Medicine
Notes…
1
Presenting problems in disorders of sodium balance and water balance
DISORDERS OF WATER BALANCE:
Daily water intake can vary from about 500 mL to several litres a day. While a certain
amount of water is lost through the stool,
sweat and the respiratory tract (‘insensible
losses’, approximately 800 mL/day), and some water is generated by oxidative
metabolism
(‘metabolic water’, approximately 400 mL/day), the kidneys are chiefly
responsible for adjusting water excretion to maintain constancy of body water content and
body fluid osmolality (reference range 280
–295 milliosmol/kg).
Presenting problems in disorders of water balance:
Disturbances in body water balance, in the absence of changes in sodium balance, alter
plasma sodium concentration and hence plasma osmolality. When extracellular
osmolality changes abruptly, water flows rapidly across cell membranes with resultant cell
swelling (during hypo-osmolality) or shrinkage (during hyperosmolality).
Cerebral function is very sensitive to such volume changes, particularly brain swelling
during hypo-osmolality, which can lead to an increase in intracerebral pressure and
reduced cerebral perfusion.
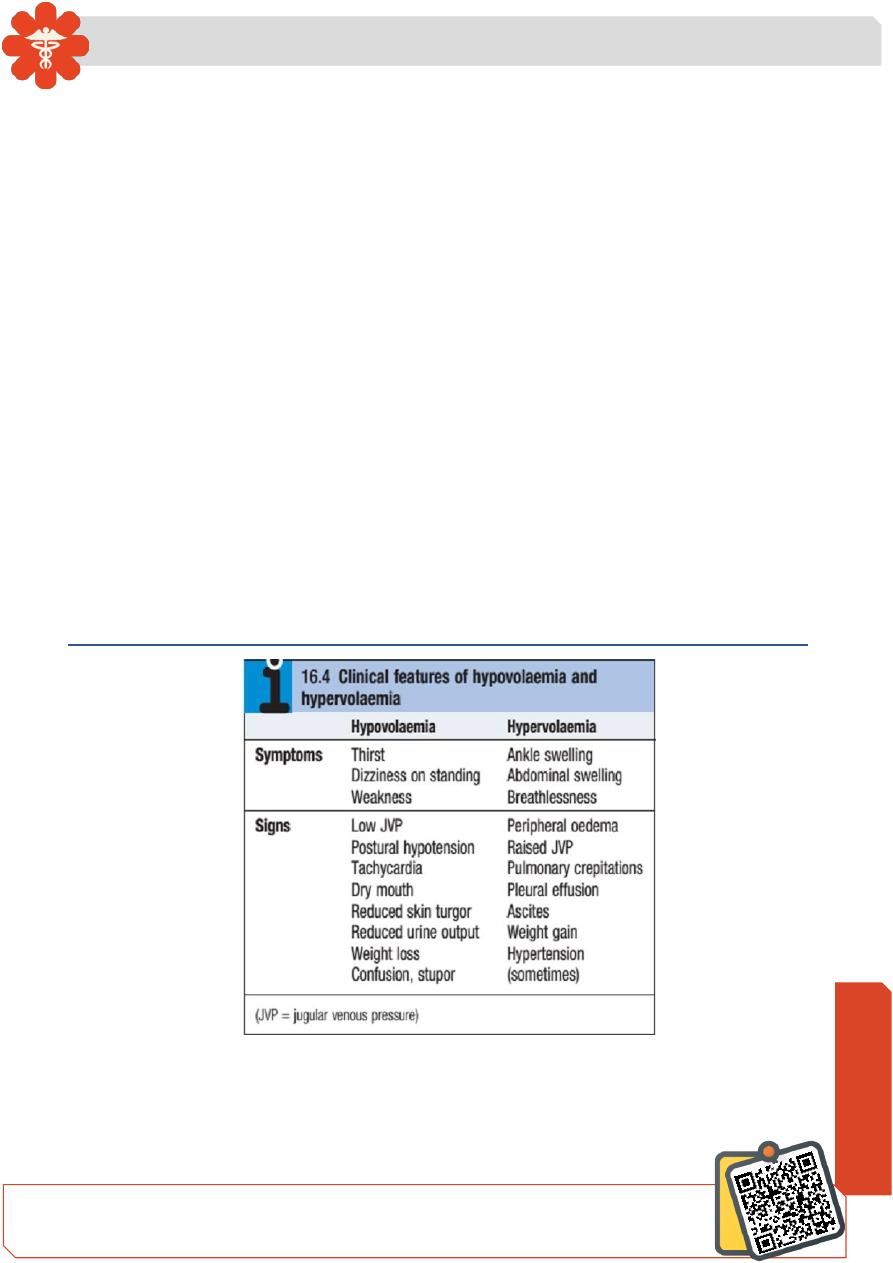
The diagnosis of hypovolaemia is based on characteristic symptoms and signs.
