
ORAL HISTOLOGY and
EMBRYOLOGY COURSE

ORAL HISTOLOGY AND EMBRYOLOGY
COURSES
• Oral Histology and Embryology Practical lectures
will be every Monday at 01:30 in Biology and
Histology lab.
• Oral Histology and Embryology Theoretical Lectures
will be every Monday at 09:00 in Dentistry Hall.
• Lecturer: Dr. Duran Kala
• Lab assistant: Rojan Arif

Exams and Grades:
• In Histology and Embryology courses There will be:
• - Midterm practical exams = 10%
• - Lab Manuals = 10 %
• - Theoretical Midterm exams = 30%
• - Final Practical exam = 10%
• - Final Theoretical exam = 40%
• - Total = 100%

CHAPTERS
• 1-TOOTH DEVELOPMENT AND GROWTH
• 2-ENAMEL
• 3-DENTIN
• 4-CEMENTUM
• 5-PULP
• 6-PDL
• 7-EMBRYOLOGY
• 8-MANDIBLE
• 9-MAXILLA
• 10-BONE TISSUE TYPES
• 11-ALVEOLAR PROCESS
• 12-ORAL MUCOSA-SALIVARY GLANDS

•Histology is the study of anatomy
that deals with the minute
structure, composition, and
functions of tissues. Oral histology
describes in detail the tissues of the
teeth, periodontium, and the
surrounding oral mucosa.
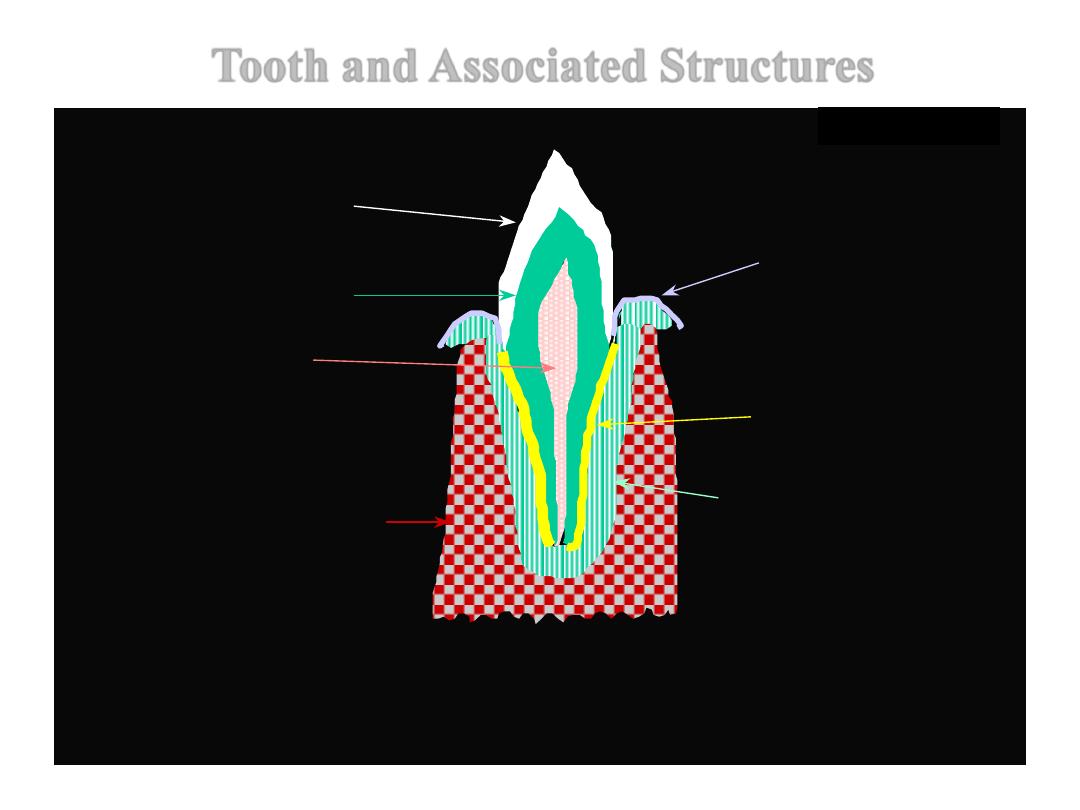
TOOTH & RELATED TISSUES: Developmental goal
PULP
DENTINE
ENAMEL
CEMENTUM
PERIODONTAL
LIGAMENT/ PDL
ALVEOLAR BONE
GINGIVA
WABeresford
Tooth and Associated Structures
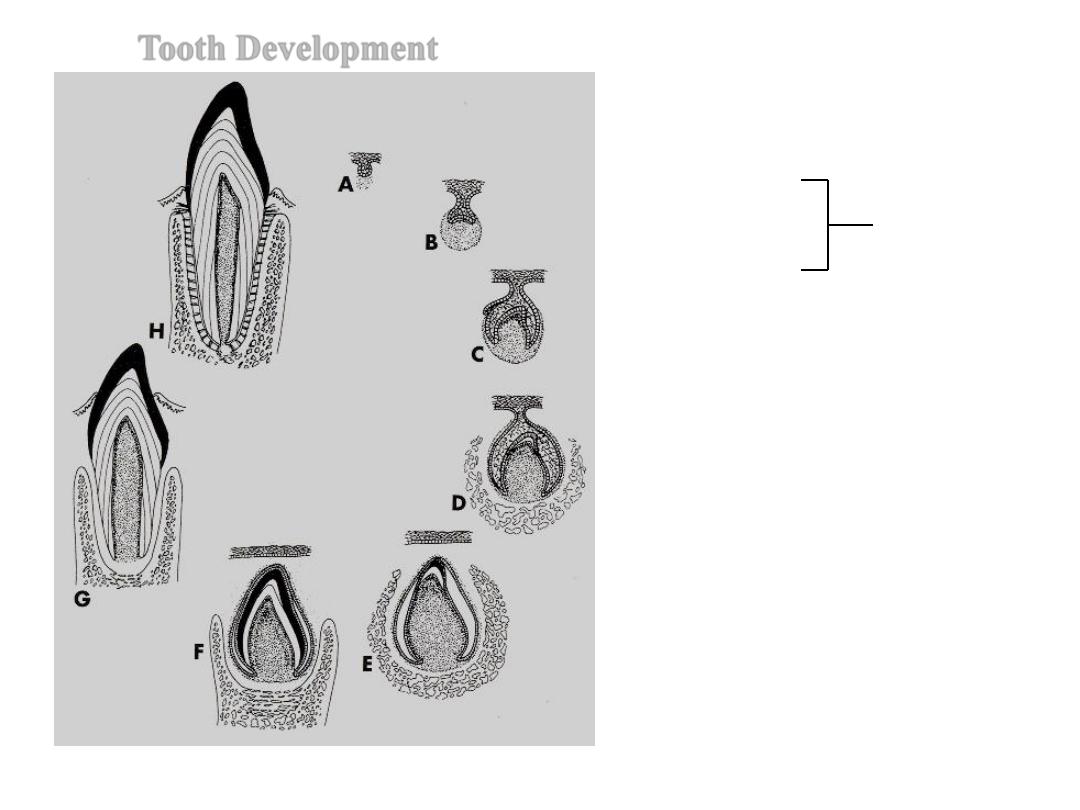
Tooth Development
A. Bud Stage
B. Cap Stage
C. Bell Stage
D and E. Dentinogenesis and
amelogenesis
F.
Crown formation
G. Root Formation and
eruption
H. Function
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
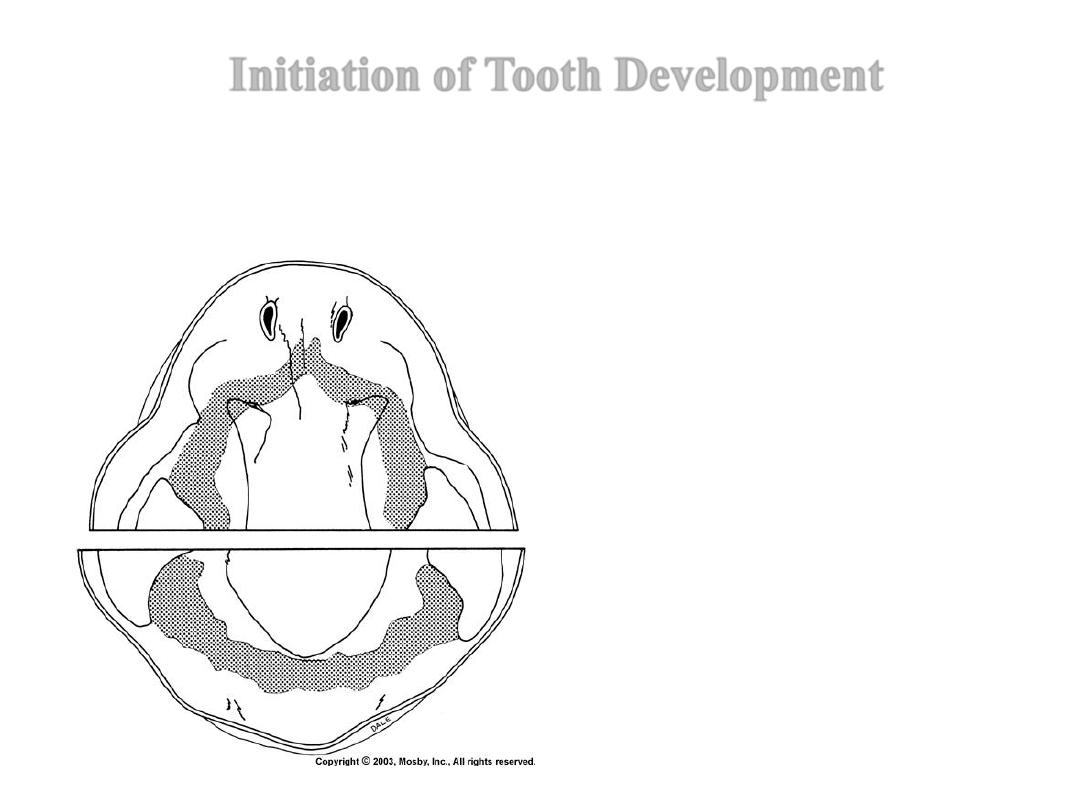
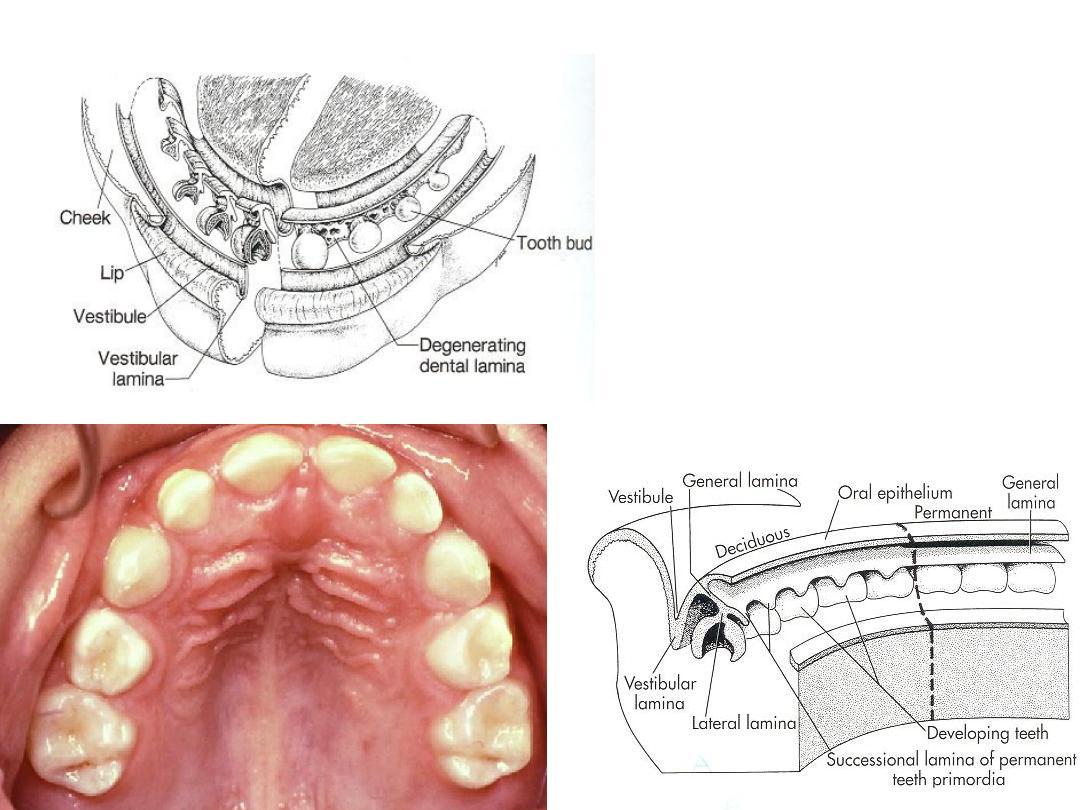
Initiation of Tooth Development
The initiation of tooth development begins at 37 days of development
with formation of a continuous horseshoe-band of thickened epithelium
in the location of upper and lower jaws – Primary Epithelial Band
Each band of epithelium will give
rise to 2 sub divisions:
1. Dental lamina and
2. Vestibular lamina
Responsible for
the formation of the vestibule (the
space bordered by the junction of the
gingiva and the tissue of the inner
cheek)
Figure from Ten Cate’s Oral Histology, Ed., Antonio Nanci, 6
th
edition
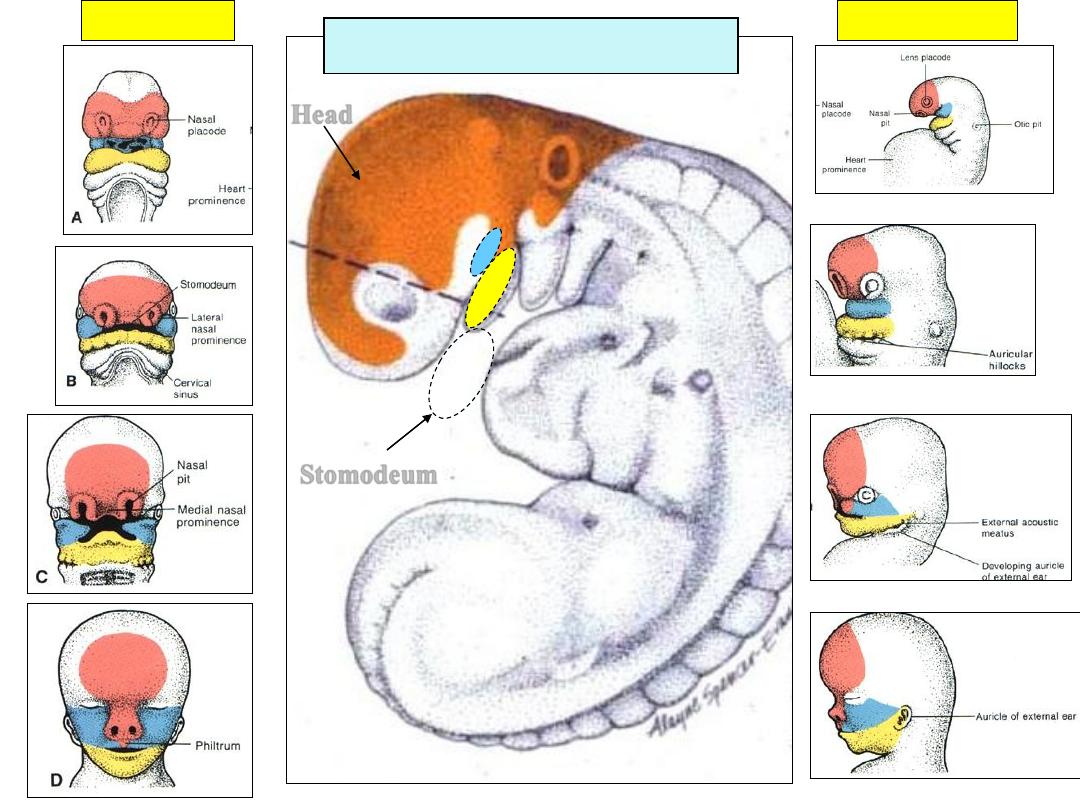
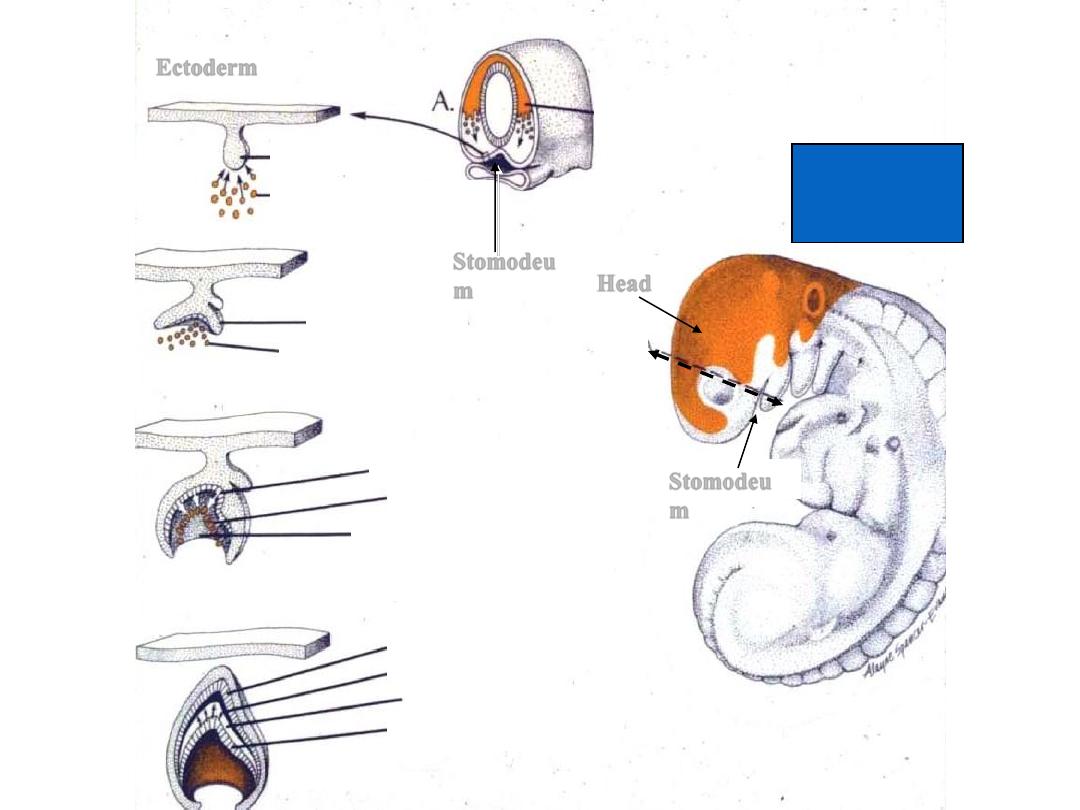
At 5-6 w.i.u. Embryo
Head
Stomodeum
Heart
Front view
Lateral view
