
Disorders of the urinary bladder

Either congenital or acquired.
The congenital anomalies include.
Ectopia vesica (bladder exstrophy).
Exstrophy of the urinary bladder is a complete
ventral defect of the urogenital sinus & the
overlying skeletal system.

Other congenital anomalies are frequently
associated with it. The lower central abdomen is
occupied by the inner surface of the posterior
wall of the bladder, whose mucosal edges are
fused with skin.
Urine spurt onto the abdominal wall from the
ureteral orifices.

The rami of the pubic bone are widely separated.
The pelvic ring thus lack rigidity, the femurs are
rotated externally, & the child waddle like duck.
Since the rectal muscles insert on the rami, they are
widely separated from each other inferiorly.
A hernia made up of exstrophic bladder &
surrounding skin, is therefore present.
Epispadias almost always accompanies it.

Many untreated exstrophic bladder reveal fibrosis,
derangement of the muscularis mucosa, & chronic
infection.
These changes tend to defeat effort to form bladder
of proper capacity.
Adenocarcinoma are the most common type of
carcinoma developing in the exstrophic bladder.

Renal infection is common, & hydronephrosis caused
by ureterovesical obstruction may be found on the
urography.
These films also reveal separation of the pubic bone.
Treatment. Usually accomplished by surgical repair
as early as 1st week.




Persistent urachus.
Embryologically, the allantois connects the
urogenital sinus with the umbilicus.
Normally the allantois is obliterated & is represented
by a fibrous band called urachus extending from the
dome of the bladder to the navel.
Urachal formation is directly related to bladder
descent.
Lack of descent is more commonly associated with
patent urachus than with bladder outlet obstruction.

Incomplete obliteration is some time occurs,
-if obliteration is complete except at the superior
end, a draining umbilicus sinus may be noted.
If it become infected the drainage will be purulent.
-If the inferior end remains open, it will
communicate with the bladder, but this does not
usually produce symptoms.

