GIT Physiology Lectures
Dr-Suroor Mohamed
MBChB.MSc-Physiology / December 2021
Gastrointestinal
System
( The Digestive System)
Lecture 1
Dr. Suroor
Mohamed
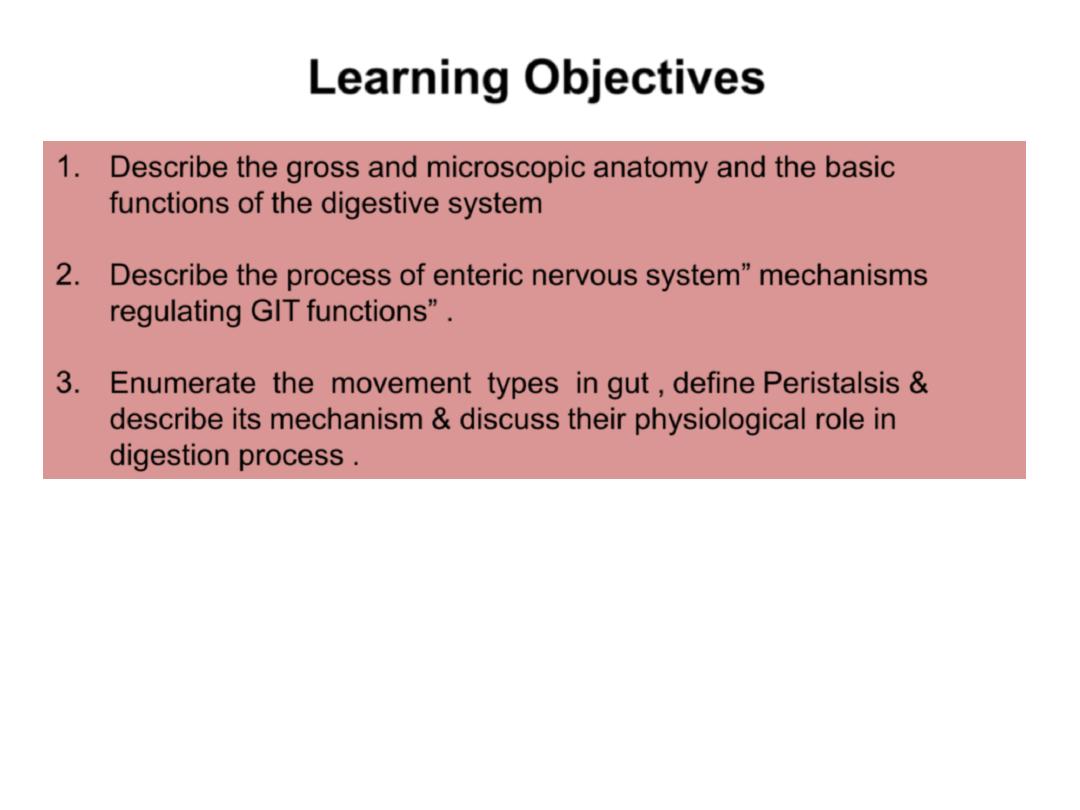
Learning Objectives
1.
Describe the gross and microscopic anatomy and the basic
functions of the digestive system
2.
Describe the process of enteric nervous
system” mechanisms
regulating GIT
functions” .
3.
Enumerate the movement types in gut , define Peristalsis &
describe its mechanism & discuss their physiological role in
digestion process .
.
