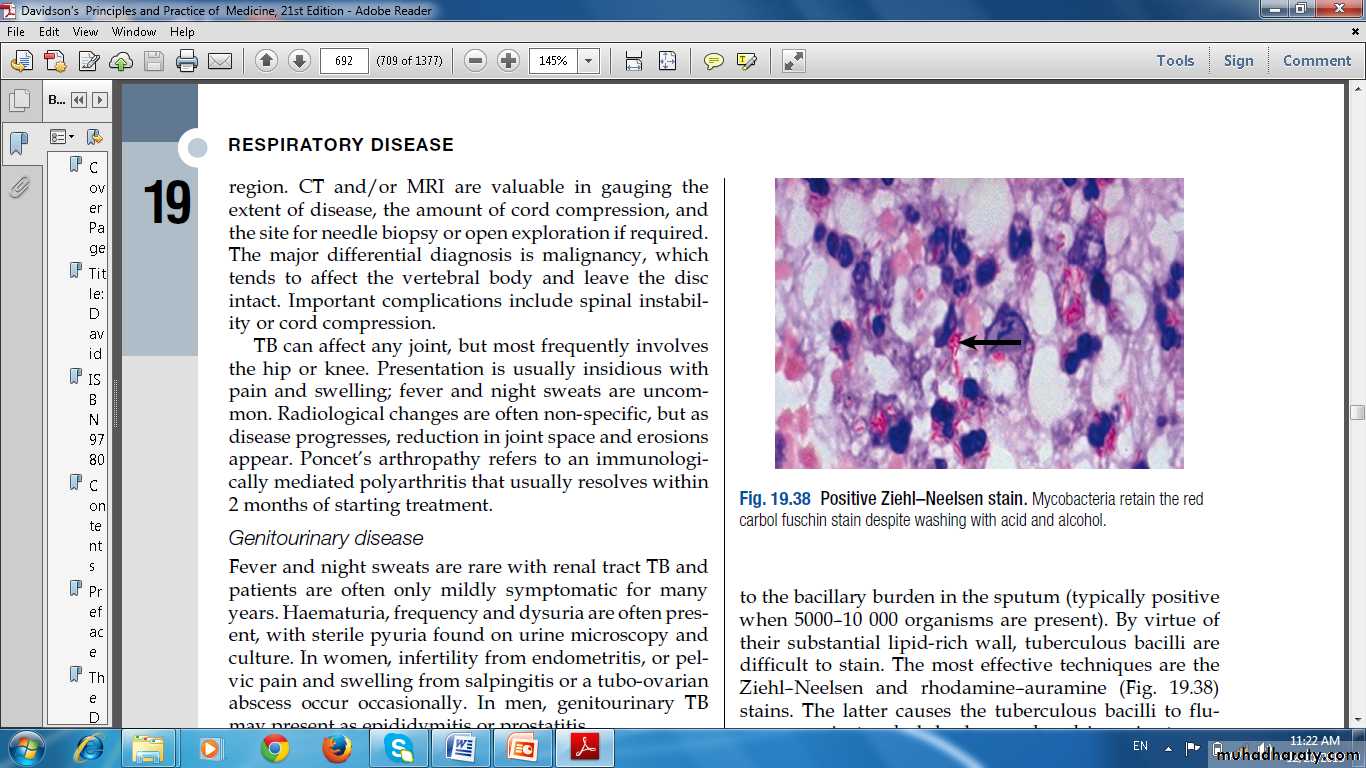
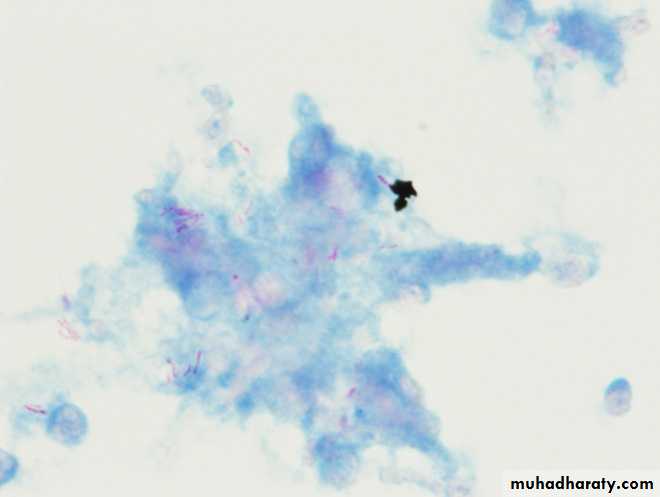
Positive Ziehl–Neelsen stain. Mycobacteria retain the redcarbol fuschin stain despite washing with acid and alcohol.
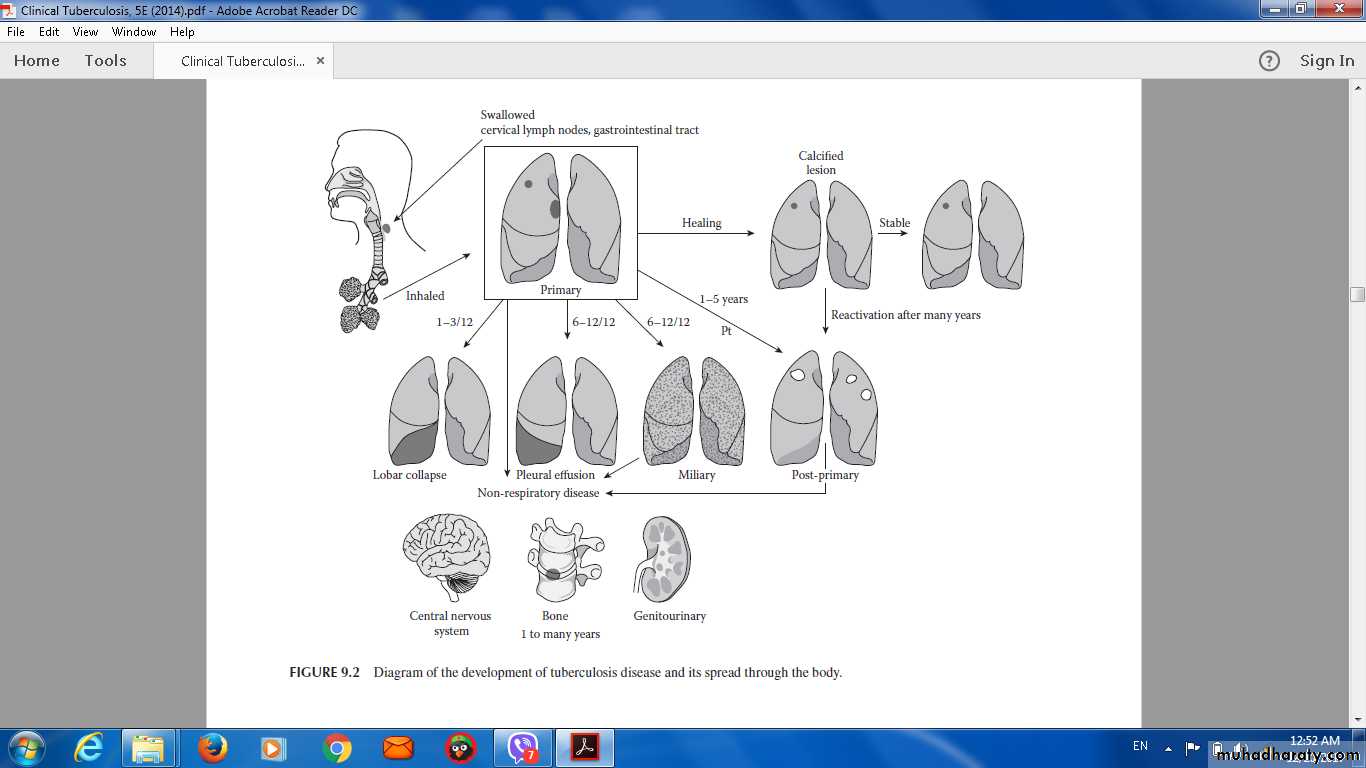
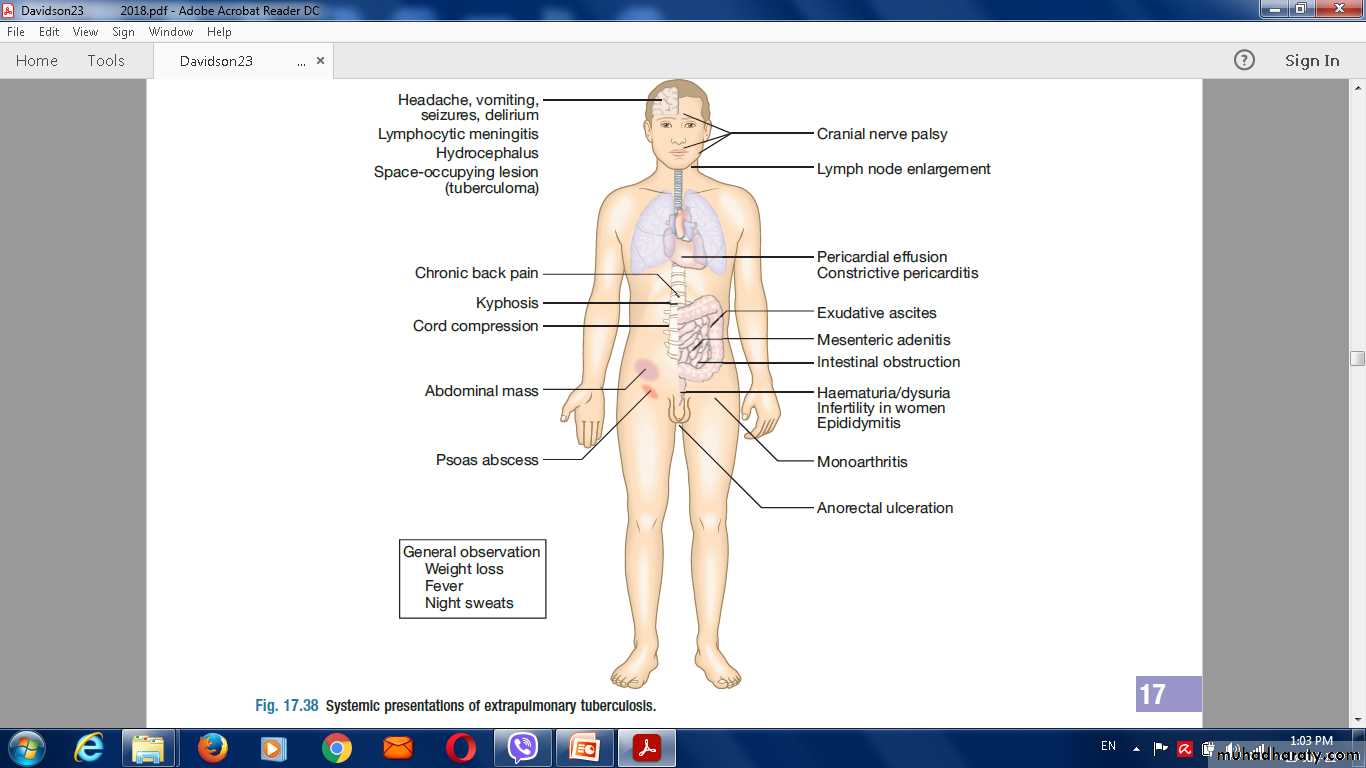
Diagram of the development of tuberculosis disease and its spread through the body.
Timetable of TB
Time from infection Manifestations3-8 weeks Primary complex, positive tuberculin skin test
3-6 months Meningeal, miliary and pleural disease
Up to 3 years Gastrointestinal, bone and joint, and lymph node disease
Around 8 years Renal tract disease
From 3 years onwards Post-primary disease due to reactivation or reinfection
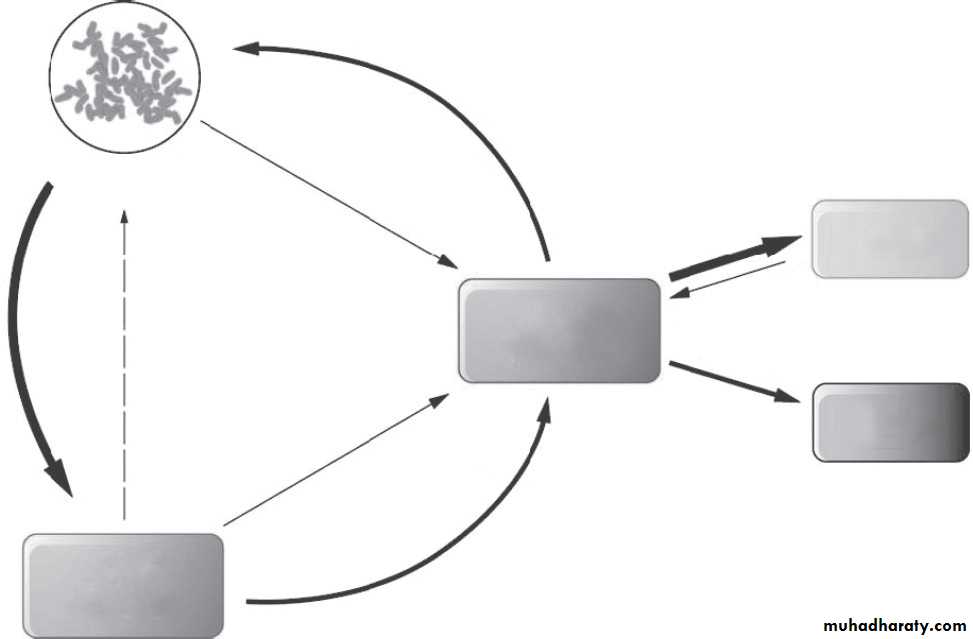
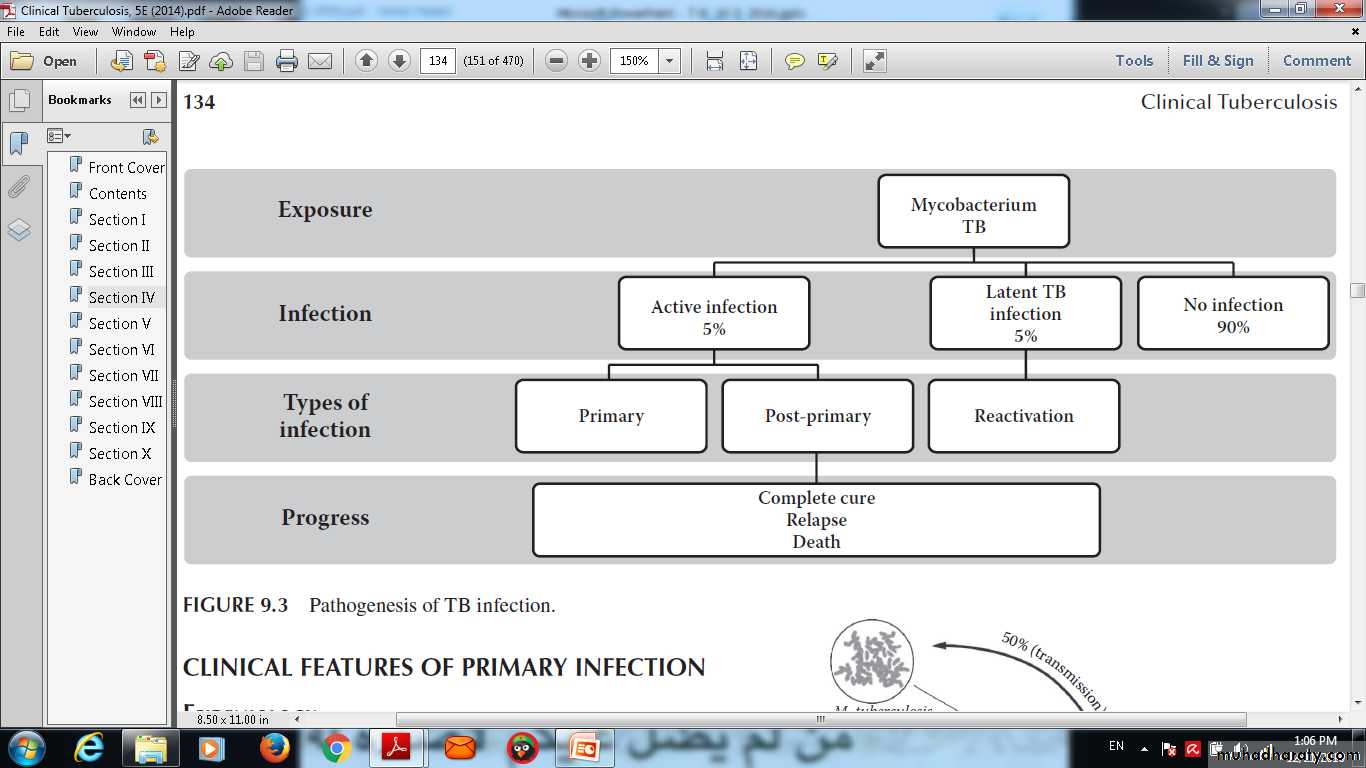
Pathogenesis of TB infection
The answer
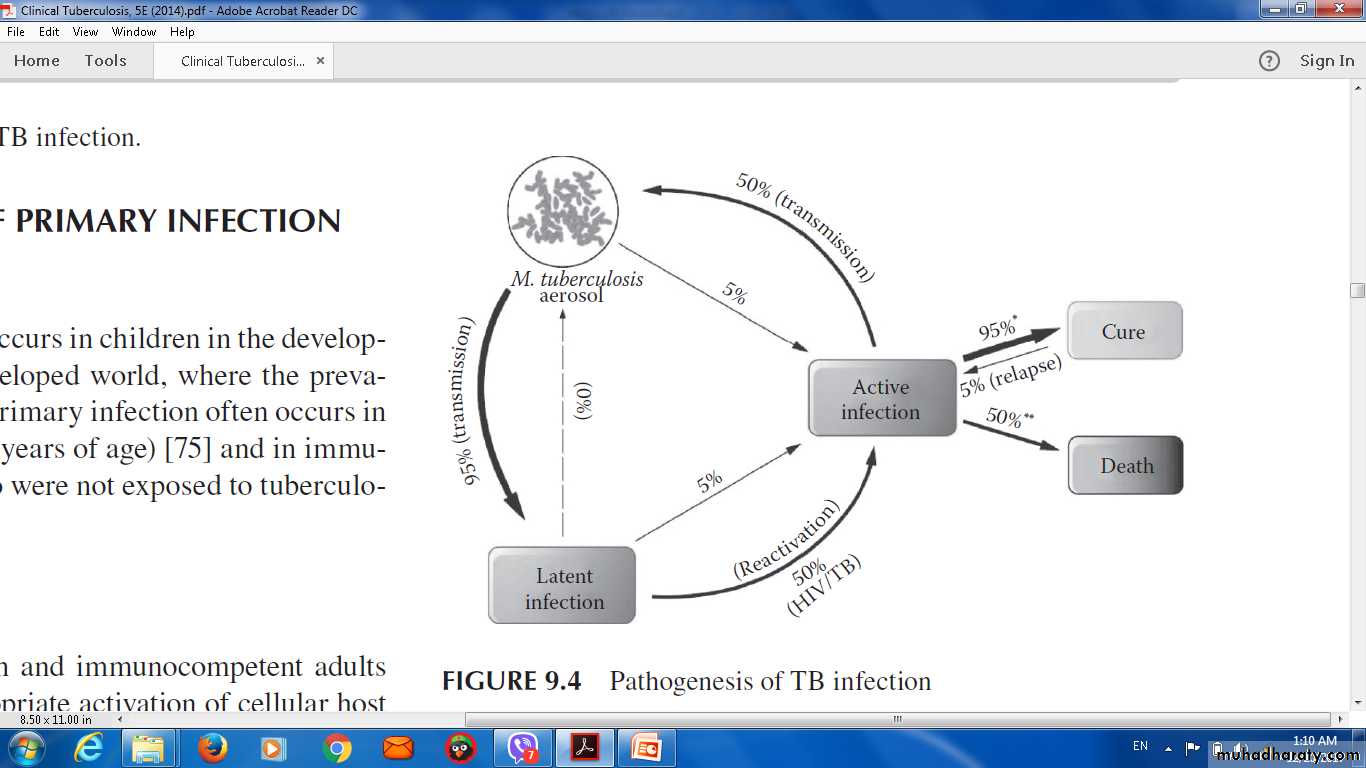
Primary pulmonary TB. (1) Spread from the primary focus tohilar and mediastinal lymph glands to form the ‘primary complex’, which inmost cases heals spontaneously. (2) Direct