Rarely the entire tract remains patent, in which
case urine drains constantly from the umbilicus.
This is apt to become obvious within few days of
birth
-if only the ends of the urachus seal off, cyst of
that body may form & may become quite large,
presenting a low midline mass.
If the cyst become infected, signs of general &
local abscess will develop
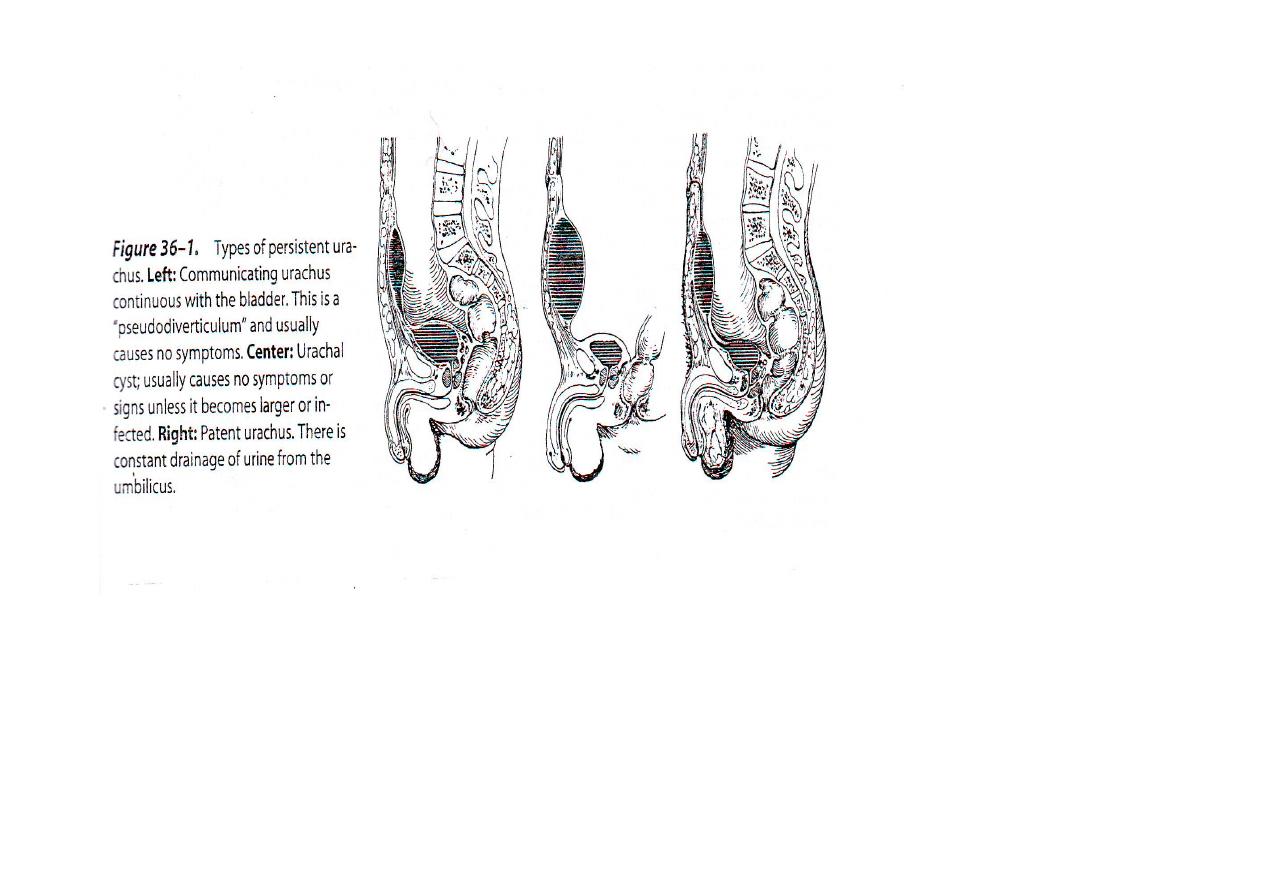

-Adenocarcinoma may occur in a urachal cyst,
particularly at its vesical extremity. & tend to
invade the tissues beneath the anterior abdominal
wall. It may be seen cystoscopically.
-Stones may be seen in a cyst of the urachus.
These can be identified on a plain x-ray film.

Treatment.
Consist of excision of the urachus, which lies on the
peritoneal surface with bladder cuff
If adenocarcinoma is present radical resection is
required.
Unless other serious congenital anomalies are
present, the prognosis is good.
The complication of adenocarcinoma offers a
poor prognosis.

Acquired diseases of the bladder
Interstitial cystitis (Hunner`s ulcer).
Is primarily disease of middle aged women.
It is characterized by fibrosis of vesical wall, with
consequent loss of bladder capacity.
Frequency, urgency, & pelvic pain with bladder
distension are the principle symptoms.
●
A syndrome of mystery in urology
●
A diagnosis of exclusion
●
Triad diagnostic characteristics –
Suprapubic pain at full bladder and relieved
after voiding, with severe frequency and
nocturia
Sterile urine
Characteristic cystoscopic findings
Interstitial cystitis

Pathogenesis.
Infection does not appear to be the cause of fibrosis
of the bladder wall, because the urine is usually
normal.
The cause still unknown, but the primary change is
fibrosis in the deeper layer of the bladder.
The capacity of the organ is decreased, sometimes
markedly.

The mucosa is thinned, especially where mobility is
greatest as the bladder fill & empties (ie, over the
dome), and small ulcers or cracks, in the mucus
membrane may be seen in this area.
In the most sever cases the normal mechanism of
the ureterovesical junctions is destroyed, leading to
vesicoureteral efflux.
Hydroureteronephrosis & pyelonephritis may ensue.

Clinical findings.
Interstitial cystitis should be considered when
middle aged woman with clear urine complains of
sever frequency & nocturia & suprapubic pain on
vesical distention.
There is long history of slowly progressive
frequency & nocturia, both of which may be sever.
The history does not suggest infection (burning on
urination, cloudy urine).