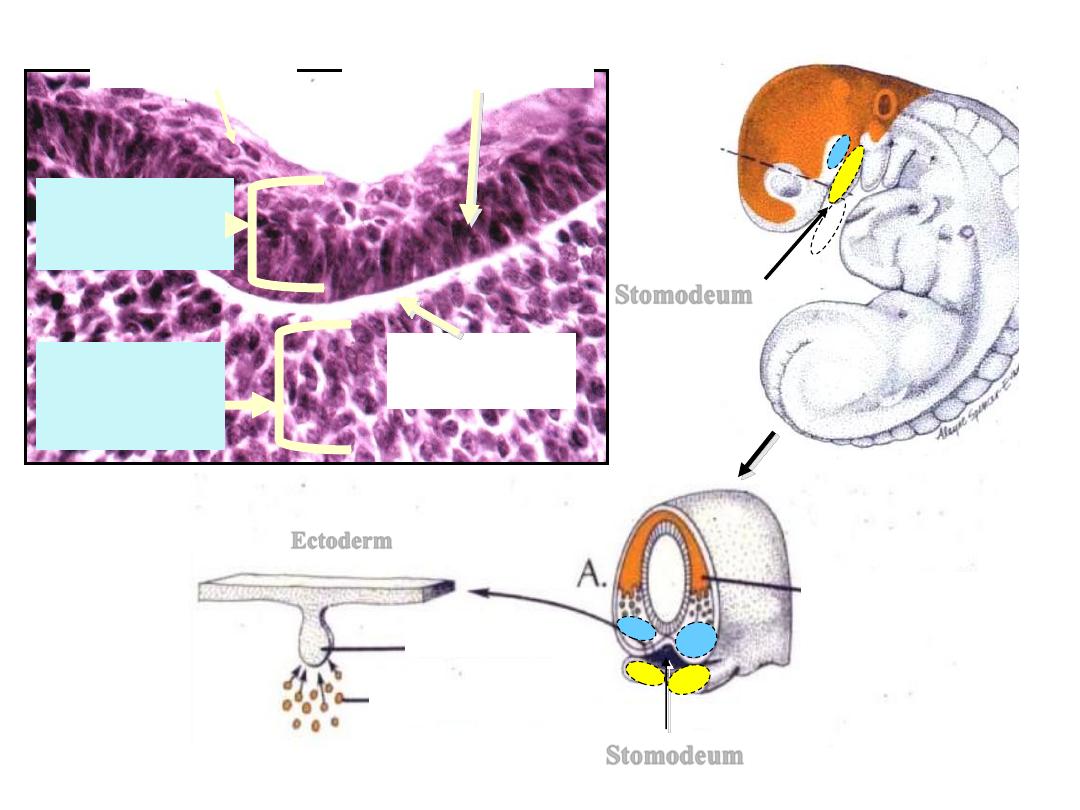
Stomodeum
Stomodeum
Ectoderm
Dental
lamina
Future dental
papilla
Neural Crest Cells
A
Flat cells
Columnar cells
Basement
membrane
MESODERM
Connective
tissue
ECTODERM
( S.SQ.E. )
Stomodeum
Developing Tongue
Dental lamina
Maxillary Process
Mandibular process
http://www.usc.edu/hsc/dental/ohisto/
Dental Lamina
• Dental lamina appears as a thickening
of the oral epithelium adjacent to
condensation of ectomesenchyme
• 20 areas of enlargement or knobs
appear, which will form tooth buds
for the 20 primary teeth
• Not all will appear at the same time.
The first to develop are those of the
anterior mandible region
• At this early stage the tooth buds
have already determined their crown
morphology
• Successional lamina: lamina from
which permanent teeth develop
• The dental lamina begins to function
at 6
th
prenatal week and continues to
15
th
year of birth (3
rd
molar)
Primary epithelial
band
Ectomesenchyme
Figures from: http://www.usc.edu/hsc/dental/ohisto/
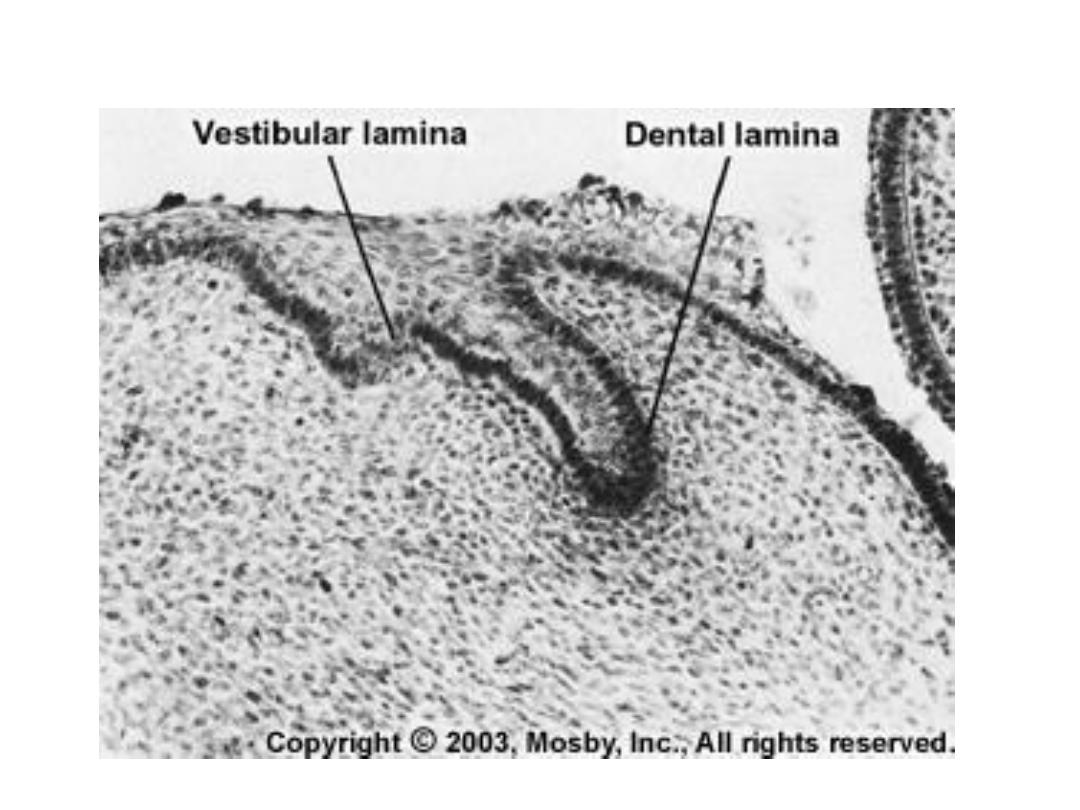
Vestibular Lamina
Figure from Ten Cate’s Oral Histology, Ed., Antonio Nanci, 6
th
edition
Ectomesenchyme (ek´tōmez´ nkīm),
n a mass of tissue consisting of neurocrest cells present
in the early formation of an embryo. It eventually forms
the hard and soft tissues of the neck and cranium.
Tooth development is a continuous process, however
can be divided into 3 stages:
1. Bud Stage
2. Cap Stage
3. Bell Stage
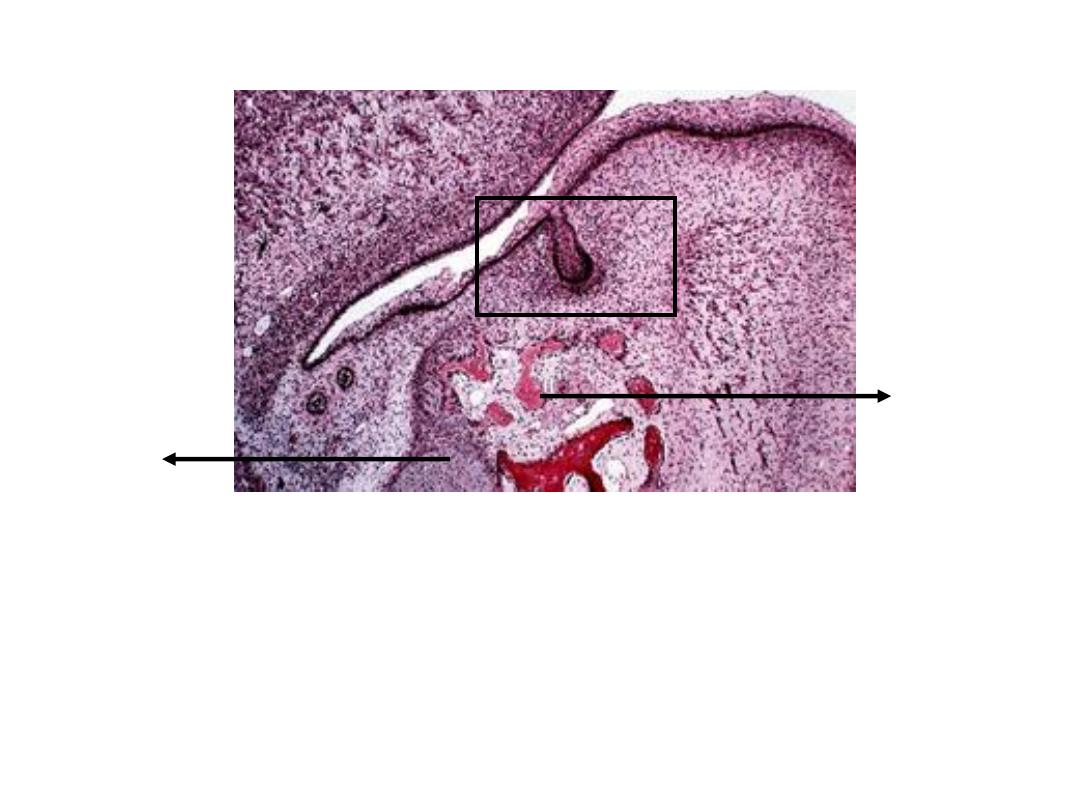
1. Bud Stage
•
Bud stage is characterized by rounded, localized growth of
epithelium surrounded by proliferating(reproducing rapidly )
mesenchymal cells which are packed closely beneath and
around the epithelial buds
Meckel’s
cartilage
Intramembranous
ossification
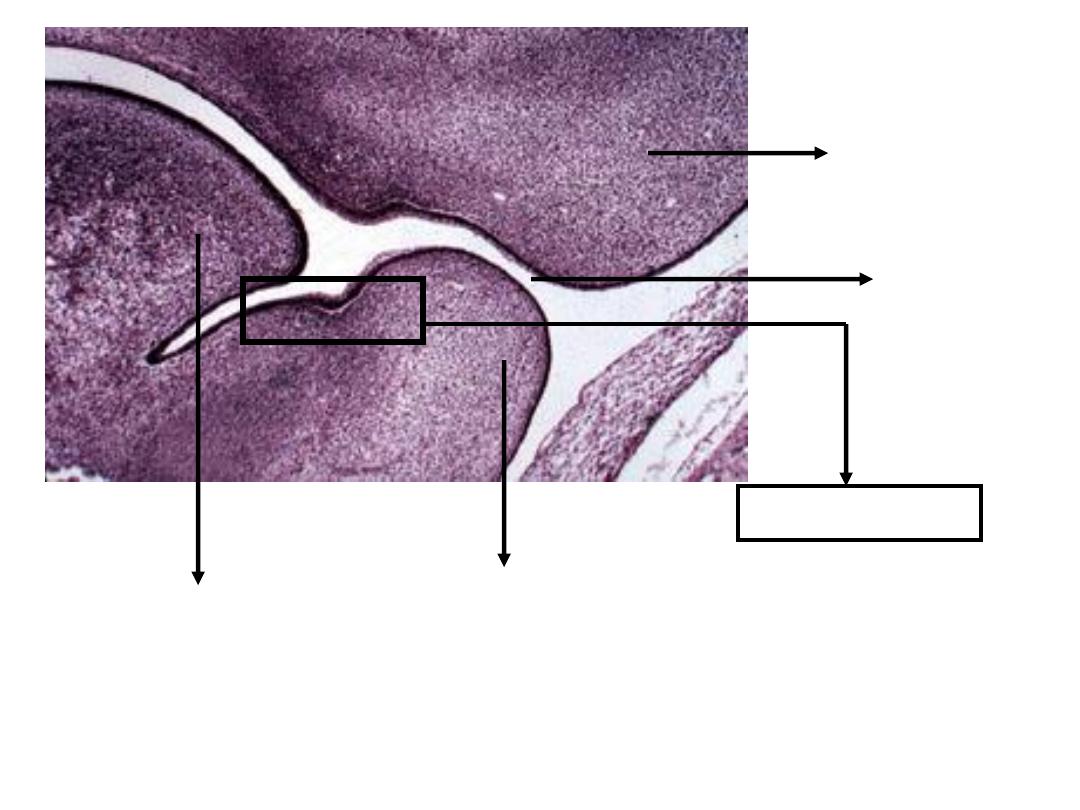
1. Bud Stage
In the bud stage, the enamel organ consists of
peripherally located low columnar cells and centrally
located polygonal cells
http://www.usc.edu/hsc/dental/ohisto/
2. Cap Stage
Vestibular lamina
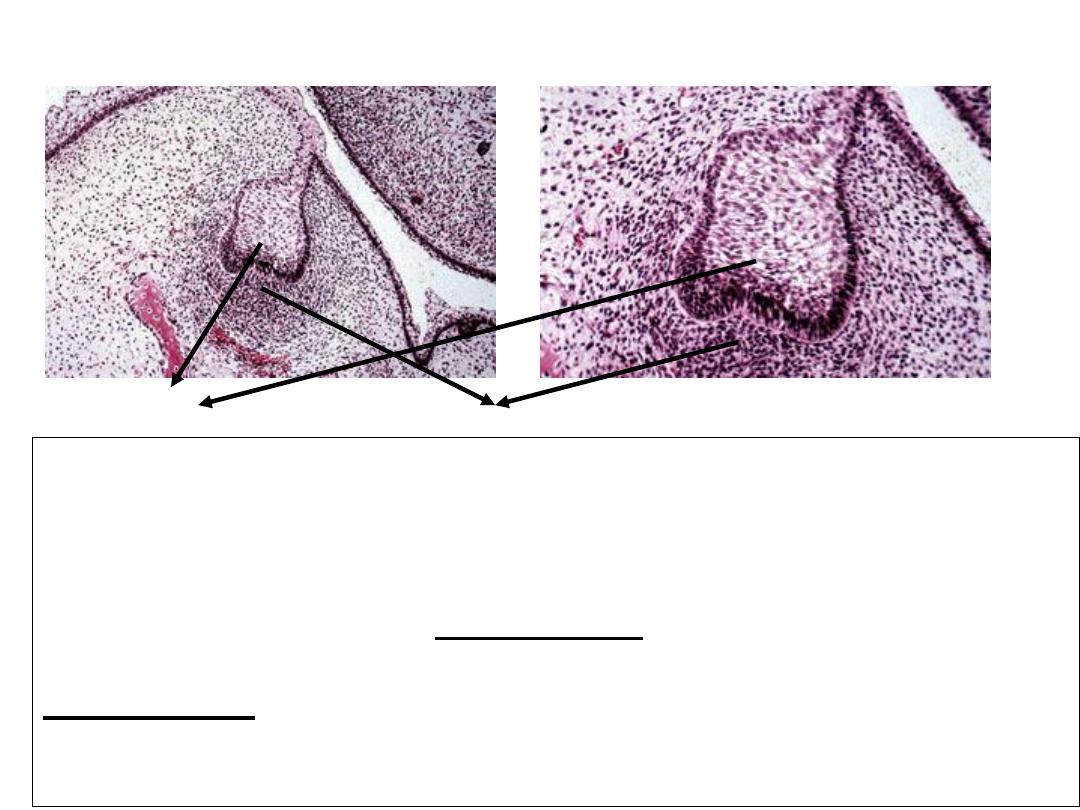
2. Cap Stage
Condensation of the ectomesenchyme immediately subjacent to the tooth
bud caused by lack of extracellular matrix secretion by the cells thus
preventing separation. Histodifferentiation begins at the end of cap
stage.