The Components of the Digestive
System
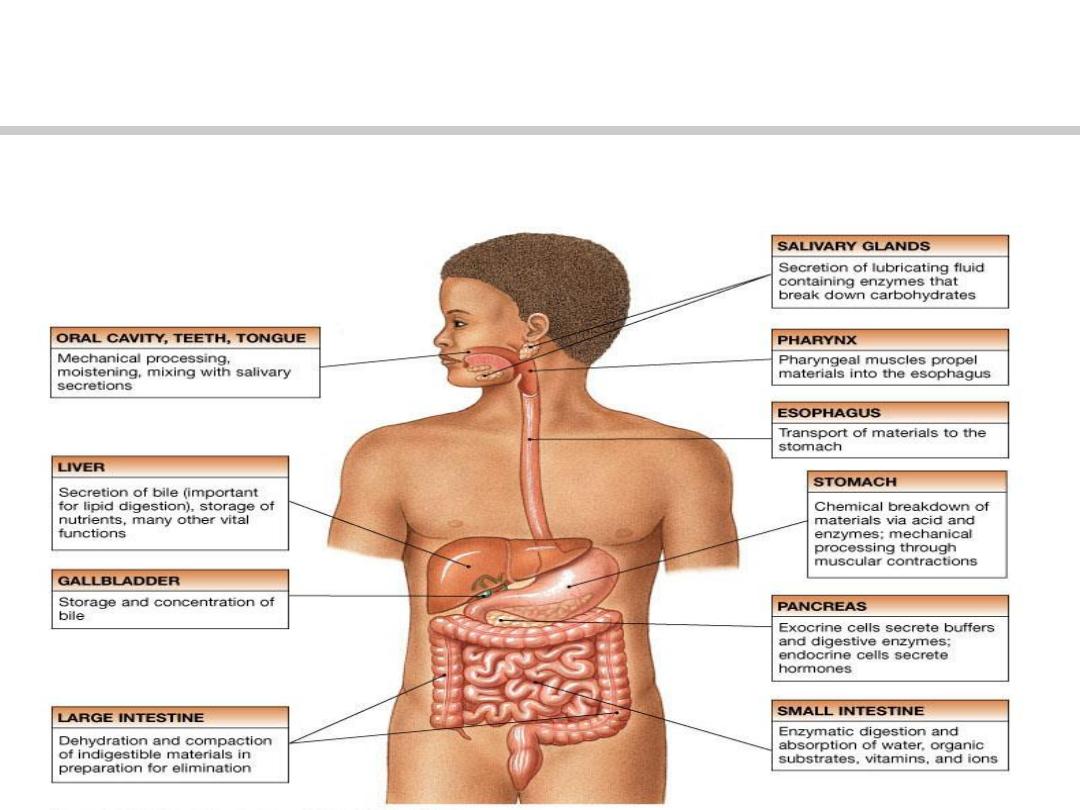
This system consist of: the mouth, esophagus, stomach, small intestine, large
intestine and also three glands connected to the tract (liver, pancreas, and salivary
glands).
The primary function of the alimentary tract
is to break down food and to provide the body with a continual
supply of water, electrolytes and nutrients. To achieve this function, the GIT must performs the following processes:
ingestion, movement, digestion, absorption, secretion and defecation.
The digestive system is a tube running from mouth to anus. It provides the body with a continual supply of water,
electrolytes, vitamins, and nutrients, which requires:
(1) movement of food through the alimentary tract;
(2) secretion of digestive juices and digestion of the food
(3) absorption of water, various electrolytes, vitamins, and digestive products;
(4) circulation of blood through the gastrointestinal organs to carry away the absorbed substances
(5) control of all these functions by local, nervous, and hormonal systems.