Suprapubic pain is usually marked when bladder is
full.
Pain may also be experienced in the urethra or
perineum, its relieved on voiding.
Gross hematuria occasionally noted, usually when
urination postponed (ie, following vesical
overdistension).

The patient is tense & anxious, whether its
primary or secondary to the prolonged symptoms
is not clear.
A history of allergy may be obtained.

Physical examination is usually normal.
Some tenderness in the suprapubic area may be
noted.
Laboratory finding.
The urine is almost always free of infection,
microscopic hematuria may be noted.
Renal function tests are normal unless complicated
by reflux or obstruction.

x-ray finding.
Excretory urograms are usually normal unless
reflux has occurred, in which case
hydronephrosis is found.
The accompanying cystogram reveals a bladder
of small capacity, reflux into dilated upper tract
may be noted on cystography.
Instrumental examination.
Cystoscopy is usually diagnostic.
The vesical capacity as low as 60 ml.
the bladder lining may look fairly normal. However,
if the second distention is done, punctuate
hemorrhagic areas may appear over the most
distensible portion of the wall.
With further distention congestion, edematous
reaction, petechial hemorrhage ( glomerulation) are
common finding.
Differential diagnosis.
-Tuberculosis of the bladder.
-Schistosomiasis.
-Nonspecific vesical infection

Treatment.
There is no definitive treatment for interstitial
cystitis.
The therapy employed affords partial relief, but it
may be completely ineffective.
General or vesical sedative may be prescribed but
seldom afford relief.
Hydraulic overdistension or instillation of 50 ml of
50% dimethyl sulfoxide (DMSO) into the bladder
every 2 weeks for 15 min.
-Cortisone acetate 100 mg, or prednisone 10-20
mg/d, in divided doses for 21days, followed by
decreasing amount for additional 21 days, has also
been found effective.
-Antihistamine may also afford some relief.
-Heparin sodium (long acting) 20,000 IU
intravenously daily also blocks the action of
histamine.
-Surgical management in a form of iliocystoplasty
may be done to augment the vesical capacity.