Epithelial outgrowth called Enamel Organ because it will eventually
form the enamel
Dental Papilla: Ball of condensed ectomesenchymal cells (it will form
dentin and pulp). The peripheral cells adjacent to the inner dental
epithelium will enlarge and later differentiate into odontoblasts
Enamel Organ
Dental Papilla
http://www.usc.edu/hsc/dental/ohisto/
2. Cap Stage
Enamel organ
Dental papilla
Dental follicle or sac
Dental follicle or dental sac is the condensed ectomesenchymal tissue
surrounding the enamel organ and dental papilla. This gives rise to
cementum and the periodontal ligament
(support structures for tooth)
Enamel knot
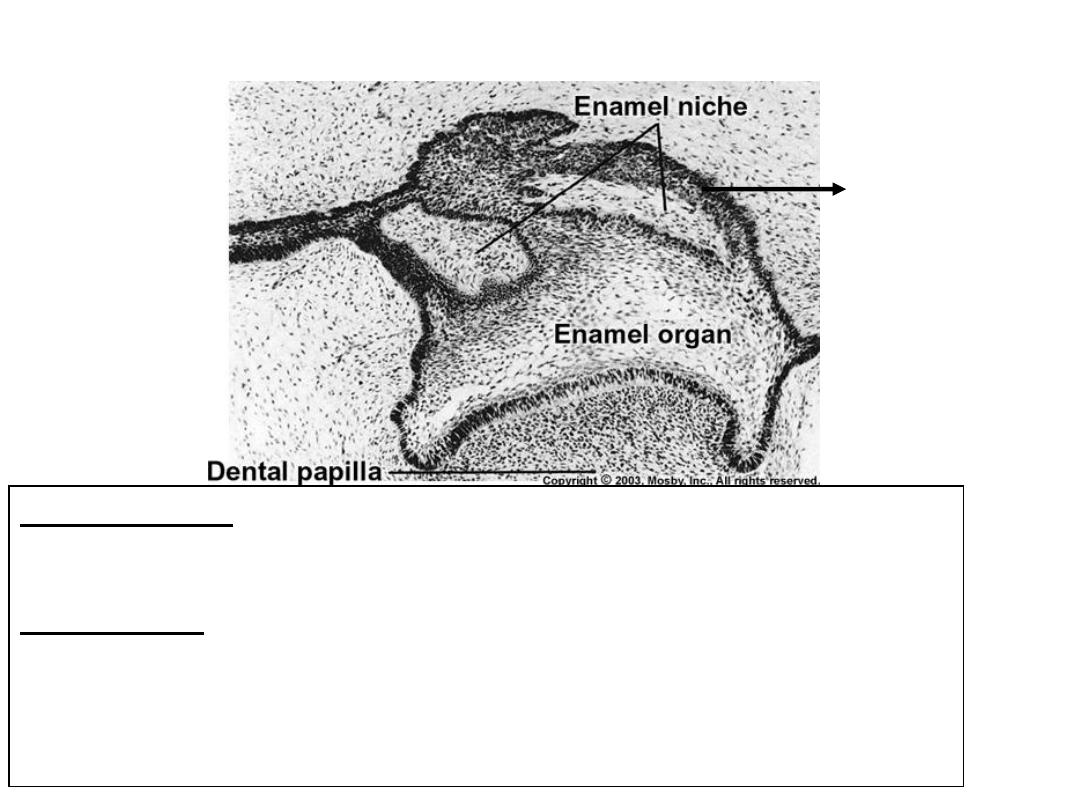
2. Cap Stage
Lateral Lamina: extension from the dental lamina that is connected
to the enamel organ
Enamel niche: It is an artifact produced during sectioning of the tissue.
It occurs because the enamel organ is a sheet of proliferating cells rather
than a single strand and contains a concavity filled with ectomesenchyme
Lateral lamina
Dental organ or tooth germ is a term used to constitute the structure that has
enamel organ, dental papilla and dental follicle
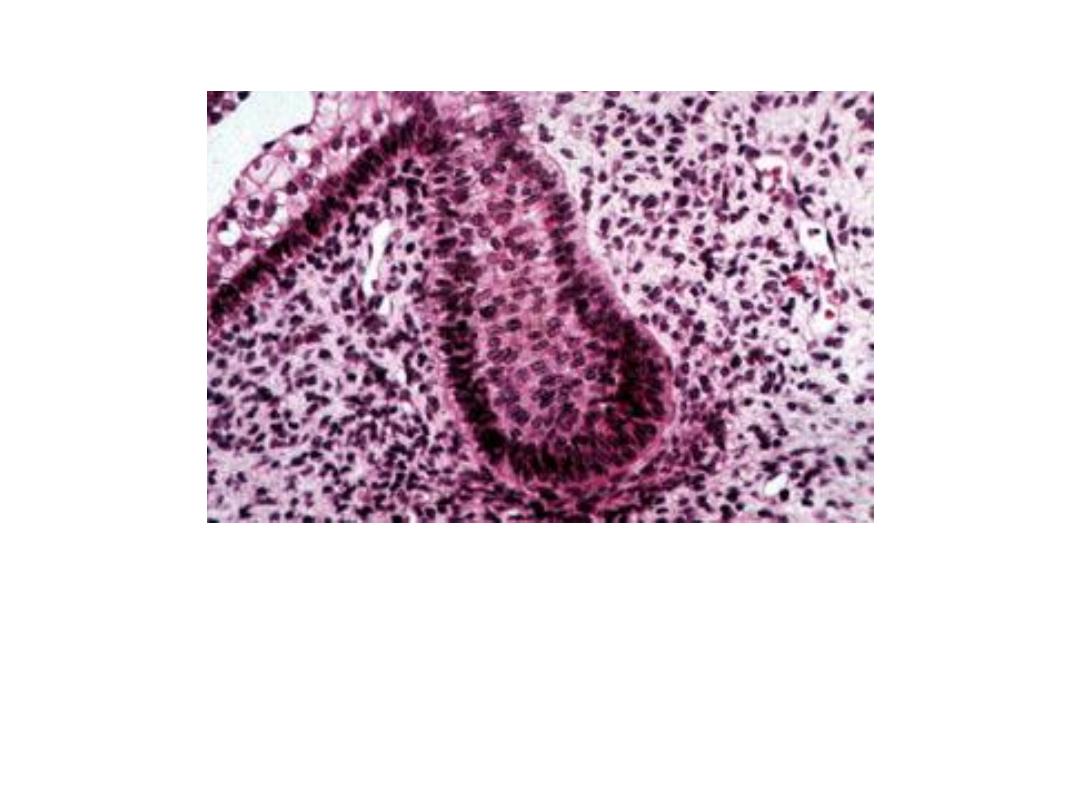
Enamel Knot: Densely packed accumulation of cells projecting from the inner
enamel epithelium into dental papilla. Exact role not known, but currently
believed to be the organizational center for cusp development (a pointed
structure on a cuspid, premolar, or molar ).
CA
P
S
TA
GE
Cell Free Zone
Inner Enamel Epithelium
Enamel cord
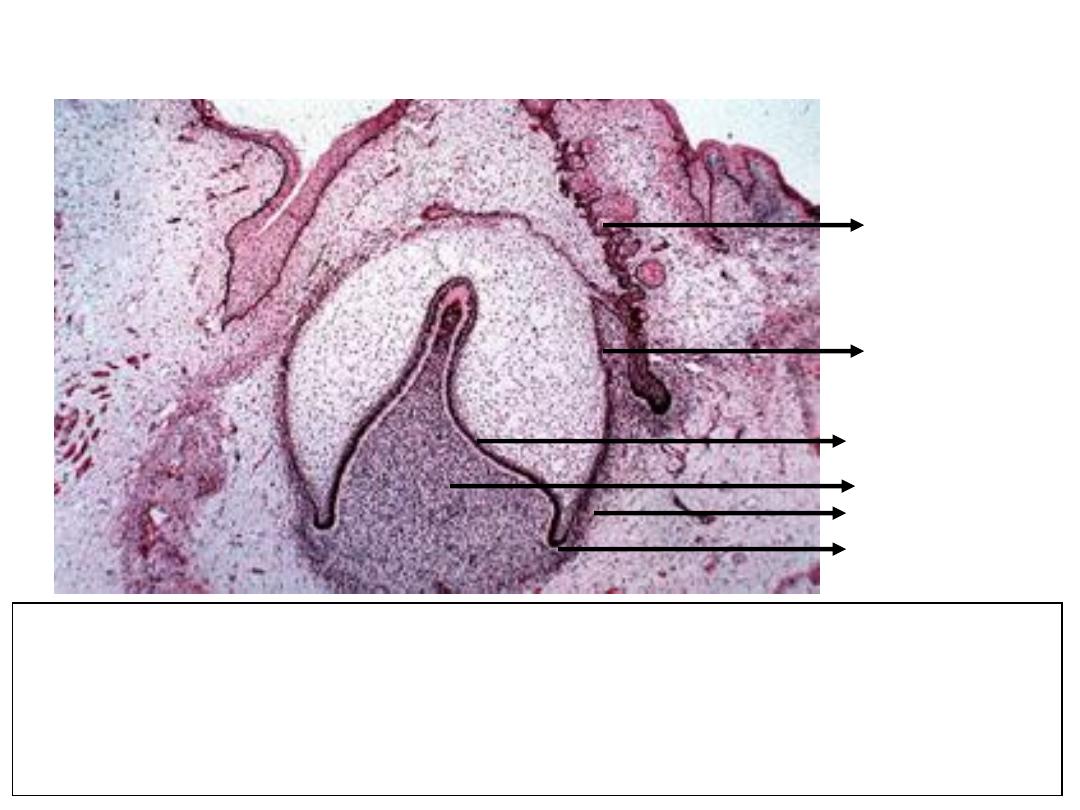
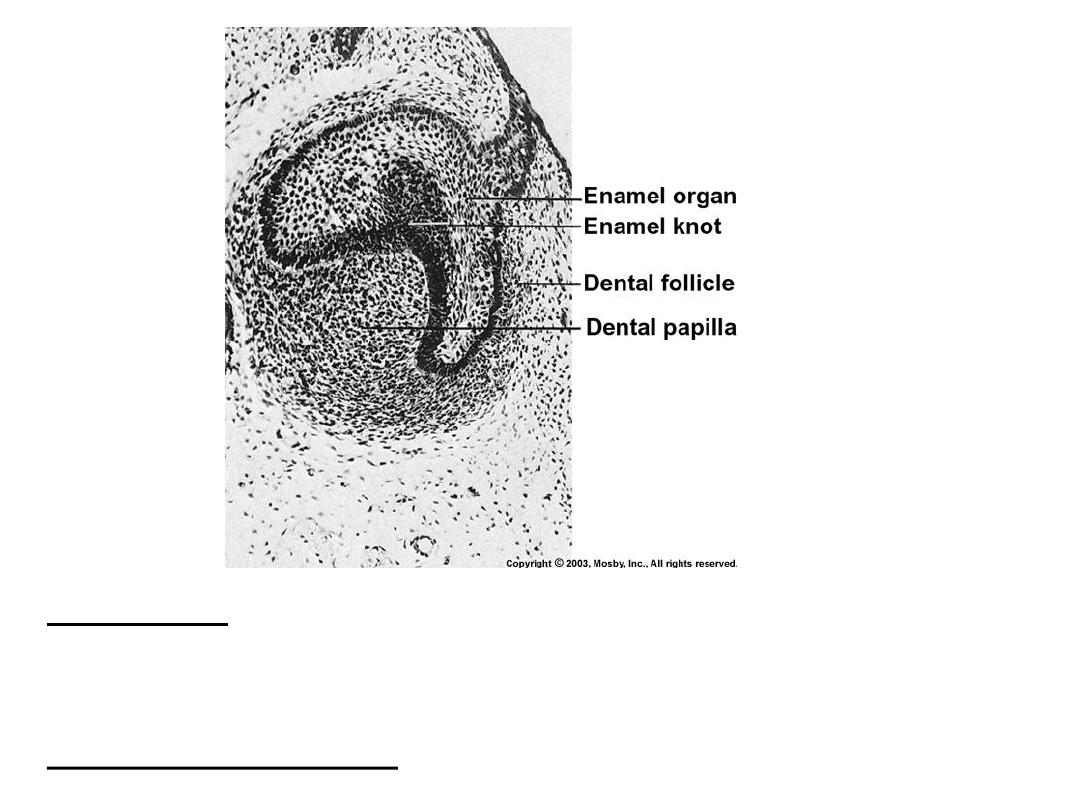
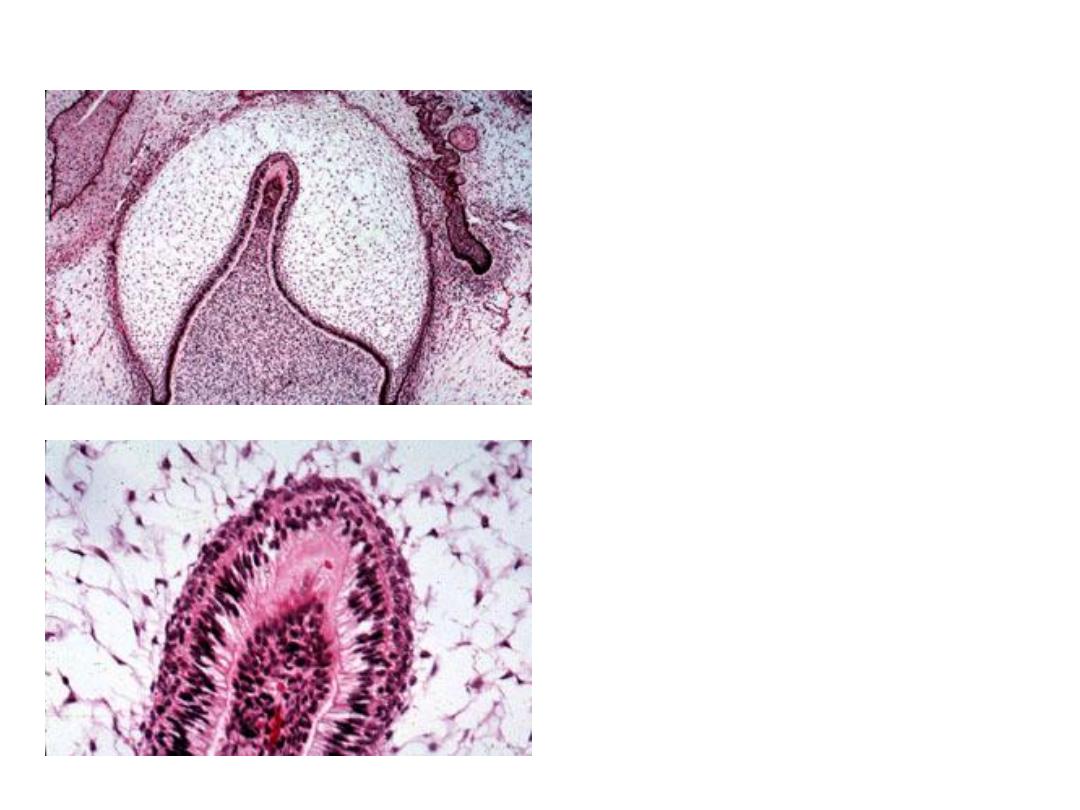
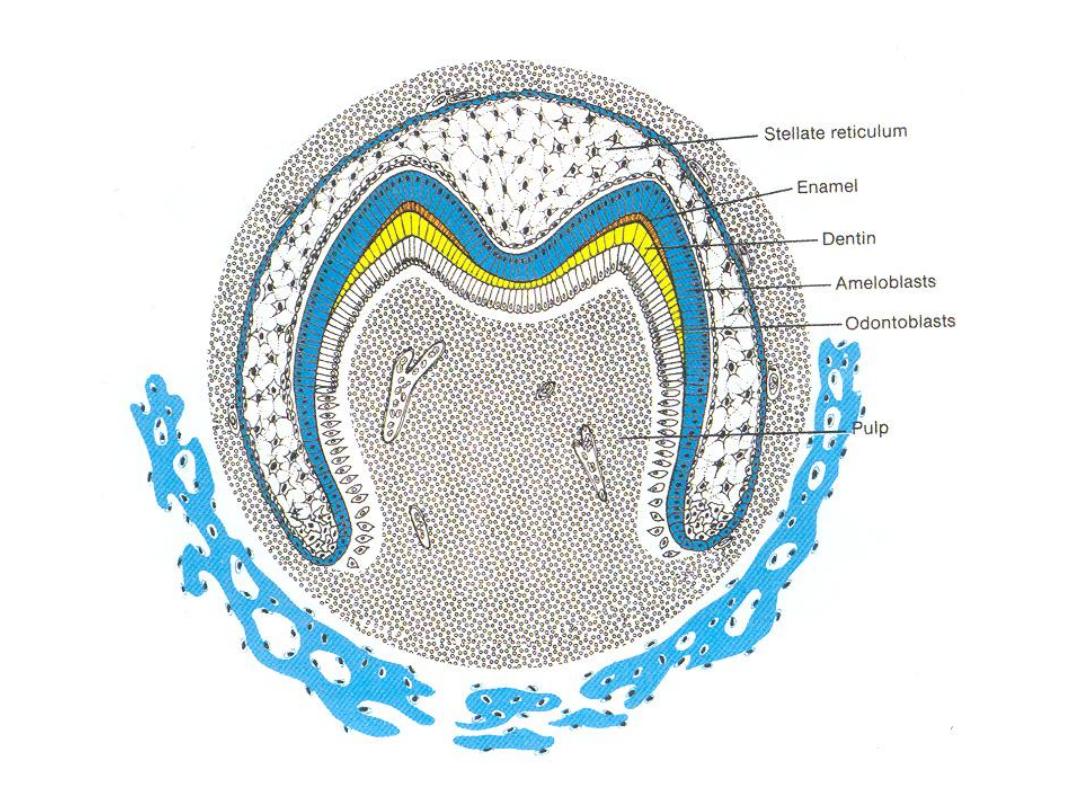
3. Bell Stage
• Continued growth leads to bell stage, where the enamel organ resembles a
bell with deepening of the epithelium over the dental papilla
• Continuation of histodifferentiation (ameloblasts and odontoblasts are defined)
and beginning of morphodifferentiation (tooth crown assumes its final shape)
Dental lamina
Outer dental
epithelium