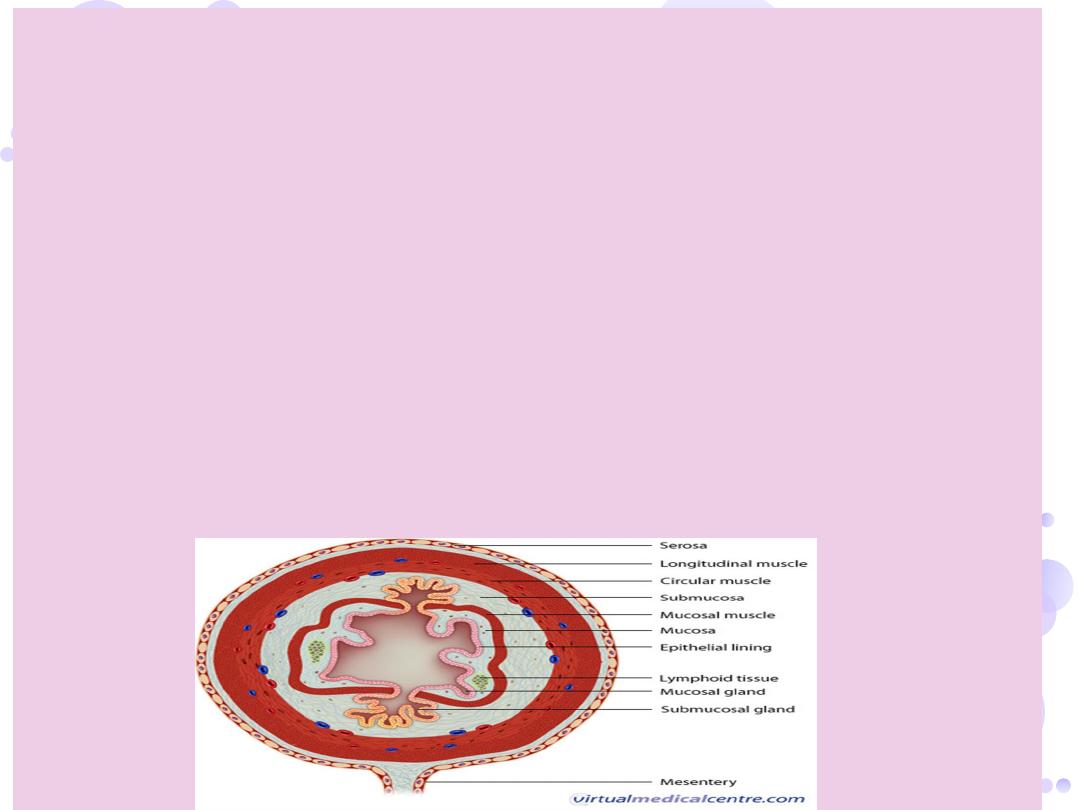
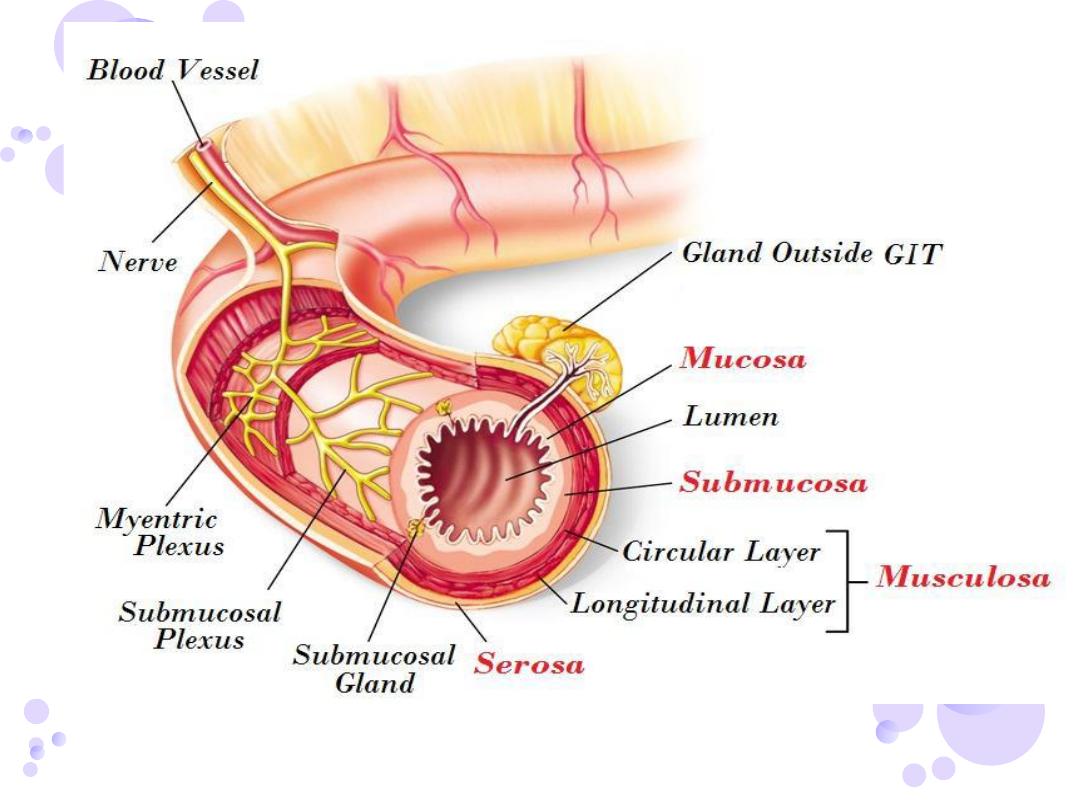
PHYSIOLOGICAL ANATOMY OF THE GASTROINTESTINAL WALL
A typical cross section of the intestinal wall show the following layers from the outer surface inward: (1) the serosa, (2)
a longitudinal smooth muscle layer, (3) a circular smooth muscle layer, (4) the submucosa, and (5) the mucosa. In
addition, sparse bundles of smooth muscle fibers, the mucosal muscle, lie in the deeper layers of the mucosa..
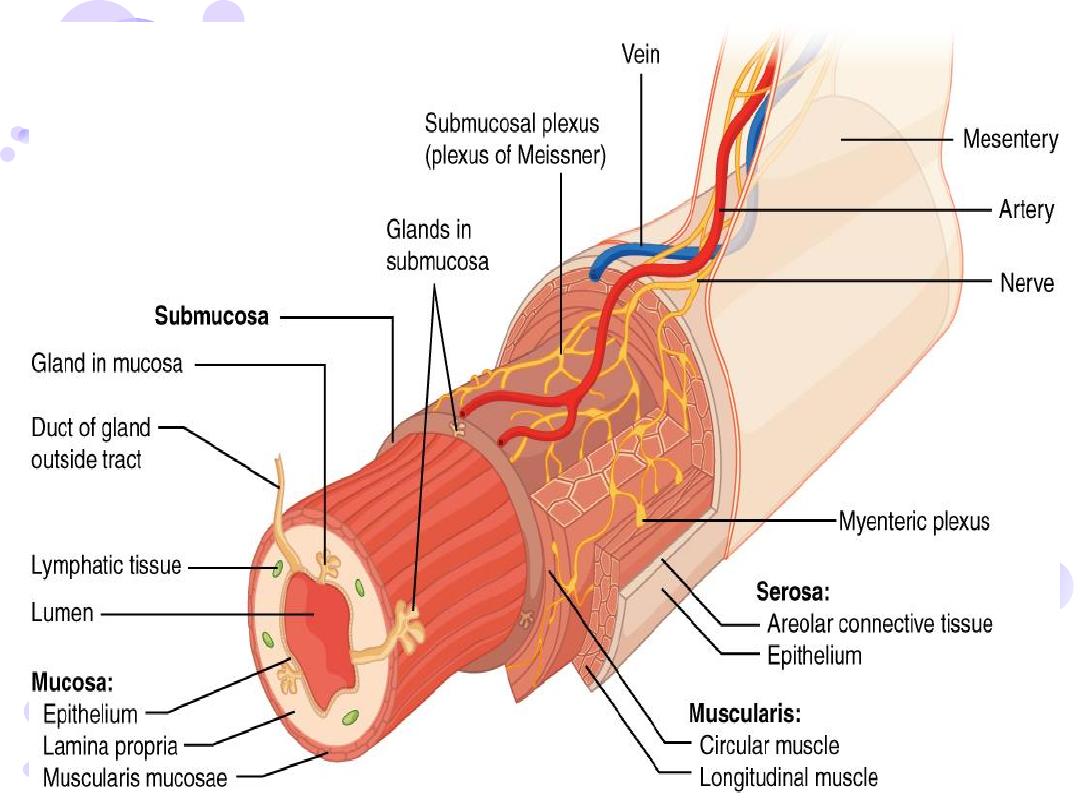
ENTERIC
—
NEURAL CONTROL OF GASTROINTESTINAL FUNCTION
NERVOUS SYSTEM
The gastrointestinal tract has a nervous system all its own called the enteric
nervous system. It lies entirely in the wall of the gut, beginning in the
esophagus and extending all the way to the anus. The number of neurons in this
enteric system is about 100 million, nearly equal to the number in the entire
spinal cord. This highly developed enteric nervous system is especially important
in controlling gastrointestinal movements and secretion.