extension of the primary focus—progressive pulmonary TB. (3) Spread to the pleura—tuberculous pleurisyand pleural effusion. (4) Blood-borne spread: few bacilli—pulmonary,skeletal, renal, genitourinary infection often months or years later; massivespread—miliary TB and meningitis.
Primary pulmonary TB.
(1) Spread from the primary focus to hilar and mediastinal lymph glands to form the 'primary complex', which in most cases heals spontaneously.(2) Direct extension of the primary focus-progressive pulmonary TB.
(3) Spread to the pleura-tuberculous pleurisy and pleural effusion.
(4) Blood-borne spread: few bacilli-pulmonary, skeletal, renal, genitourinary infection often months or years later; massive spread-miliary TB and meningitis
Factors increasing the risk of TB
I--Patient-related
Age (children > young adults < elderly)
First-generation immigrants from high-prevalence countries
Close contacts of patients with smear-positive pulmonary TB
Overcrowding (prisons,); homelessness .
Chest radiographic evidence of self-healed TB
Primary infection < 1 year previously
Smoking: cigarettes and bidis (indian cigarettes) .
II—Associated diseases
Immunosuppression: HIV, anti-TNF therapy, high-dose corticosteroids, cytotoxic agents.Malignancy (especially lymphoma and leukaemia)
Type 1 diabetes mellitus
Chronic renal failure
Silicosis
Gastrointestinal disease associated with malnutrition
Deficiency of vitamin D or A
Recent measles.
Pathogenesis and progress of T B
Clinical features:
Pulmonary diseasePrimary pulmonary TB.
Post primary pulmonary T B.
Miliary TB.
Cryptic TB.
Features of primary TB
Infection (4-8 weeks)Influenza-like illness
Skin test conversion
Primary complex
Features of primary TB
DiseaseLymphadenopathy: hilar (often unilateral). paratracheal or mediastinal .
Collapse (especially right middle lobe) .
Consolidation (especially right middle lobe) .
Obstructive emphysema .
Pleural effusion .
Endobronchial .
Miliary .
Meningitis.
Pericarditis .
Hypersensitivity
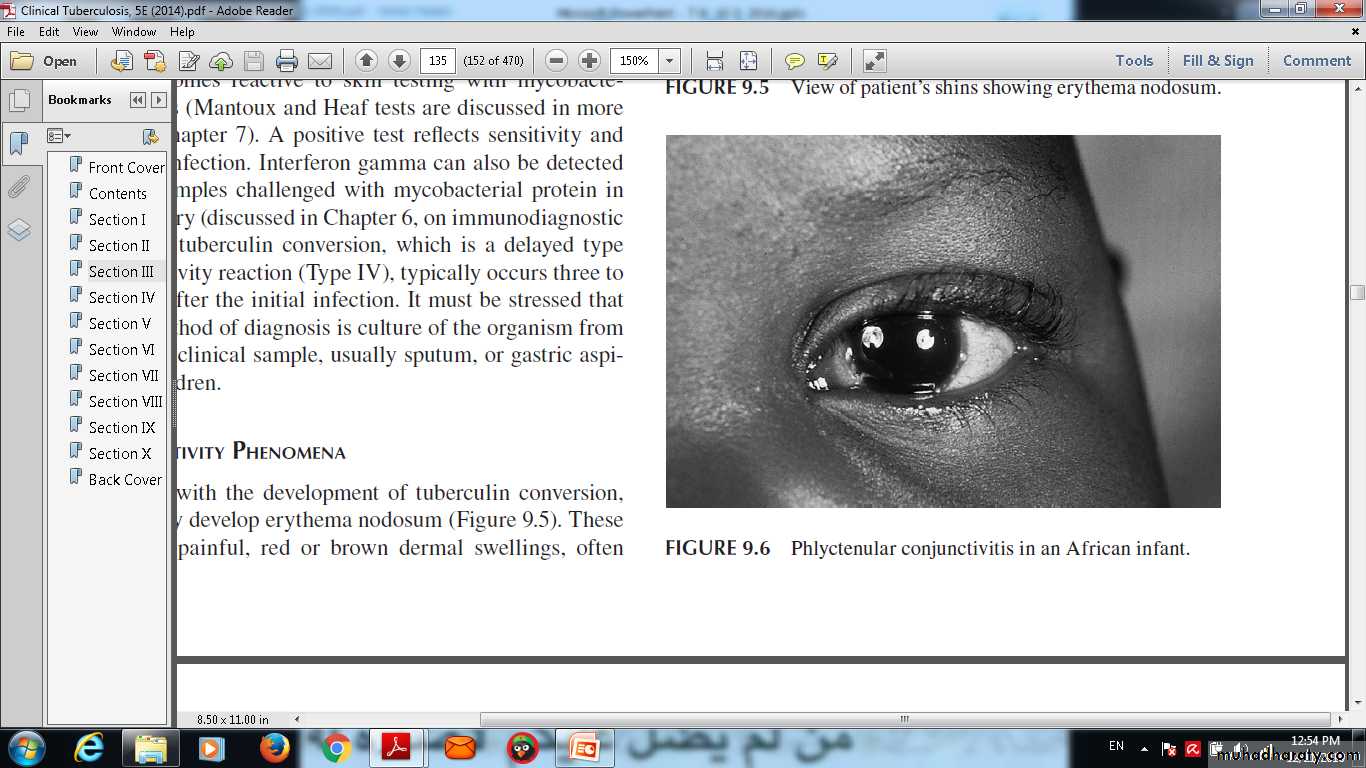
Erythema nodosum .