Inner dental
epithelium
Dental papilla
Dental follicle
Cervical loop
http://www.usc.edu/hsc/dental/ohisto/
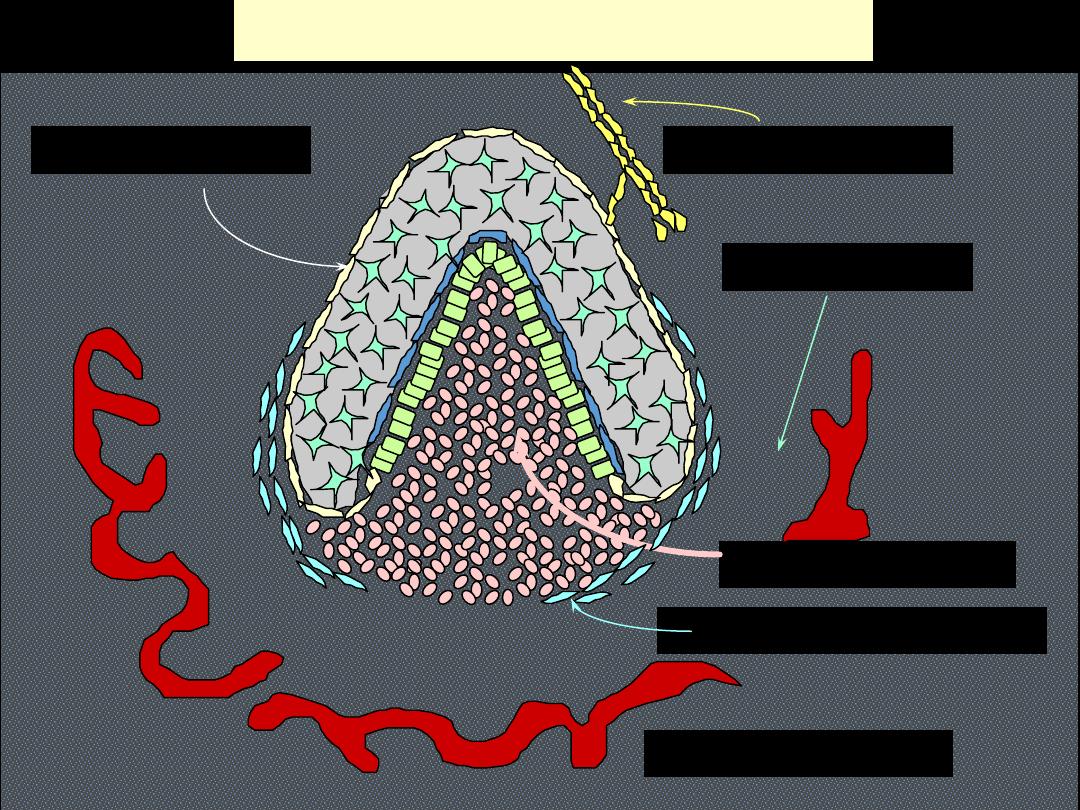
TOOTH PRIMORDIUM/GERM
DENTAL LAMINA
DENTAL PAPILLA
DENTAL SAC/FOLLICLE
DENTAL ORGAN
MESENCHYME
ALVEOLAR BONE
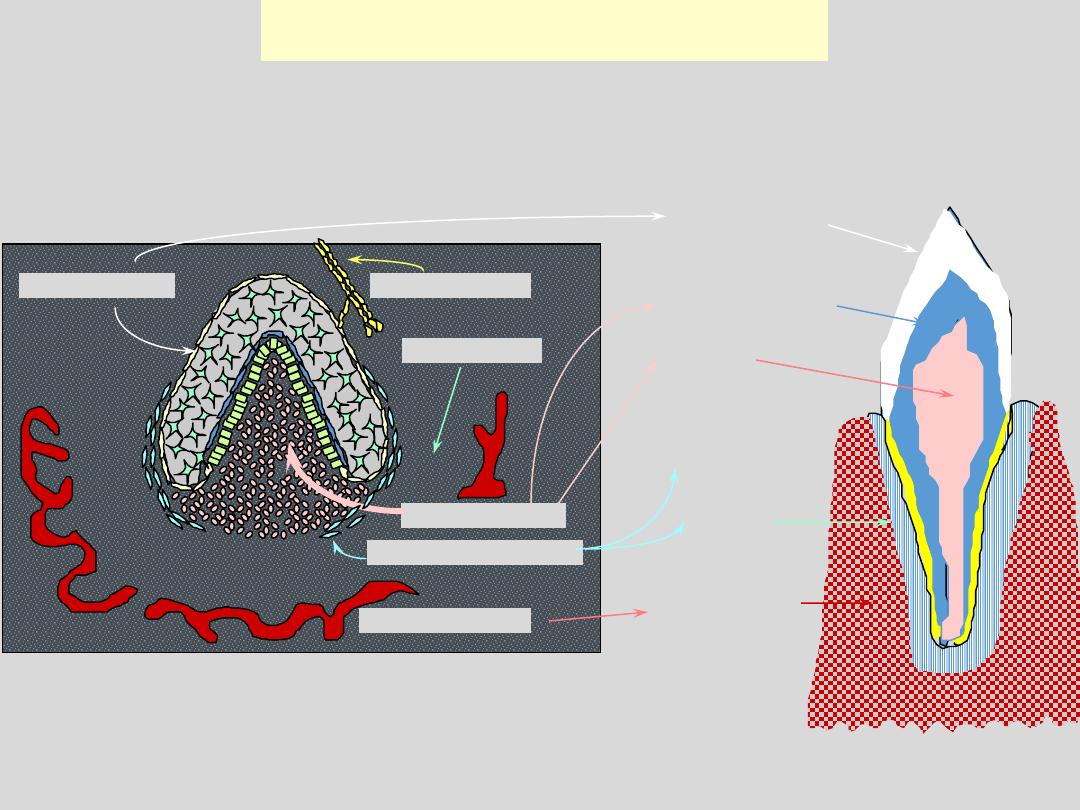
TOOTH TISSUES: Sources
DENTAL LAMINA
DENTAL PAPILLA
DENTAL SAC/FOLLICLE
DENTAL ORGAN
MESENCHYME
ALVEOLAR BONE
PULP
DENTINE
ENAMEL
CEMENTUM
PDL
A BONE
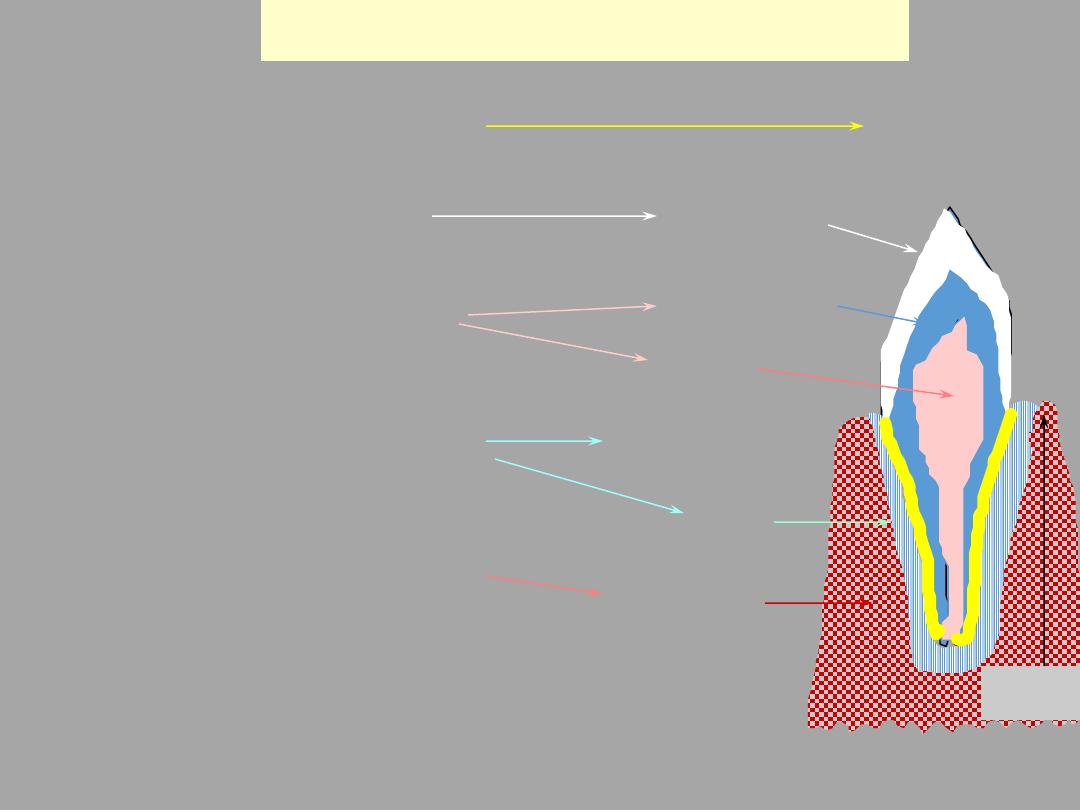
TOOTH TISSUES: Cell Sources
DENTAL LAMINA
DENTAL PAPILLA
DENTAL SAC/FOLLICLE
DENTAL ORGAN
ALVEOLAR BONE
PULP
DENTINE
ENAMEL
CEMENTUM
PDL
A BONE
TOOTH
Crest
Ameloblasts
Odontoblasts
CT cells
Cementoblasts
Fibroblasts
Osteoblasts & ‘clasts
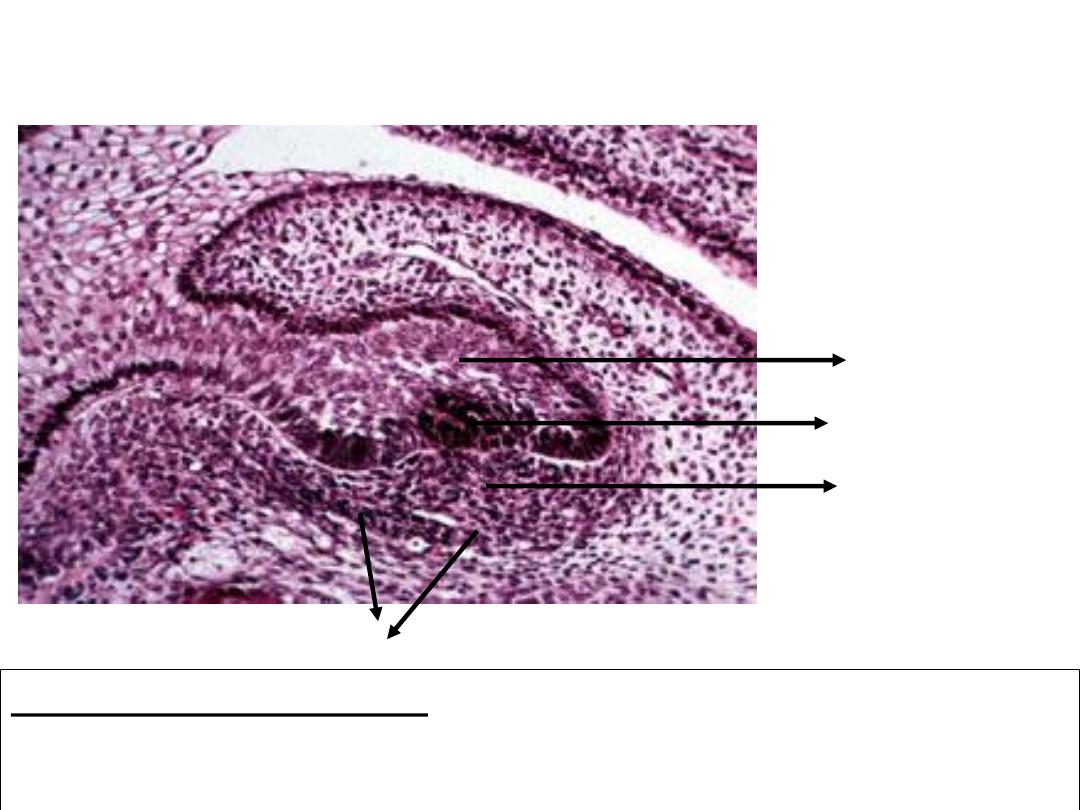
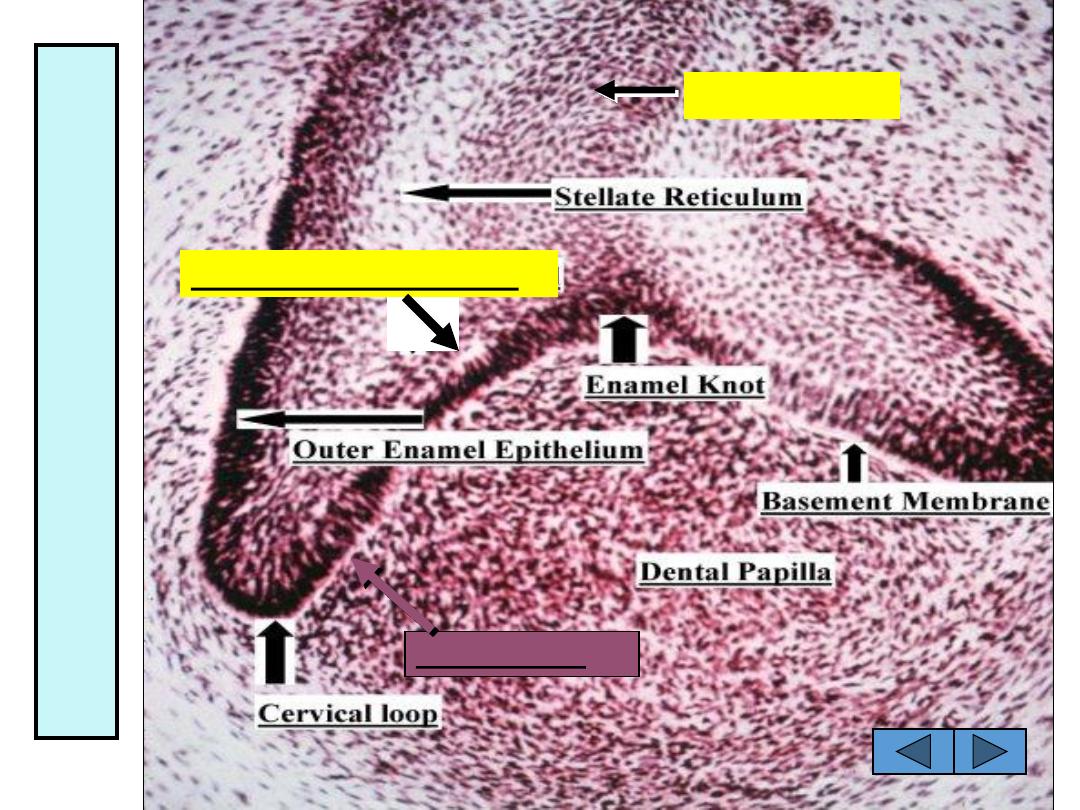
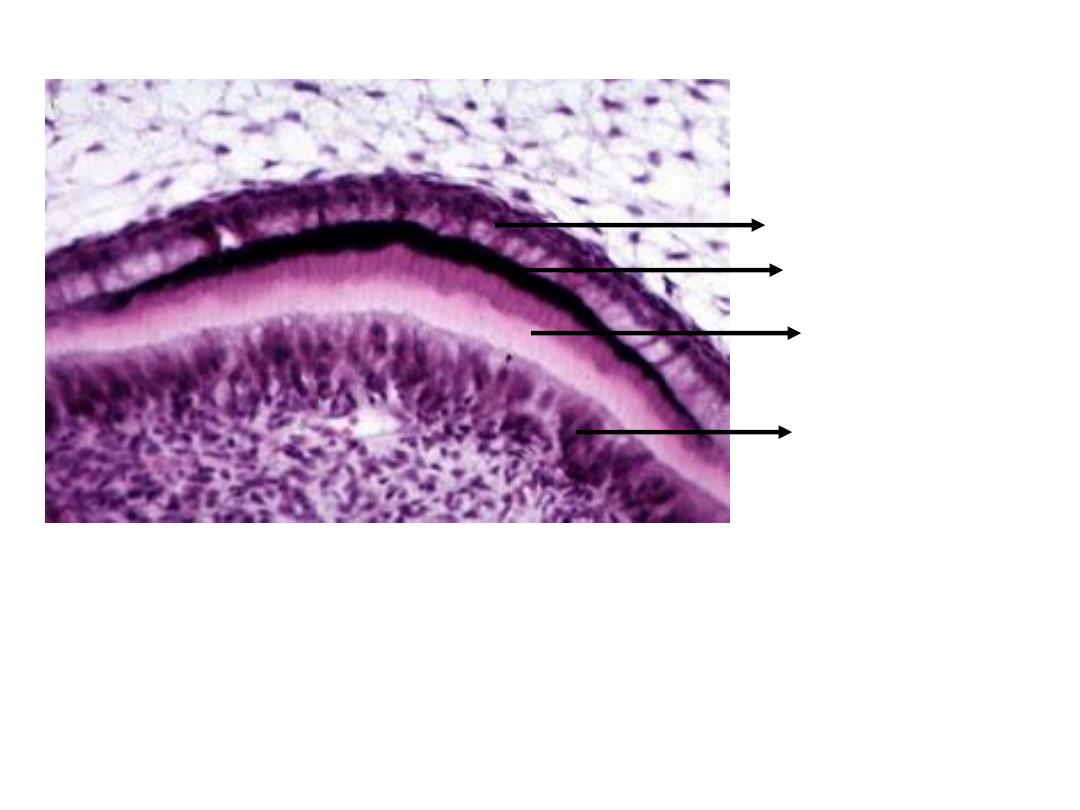
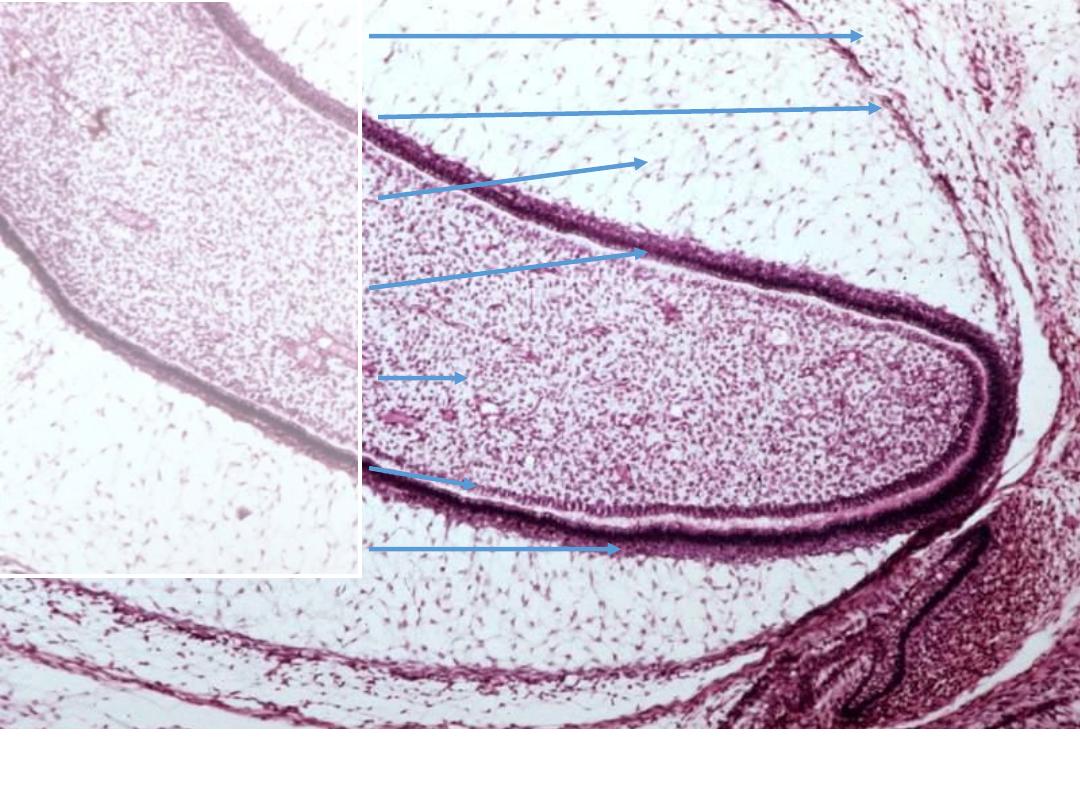
3. Bell Stage (Early)
Inner dental epithelium: Short columnar cells bordering the dental papilla.
These will eventually become ameloblasts that will form the enamel of the
tooth crown by differentiating into tall columnar cells. The cells of inner dental
epithelium exert an organizing influence on the underlying mesenchymal cells
in the dental papilla, which later differentiate into odontoblasts.
Outer dental epithelium: Cuboidal cells that cover the enamel organ. Their function is
to organize a network of capillaries that will bring nutrition to the ameloblasts. In
preparation to formation of enamel, at the end of bell stage, the formerly smooth surface
of the outer dental epithelium is laid in folds.
Stellate reticulum
Inner dental epithelium
Stratum intermedium
Dental papilla
Outer dental epithelium
http://www.usc.edu/hsc/dental/ohisto/
3. Bell Stage (Early)
Stellate reticulum
Inner dental epithelium
Stratum intermedium
Dental papilla
Stellate reticulum: Star-shaped cells with processes, present between the outer
and the inner dental epithelium. These cells secrete glycosaminoglycans,
which attract water, thereby swelling the cells and pushing them apart.
