Complements
Nov/ 22/ 2021Dr. Minen Al-Kafajy
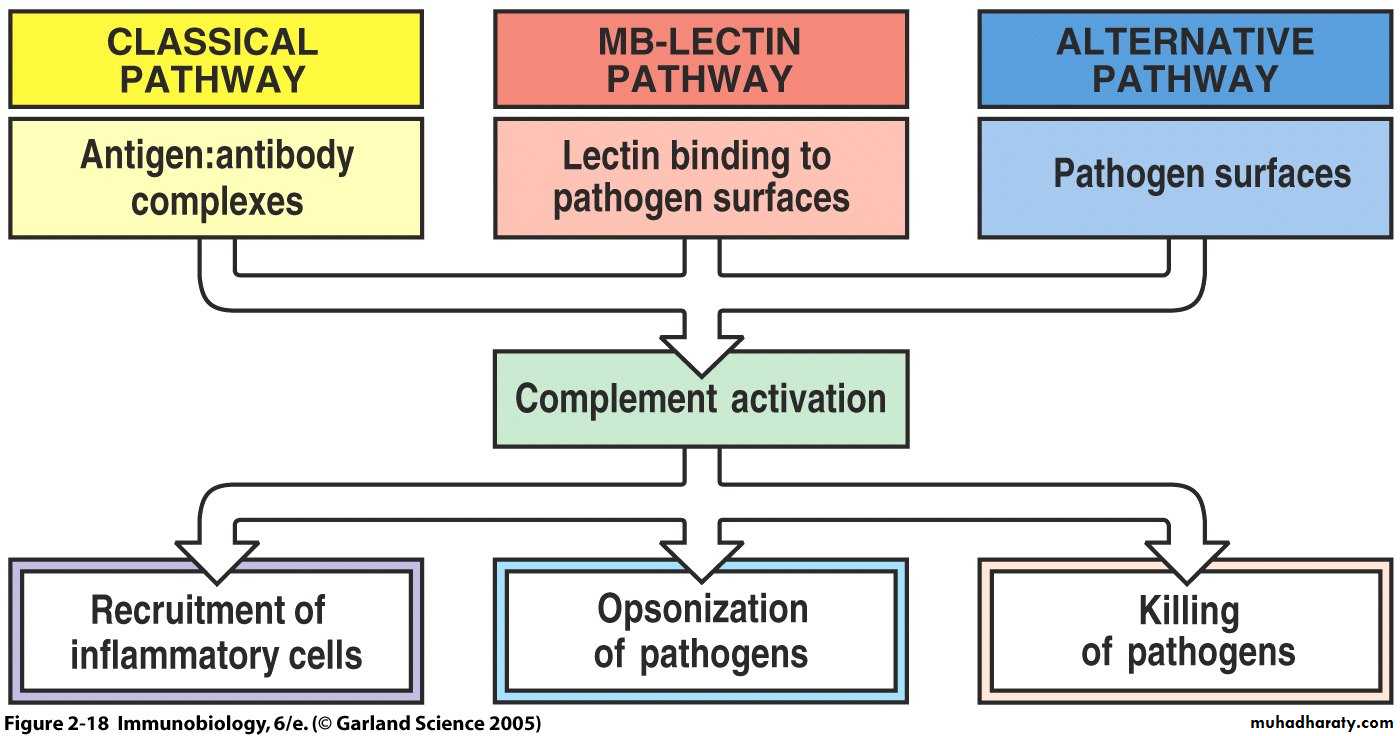
Complement
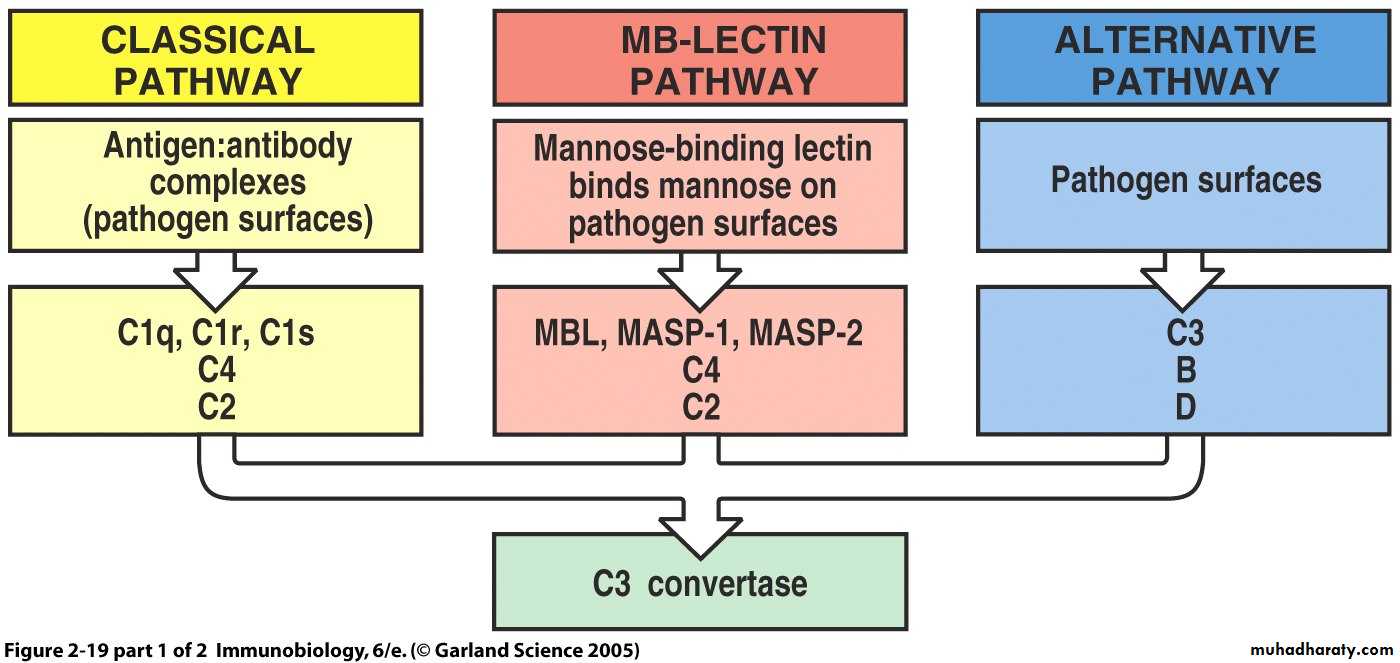
was discovered by Jules Bordet as a heat-labile component of normal plasma that causes the opsonisation and killing of bacteria. The complement system refers to a series of >30 proteins, circulating in the blood and tissue fluids. Most of the proteins are normally inactive, but in response to the recognition of molecular components of microorganisms they become sequentially activated in an enzyme cascade – the activation of one protein enzymatically cleaves and activates the next protein in the cascade.Complement can be activated via three different pathways (Figure 1), which can