• Lecture : Brucella
Dr. Faten Naeem AbbasBacteria of Brucella cause disease primarily in domestic, feral and some wild animals and most are also pathogenic for humans.
Brucellosis is thought to have been identified in the late Roman date, named because of its similarity to the organism Brucellae (later called Brucella) from carbonized cheese
Brucellosis has been associated with military campaigns, predominantly in the Mediterranean region.
The disease was first expounded by Sir David Bruce (1855-1931) British Army physician and microbiologist who discovered Micrococcus melitensis 1887, while working in Malta; hence the name ‘Malta fever’ is occasionally used for typical fever conditions caused by Brucella.
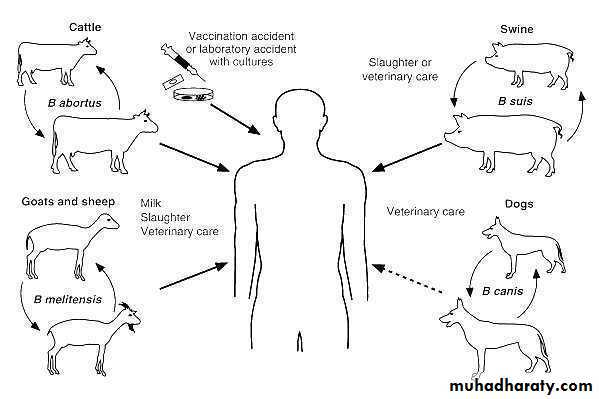
Brucellosis is a zoonotic infection is transmitted to humans as a result of direct contact with an infected animal skin and mucus membrane or indirect contact by inhalation, or ingestion of unpasteurized dairy products.
The disease is an old one that has been known by various names, including Mediterranean fever, Malta fever, intermittent typhoid, rock fever of Gibraltar, and more commonly, undulant fever.
The bacteria infect reproductive tissues, lymph nodes, and the spleen, and therefore cause inflammation, edema, and necrosis. In pregnant animals it causes placental lesions and increases the risks of abortion. Brucellosis gains public health importance when the bacteria are transmitted to human via unpasteurized milk, meat, and animal byproducts, from infected animals.
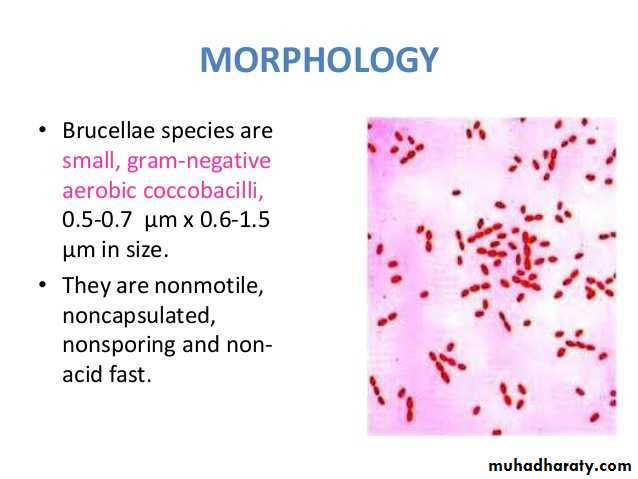
Morphology and Structure:
Brucellae are Gram-negative coccobacilli (short rods) measuring about 0.6 to 1.5 μm by 0.5-0.7 μm.They are non-sporing and lack capsules or flagella and, therefore, are non-motile.
The outer cell membrane closely resembles that of other Gram-negative bacilli with a dominant lipopolysaccharide (LPS) component and three main groups of proteins.
The metabolism of the brucellae is mainly oxidative and they show little action on carbohydrates in conventional media.
They are aerobes but some species require an atmosphere with added CO2(5-10 percent).
Multiplication is slow at the optimum temperature of 37°C and enriched medium is needed to support suitable growth.
• Brucella colonies become visible on suitable solid media in 2-3 days. The colonies of smooth strains are small, round and convex but separation, with loss of the O chains of the LPS, occurs readily to form rough or mucoid variants. These latter forms are natural in B canis and B ovis as the LPS of these lack O chains.
• Non haemolytic
• strongly positive to urease
• Not grow on MacConkey or EMB agar
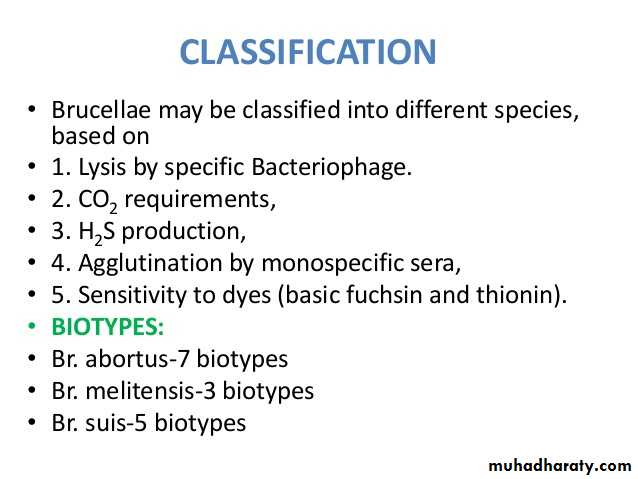
Classification:
Although six species of Brucella are known, only four are important to humans:B. melitensis (goats, sheep and camels).