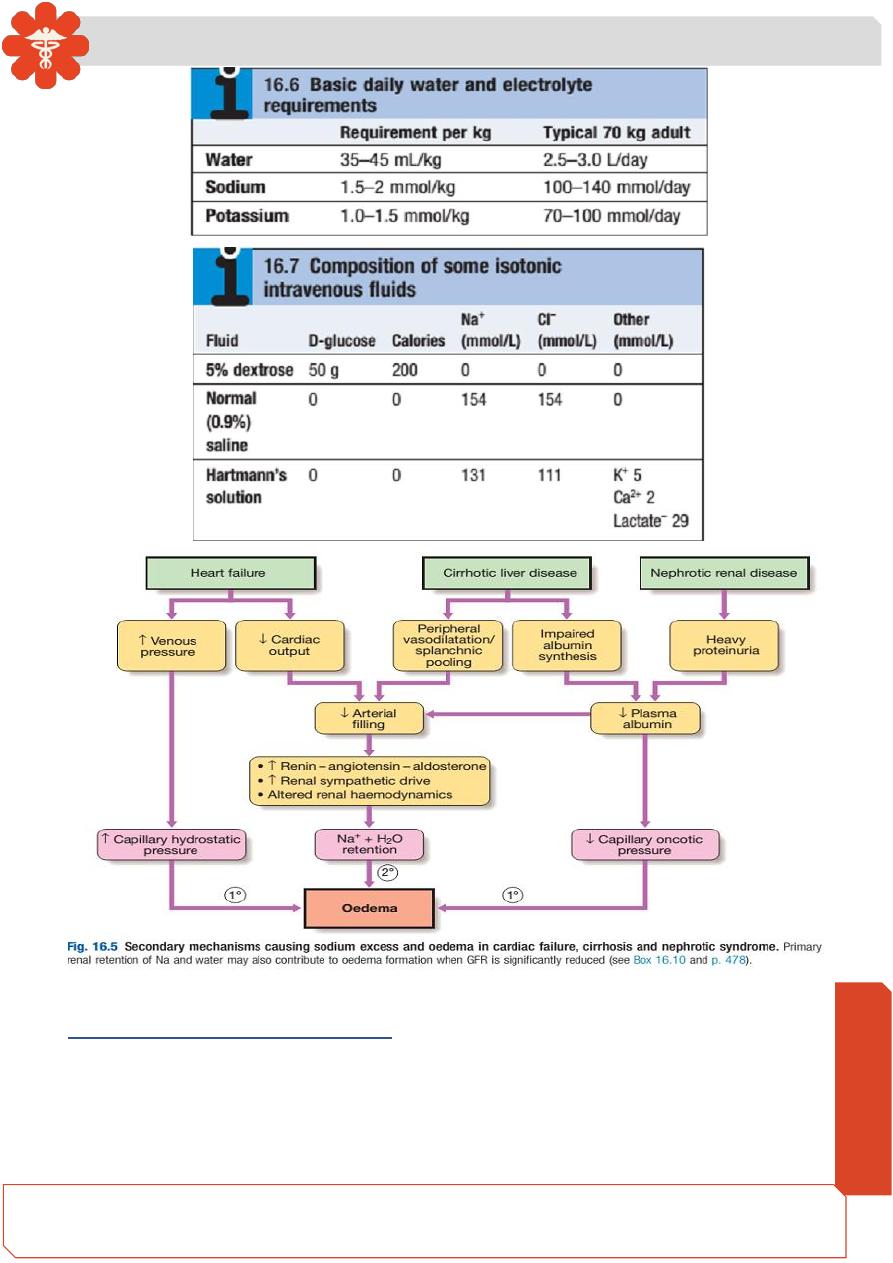
Intravenous fluid therapy:
The choice of fluid and the rate of administration depend on the clinical circumstances,
as assessed at the bedside and from laboratory data.