each cause the activation of C3, cleaving it into a large fragment, C3b, that acts as an opsonin, and a small fragment C3a (anaphylatoxin) that promotes inflammation. Activated C3 can trigger the lytic pathway, which can damage the plasma membranes of cells and some bacteria. C5a, produced by this process, attracts macrophages and neutrophils and also activates mast cells.
Overview of Complement
Classical PathwayAlternative Pathway
Lectin PathwayAntibody binds to specific
antigen on pathogen surfaceMannose-binding protein
binds pathogen surface
Pathogen surface creates
environment conducive tocomplement activation
Complement Activation
Formation of C3 and C5 convertasesMembrane Attack Pathway
Cytolysis of some pathogensOpsonization & phagocytosis
of some pathogensInflammatory response
Clearance ofImmune complexes
Clearance of
Apoptotic Cells
Classical Pathway
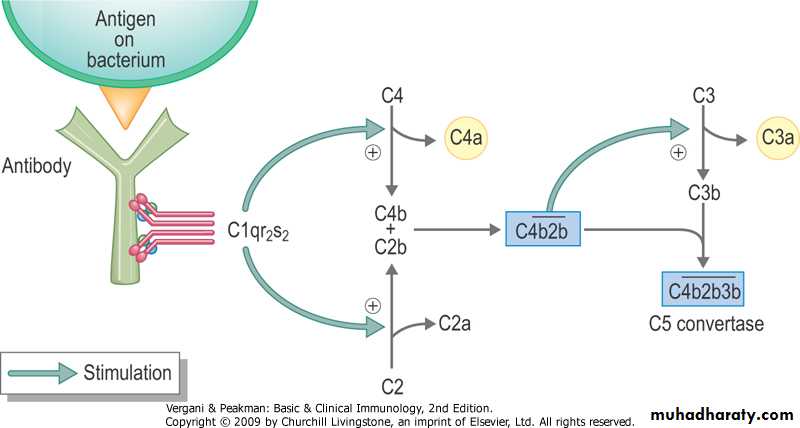
This pathway involves complement components C1, C2 and C4. The pathway is triggered by antibody-antigen complexes binding to C1, which itself has three subcomponents C1q, C1r and C1s. The pathway forms a C3 convertase, C4b2a, which splits C3 into two fragments; the large fragment, C3b, can covalently attach to the surface of microbial pathogens and opsonise them; the small fragment, C3a, activates mast cells, causing the release of vasoactive mediators such as histamine.The Classical Pathway
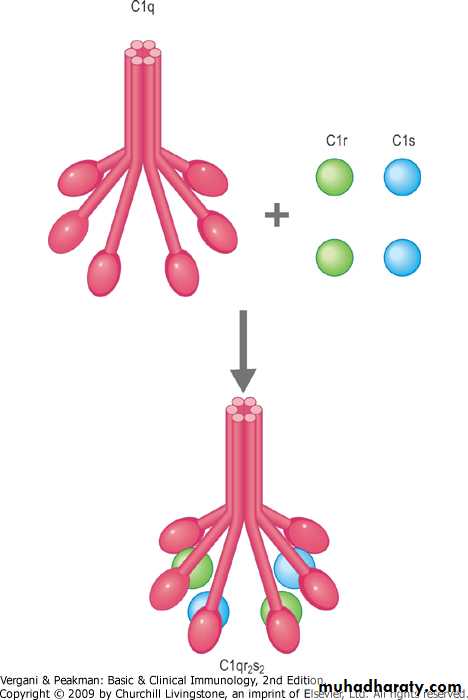