However, they still maintain contact with each other, thus becoming star-shaped.
They have a cushion-like consistency that may support and protect the delicate
enamel organ. It is absent in the portion that outlines the root portions.
Stratum intermedium: Cell layer between the inner dental epithelium and
stellate reticulum which have high alkaline phosphatase activity. They assist
inner dental epithelium (ameloblasts) to form enamel.
Outer dental epithelium
http://www.usc.edu/hsc/dental/ohisto/
Stellate reticulum
Inner dental epithelium
Stratum intermedium
Dental papilla
Outer dental epithelium
Dental Papilla: Before the inner dental epithelium begins to produce enamel,
the peripheral cells of the mesenchymal dental papilla differentiate into
odontoblasts under the organizing influence of the epithelium. First, they assume
a cuboidal shape and then a columnar form and acquire the specific potential to
produce dentin.
http://www.usc.edu/hsc/dental/ohisto/
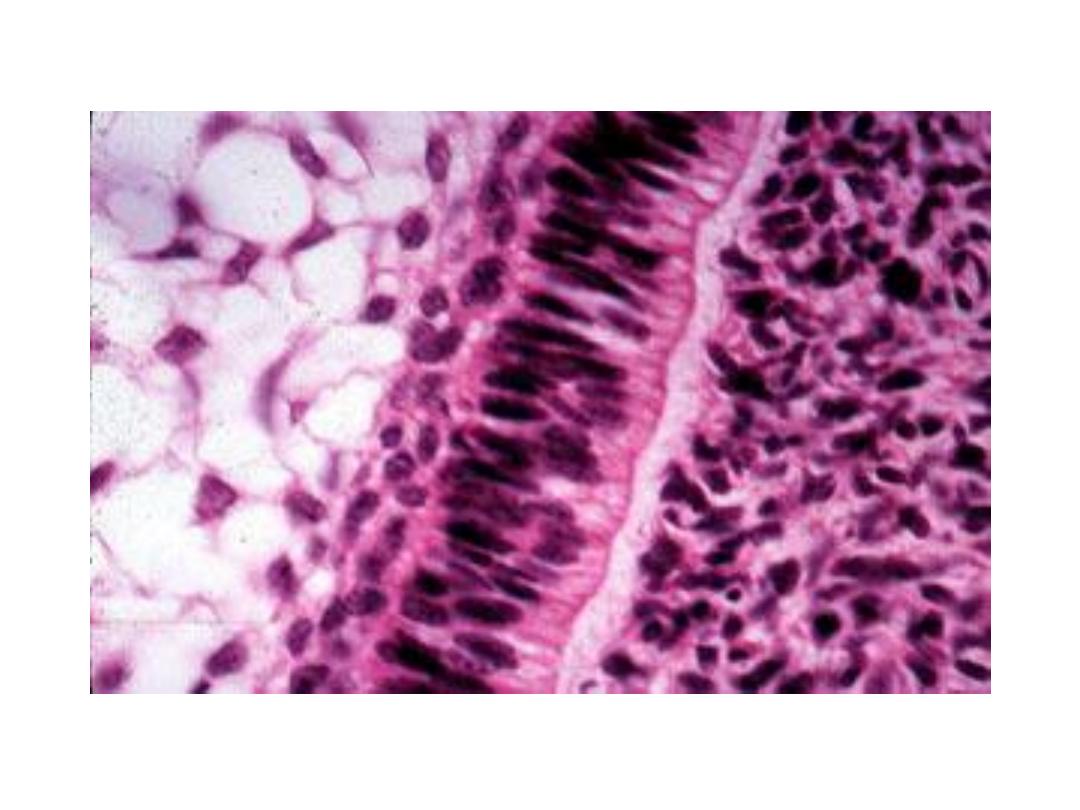
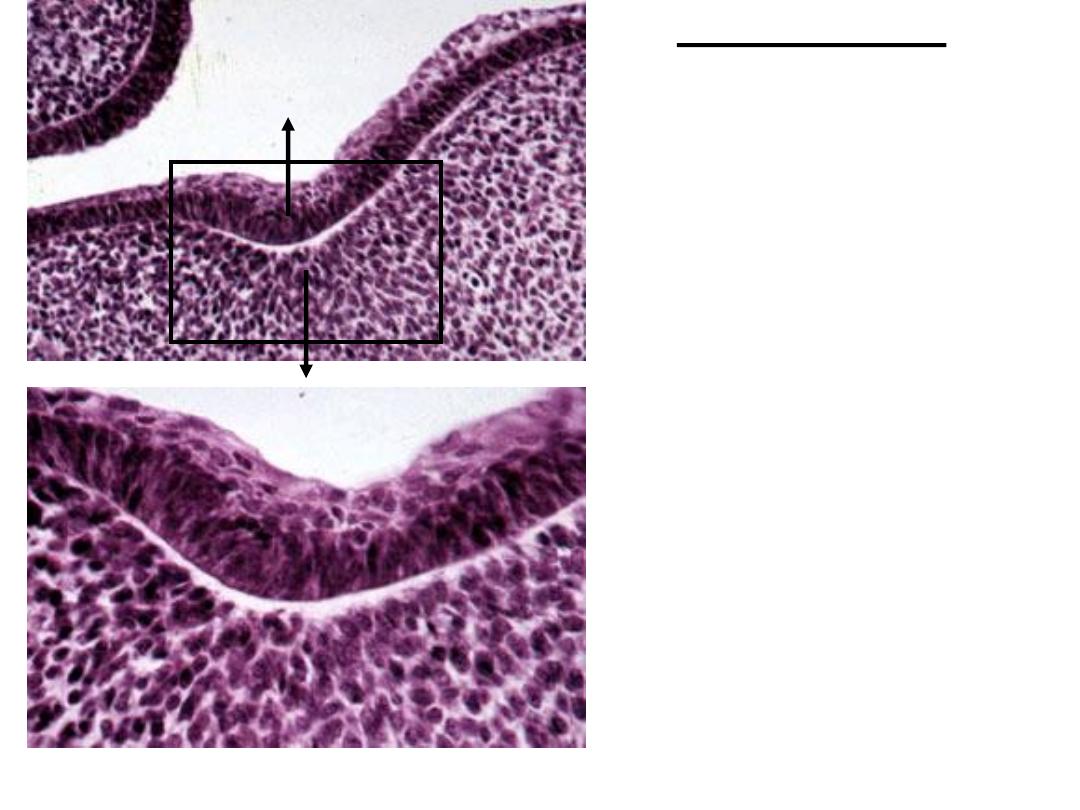
3. Bell Stage
Higher power view
http://www.usc.edu/hsc/dental/ohisto/
Inner dental epithelium
Outer dental epithelium
Cervical loop
Cervical loop: Area where the inner and the outer dental epithelium meet at
the edge of the enamel organ. This point is where the cells will continue to
divide until the tooth crown attains its full size and which after crown
formation will give rise to the epithelium for root formation. Is also called
“Zone of Reflexion”.
3. Bell Stage
http://www.usc.edu/hsc/dental/ohisto/
Enamel cord
Enamel cord: Pattern of enamel knot that extends between the inner and
outer dental epithelium
Enamel knot
3. Bell Stage
http://www.usc.edu/hsc/dental/ohisto/
SUCCESSIONAL LAMINA:
lamina from which permanent teeth develop
Neural Crest Cells
Ectoderm
Dental
lamina
Future dental
papilla
Dental organ
Dental papilla
Dental papilla
Ameloblasts
Differentiating
odontoblasts
Odontoblasts
New ameloblasts
New enamel
Denti
n
5-6 w.i.u.