Phlyctenular conjunctivitis .
Dactylitis.
Erythema nodosum
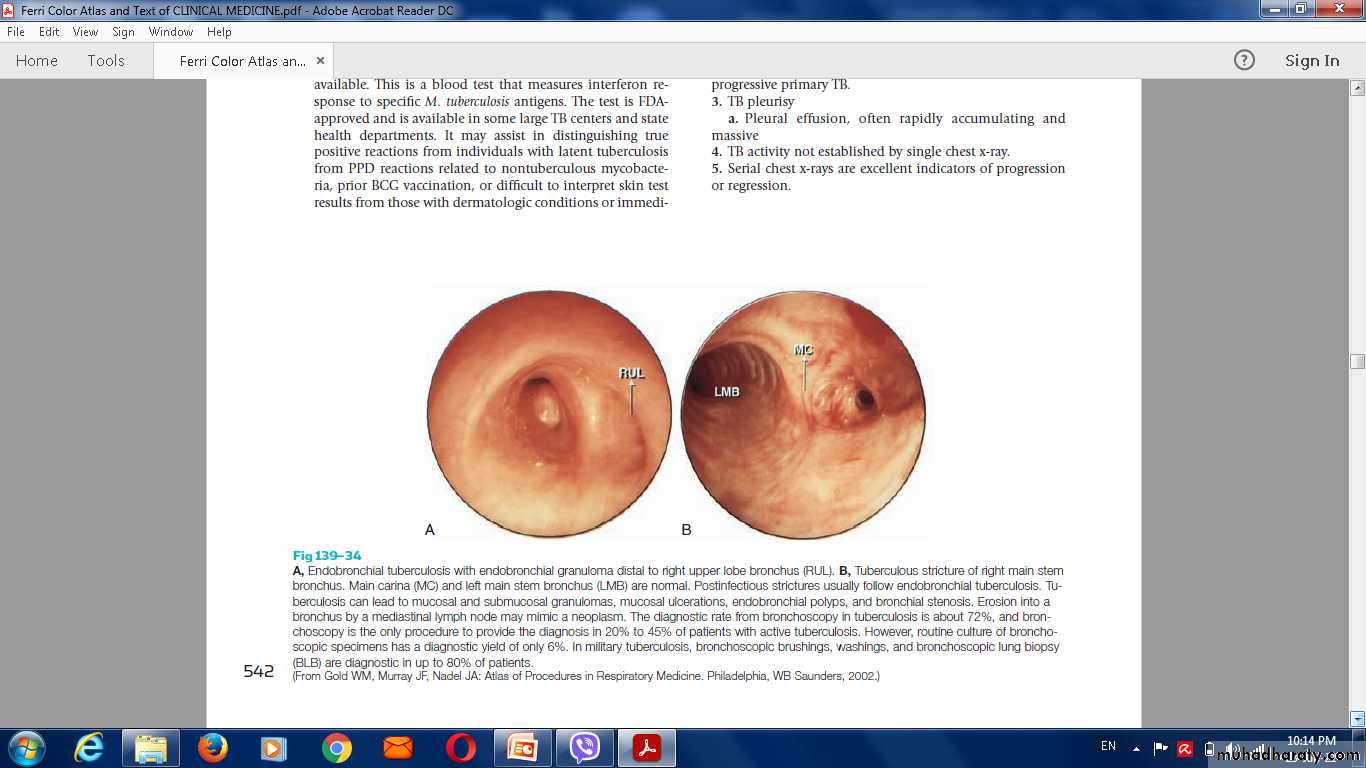
Endobronchial TB
Phlyctenullar conjuctivitis
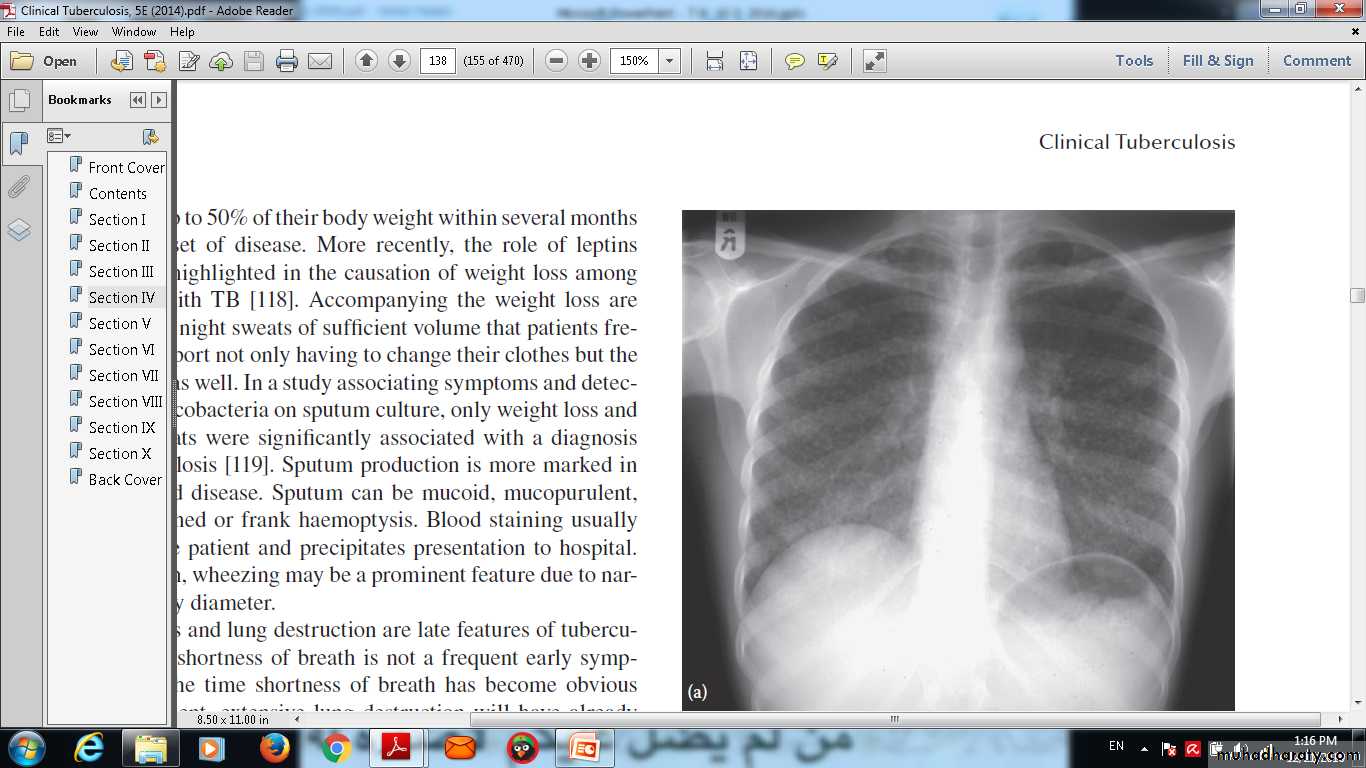
Miliary TB
Blood-borne disseminationacute
2-3 weeks of fever,
night sweats,
anorexia,
weight loss
dry cough.