B. abortus (Cows, camels, cattle, buffalo).
B. suis (pigs).
B. canis (dogs).
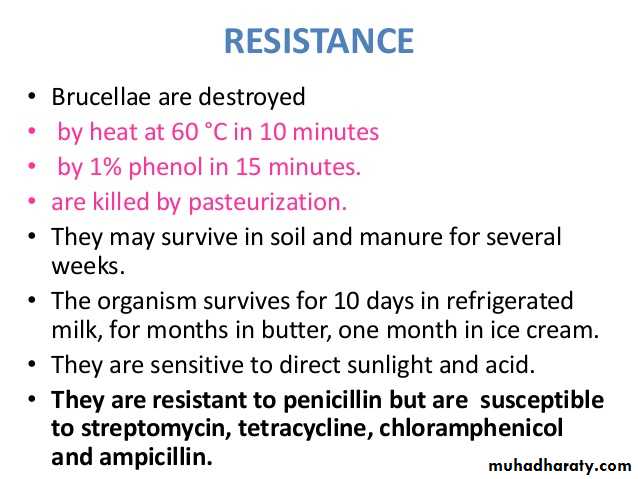
Sensitive to sunlight, ionizing radiation.
killed by boiling and pasteurization.Resistant to freezing and drying, facilitating airborne transmission to the respiratory tract and conjunctiva.
Survive up to 2 months in soft cheese.
Virulence factors
1-adhesins used for adhesion of brucella by epithelial cells2- LPS which include lipid A3-lipoprotein4- type IV secretion system (vir B and periplasmic cyclic beta, 1,2 glucans)Pathogenesis:
Brucella organisms, which are small aerobic intracellular coccobacilli, localize in the reproductive organs of host animals, causing abortions and sterility. They are shed in large numbers in the animal’s urine, milk, placental fluid, and other fluids. Humans are accidental hosts, but brucellosis continues to be a major public health concern worldwide and is the most common zoonotic infection. That characterized by an acute bacteremia phase followed by a chronic stage that may extend over many years and may involve many tissues.The common routes of infection in humans are the intestinal tract (ingestion of infected milk), mucous membranes (droplets), and skin (contact with infected tissues of animals). The organisms progress from the portal of entry via lymphatic channels and regional lymph nodes to the thoracic duct and the bloodstream which distributes them to the parenchyma organs. Granulomatous nodules that may develop into abscesses form in lymphatic tissue, liver, spleen, bone marrow, and other parts of the reticuloendothelial system.
Mechanism of pathogenesis
Skin , contaminated milk and cheese, Aerosols to the mucosa of nose, mouth & conjunctiva))↓
Local multiplication
Slight ulceration of mucosa, PMN phagocytize but Brucella multiply in them
↓
Lymphatic system (local lymph nodes)
↓
Reticulo-endothelial system
(Liver, spleen, and bone marrow)
(chronic inflammation (granulomas → abscesses
↓
Septicemia
↓
Generalized infections
(Meningitis, L-forms in bone marrow)
Clinical Picture of Brucellosis in Cattle
Brucellosis is a widespread reproductive disease, commonly causing abortion, death of young ones, stillbirth, retained placenta or birth of weak calves, delayed calving, male infertility, and marked reduction in milk yield
In animals, brucellosis symptoms can be varied from severe acute to sub-acute or chronic, depending upon the organ of infection and the type of animal. When a pregnant animal is infected by Brucella, a visible swelling of the mammary gland to the navel region and bleeding from the vagina is not uncommon, even if the cow does not abort. The enlarged udder size (appearance of the 9th month of a pregnant cow) could be used as an indication for the high stage of the disease, where animals shed bacteria in urine, milk, and vaginal discharges.
Human Brucellosis:
The usual incubation period of one to four weeks can be extended up to several monthsFever is one of the most common symptoms
Brucellosis also increases the risk of spontaneous abortion, premature delivery, miscarriage, and intrauterine infection with fetal death in humans as well,
In humans, brucellosis is not confined to the reproductive system, but is also known to cause neurobrucellosis
The disease may be
• Asymptomatic.• Acute (< 2 months)
• Sub acute (2-12 months)
• Chronic (> 1 year) incapacitating disease with severe complications.
Diagnosis of Brucellosis
Tools for diagnosis of brucellosis include culture, serology, and polymerase chain reaction (PCR) .• Culture: Definitive diagnosis depends on the isolation of brucellae from blood, CSF, BM, or joint fluid or from a tissue aspirate or biopsy sample, usually successful in 50–70%.
• Blood cultures are positive in 75–80% for melitensis and 50% of those caused by B. abortus.
• Bone marrow culture should not be used routinely but may increase the diagnostic yield, particularly if antibiotics have been given before specimens are taken.
• CSF culture in neurobrucellosis is positive in about 30%.The laboratory should be alerted to a suspected diagnosis of brucellosis.
Serology : May also aid diagnosis.
Serum agglutination (standard tube agglutination (SAT)ELISA (enzyme-linked immunosorbent assay)
Rose Bengal agglutination
Coombs test
2-mercaptoethanol agglutination (2-ME)
Polymerase chain reaction (PCR) .
• The peripheral blood–based polymerase chain reaction (PCR) has enormous potential to detect bacteremia, to predict relapse, and to exclude "chronic brucellosis." PCR is probably more sensitive and is certainly quicker than blood culture, and it does not carry the attendant biohazard risk posed by culture.Treatment:
Though the complex nature of brucellosis makes it harder to treat, long-term treatment with an antibiotic is thought to be beneficial. In most cases, antibiotics in combination are found to be more effective against the infection; however, the state of the disease still does not lose its importance.
The antimicrobials most commonly used include doxycycline (Vibramycin), streptomycin, rifampin (Rifadin), gentamicin (Garamycin), and trimethoprim-sulfa methoxazole (Bactrim, Septra).
The combination of antibiotics used will vary based on disease severity, age and pregnancy.