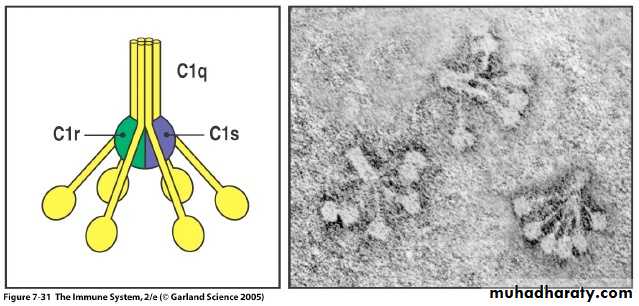
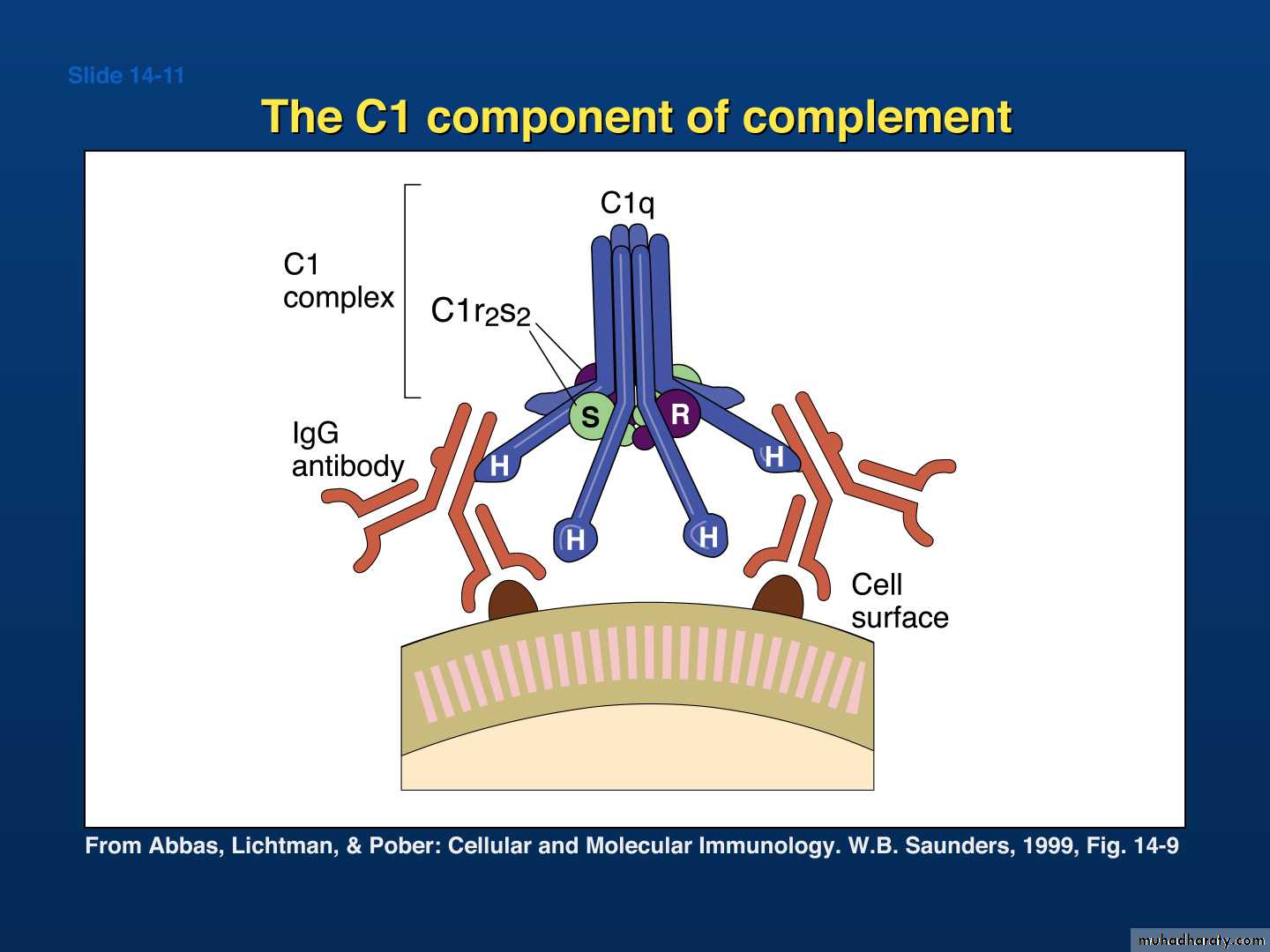
Activation of C1:C1 consists of C1q , C1r, and C1s
Subunits are held together by Calcium ions
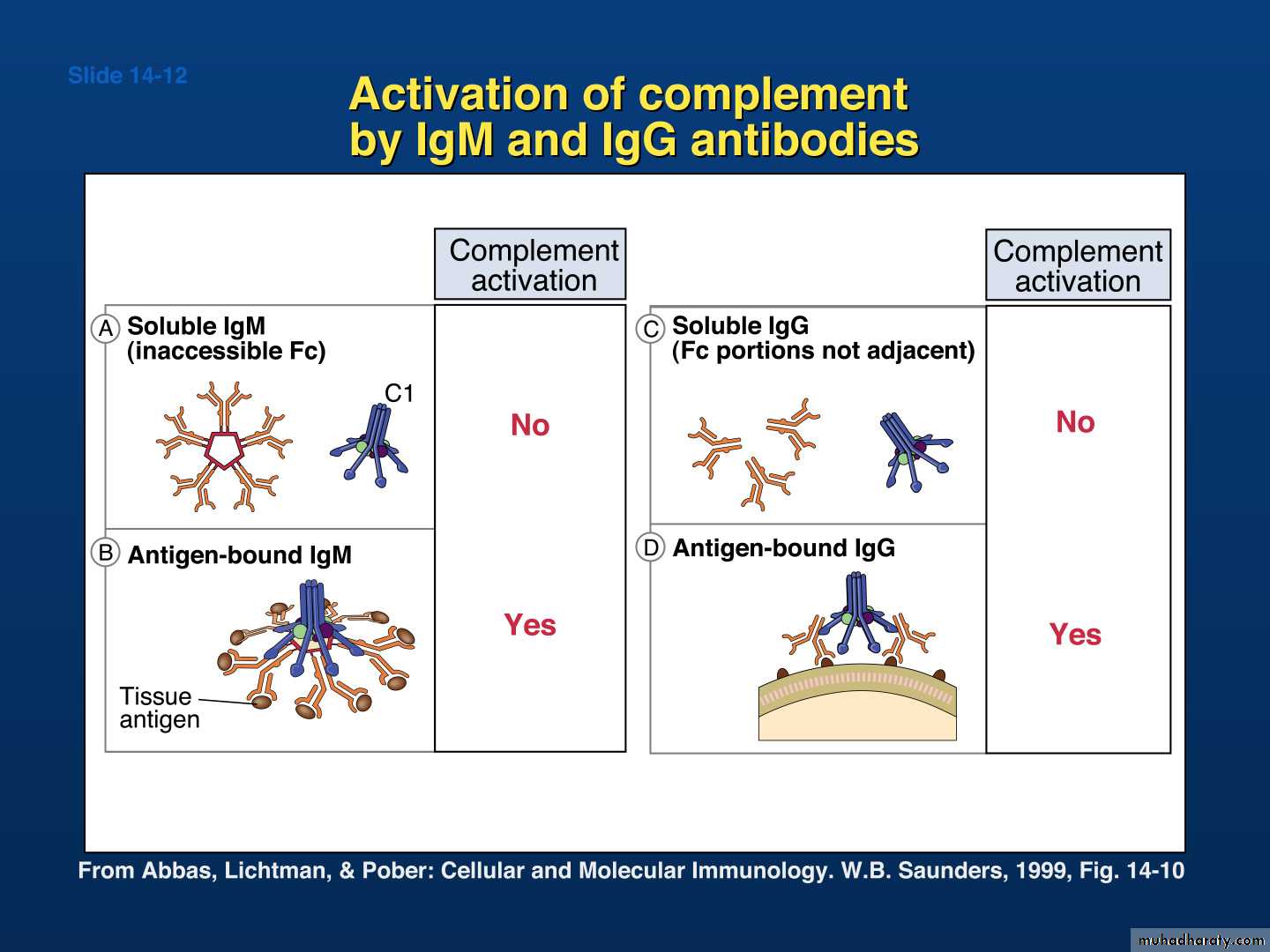
C1q is a polymer of 6 identical unitsC1q activation requires binding to a c1q- specific receptor on the FC region of at least 2 adjacent molecules of IgG or a single molecule of IgM, a reaction that requires Calcium ions
Molecular structure of C1
IgA and IgE cannot activate complement
The Classical PathwayIgG4, IgA, and IgE do not have complement receptors
Activated C1q activates C1r which in turn activates C1s
Activated C1s has esterolytic and proteolytic properties which acts on C4 splitting it into two fragments; C4a and C4b
