Osteomyelitis
5th stageDr.Kalid Ali Zayer
Osteomyelitis
Is an inflammation of the bone caused by an infecting organism.
Classification:
Depending on the duration of symptoms:
Acute pyogenic: are characterized by the formation of pus.
Subacute.
Chronic:
Chronic pyogenic infection: may follow on unresolved acute infection.
Chronic non-pyogenic infection: may result from invasion by organisms that produce a cellular reaction leading to granulomatous infection. Typically seen in tuberculosis.
Depending on the mechanism of infection:
Exogenous or haematogenous; less often contiguous.
General aspects of bone infection
Micro-organisms may reach the musculoskeletal tissues by:Direct introduction through the skin (a pinprick, an injection, a stab wound, a laceration, an open fracture or an operation).
Direct spread from a contiguous focus of infection.
Indirect spread via the blood stream from a distant site such as the nose or mouth, the respiratory tract, the bowel or the genitourinary tract.
Acute Haematogenous Osteomyelitis
Aetiology
It is the most common type of bone infection. It is mainly a disease of children. When adults are affected it is usually because their resistance is lowered.
The organisms reach the bone through the blood stream.
Trauma may determine the site of infection, possibly by causing a small haematoma or fluid collection in a bone, in patients with concurrent bacteraemia.
The causal organism:
Staphylococcus aureus is the most common microorganism in both adults and children (found in over 70% of cases), less often streptococcus (Streptococcus pyogenes).
In children 1-4 years of age, Haemophilus influenzae and Kingella kingae used to be a fairly common pathogen for osteomyelitis and septic arthritis.
Patients with sickle-cell disease are prone to infection by Salmonella typhi.
Unusual organisms like Escherichia coli, Pseudomonas aeruginosa, Proteus mirabilis and the anaerobic Bacteroides fragilis are more likely to be found in heroin addicts and as opportunistic pathogens in patients with compromised immune defense mechanisms.