embryo
Head
Stomodeu
m
A
Stomodeu
m
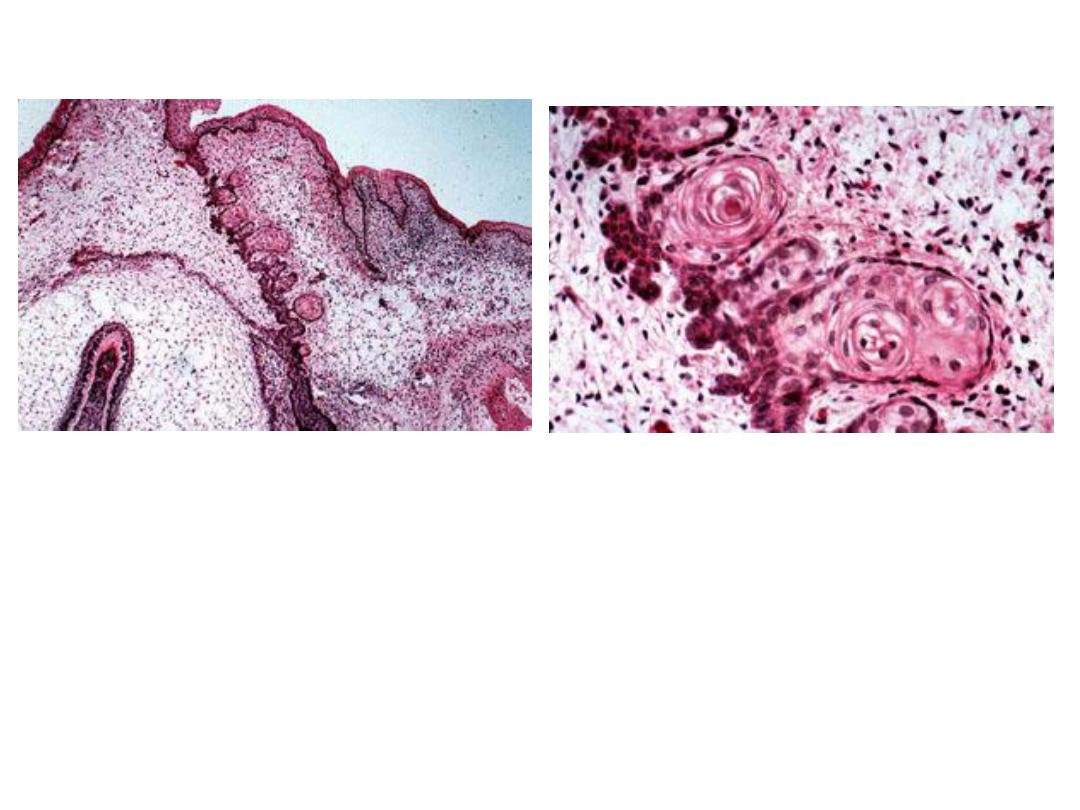
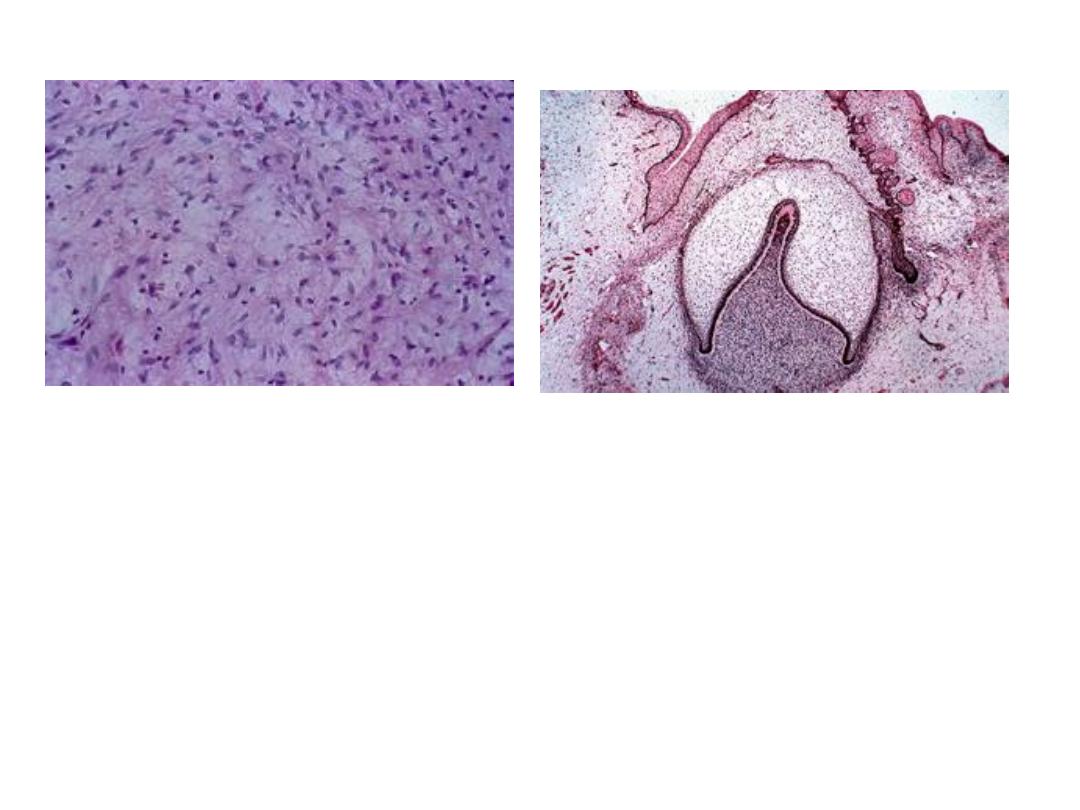
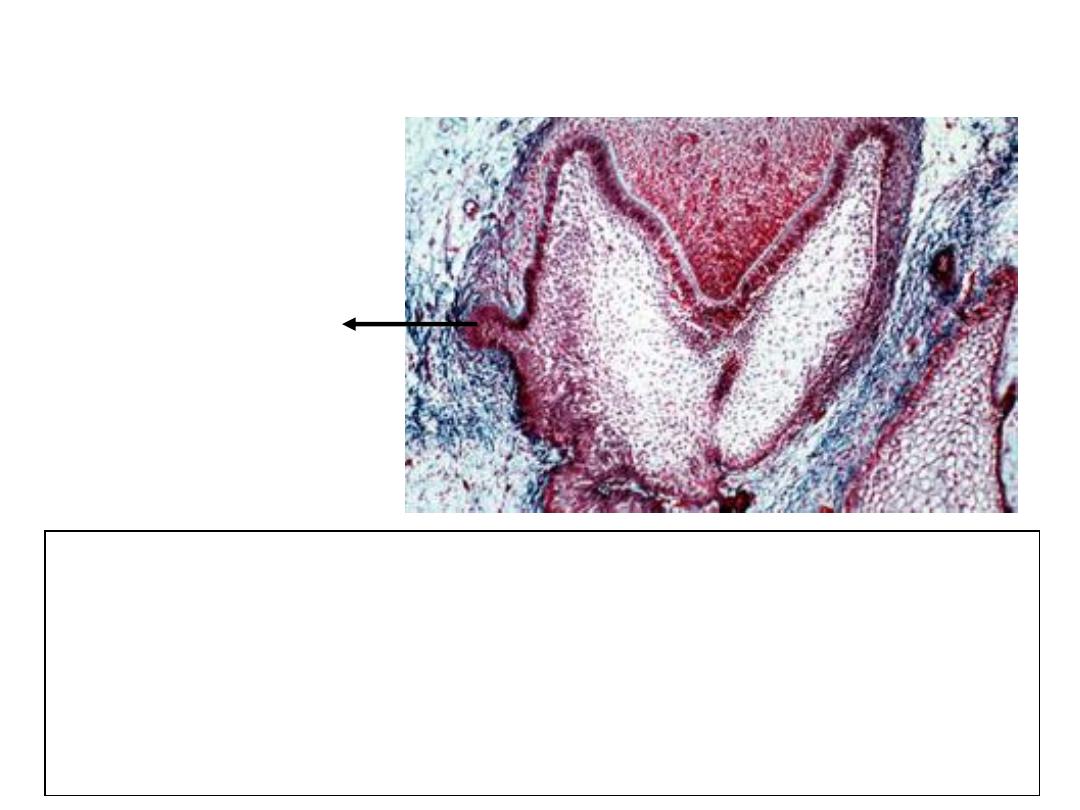
3. Bell Stage
Dental lamina (and the lateral lamina) will disintegrate and loose contact
with oral epithelium. Sometimes, these epithelial cells will persist when
they are called “epithelial pearls” or “cell rests of Serre”
Clinical significance: Cysts will develop in these (eruption cysts) and prevent
eruption, or they may form odontomas (tumors) or may form supernumery
teeth
http://www.usc.edu/hsc/dental/ohisto/

Eruption Cyst
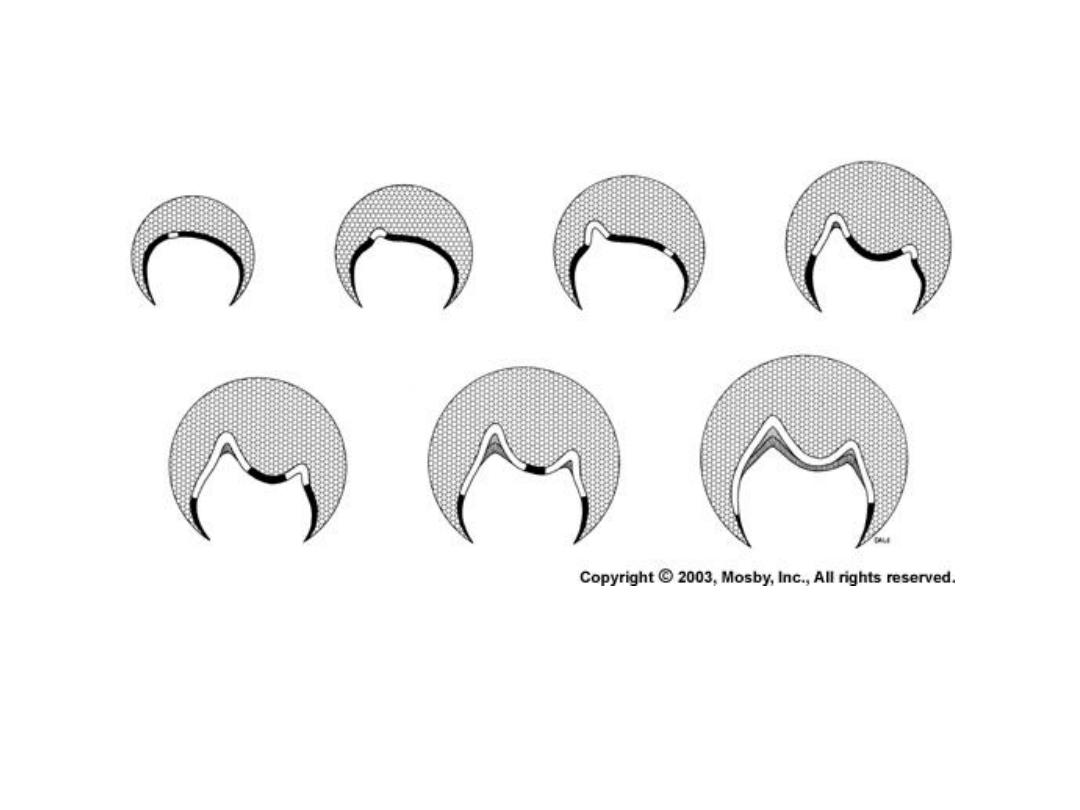
Future crown patterning also occurs in the bell stage, by folding of the
inner dental epithelium. Cessation(stopping) of mitotic activity within the inner
dental epithelium determines the shape of a tooth.
Crown Pattern Determination
Vascular and Nerve Supply during Tooth Development
Vascular Supply: Clusters of blood vessels in dental follicle and papilla
Clustering of vessels in papilla coincide with position
of root formation
Enamel organ is avascular, however vessels seen in
close association in the follicle
Nerve Supply: Initially noted in the dental follicle during bud to cap stage
However after start of dentinogenesis, seen in dental papilla
Nerve fibers do not enter enamel organ

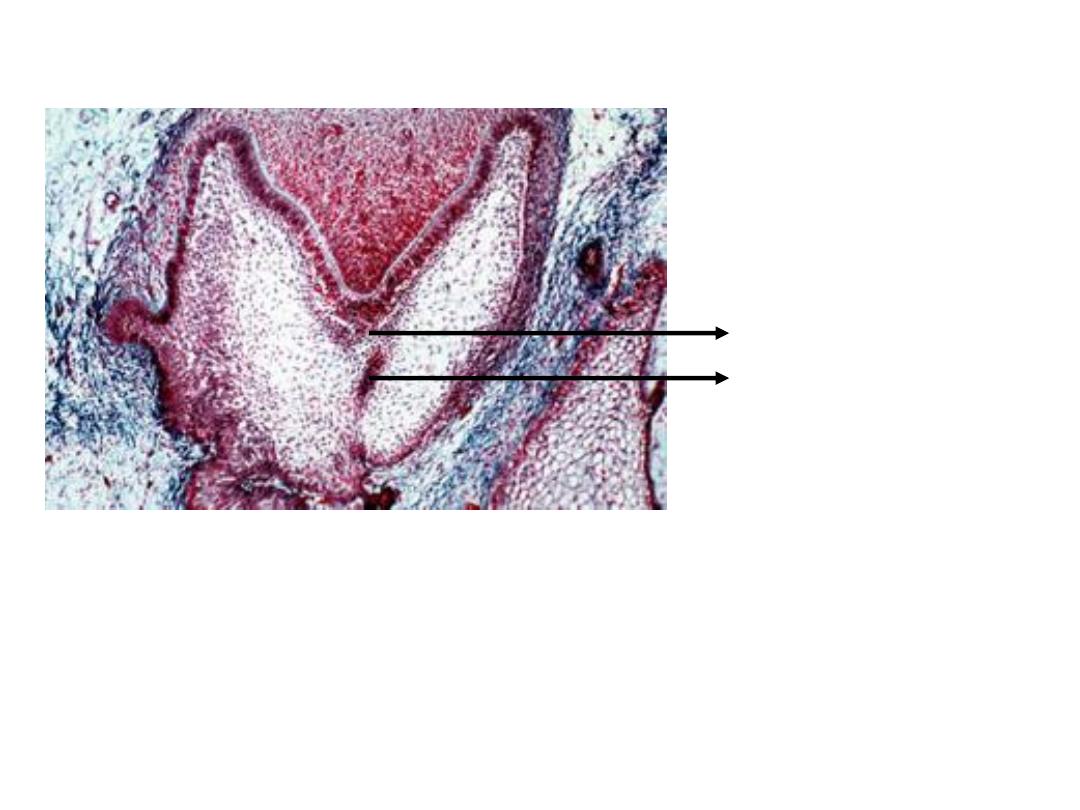
Clinical Correlation. Several odontogenic cysts and tumors can arise
from developing tooth structures. Two such conditions are:
1.
Ameloblastoma – which are tumors of odontogenic epithelium that
may arise from cell rests of enamel organ or from the developing
enamel organ among other things
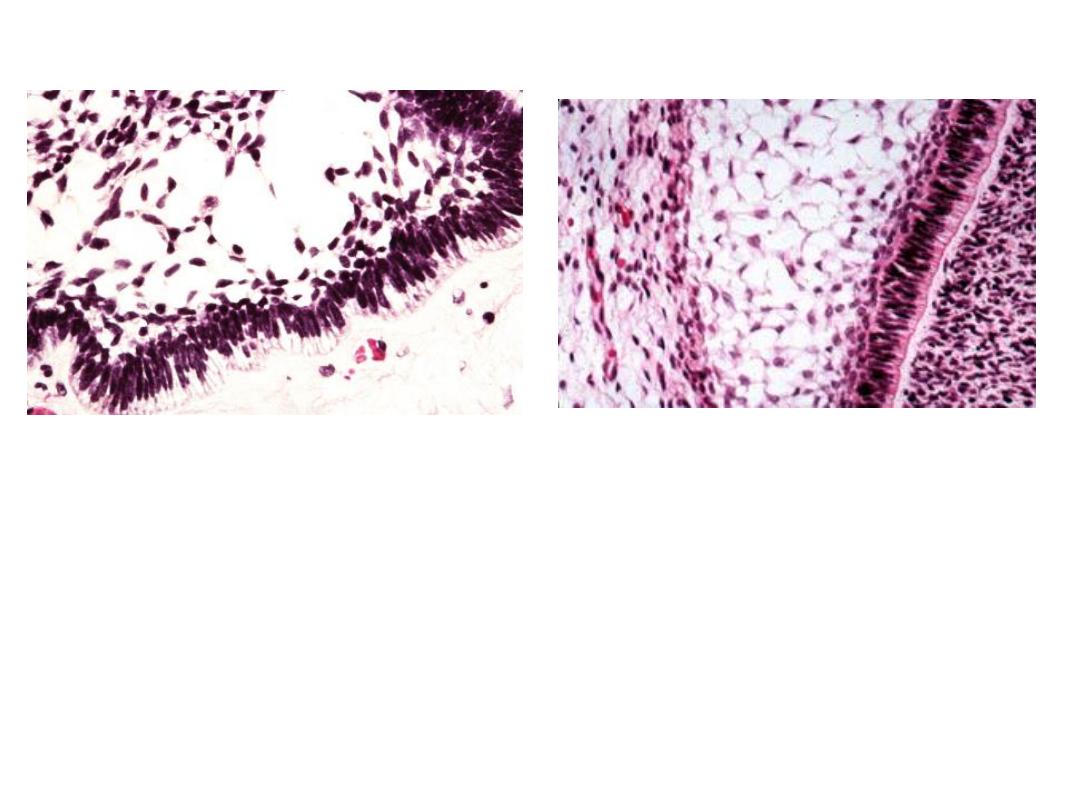
Histology resembles enamel organ epithelium with peripheral columnar
ameloblast-like cells surrounding loosely arranged stellate-reticulum-like cells
Ameloblastoma
Enamel Organ
2.
