Immunity to infection12-6-2021
Dr. Minen Al-Kafajy08 كانون الأول، 21
Dr. Minen Al-Kafajy
1
Introduction
From the moment of birth, the host is constantly exposed to a wide variety of bacteria and viruses. In general, the host manages to either eliminate or ward off these invading organisms, and a symbiosis is achieved between microbes and the host. How does this occur? There are two major pathways to achieve this resistance: non-specific and adaptive.08 كانون الأول، 21
Dr. Minen Al-Kafajy
2
The establishment of an infection depends on several factors:
Characteristics of the microorganismNumber of organisms
Mode of transmission (how and where they contact the host)
Stability of the organism (in and outside of the host)
08 كانون الأول، 21
Dr. Minen Al-Kafajy
3
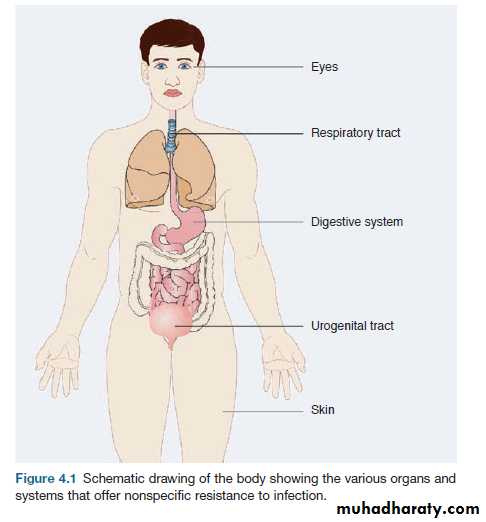
NONSPECIFIC RESISTANCE
Nonspecific or natural resistance refers tobarriers, secretions, and normal flora that
make up our external defenses.
Phagocytes and complement are also involved.
Mechanical barriers are highly effective, and the skin (our largest organ) is highly suited to this protection
Dr. Minen Al-Kafajy
4
08 كانون الأول، 21
Various organs and systems that offer nonspecific resistance to infection
08 كانون الأول، 21Dr. Minen Al-Kafajy
5
Macrophages is a non-specific resistance
Macrophages reside in the subepithelial tissues of the skin and intestine and line the alveoli of the lungs. Microbes that penetrate an epithelial surface will encounter local tissue macrophages called histocytes. If the organism enters via blood or lymph, then defense is provided by fixed macrophages called Kupffer cells, which line the sinusoids of the liver. Similarly fixed macrophages called Langerhans cells are also present in the epidermis of the skin. Once engaged with the organism, these macrophages release a number of macrophage-derived cytokines, which nonspecifically amplify the immunological and inflammatory reactions to the invading microbe.
08 كانون الأول، 21
Dr. Minen Al-Kafajy
6
How pathogenic resist phagocytosis
Group A streptococci have cell surface structures called M proteins of which there are now more than 120 antigenically distinct molecules that inhibit direct phagocytosis, mainly by preventing deposition of complement on the organism.08 كانون الأول، 21
Dr. Minen Al-Kafajy7
How pathogenic resist phagocytosis
pneumococcal polysaccharide capsule of which there are thirty to forty distinct polysaccharides. Another approach (taken by both group A streptococci and staphylococci) is the release of potent extracellular toxins, which kill phagocytes with the formation of pus. An intriguing bacterium, Mycobacterium tuberculosis, can be ingested by phagocytes but resists intracellular killing, often persisting for years in the macrophage.08 كانون الأول، 21
Dr. Minen Al-Kafajy
8
ADAPTIVE IMMUNITY
A specific immune response to invading microbes is conveniently divided into:humoral and cellular immunity.
The importance of each arm of the specific response varies from infection to infection.
Experimental animal models and naturally occurring immunodeficiency states clearly demonstrate that certain components of the immune response are crucial for controlling a particular infection.
08 كانون الأول، 21
Dr. Minen Al-Kafajy
9
individuals with antibody deficiencies:
are particularly prone to repeated infections with pyrogenic bacteria.
Yet, replacement therapy with immunoglobulin
greatly reduces the number of infections.
Interestingly, these individuals can mount a normal response to most viruses (varicella, measles, mumps, etc.).