The enteric nervous system is composed mainly of two plexuses, shown in
Figure below: (1) an outer plexus lying between the longitudinal and circular
muscle layers, called the
myenteric plexus or Auerbach’s plexus
, and (2)
an inner plexus, called the
submucosal plexus or Meissner’s plexus
, which
lies in the submucosa
.
The myenteric plexus controls mainly the gastrointestinal movements, and the
submucosal plexus controls mainly gastrointestinal secretion and local blood
flow.. Although the enteric nervous system can function independently of these
extrinsic nerves, stimulation by the parasympathetic and sympathetic
systems can greatly enhance or inhibit gastrointestinal functions.

DIFFERENCES BETWEEN THE MYENTERIC AND SUBMUCOSAL PLEXUSES
The myenteric plexus consists mostly of a linear chain of many interconnecting
neurons that extends the entire length of the gastrointestinal tract. Because
the myenteric plexus extends all the way along the intestinal wall and lies
between the longitudinal and circular layers of intestinal smooth muscle, it is
concerned mainly with controlling muscle activity along the length of the gut.
When this plexus is stimulated, its principal effects are (1) increased tonic
contraction, or “tone,” of the gut wall; (2) increased intensity of the rhythmical
contractions; (3) slightly increased rate of the rhythm of contraction; and (4)
increased velocity of conduction of excitatory waves along the gut wall, causing
more rapid movement of the gut peristaltic waves.
The myenteric plexus should not be considered excitatory because some of its
neurons are
inhibitory
; their fiber endings secrete an inhibitory transmitter,
possibly
vasoactive intestinal polypeptide
or some other inhibitory peptide. The
resulting inhibitory signals are especially useful for inhibiting some of the
intestinal sphincter muscles that impede movement of food along successive
segments of the gastrointestinal tract, such as the
pyloric sphincter
, which
controls emptying of the stomach into the duodenum, and the sphincter of the
ileocecal valve
, which controls emptying from the small intestine into the cecum.

The submucosal plexus, in contrast to the myenteric plexus, is mainly concerned with
controlling function within the inner wall of each minute segment of the intestine. For
instance, many sensory signals originate from the gastrointestinal epithelium and are then
integrated in the submucosal plexus to help control local intestinal secretion, local
absorption, and local contraction of the submucosal muscle that causes various degrees of
infolding of the gastrointestinal mucosa
TYPES OF NEUROTRANSMITTERS SECRETED BY ENTERIC NEURONS
different neurotransmitter substances that are released by the nerve endings of
different types of enteric neurons, including: (1) acetylcholine, (2) norepinephrine, (3)
adenosine triphosphate, (4) serotonin, (5) dopamine, (6) cholecystokinin, (7) substance P,
(8) vasoactive intestinal polypeptide VIP , (9) somatostatin, (10) leu-enkephalin, (11) met-
enkephalin.
Acetylcholine most often excites gastrointestinal activity
.enhances the activity of most
GIT functions, and causing sphincters to relax, so they are stimulatory to GIT.
Norepinephrine almost always inhibits gastrointestinal activity, as does epinephrine
, which
reaches the gastrointestinal tract mainly by way of the blood after it is secreted by the
adrenal medullae into the circulation..
In general, stimulation of the SNS inhibits activity in the GIT, while causing sphincters to
contract causing effects essentially opposite to those of the PNS.