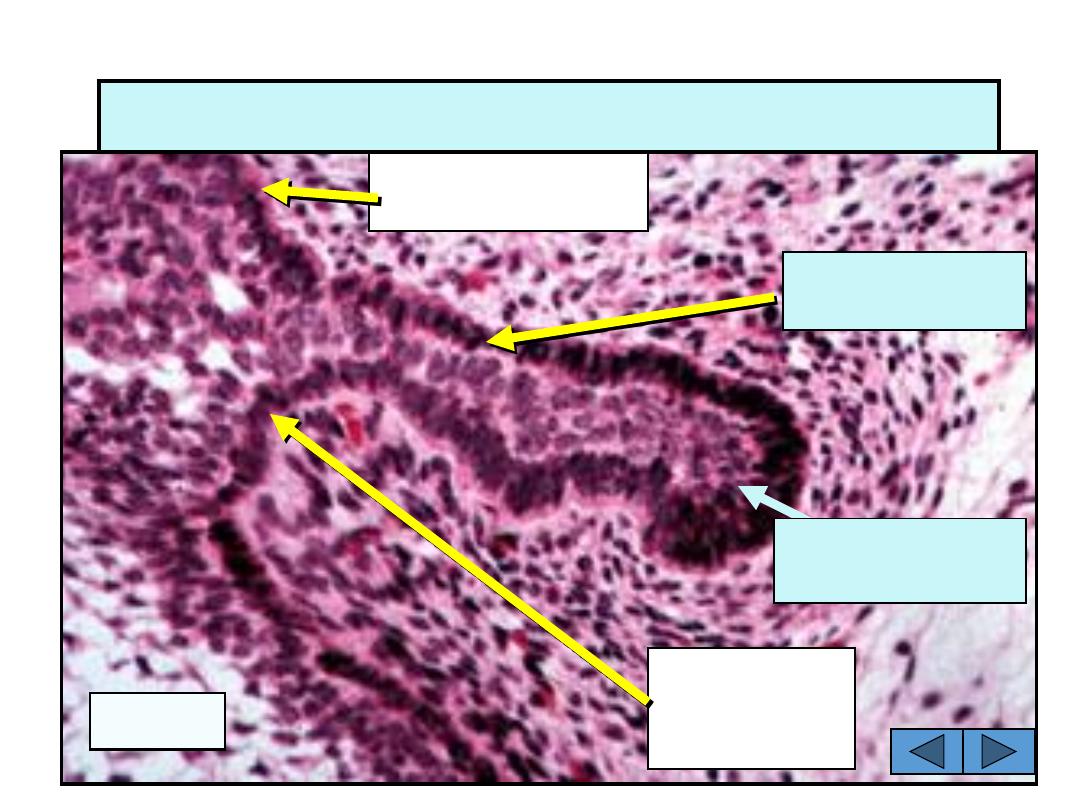
Odontogenic Myxoma: Tumor of the jaw that arise from odontogenic
ectomesenchyme. Histologically, looks similar to mesenchymal portion
of a developing tooth (dental papilla).
Odontogenic myxoma
Developing tooth
Formation of Permanent Dentition
Successional tooth bud
The tooth germs that give rise to permanent incisors, canines and premolars form
as a result of further proliferative activity within the dental lamina, lingual to the
deciduous tooth germ
The developing permanent molars have no deciduous predecessor and their tooth
germs originate from the dental lamina that extends posteriorly beneath the oral
epithelium after the jaws have grown
http://www.usc.edu/hsc/dental/ohisto/
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
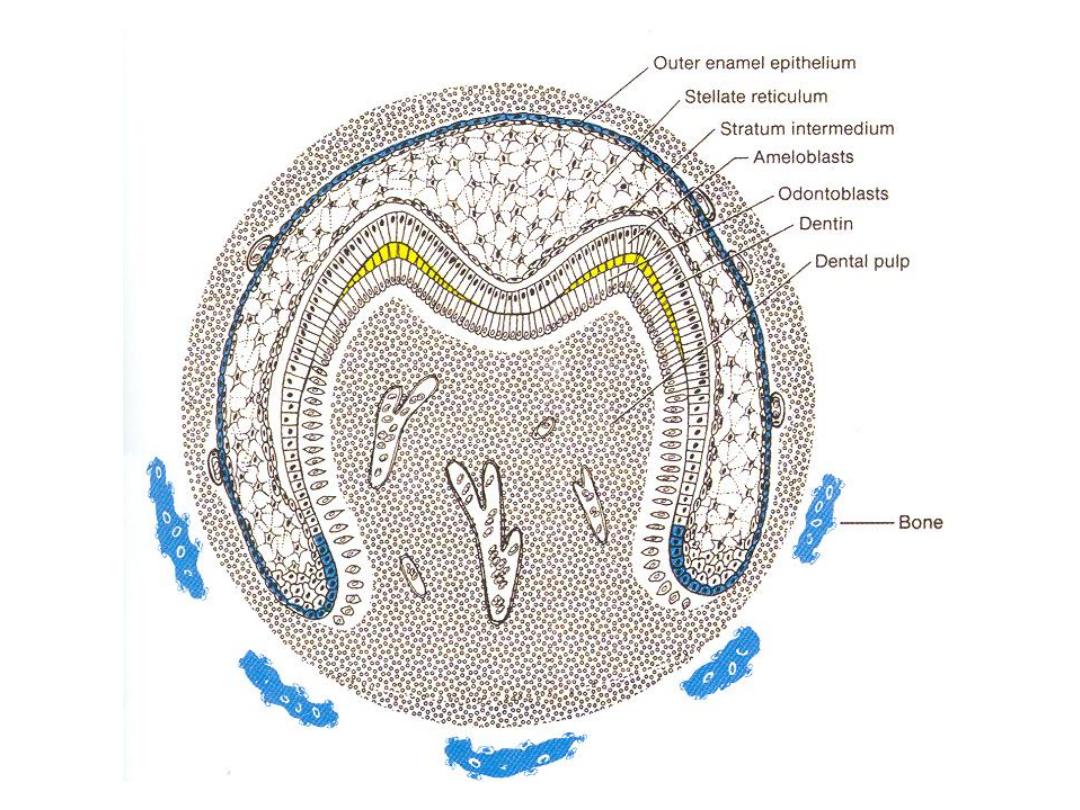
Bell Stage
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
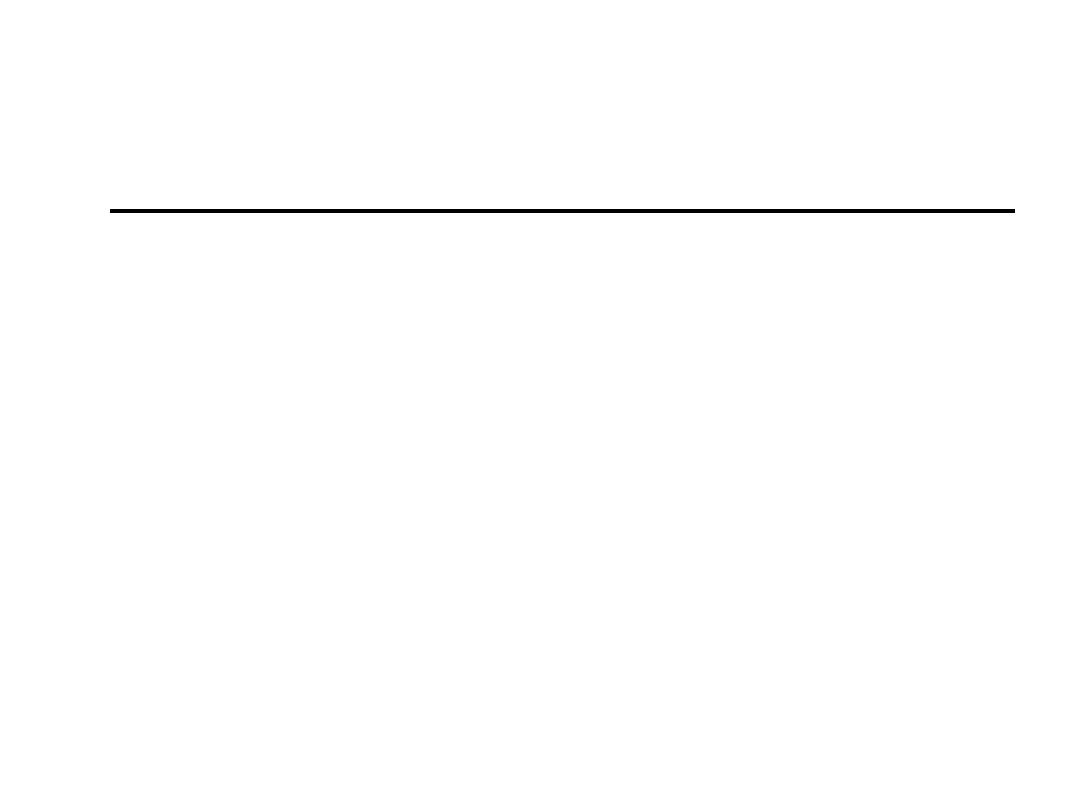
Hard Tissue Formation
Deposition of dental hard tissues is
called “apposition”
After the crown attains its final
shape during cap to early bell stage,
the inner dental epithelial cells stop
to proliferate, except the cells at the
cervical loop
First layer of dentin appears at the
cusp tips and progresses cervically,
and the columnar cells of the inner
dental epithelium become elongated
and show reverse polarization,
with the nuclei adjacent to stratum
intermediate (ameloblasts)
The boundary between the odontoblasts
and inner dental epithelium defines the
future dentino-enamel junction
http://www.usc.edu/hsc/dental/ohisto/

For dentinogenesis and amelogenesis to take place normally,
the differentiating odontoblasts and ameloblasts will receive
signals form each other – “reciprocal induction”
Stages of Apposition
1. Elongation of inner dental epithelium
2. Differentiation of odontoblasts
3. Formation of dentin
4. Formation of enamel
At the same time or soon after the first layer of dentin (mantle dentin) is formed,
the inner dental epithelial cells differentiate into ameloblasts and secrete enamel
proteins. These proteins further will help in the terminal differentiation of
odontoblasts. The ameloblasts will then start laying down organic matrix of
enamel against the newly formed dentinal surface. The enamel matrix will
mineralize immediately and form the first layer of enamel. The formation of
enamel is called amelogenesis.
Ameloblasts
First layer of enamel
Dentin
Odontoblasts
http://www.usc.edu/hsc/dental/ohisto/
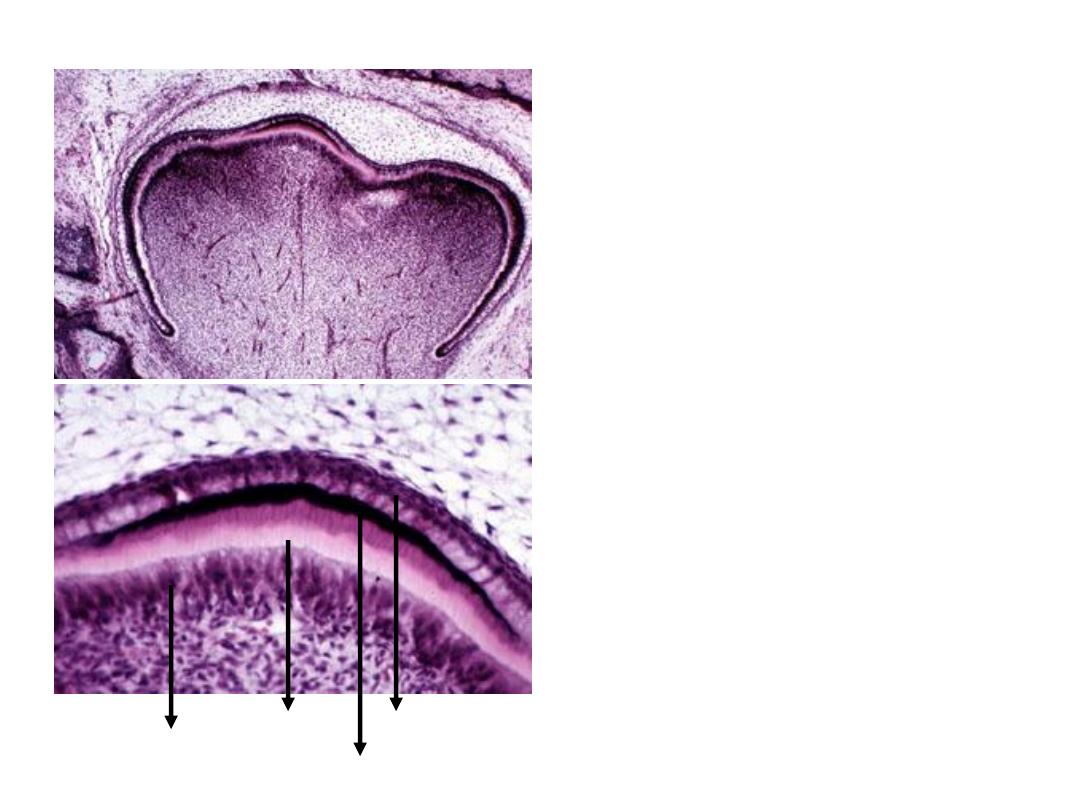
Apposition
At the same time when the inner
dental epithelium is differentiating,
the undifferentiated ectomesenchymal
cells increase rapidly in size and
ultimately differentiate into odontoblasts
Differentiation of odontoblasts from
ectomesenchymal cells are induced by
influence from the inner dental epithelium
Experiments have shown that if there is
no inner dental epithelium, there is no
dentin formed
Odontoblasts Dentin
Enamel
Ameloblasts
http://www.usc.edu/hsc/dental/ohisto/
Structures at Appositional Stage
Dental follicle
Outer Dental Epith.
Stellate reticulum
Inner Dental Epith.