Pathogenesis
In children, the infection usually starts in the vascular metaphysis of a long bone, most often in the proximal tibia or in the distal or proximal ends of the femur.In adults, haematogenous infection mostly affecting the vertebrae.
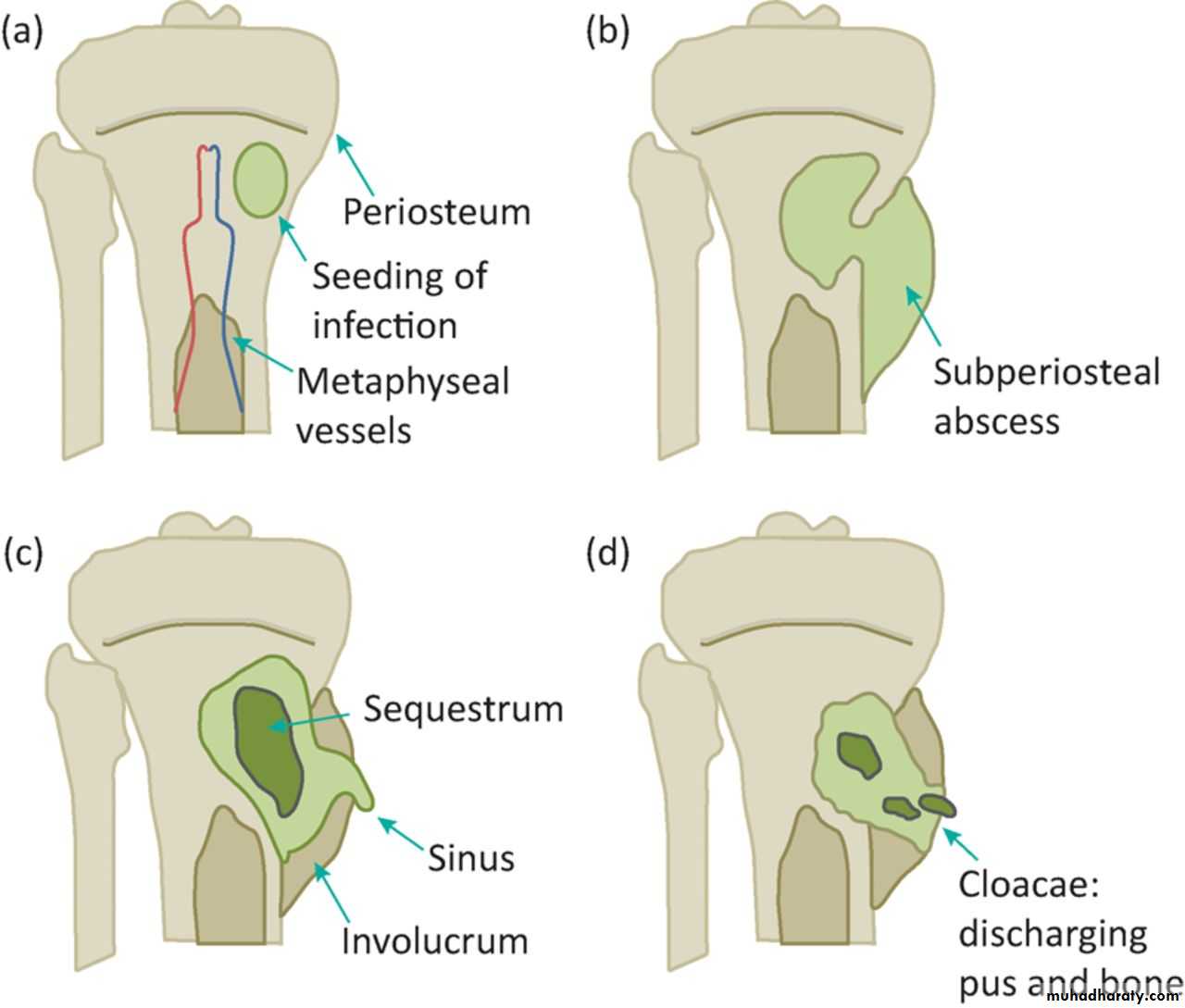
Five stages (The ‘classical’ picture is seen in children between 2 and 6 years):
Acute inflammation: ischemia and intense pain.Suppuration: 2nd or 3rd day, pus. (subperiosteal abscess).
Necrosis: a week, bone death, and Pieces of dead bone may separate (Sequestra) varying in size.
New bone formation: by the end of 2nd week, from stripped periosteum (involucrum), enclosing the sequestrum and infected tissue. If the infection persists, pus and tiny sequestrae may discharge through perforations (cloacae) in the involucrum and track by sinus(es) to the skin surface.
Resolution and healing or intractable chronicity.
Clinical features
Children (4-6) year old: severe pain, malaise and a fever. The child looks ill and feverish; the pulse rate over 100. The child refuses to move the limb (‘pseudoparalysis’), or to allow it to be handled or even touched. There is acute tenderness near one of the larger joints.
Infants and children under a year old: the constitutional symptoms are mild; the baby drowsy but irritable.
Adults: The commonest site is the thoracolumbar spine. There may be a history of some urological procedure followed by a mild fever and backache. Local tenderness is not very marked.
Very elderly: and in those with immune deficiency, systemic features are mild and the diagnosis is easily missed.
Diagnostic imaging
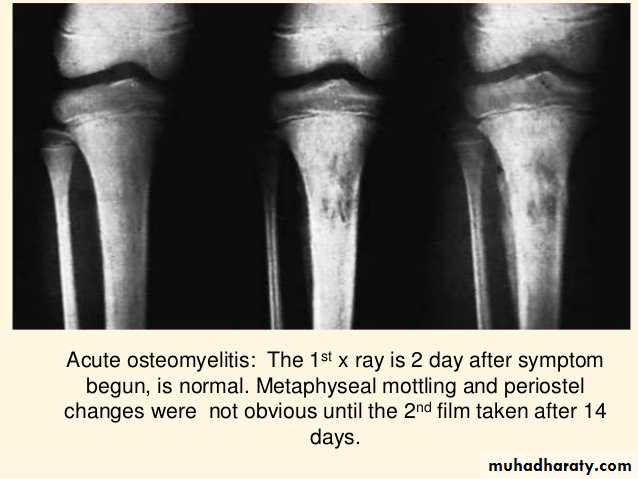
Plain X-ray: obvious by the end of 2nd week: diffuse rarefaction, then periosteal new bone formation, then squestrum, but treatment should not be delayed until x-ray changes appear.Ultrasonography: may detect a subperiosteal collection of fluid in the early stages of osteomyelitis.