It is initiated in the stomach as a response to vagal stimulation. PNS Cranial part by Vagus
nerves innervate esophagus, stomach, little innervations to small intestine, pancreas,
and first half of the large intestine.Vagotomy abolishes the motor activity in the
stomach, but leaves the periodic activity in the small bowel intact
The sacral fibers originate in S2, S3 S4 sacral segments of the spinal cord, and
supply the distal part of the large intestine.
.
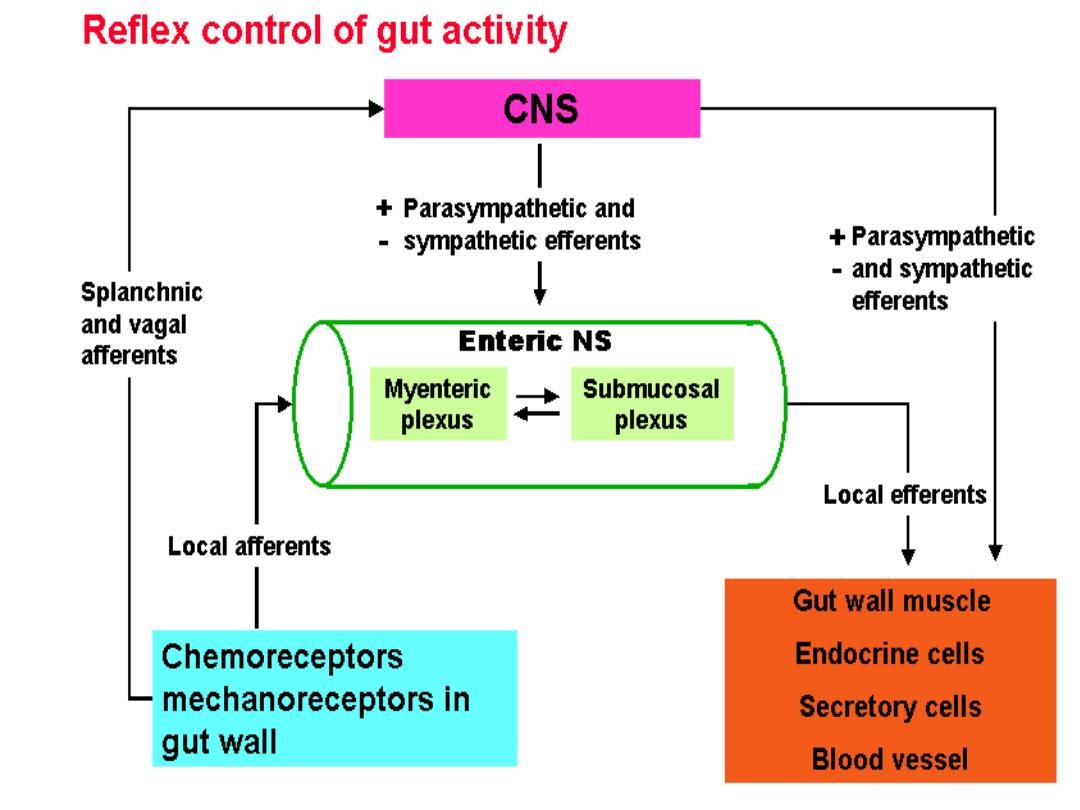
Long reflex arc
Short reflex arc
FUNCTIONAL TYPES OF MOVEMENTS IN THE GASTROINTESTINAL TRACT
Two types of movements occur in the gastrointestinal tract: (1) propulsive movements,
which cause food to move forward along the tract at an appropriate rate to accommodate
digestion and absorption, and (2) mixing movements, which
keep the intestinal contents thoroughly mixed at all times
PROPULSIVE MOVEMENTS—PERISTALSIS
قوة دافعت
/
موجت متعاقبت
A contractile ring appears around the gut and then moves forward; this mechanism is
analogous to putting one’s fingers around a thin distended tube, then constricting the
fingers and sliding them forward along the tube. Any material in front of the contractile
ring is moved forward.