C4b complexes with C1s forming an active component that acts on C2 splitting it into C2a and C2b
C2a binds to C4b creating a very active complex called the C3 convertase, where a single molecule can activate hundreds of C3 molecules
The Classical Pathway
C3 is split by C4b2a into C3a and C3b
C3b binds to cells and to C4b2a to generate C5 convertase which splits C5 into C5a and C5b
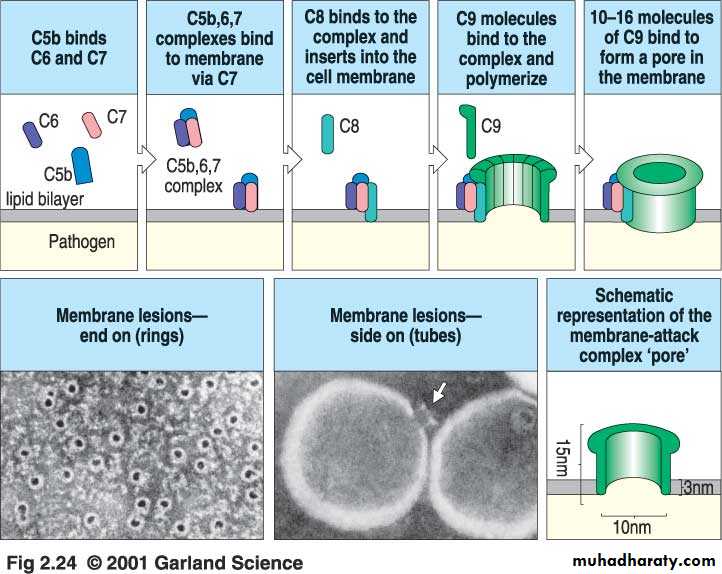
C5b binds to cells and activates C6 and C7The complex C5b67 activates C8 and C9 forming a giant molecule with a molecular weight of 106 Daltons called the membrane attack complex (MAC)
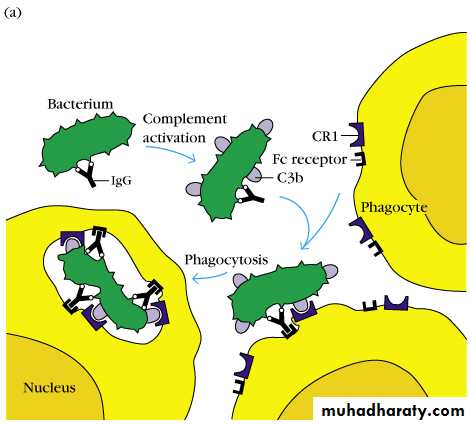
C3b can bind to bacteria and enhance phagocytosis.