N
eed S
om
e H
el
p?
Medicine
Notes…
2
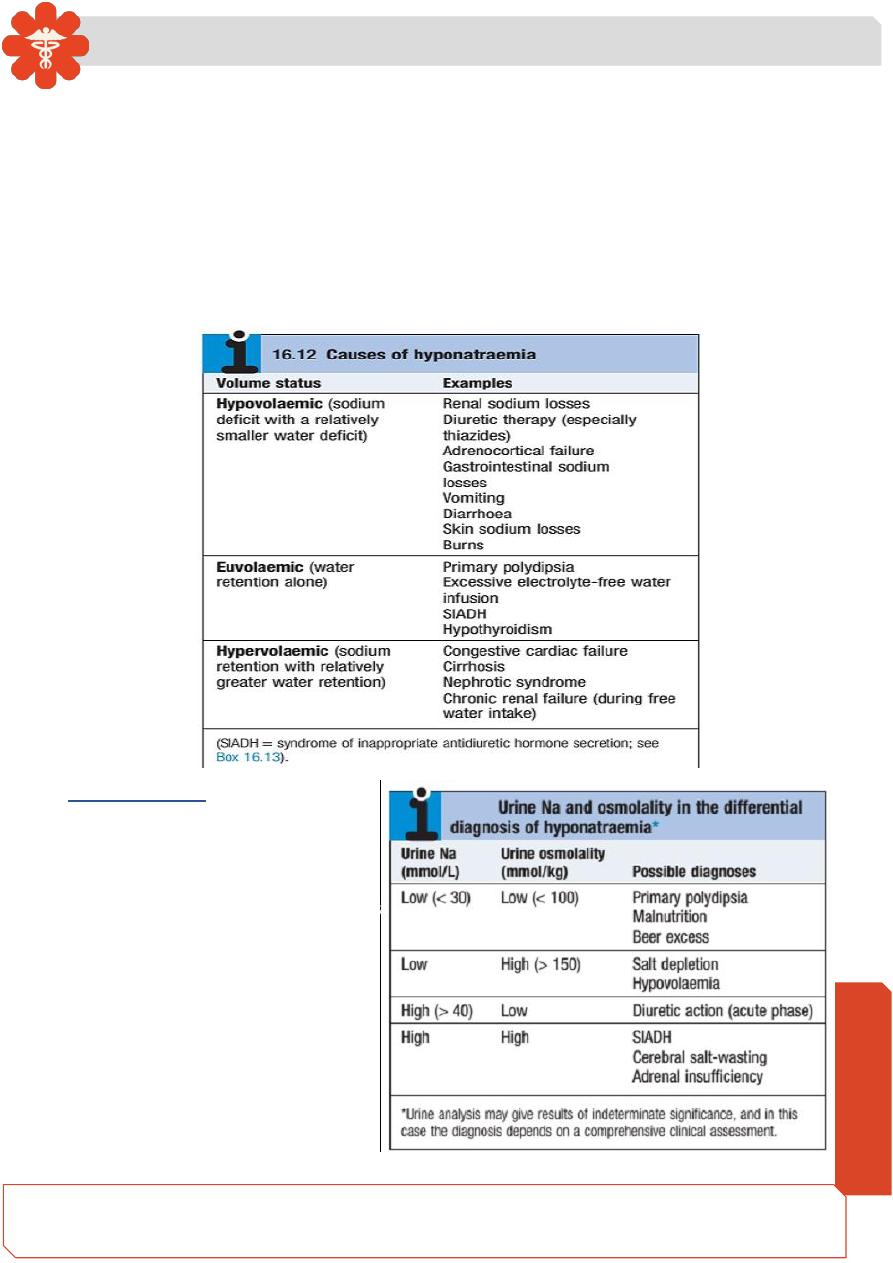
Hyponatraemia:
Aetiology and clinical assessment:
Hyponatraemia (plasma Na <135 mmol/L) is a common electrolyte abnormality, which is
often asymptomatic but which can also be associated with profound disturbances of
cerebral function, manifesting as anorexia, nausea, vomiting, confusion, lethargy,
seizures and coma.