Peristalsis is an inherent property
خاصيت مميزة
of many syncytial smooth muscle tubes; stimulation at any point in the gut can cause a
contractile ring to appear in the circular muscle, and this ring then spreads along the gut
tube. (Peristalsis also occurs in the bile ducts, glandular ducts, ureters, and many other
smooth muscle tubes of the body.) It is due to contraction of the smooth muscle and it's
not unique for GIT it is also occurs in other organs like ureters
In peristalsis, contraction of a small section of proximal muscle , relaxation of the muscle
just distal to it ,wavelike motion moves food along the GIT
.
Peristalsis has one direction of movement called oral to caudal direction (oral to rectal)
while in abnormal conditions e.g vomiting, the direction will be reversed (opposite).
The stimulus for peristalsis is distention of lumen of GIT by food (or other material even a
foreign body). This distention is going to stimulate the mechanoreceptor which will send
impulse to Myenteric nerve plexus which will initiates peristalsis.
.
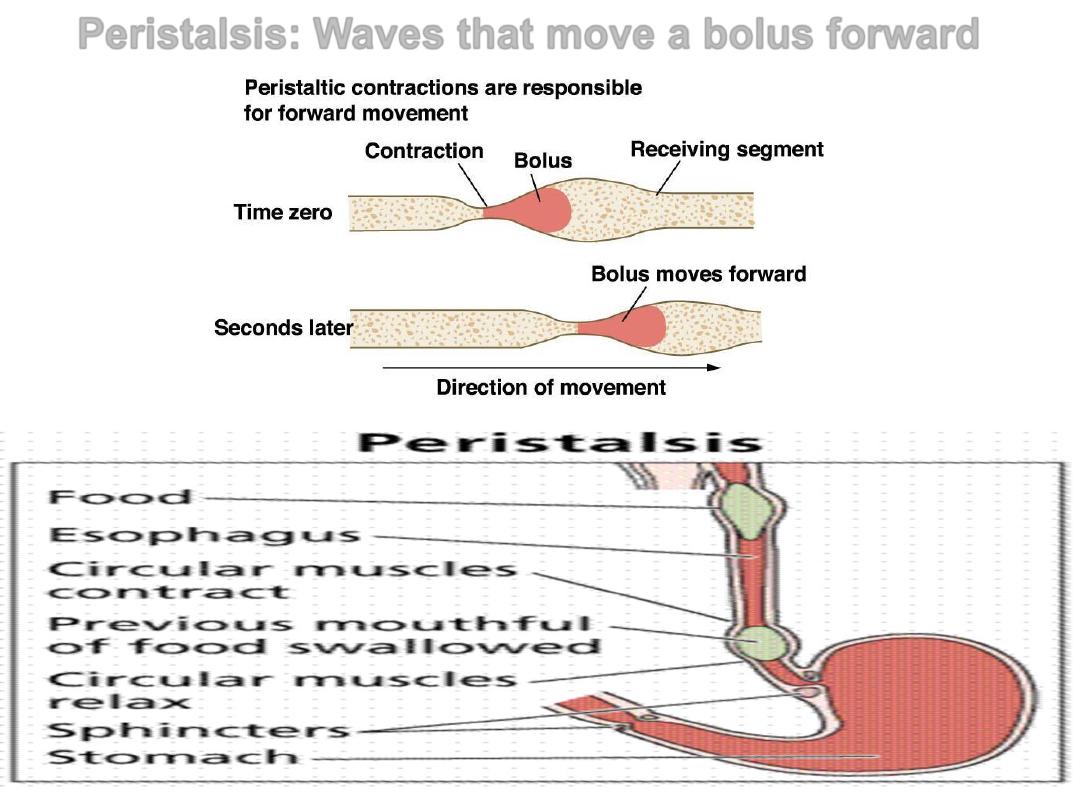
Peristalsis: Waves that move a bolus forward
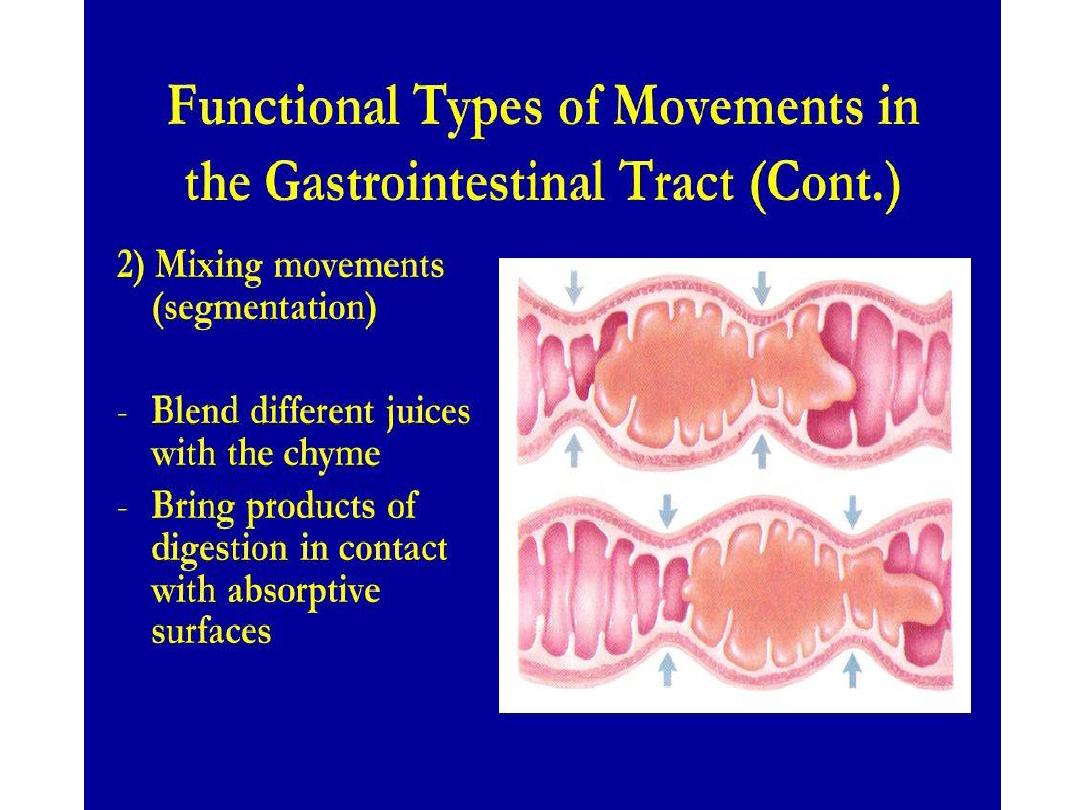
MIXING MOVEMENTS “ segmentation “
Mixing movements differ in different parts of the alimentary tract. In some
areas,
the peristaltic contractions cause most of the mixing
. This is
especially true when forward progression of the intestinal contents is
blocked by a sphincter so that a peristaltic wave can then only
churn
the
يخض بعنف
intestinal contents, rather than propelling them forward.
At other times, local intermittent constrictive contractions occur every few
centimeters in the gut wall. These constrictions usually last only 5 to 30
seconds; new constrictions then occur at other points in the gut, thus
“chopping”
cut
and “shearing”
part
the contents first here and then there.
The usual stimulus for intestinal peristalsis is distention of the gut
. That
is, if a large amount of food collects at any point in the gut, the stretching of
the gut wall stimulates the enteric nervous system to contract the gut wall 2
to 3 centimeters behind this point, and a contractile ring appears that
initiates a
peristaltic movement
. Other stimuli that can initiate peristalsis
include
chemical or physical irritation
of the epithelial lining in the gut. Also,
strong parasympathetic vagus
nervous signals to the gut will elicit strong
peristalsis.
Paralytic ileus
is a temporary cessation of gut motility that is most commonly caused
by abdominal surgery. Other common causes “appendicitis, hypokalemia,
and narcotics”.
Signs and symptoms of paralytic ileus include nausea and vomiting,
abdominal distension, and absent bowel sounds.