Bone Scan: is a highly sensitive investigation, even in the very early stages.
MRI: It is extremely sensitive, even in the early phase of bone infection.
Laboratory investigations
Aspiration of pus or fluid from the metaphyseal subperiosteum for microbiological examination is the most certain way to confirm the clinical diagnosis.Blood cultures are positive in less than half of the cases.
The C-reactive protein (CRP) values are elevated within 12–24 hours and ESR within 24–48 hours after the onset of symptoms. WBC count rises.
Antistaphylococcal antibody titers may be raised.
Treatment
If osteomyelitis is suspected on clinical grounds, blood and fluid samples should be taken for laboratory investigations and then treatment started immediately without waiting for final confirmation of the diagnosis.
Four aspects:
Supportive treatment for pain and dehydration.
Splintage of the affected part.
Appropriate antimicrobial therapy: parentral: start empirical treatment as combination of flucloxacillin and fusidic acid or third generation cephalosporin like cefotaxime. Patients at risk of meticillin-resistant Staphylococcus aureus (MRSA) should be treated with intravenous vancomycin (or similar antibiotic) together with a third-generation cephalosporin.
Surgical drainage: indicated if the patient presented late or symptoms do not improve within 36 hours or there is pus.
Complications:
Septicemia or pyaemia.Suppurative arthritis.
Epiphyseal damage and altered bone growth.
Metastatic infection: may affects other bones, joints, brain, and lung.
Chronic osteomyelitis.
Subacute Haematogenous Osteomyelitis
This condition is no longer rare, and in some countries the incidence is equal to that of acute osteomyelitis.Its relative mildness is probably due to the organism being less virulent or the patient more resistant (or both).
It occurs in the metaphysis of long bones of the lower extremities of young adults, the distal femur and the proximal and distal tibia are the favorite sites.
The organism is almost always Staphylococcus aureus.
Brodie's abscess
There is a well defined cavity in cancellous bone containing seropurulent fluid, rarely pus. Pain is the predominant symptom.
X-ray: round or oval radiolucent ‘cavity’ 1–2 cm in diameter surrounded by zone of sclerosis, the rest of bone is normal. Treatment is surgery.
Chronic osteomyelitis
Chronic osteomyelitis is nearly always a sequel to acute osteomyelitis.Occasionally, is chronic from the beginning.
Nowadays, the commonest of all predisposing factors is local trauma, such as an open fracture or a prolonged bone operation, especially if this involves the use of a foreign implant.
Pathogenesis:
Staphylococcus is the usual causative organism.Streptococci, pneumococci, typhoid bacilli, or others.
The infection is often mixed.
In the presence of foreign implants, Staphylococcus epidermidis is the commonest of all.
Pathology:
The hallmark is infected dead bone within a compromised soft tissue envelope. Bone is destroyed and cavities containing pus and pieces of dead bone (Squestra) surrounded by thick sclerotic bone (Involucrum). Perforation(s) (Cloacae) in the involucrum tract to the skin (sinus). Systemic antibiotics essentially ineffective.Why Chronic osteomyelitis?
Scar formation.Presence of dead and dying bone around the focus of infection.
Poor penetration of new blood vessels.
Presence of non-collapsing cavities in which microbes can thrive.
Bacteria covered in a protein–polysaccharide slime (glycocalyx) that protects them from both the host defenses and antibiotics especially when there is metal.
There is also evidence that bacteria can survive inside osteoblasts and osteocytes and be released when the cells die.