Medicine
Notes…
3
The likelihood of symptoms occurring is related more to the speed at which electrolyte
abnormalities develop rather than their severity. When plasma osmolality falls rapidly,
water flows into cerebral cells, which become swollen and ischaemic. However, when
hyponatraemia develops gradually, cerebral neurons have time to respond by reducing
intracellular osmolality, through excreting potassium and reducing synthesis of
intracellular organic osmolytes .
The osmotic gradient favouring water movement into the cells is thus reduced and
symptoms are avoided.
Investigations:
Plasma and urine electrolytes and
osmolality are usually the only
tests required to classify the
hyponatraemia

Medicine
Notes…
4
Management
The treatment of hyponatraemia is critically dependent on its rate of development, severity
and underlying cause. If hyponatraemia has developed rapidly (over hours to days), and
there are signs of cerebral oedema such as obtundation or convulsions, sodium levels
should be restored to normal rapidly by infusion of hypertonic (3%) sodium chloride. A
common approach is to give an initial bolus of 100 mL, which may be repeated once or
twice over the initial hours of observation, depending on the neurological response and
rise in plasma sodium.
On the other hand, rapid correction of hyponatraemia that has developed slowly
(over weeks to months) can be hazardous, since brain cells adapt to slowly developing
hypo osmolality by reducing the intracellular osmolality, thus maintaining normal cell
volume .
Under these conditions, an abrupt increase in extracellular osmolality can lead to
water shifting out of neurons, abruptly reducing their volume and causing them to detach
from their myelin sheaths.
The resulting
‘myelinolysis’ can produce permanent structural and functional
damage to mid-brain structures, and is generally fatal.
The rate of correction of the plasma Na concentration in chronic asymptomatic
hyponatraemia should not exceed 10 mmol/L/day, and an even slower rate is generally
safer.

Medicine
Notes…
5
The underlying cause should be treated. For hypovolaemic patients, this involves
controlling the source of sodium loss, and administering intravenous saline if clinically
warranted. Patients with dilutional hyponatraemia generally respond to fluid restriction in
the range of 600
–1000 mL/day, accompanied where possible by withdrawal of the
precipitating stimulus (such as drugs causing SIADH).
If the response of plasma sodium is inadequate, treatment with demeclocycline
(600
–900 mg/day) may be of value by enhancing water excretion, through its inhibitory
effect on responsiveness to ADH in the collecting duct. An effective alternative for subjects
with persistent hyponatraemia due to prolonged SIADH is oral urea therapy (30
–45
g/day), which provides a solute load to promote water excretion. Where available, oral
vasopressin receptor antagonists such as tolvaptan may be used to block the ADH-
mediated component of water retention in a range of hyponatraemic conditions.
Hypervolaemic patients with hyponatraemia need treatment of the underlying condition,
accompanied by cautious use of diuretics in conjunction with strict fluid restriction.
Potassium-sparing diuretics may be particularly useful in this context where there is
significant secondary hyperaldosteronism.