Yet the absence of mucosal antibody does make them susceptible to some enteroviruses.
08 كانون الأول، 21
Dr. Minen Al-Kafajy
10
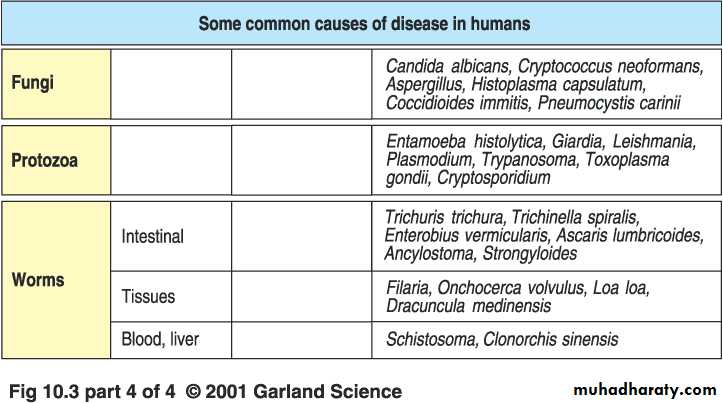
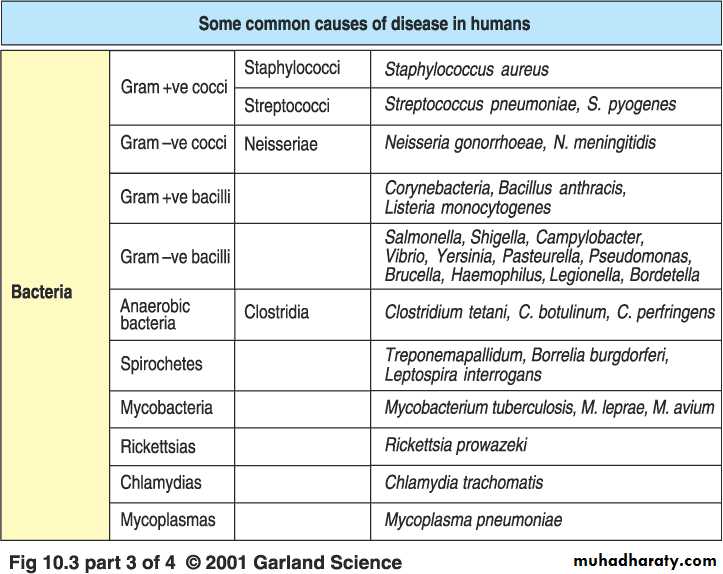
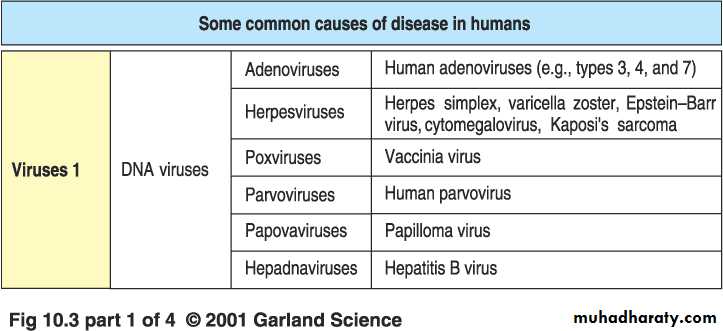
Major classes of pathogens
BACTERIAL INFECTION
The immune system responds to bacterial infections in two major ways.
First, it may respond to soluble products of the cell such as toxins or released structural antigens like LPS of a given gram-negative bacterial cell.
Most bacterial antigens are T-cell dependent and require helper T cells for initiation of the immune response. Yet certain cell antigens, such as the pneumococcal polysaccharides, are T-cell independent.
They are large-molecular-weight molecules, and in children, antibody response to these antigens may take four to six years. Thus, younger children are susceptible to these infections.