Hepatosplenomegaly
headache may indicate tuberculous meningitis.
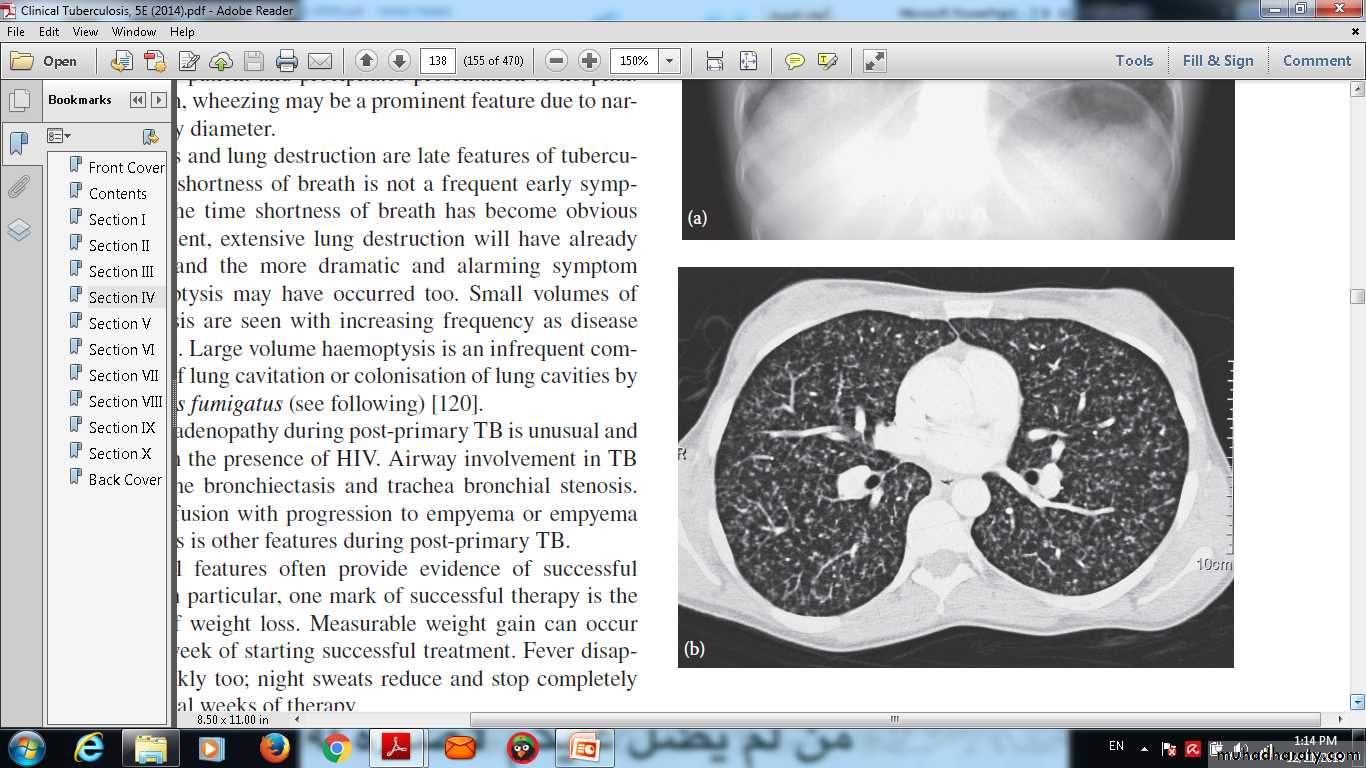
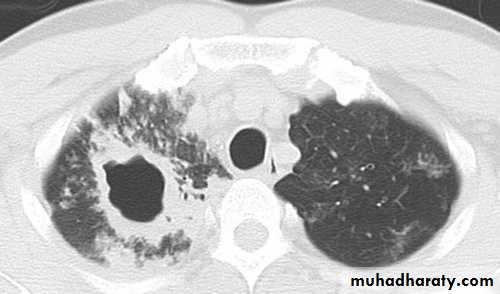
(a) Chest x-ray and (b) CT scan from a 27-year-old student with disseminated tuberculosis . Multiple small opacities (miliary shadowing) are seen in the periphery of the chest x-ray and much more clearly in all areas of the CT scan
(a) Chest x-ray and (b) CT scan from a 27-year-old student with disseminated tuberculosis . Multiple small opacities (miliary shadowing) are seen in the periphery of the chest x-ray and much more clearly in all areas of the CT scan
Auscultation of the chest is frequently normal, advanced disease crackles .
Fundoscopy show choroidal tubercles.The classical appearances on chest X-ray are of fine 1-2 mm lesions ('millet seed').
Anaemia and leucopenia reflect bone marrow involvement.
'Cryptic' miliary TB
Age over 60 yearsIntermittent low-grade pyrexia of unknown origin
Unexplained weight loss, general debility (hepatosplenomegaly in 25-50%)
Normal chest X-ray
Blood dyscrasias; leukaemoid reaction, pancytopenia
Negative tuberculin skin test
Confirmation by biopsy (granulomas and/or acid-fast bacilli demonstrated) of liver or bone marrow
Post-primary disease
Exogenous ('new' infection)
Endogenous (reactivation of a dormant primary lesion)Lung apices .
The onset insidious, slowly over several weeks.
Systemic symptoms
progressive pulmonary symptoms .
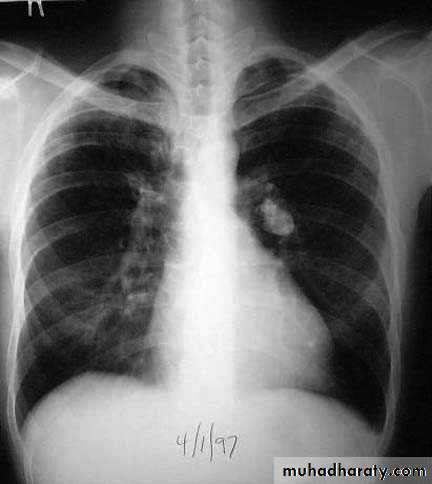
Radiological changes include
opacification in one or both of the upper lobes,
consolidation
collapse
cavitation
tuberculous pneumonia
Chronic complications of pulmonary TB
PulmonaryMassive haemoptysis
Cor pulmonale
Fibrosis/emphysema
Atypical mycobacterial infection
Aspergilloma
Lung/pleural calcification
Obstructive airways disease
Bronchiectasis .