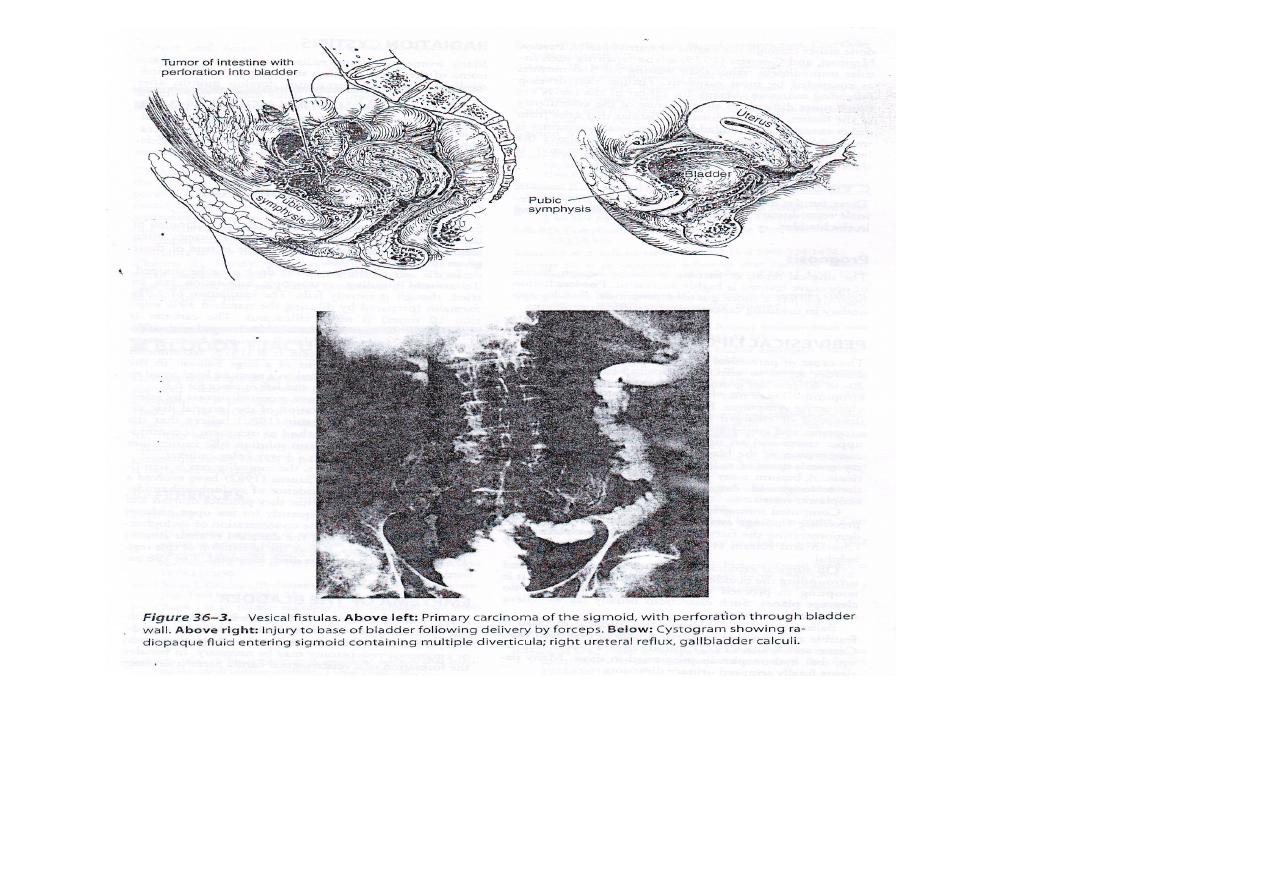
Vesical fistulas
Vesical fistulas are common.
The bladder may communicating with
the skin,
intestinal tract, or
female reproductive organs.
The primary disease is usually not urologic.

The causes are as follows:
1- primary intestinal disease diverticulitis (50-
60%), cancer of the colon (20-25%),& crohn
disease (10%)
2- primary gynecologic disease, pressure
necrosis following difficult labor, advanced
cancer of the cervix.
3- treatment for gynecologic disease following
hysterectomy, low cesarean section, or
radiotherapyfor tumor.
4- trauma.

Clinical finding
A –vesicointestinal fistula.
Symptoms include vesical irritability, the passage of
feces & gas through the urethra, & usually a change
in bowel habit (eg, constipation, abdominal distention,
& diarrhea) caused by the primary intestinal disease.

Signs of bowel obstruction may be elicited,
abdominal tenderness may be found if the cause is
inflammatory.
The urine is always infected.
A barium enema, upper gastrointestinal series, or
sigmoidoscopic examination may demonstrate the
communication.
Following a barium enema, centrifuged urine on
an x-ray cassette & an exposure made.
The presence of radiopaque barium establish the
diagnosis of vesicocolonic fistula.

Cystogram may reveal gas in the bladder or reflux
of the radiopaque material into the bowel.
Cystoscopic examination, the most useful
diagnostic procedure, show sever localized
inflammatory
reaction from which bowel content may exude.
Catheterization of the fistulous tract may be
feasible;
the instillation of radiopaque fluid often establish
the diagnosis.

B –vesicovaginal fistula.
This relatively common fistula is secondary to
obstetric, surgical, or radiation injury or to the
invasive cancer of the cervix.
The constant leakage of urine is most distressing
to the patient.
Pelvic examination usually reveals the fistulous
opening, which also can be visualized with the
cystoscope.
It may be possible to pass ureteric catheter
through the fistula into the vagina.