08 كانون الأول، 21
Dr. Minen Al-Kafajy
12
BACTERIAL INFECTION
08 كانون الأول، 21Dr. Minen Al-Kafajy
13
Streptococcal antigens include specific toxins such as streptolysins O and S that lyse blood and tissue cells and pyrogenic exotoxins, which act as superantigens to overstimulate the host responses. There are also specific enzymes such as hyaluronidase and streptokinase, which help promote the spread of infecting streptococcus. Perhaps most important is the M protein , a cell surface antigen of the group A streptococcus that allows the bacteria to evade immune defenses (especially neutrophils and complement).
BACTERIAL INFECTION
M protein functions is to bind host factor H, which prevents complement C3 from depositing on the streptococcal surface. Since efficient phagocytosis by neutrophils requires interaction with its C3 receptor, factor H prevents this interaction.08 كانون الأول، 21
Dr. Minen Al-Kafajy
14
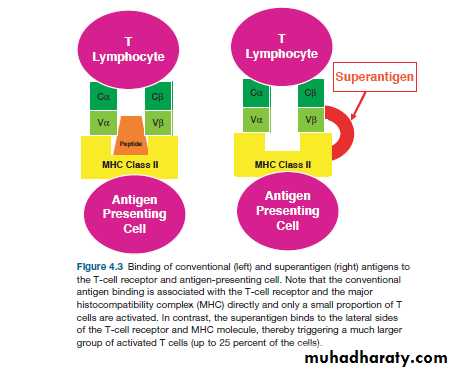
BACTERIAL SUPERANTIGENS
Among the toxins secreted by bacteria is a special group from the streptococcal and staphylococcal family of toxins called superantigens (SAg).
toxins bind to the lateral surface of both the T-cell receptor and the MHC (see Figure 4.3). Thus, in contrast to a conventional peptide antigen, which stimulates only one in 104 to108 T cells.
the superantigen may bind up to approximately 1:50 T cells. The result is a veritable explosion of cytokines resulting in high fever, hypotension, and multiorgan shock. Death often occurs within 24 hours of the release of these toxins.
08 كانون الأول، 21
Dr. Minen Al-Kafajy
15
Superantigen
08 كانون الأول، 21Dr. Minen Al-Kafajy
16
TYPES OF DEFENSE SYSTEMS
1- Immediate immune responseComplement
Phagocytosis
Natural Antibodies
2- Early immune response
3- Late immune response
08 كانون الأول، 21Dr. Minen Al-Kafajy
17
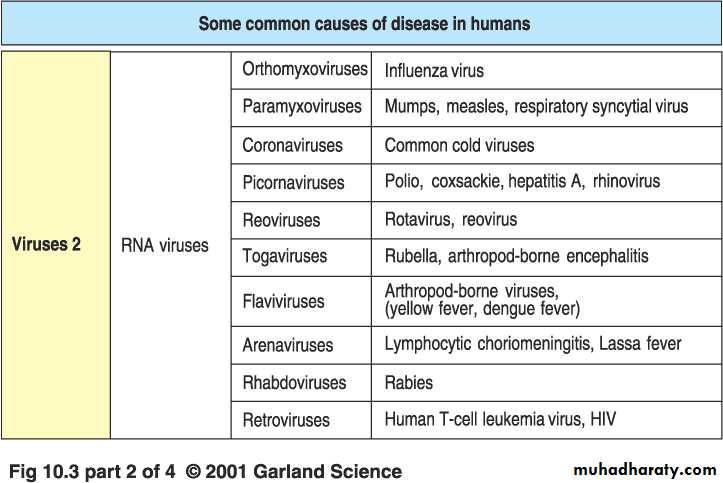
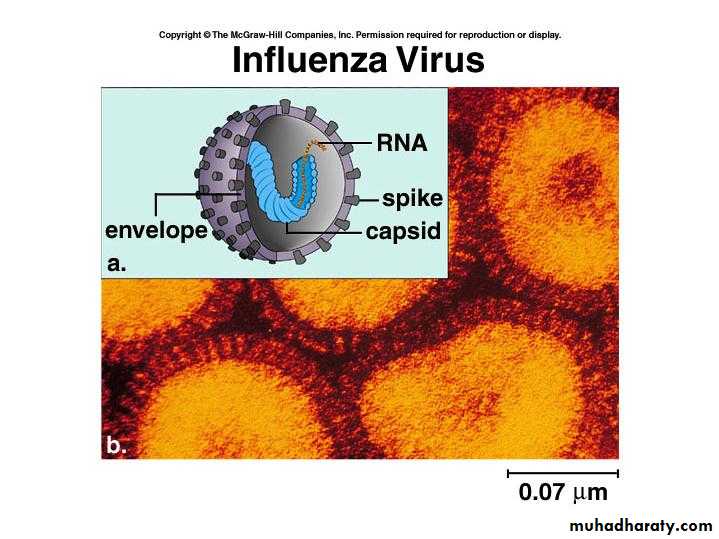
Immunity to Viruses