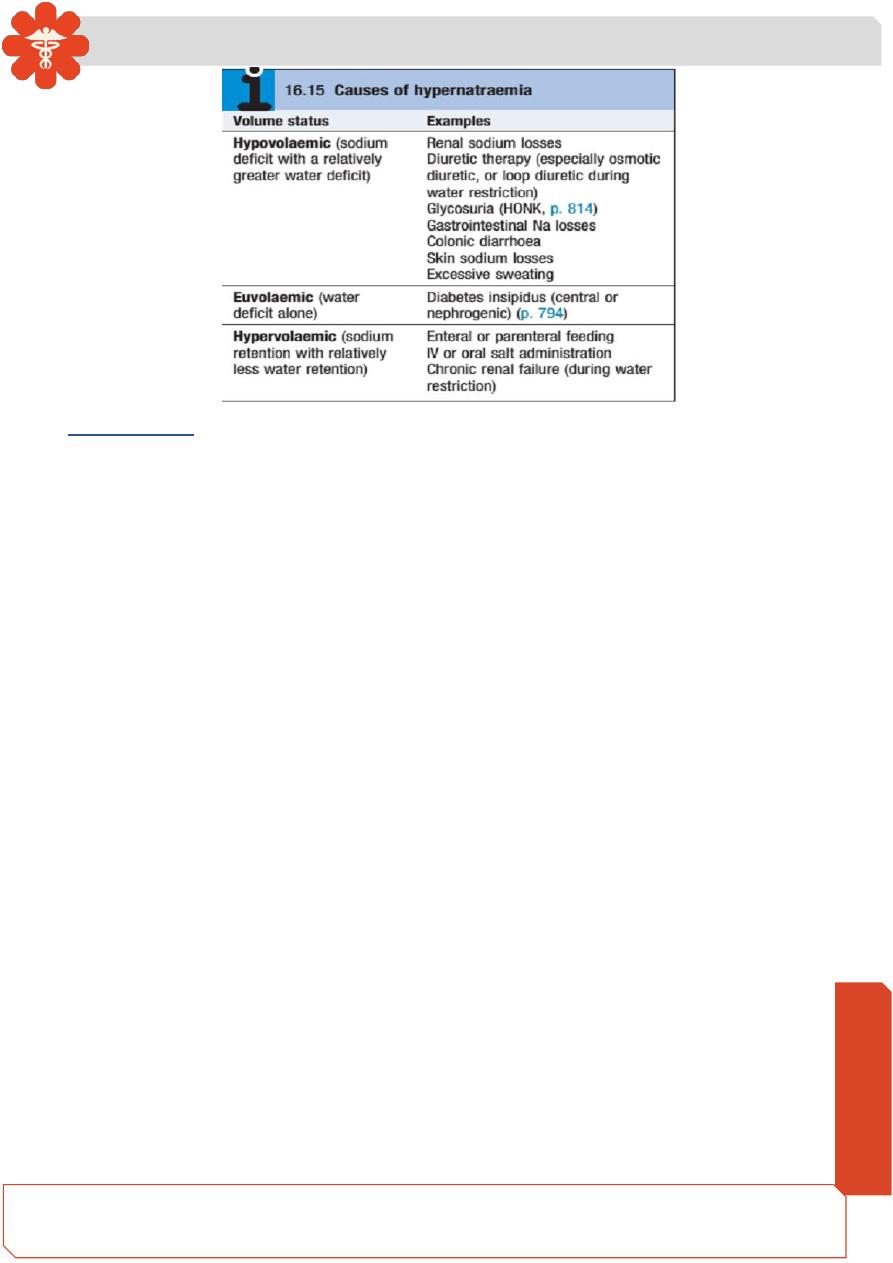
Hypernatraemia:
Aetiology and clinical assessment:
Just as hyponatraemia represents a failure of the mechanisms for diluting the urine during
free access to water, so hypernatraemia (plasma Na >148 mmol/L) reflects inadequate
concentration of the urine in the face of restricted water intake.
Patients with hypernatraemia generally have reduced cerebral function, either as a
primary problem or as a consequence of the hypernatraemia itself, which results in
dehydration of neurons and brain shrinkage. In the presence of an intact thirst mechanism
and preserved capacity to obtain and ingest water, hypernatraemia may not progress very
far. If adequate water is not obtained, dizziness, confusion, weakness and ultimately coma
and death can result.
Medicine
Notes…
6
Management:
Treatment of hypernatraemia depends on both the rate of development and the underlying
cause.
If there is reason to think that the condition has developed rapidly, neuronal shrinkage
may be acute and relatively rapid correction may be attempted. This can be achieved by
infusing an appropriate volume of intravenous fluid (isotonic 5% dextrose or hypotonic
0.45% saline) at an initial rate of 50
–70 mL/hour. However, in older, institutionalised
patients it is more likely that the disorder has developed slowly, and extreme caution
should be exercised in lowering plasma sodium to avoid the risk of cerebral oedema.
Where possible, the underlying cause should also be addressed.