Clinical features:
Acute flares: pain, pyrexia, redness and tenderness have recurred.Discharging sinus and excoriation of the surrounding skin. In longstanding cases the tissues are thickened and often puckered or folded inwards where a scar or sinus adheres to the underlying bone. OR
Pathological fracture.
Imaging:
Plain x-ray: the classical appearance is called honeycombed appearance: bone resorption either as a patchy loss of density or as frank excavation around an implant with thickening and sclerosis of the surrounding bone.
CT & MRI: show the extent of bone destruction and hidden abscesses and sequestra.
Sinogram: may help to localize the site of infection
Treatment:
Despite advances in antibiotic therapy, chronic osteomyelitis seldom eradicated by antibiotics alone. Yet bactericidal drugs are important (a) to suppress the infection and prevent its spread to healthy bone and (b) to control acute flares.
Acute flares often subside with rest and antibiotics.
Abscess must be drained.
Persistent discharging sinuses need extensive surgery. (Bone graft, Muscle flap).
Pathological fracture need fixation.
Amputation: dangerous or damn nuisance limb.
Complications:
Pathological fracture.Bone deformity.
Squemous cell carcinoma in chronic skin sinus.
The limb some time become chronically painful and useless (damn nuisance limb).
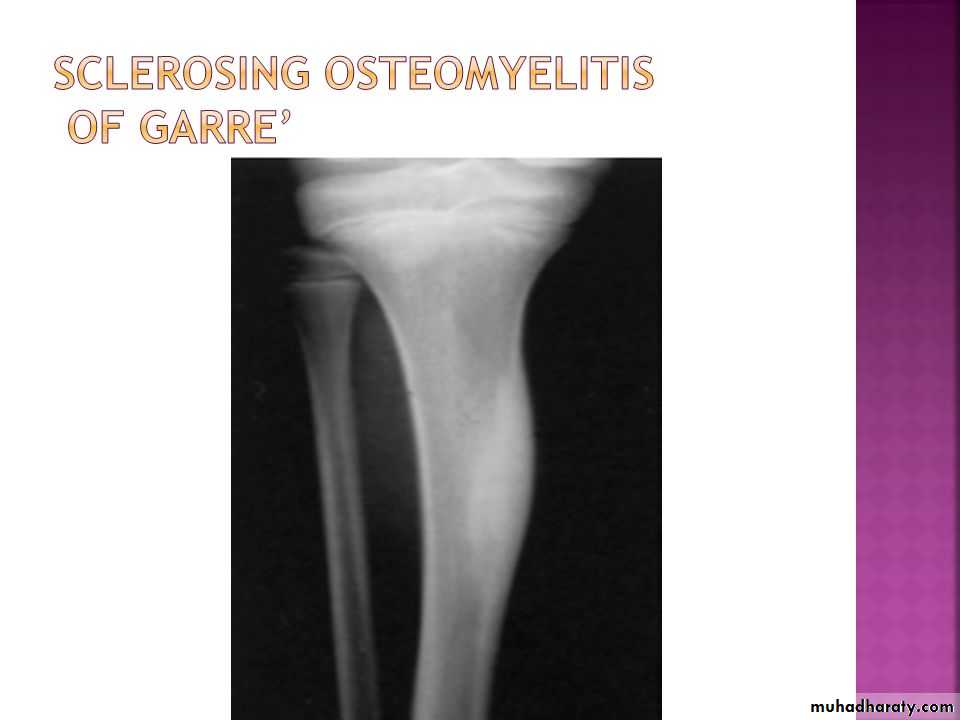
Chronic osteomyelitis of Garre:
Is nonsuppurative osteomyelitis which is characterized by marked sclerosis and cortical thickening. but‼ there is no abscess, only a diffuse enlargement of the bone at the affected site – usually the diaphysis of one of the tubular bones or the mandible.Insidious onset, moderate, intermittent pain of long duration.
X-rays; increased bone density and cortical thickening; in some cases the marrow cavity is completely obliterated. There is no abscess cavity.
Treatment by surgery.