Viruses are obligate intracellular microorganismsThey require the host cells to drive protein synthesis and metabolize sugar
Viroids are infectious agents that consist of nucleic acids alone
Prions are infectious proteins associated with degenerative neurological diseases of human
08 كانون الأول، 21
Dr. Minen Al-Kafajy
18
08 كانون الأول، 21
Dr. Minen Al-Kafajy19
Mechanisms involving T cells
CD8+ cells ; These are MHC class 1 restricted cells that focus on the site of virus replication and destroy virus infected cells
CD4+ cells ;
Key factor in defense against viral infectionINF gamma is important for the activation of TNF alpha which induce apoptosis
08 كانون الأول، 21
Dr. Minen Al-Kafajy
20
Immunopathology of Viral Infection
1- Response to viral infection may cause tissue damageAg-Ab complex deposition in kidney and blood >>> inflammatory response >>> T cell mediated damage >> killing of host cells
2- Virus may infect immune cells
3- Viral infection may induce autoimmunity due to antigenic mimicry
08 كانون الأول، 21
Dr. Minen Al-Kafajy
21
Immunity to EPV
08 كانون الأول، 21Dr. Minen Al-Kafajy
22
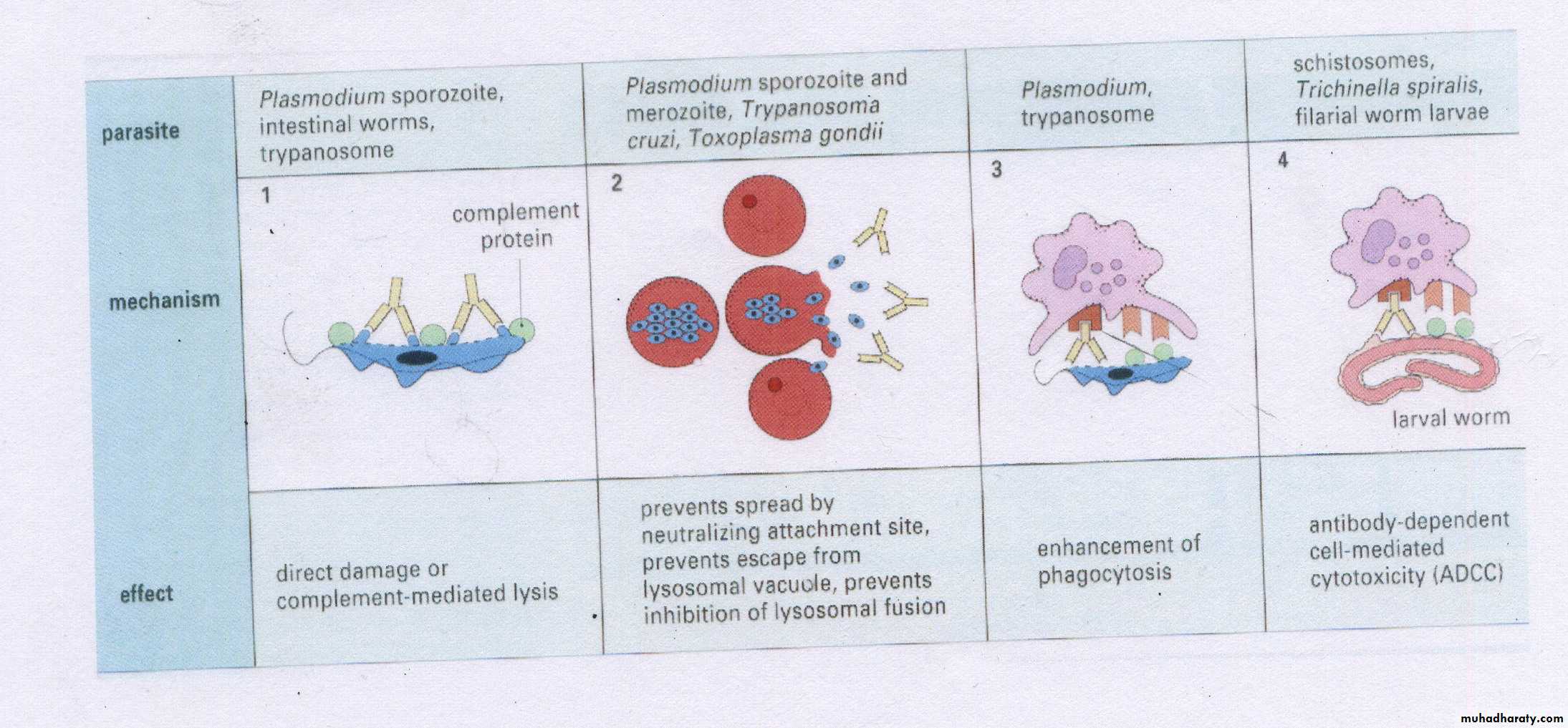
Immunity to Parasites
Stimulate a number of immunological defense mechanismsBoth humoral and cellular responses
Immune response depends on the stage and the type of infection
Most parasites pass through a complicated life cycle
08 كانون الأول، 21
Dr. Minen Al-Kafajy23
Features of Parasitic infection:
1- Infect large number of people2- Parasitic infection have common features
Varity and large quantity of Ag
Ability to change their surface Ag
Complicate life cycle
Different mode of entry
3- Most parasites are host specific
4- Host resistance to parasite may be genetic
5- Many parasitic infections are chronic
08 كانون الأول، 21
Dr. Minen Al-Kafajy
24
Effector mechanisms by Immune cells
MACROPHAGES
Provide strong defense against small parasites
Secrete factors that kill parasites without ingestion
Secrete cytokines that activate other immune cells
Synthesize nitric oxide that act as parasite toxin