Bronchopleural fistula
Case
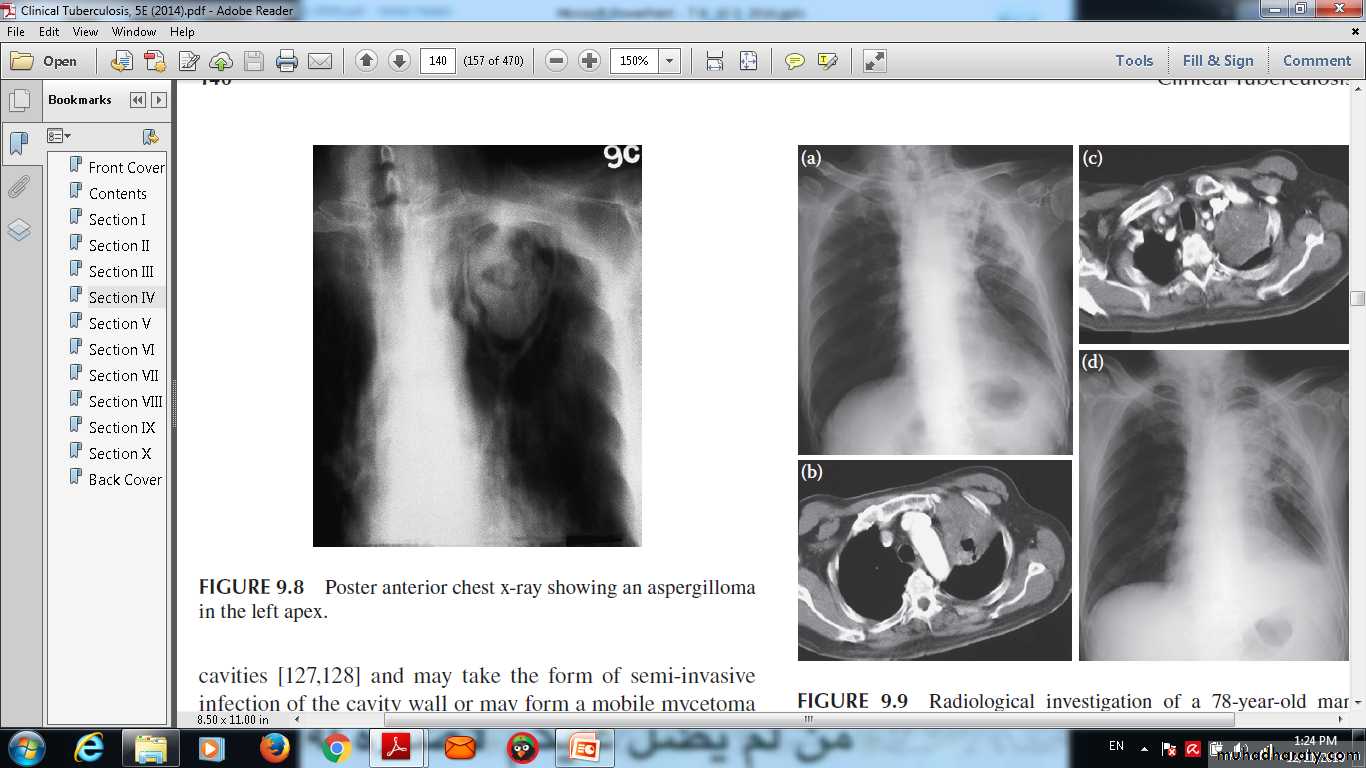
Radiological investigation of a 78-year-old man with a six-week history of productive cough, fever, left-sided chest pain, dyspnoea on exertion and hoarse voice . (a) Chest x-ray and (b) CT scan showed (c) a soft tissue mass in the left upper lobe that encased the left upper lobe bronchus. (d) A chest x-ray performed at the end of TB treatment showed a significant resolution of the initial consolidation seen in the left upper lobe, persistence of the mass (diagnosed as being carcinoid tumour), left upper lobe fibrosis, loss of left lung volume, a left pleural effusion and a large heart shadow
.
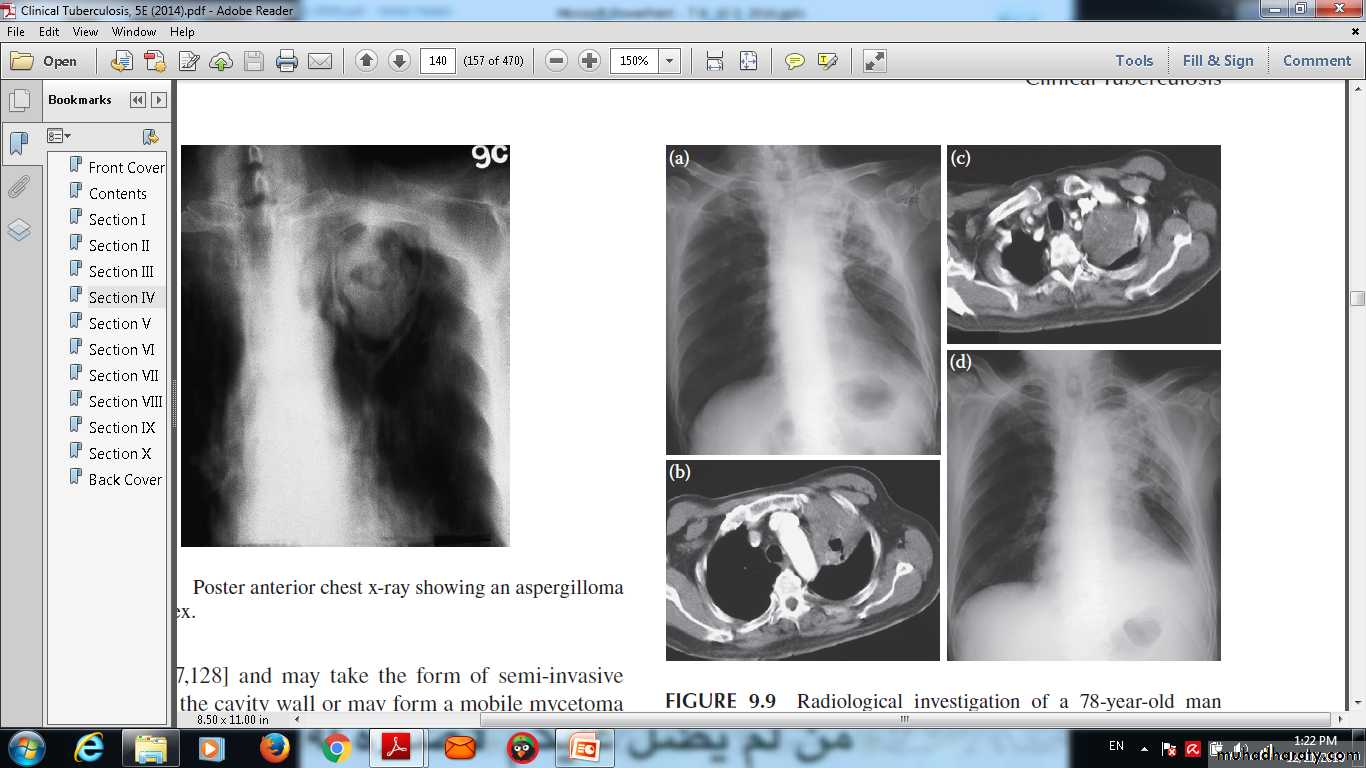
Posteroanterior chest x-ray showing an aspergilloma in the left apex.
Non-pulmonary complication
Empyema necessitans
Laryngitis
Enteritis.
Anorectal disease .
Amyloidosis.