The Classical Pathway
C5b6789 bound to cells insert themselves into the cell membrane and produce transmembrane channels allowing ions to pass throughThe osmotic equilibrium of the cell is disturbed with rapid influx of water into the cell which swells and lyses
Complement functions related to immune defense
Terminal complement components and the formation of the membrane attack complex
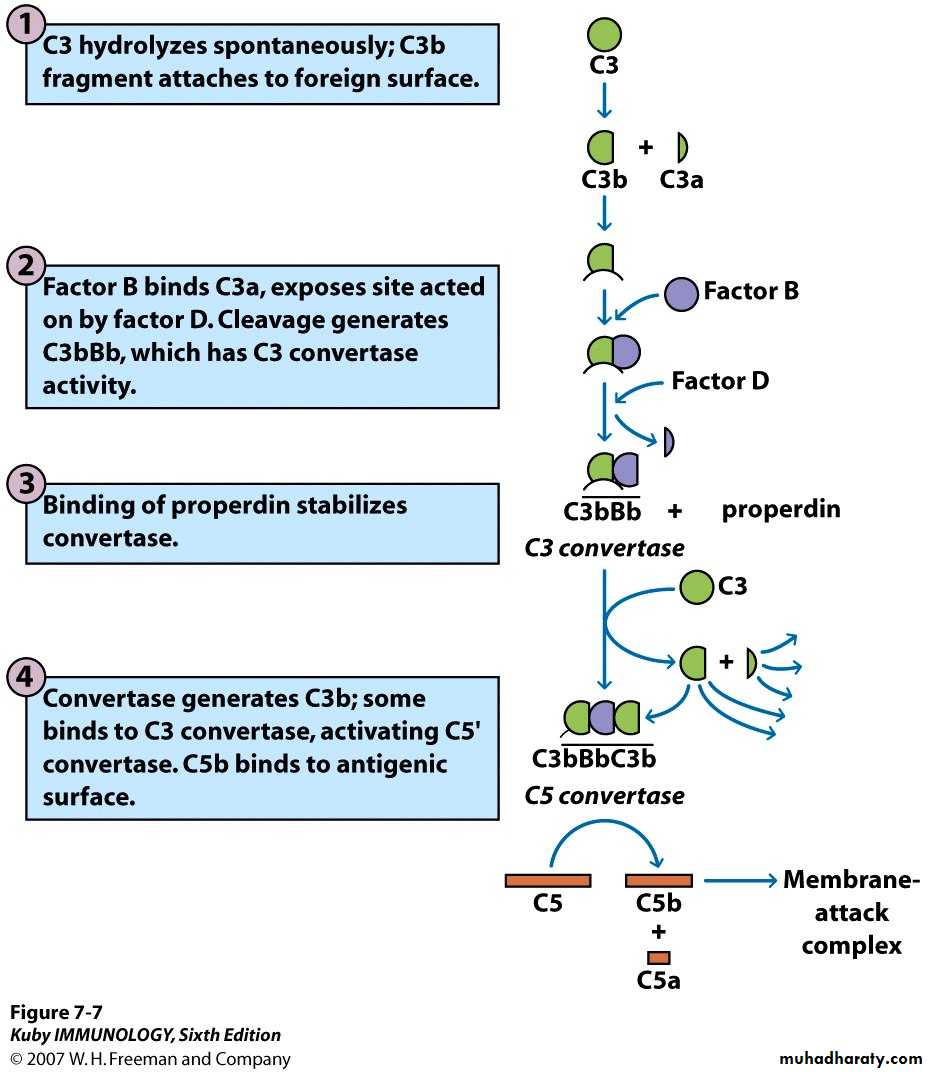
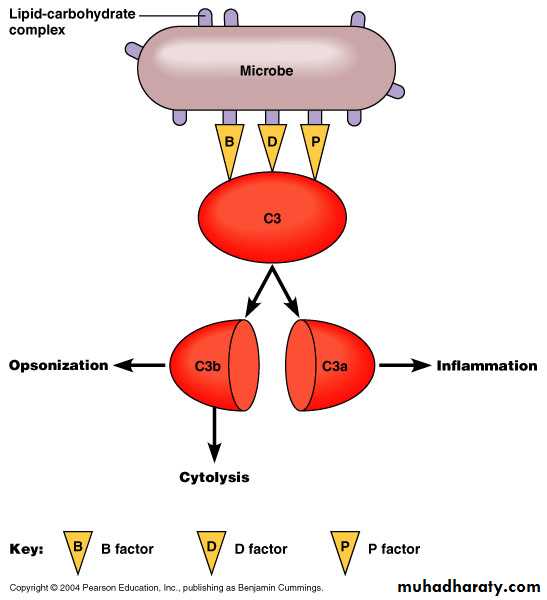
The Alternative (properdin) PathwayActivators: Bacterial LPS, cell wall of some bacteria, some yeast cells, aggregated IgA, and a factor
Components: C3 – C9, factor B, factor D, and Properdin
C3b present in trace amounts in serum combines with factor B forming C3bBThe alternative system
C3 is the principal protein of concern.
Exists in high concentrations
Contains an unstable internal thiolester with slow “spontaneous” (or serum protease mediated) cleavage.By convention, the smaller product is designated “a” and the larger “b” (though there is one exception.)
C3b can bind to bacteria and enhance phagocytosis.
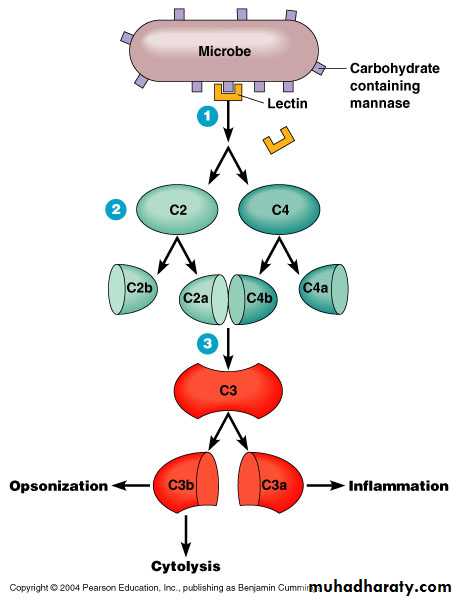
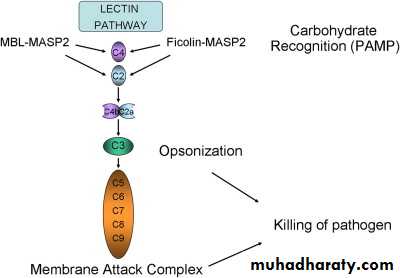
Mannose-binding Lectin PathwayThis pathway is activated by the binding of mannose-binding lectin (MBL) to mannose residues on the pathogen surface. This in turn activates the MBL-associated serine proteases, MASP-1 and MASP-2, which activate C4 and C2, to form the C3 convertase, C4b2a.
Alternative Pathway
Figure 16.14Lectin Pathway
Figure 16.15General Functions of Complement
Role of Complement in DiseaseThe complement system plays a critical role in inflammation and defence against some bacterial infections. Complement may also be activated during reactions against incompatible blood transfusions, and during the damaging immune responses that accompany autoimmune disease. Deficiencies of individual complement components or inhibitors of the system can lead to a variety of diseases (Table 1), which gives some indication of their role in protection against disease
Table 1. Diseases associated with complement deficiencies
• Complement Deficiency• Disease
• C3 and Factor B
• Severe bacterial infections
• C3b-INA, C6 and C8
• Severe Neisseria infections
• Deficiencies of early C components C1, C4, C2.
• Systemic lupus erythematosus (SLE), glomerulonephritis and polymyositis
• C1-inhibitor
• Hereditary angioedema