Vaginography often successfully shows
ureterovaginal, vesicovaginal, & rectovaginal
fistulas.
A 30-ml foley catheter is inserted into the vagina,
& the balloon is distended.
A radiopaque solution is instilled & appropriate
x-rays are taken.
Biopsy of the edges of the fistula may show
carcinoma.

Differential diagnosis.
Its necessary to differentiate ureterovaginal from
vesicovaginal fistula,
phenazopyridine (pyridium) is given by mouth to
color the urine orange.
One hour later, 3 cotton pledgets are inserted into
the vagina, & methylene blue solution is instilled
into the bladder.
The patient should then walk around, after which
the pledgets are examined.

If the proximal cotton ball is wet or stained orange,
the fistula is ureterovaginal.
If the deep cotton pledget contain blue fluid, the
diagnosis is vesicovaginal fistula.
If only the distal pledget is blue, the patient
probably has urinary incontinence.

Treatment.
A –vesicointestinal fistula.
If the lesion is in the rectosigmoid, treatment
consist of proximal colostomy.
-When the inflammatory reaction has subside, the
involved bowel may be resected, with closure of
the opening of the bladder.
-The colostomy can be closed later.
Small bowel or appendiceal vesical fistula require
bowel or appendiceal resection & closure of the
vesical defect.

B –vesicovaginal fistula.
Tiny fistulous opening may become sealed
following the introduction of an electrode into the
fistula.
As the electrode is withdrawn, the fistula is
coagulated with electrosurgical unit to destroy the
epithelium of the tract.
An indwelling catheter should be left in place for 2
weeks or more.

Large fistulas secondary to obstetric or surgical
injuries respond readily to surgical repair, which
may be done through the vagina or transvesically
after 3-6 months.
Fistulas develop secondary to radiation therapy, or
direct extension by cancer are difficult to close.

Non infectious hemorrhagic cystitis
Some patients following radiotherapy for
carcinoma of cervix or bladder, are prone to
intermittent often serious vesical hemorrhage.
The same is true of those given cyclophosphamide.
In the case of later the drug must be stopped.

To control bleeding, Cystoscopic fulguration can
be tried, though it usually fails.
The instillation of 3.9% formalin ( preparing by
diluting the standard 39% solution 10 times, ie
50 ml for 500ml normal saline) is more
efficacious.
The catheter is clamped for 30 min &
the bladder lavaged with 10% alcohol.
A second or third instillation may be necessary
on subsequent days.

Other methods like inflation of balloon inside the
bladder for 6 hr. or
• embolization of internal iliac artery,
• continuous irrigation with 1% alum solution (the
ammonium or potassium salt) through 3-ways
foley catheter.

To reduce the incidence of cyclophosphamide
induced hemorrhagic cystitis, they produce diuresis
& patient void frequently (or use open catheter
drainage).
This reduce the concentration of cyclophosphamide
metabolites & the duration of their contact with
bladder mucosa.
Despite these measures the mortality rate is
significant.

Normal intravesical pressure at the beginning of micturition
is about
a.
50 cm of water
b.
40 cm of water
c.
30 cm of water
d.
5 cm of water
The antibiotic of choice in interstitial cystitis is
e.
Doxycycline
f.
Gentamicine
g.
Ciprofloxacine
h.
None

Arterial supply to the bladder includes
a.
The superior vesical artery
b.
The obturator artery
c.
The uterine artery
d.
All of the above
Pneumaturia may be due to all of the following except
e.
Diverticulitis
f.
Colon cancer
g.
Recent urinary tract instrumentation
h.
Ectopic ureter

The first event to occur with normal micturition is
a.
Relaxation of the bladder neck
b.
Relaxation of the external striated sphincter
c.
Contraction of the bladder body
d.
Contraction of the trigon
A woman who complain of unconscious leakage may have all
the following except
e.
Vesicovaginal fistula
f.
Urge incontinence
g.
Overflow incontinence
h.
Intrinsic sphincteric deficiency