Poncet's polyarthritis
Diagnosis of TB
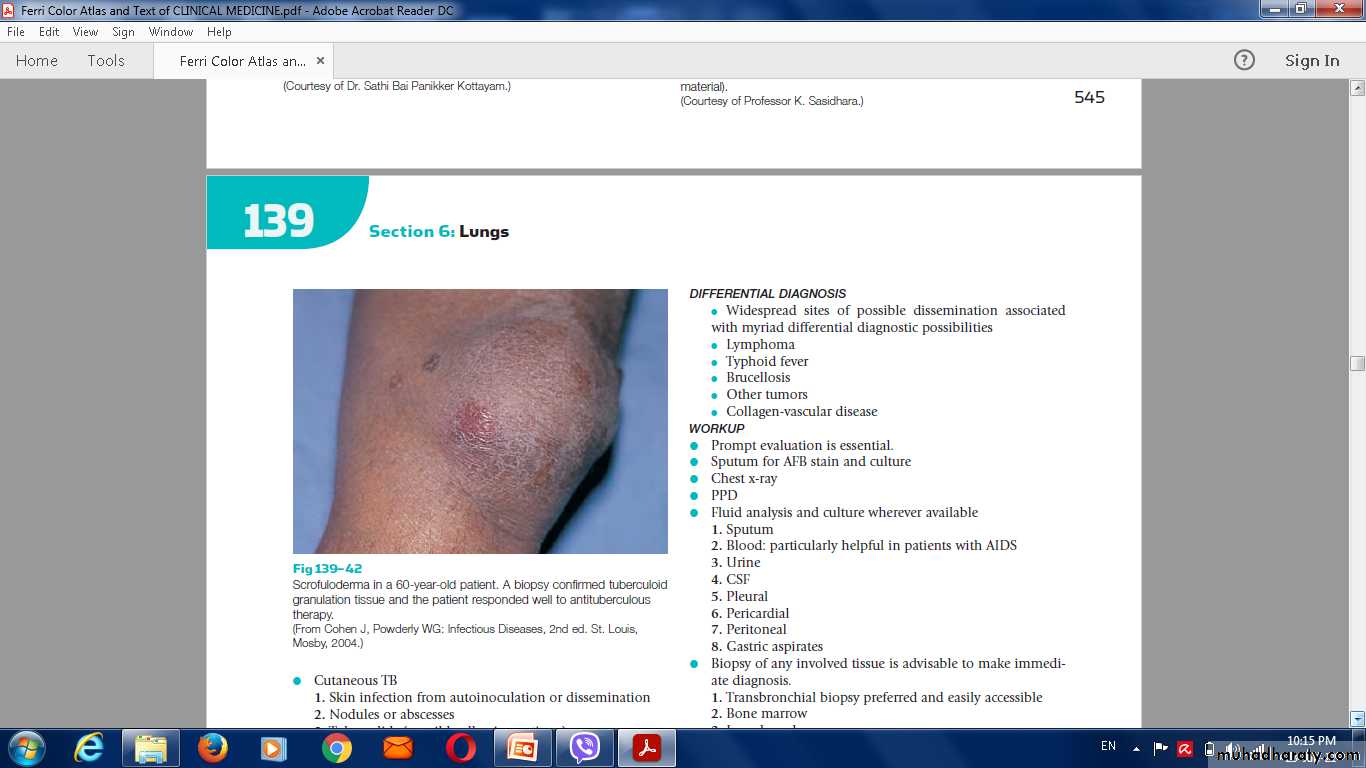
Specimens required
Pulmonary
Sputum (induced with nebulised hypertonic saline if not expectorating)
Bronchoscopy with washings or BAL
Gastric washing (mainly used for children)
Extrapulmonary
Fluid examination (cerebrospinal, ascitic, pleural, pericardial, joint): yield classically very low
Tissue biopsy (from affected site); also bone marrow/liver may be diagnostic in patients with disseminated disease
Diagnostic tests
Circumstantial (ESR, CRP, anaemia etc.)Tuberculin skin test (low sensitivity/specificity; useful only in primary or deep-seated infection)
Stain
Ziehl-Neelsen
Auramine fluorescence
Nucleic acid amplification
Culture
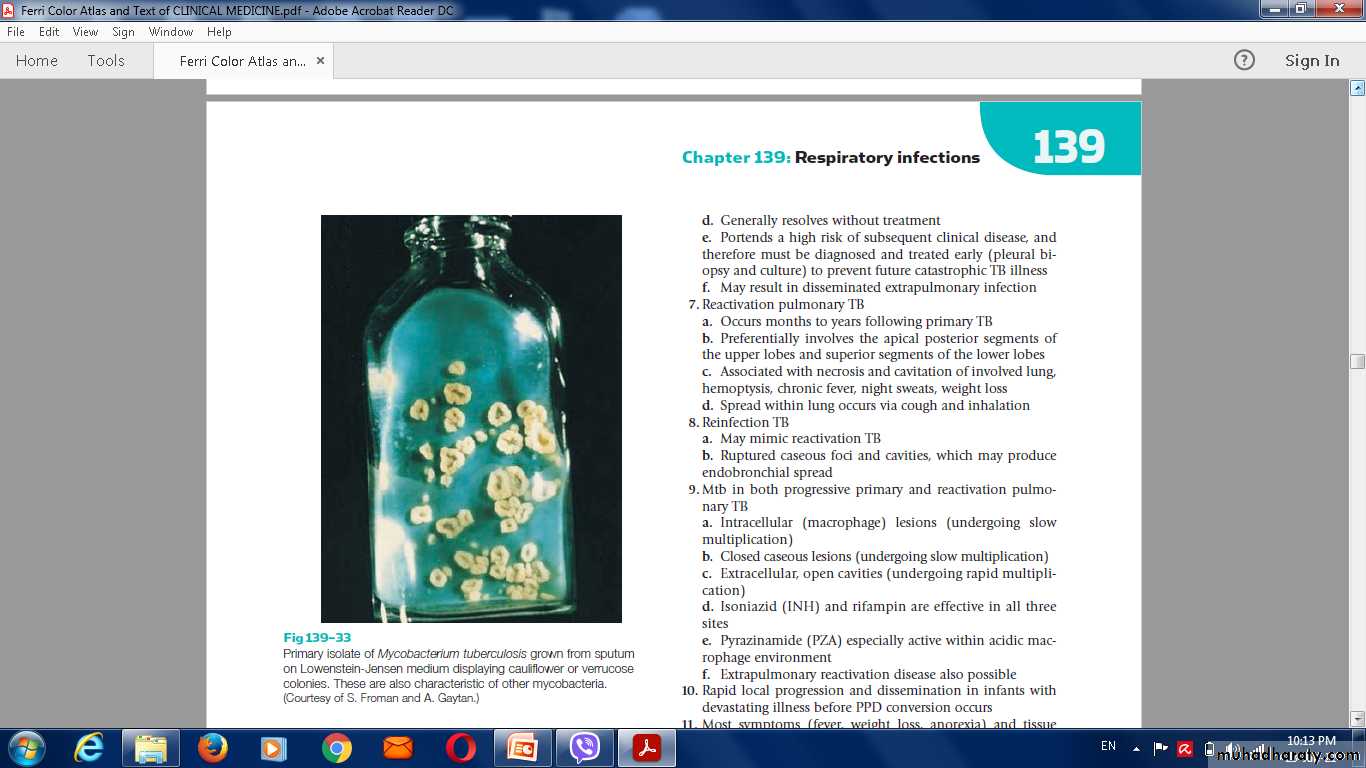
Solid media (Löwenstein-Jensen, Middlebrook)
Liquid media (e.g. BACTEC or MGIT)
Response to empirical antituberculous drugs (usually seen after 5-10 days)
Sputum AFB positive
T B bacilli
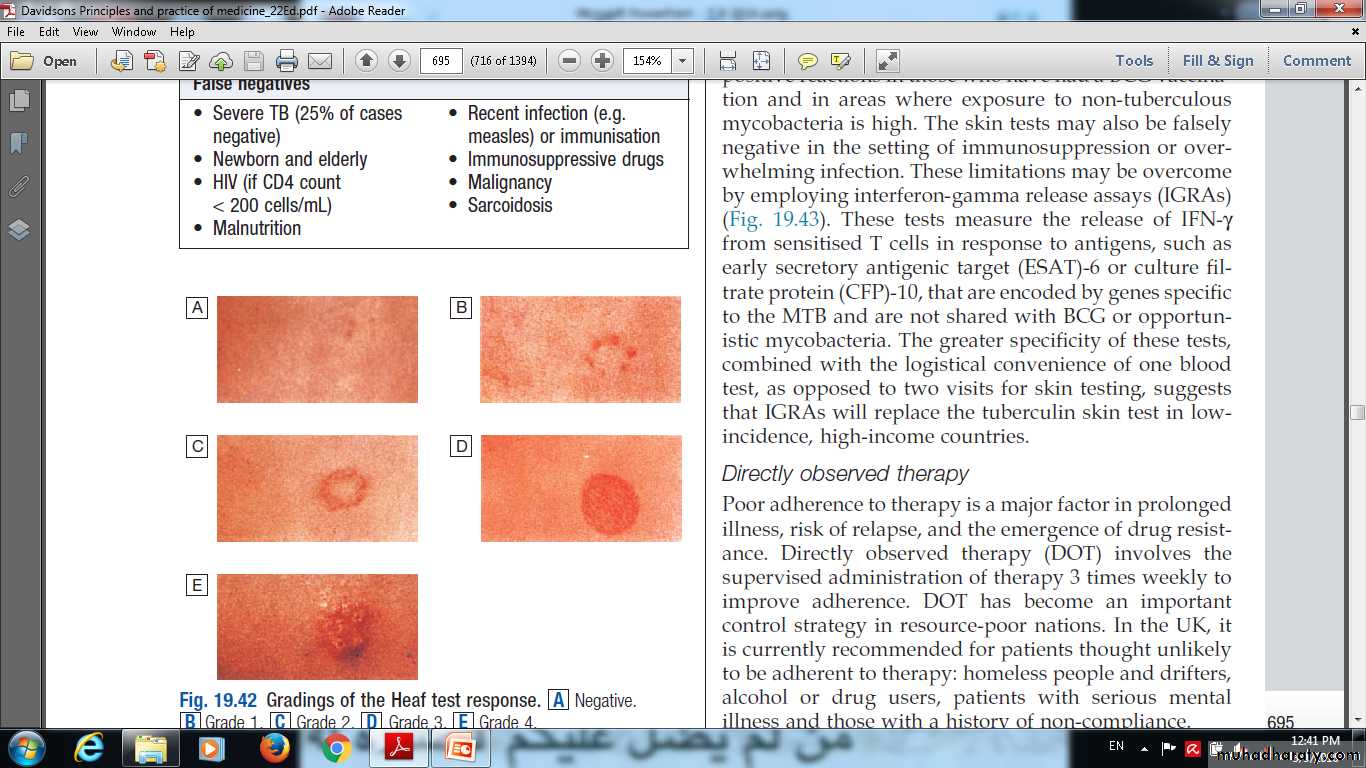
Skin testing in TB:
tests using purified protein derivative (PPD)Heaf test
Mantoux test
Results may be:
False negatives
false-positive
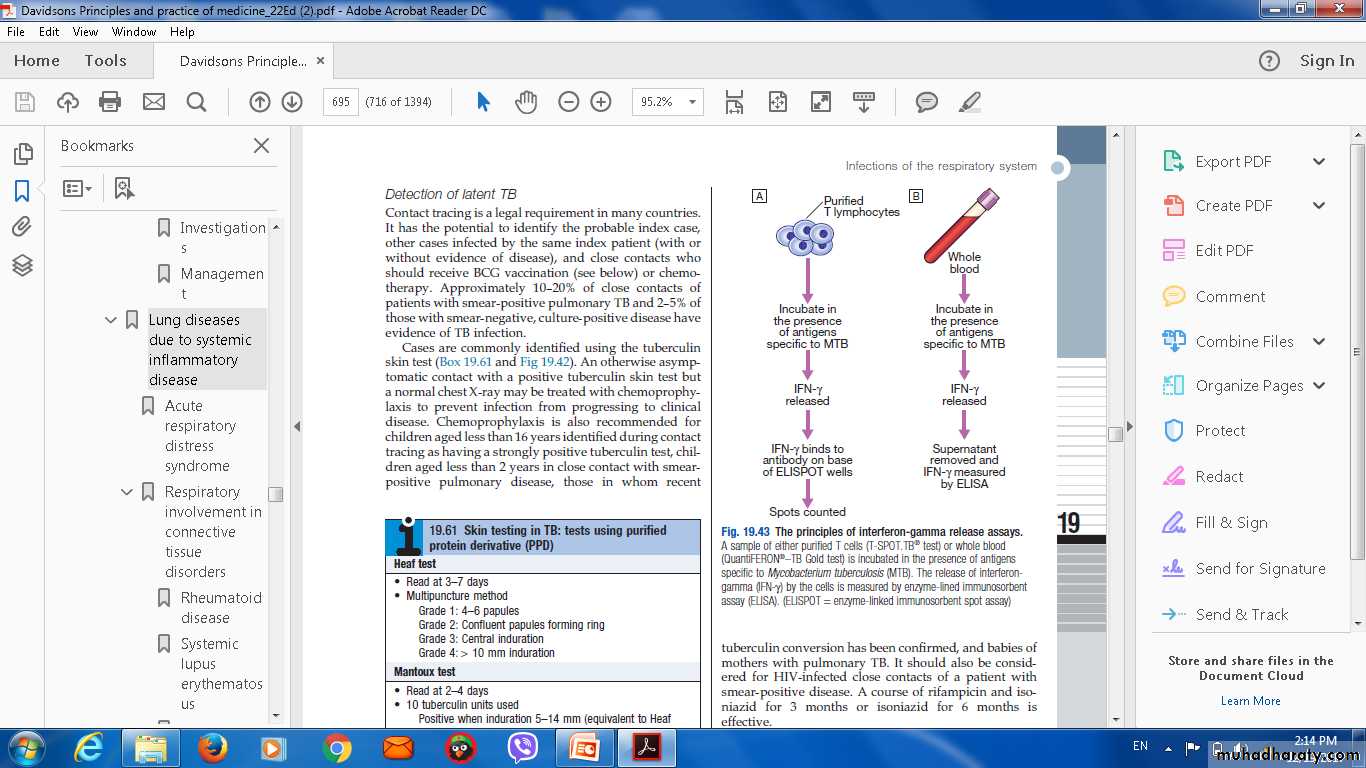
Gradings of the Heaf test response. A Negative.B Grade 1. C Grade 2. D Grade 3. E Grade 4.
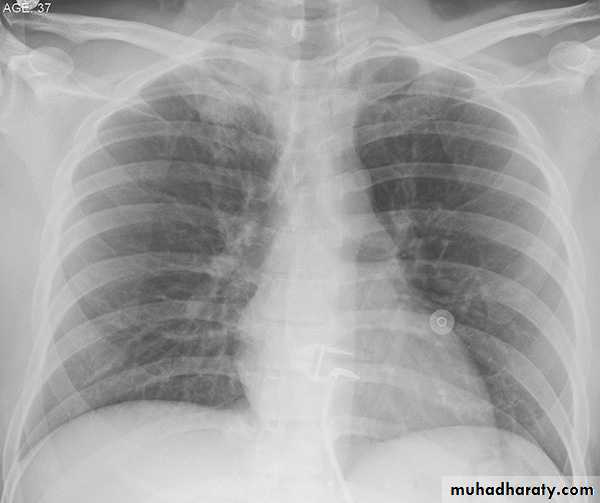
Chest Xray TB
Chest Xray
Chest Xray
Chest Xray
CT Chest pulmonary TB show cavitation
Other TEST FOR PULMONARY TB
Interferon-gamma release assays (IGRAs).culture filtrate protein (CFP)-10..
The principles of( IFN- Interferon-gamma release assays).
Chemotherapy
Indication:Patient who is smear-positive,
smear-negative but with typical chest X-ray changes.
Quadruple therapy has become standard
Fixed-dose tablets combining two or three drugs are generally favoured:(rifampicin, isoniazid and pyrazinamide) daily for 2 months(initial phase)
(rifampicin and isoniazid) daily for 4 months(continous phase) .
Duration of treatment
Six months of therapyall patients with new-onset, uncomplicated pulmonary disease.
9-12 months of therapy
HIV-positive