Activation of macrophages is a general feature of early stage of infection
08 كانون الأول، 21
Dr. Minen Al-Kafajy
25
NEUTROPHILS
Can kill large and small parasitesPhagocytic activation
Have granules that contain cytotoxic proteins
Have Fc and complement receptors >> ADCC
PLATELETS
Cytotoxic activities against larval stagesActivation are enhanced by cytokines
08 كانون الأول، 21
Dr. Minen Al-Kafajy
26
EOSINOPHILS
Characterize parasitic infection
Thought to be specific against tissue parasites
Limit migration of parasites through the host
Less phagocytic than neutrophils
Act in accordance with mast cells
08 كانون الأول، 21
Dr. Minen Al-Kafajy
27
Role of T cells
The type of T cells involved is determined by the type and the stage of the infectionCytokines enhance protective immunity against intracellular parasites
T helper 2 cells are essential for the elimination of intestinal worms08 كانون الأول، 21
Dr. Minen Al-Kafajy28
Role of Antibodies
Parasites induce production of specific and non specific Abs
Antibodies have several functions on parasites
-Act directly on protozoa
-Block attachment to host cells
-Important for Phagocytosis
08 كانون الأول، 21
Dr. Minen Al-Kafajy29
08 كانون الأول، 21
Dr. Minen Al-Kafajy30
08 كانون الأول، 21
Dr. Minen Al-Kafajy
31
للاطلاع
FUNGAL INFECTION
Fungi cause many diseases, most of which are adequately handled by the immune system of the normal host. However, the increased use of immunosuppressive drugs – the immunosuppression secondary to HIV infection – has raised our awareness of these infections. For example, Candida albicans can cause superficial infections in the normal host and is found throughout the intestinal tract and commonly in the vagina. The organism is usually kept under control by the bacterial flora, but changes in these flora secondary to overuse of antibiotics or changes in hormone balance will favor a chronic superficial infection. All of this is exacerbated in the immunocompromised host.08 كانون الأول، 21
Dr. Minen Al-Kafajy
32