drug intolerance
12 months
Meningitis
Added to treatment Pyridoxine
pregnant women
malnourished patients.
Where drug resistance is not anticipated, patients can be assumed to be non-infectious after 2 weeks of appropriate therapy.
Admission to a hospital unit if :
Uncertainty about the diagnosis.
Intolerance of medication.
Questionable compliance.
adverse social conditions .
a significant risk of multidrug-resistant TB (MDR-TB: culture-positive after 2 months on treatment, or contact with known MDR-TB).
Recommendations in treatment
Do baseline liver function and regular monitoring.Adverse drug reactions occur in about 10% of patients.
Corticosteroids reduce inflammation
Surgery is still occasionally required but usually only after a full course of antituberculosis treatment.A positive sputum smear at 5 months defines treatment failure
Control and prevention1-detection of latent TB
2- treatment of active and latent TB.
Detection of latent TB
Contact tracing .
Probable index case.
Close contacts who should receive BCG vaccination or chemotherapy.
Rifampicin plus isoniazid for 3 months or isoniazid for 6 months is effective.
Vaccines
BCG (the Calmette-Guérin bacillus), a live attenuated vaccine,. BCG appears to be effective in preventing disseminated disease
Directly observed therapy (DOT)
Poor adherence to therapy is a major factor in:
prolonged infectious illnessrisk of relapse
the emergence of drug resistance.
Recommended
unlikely to be adherent to therapy
homeless,
alcohol
drug users
serious mental illness
non-compliance
TB and HIV/AIDS
It is recommended that all patients with TB should be counselled and tested for HIV disease.Mortality is high and TB is a leading cause of death in HIV patients.
Drug-resistant TB
defined by the presence of resistance to any first-line agent.
Multidrug-resistant (MDR) TB.
Extensively drug-resistant (XDR).
Diagnosis is challenging
Prognosis
Following successful completion of chemotherapy, cure should be anticipated in the majority of patients.A small risk of relapse.
• Thank u
QQIUZE