Pulp
Odontoblasts
Stratum intermedium
©Copyright 2007, Thomas G. Hollinger, Gainesville, Fl
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
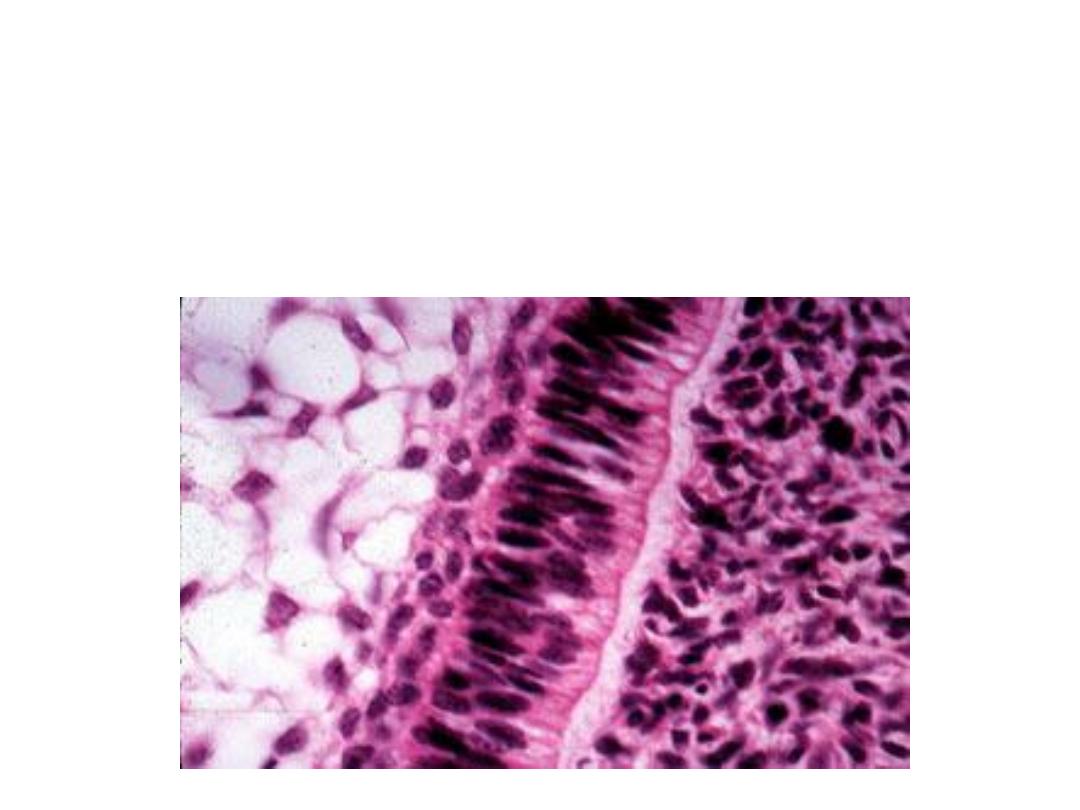
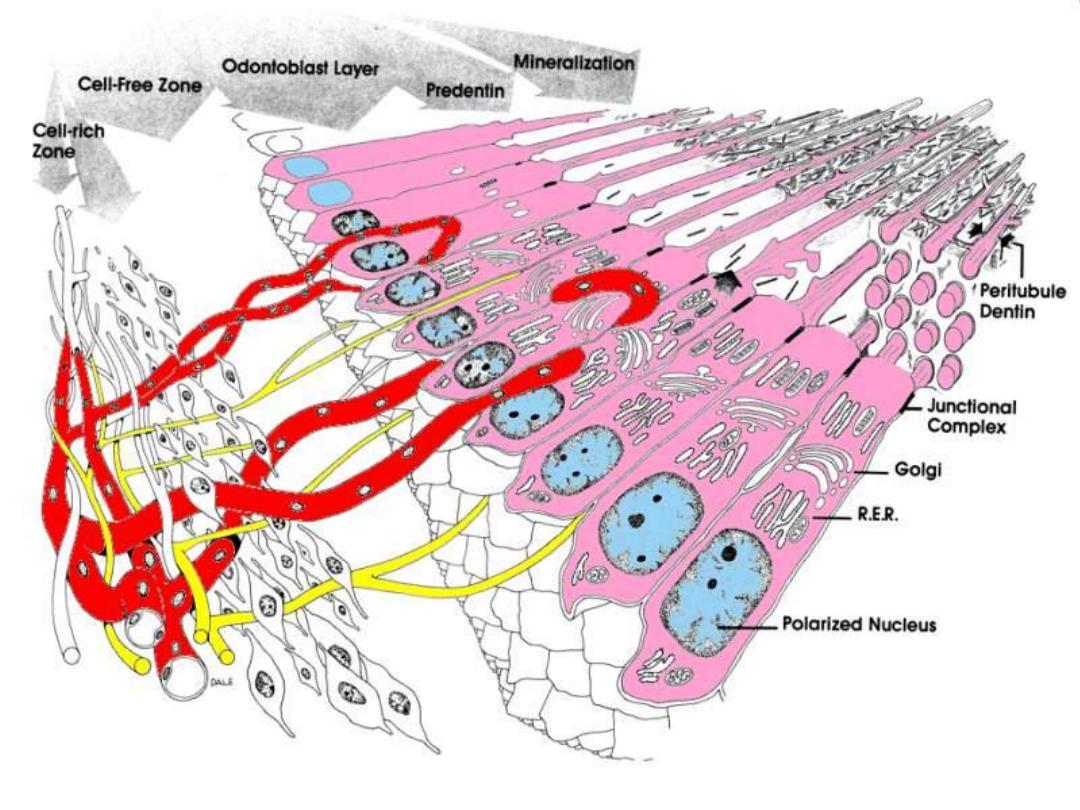
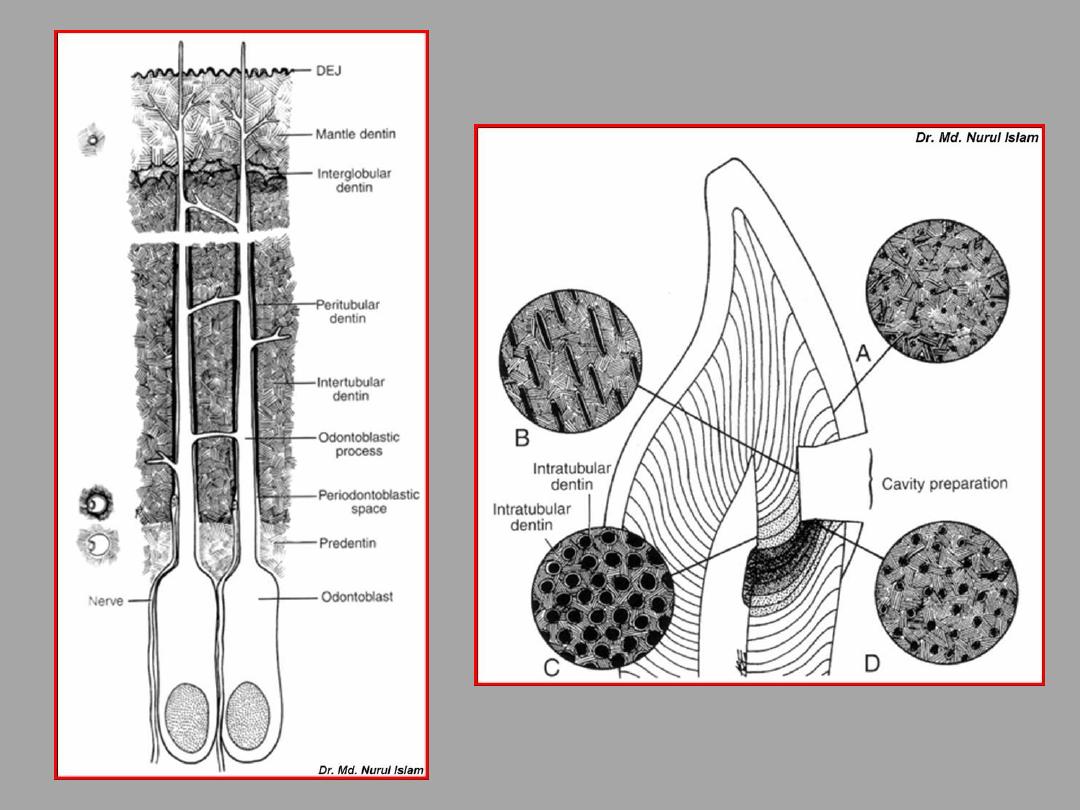
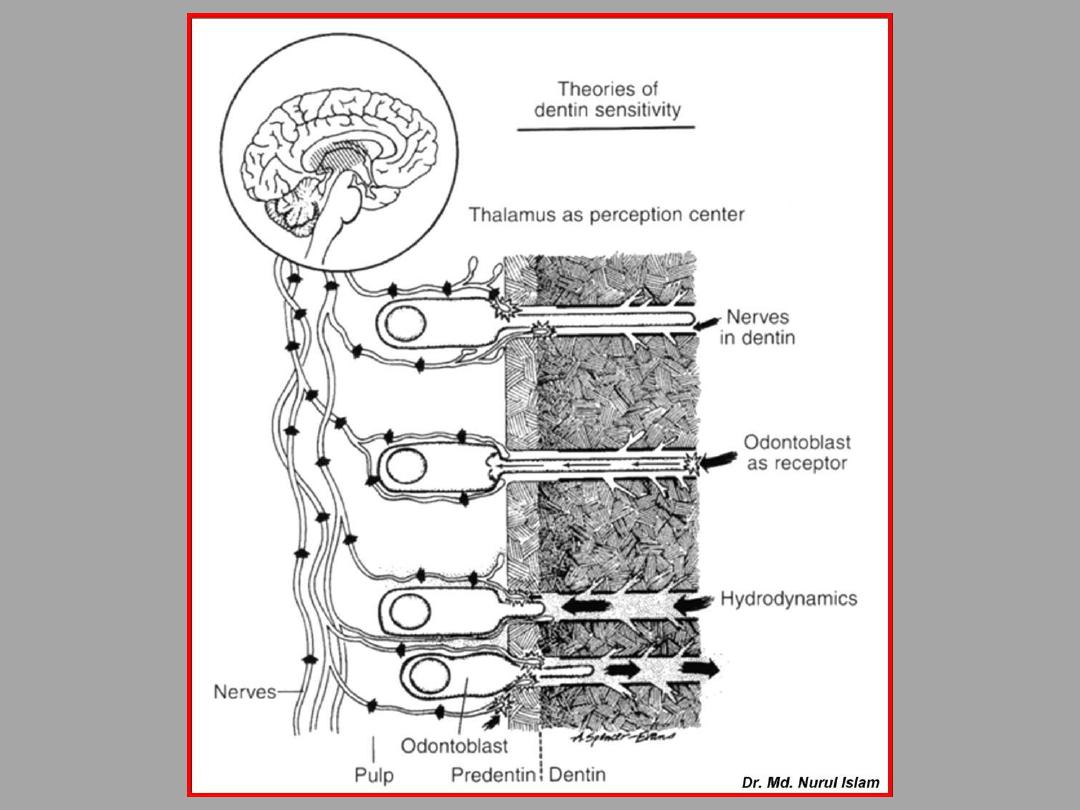
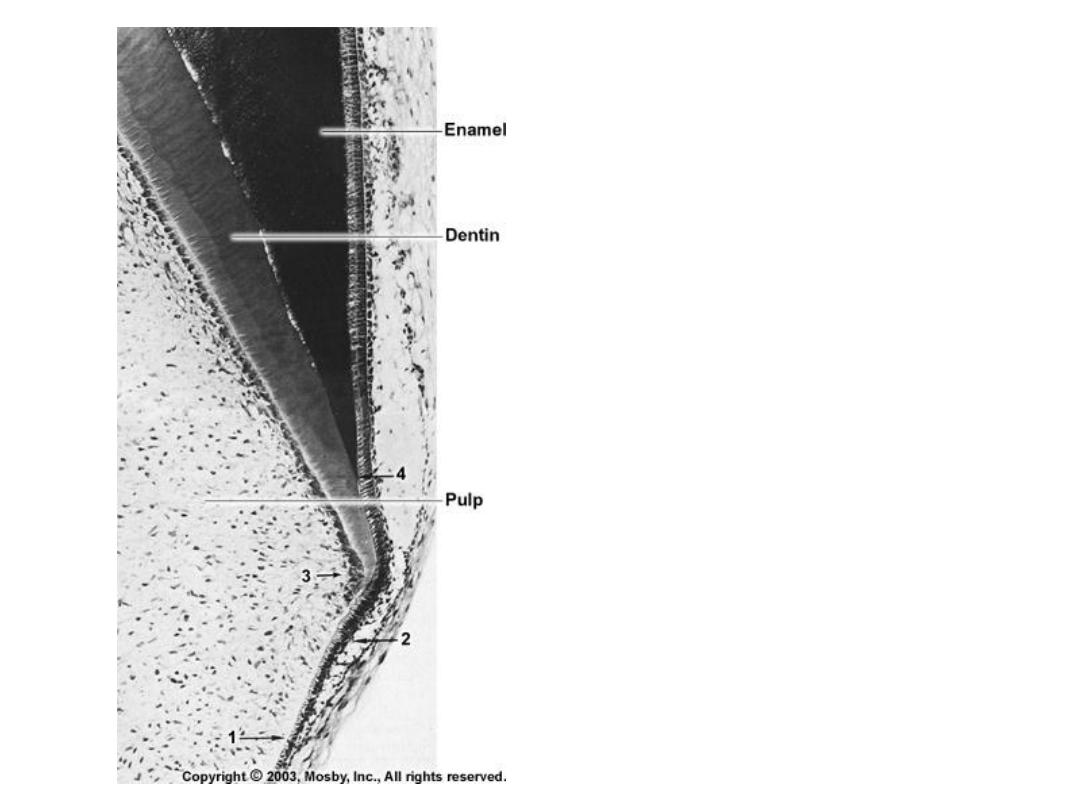
Dentinogenesis
Dentin is formed by odontoblasts that differentiate from ectomesenchymal
cells of dental papilla with influence from the inner dental epithelium
Differentiation of odontoblasts is mediated by expression of signaling
molecules and growth factors in the inner dental epithelial cells
http://www.usc.edu/hsc/dental/ohisto/
Odontoblasts are highly polarized with the nuclei away from inner dental epith.
Following differentiation of odontoblasts, first layer of dentin is produced,
characterized by appearance of large-diameter type III collagen fibrils (0.1
to 0.2
m in dia) called von Korff’s fibers, followed by type I collagen fibers
– MANTLE DENTINE
At the same time as initial dentin deposition, the odontoblasts will develop stubby
Processes (short and thick extensions) at the side close to the inner dental
epithelium which extend into forming extracellular matrix
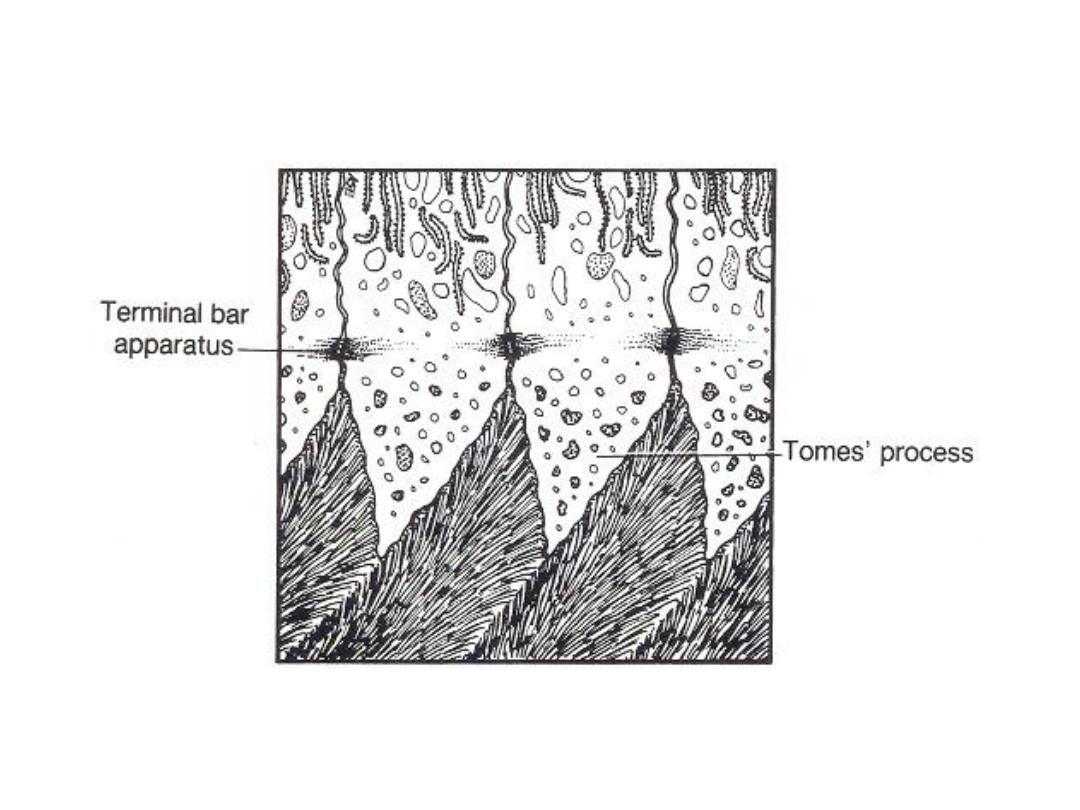
As the odontoblasts move pulpward, the odontoblast process (Tomes´ fiber) will
elongate and become active in dentine matrix formation
It is initially called predentin and following mineralization is called dentin
Dentinogenesis
Oral Histology, 5
th
edition, A R Ten Cate
©Copyright 2007, Thomas G. Hollinger, Gainesville, Fl
The odontoblasts as they differentiate will start elaborating organic matrix
of dentin, which will mineralize. As the organic matrix of dentin is deposited,
the odontoblasts move towards the center of the dental papilla, leaving behind
cytoplasmic extensions which will soon be surrounded by dentin. Therefore,
a tubular structure of dentin is formed.
odontoblasts
dentin
ameloblasts
http://www.usc.edu/hsc/dental/ohisto/
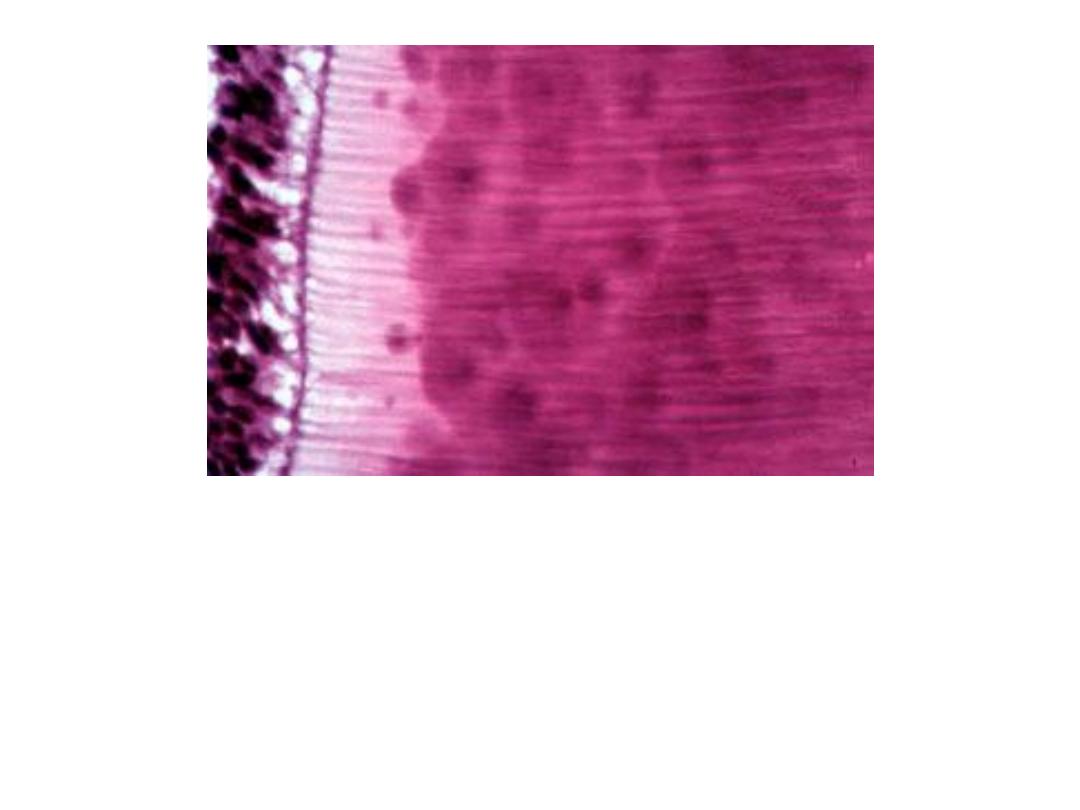
Odontoblasts with cytoplasmic processes forming dentinal tubules
http://www.usc.edu/hsc/dental/ohisto/
2 steps of dentinogenesis:
1. Formation of collagen matrix
2. Deposition of calcium and phosphate
(hydroxyapatite) crystals in the matrix
Odontoblast
like squamous
epithelium
DENTIN:Composition
Collagen fibrils matriks, mineral
Crystalls,
glycoproteins & proteoglycans
Processes (fibers) of Odontoblast are lining
through the dentine tubules but cell bodies
are located in pulp region.
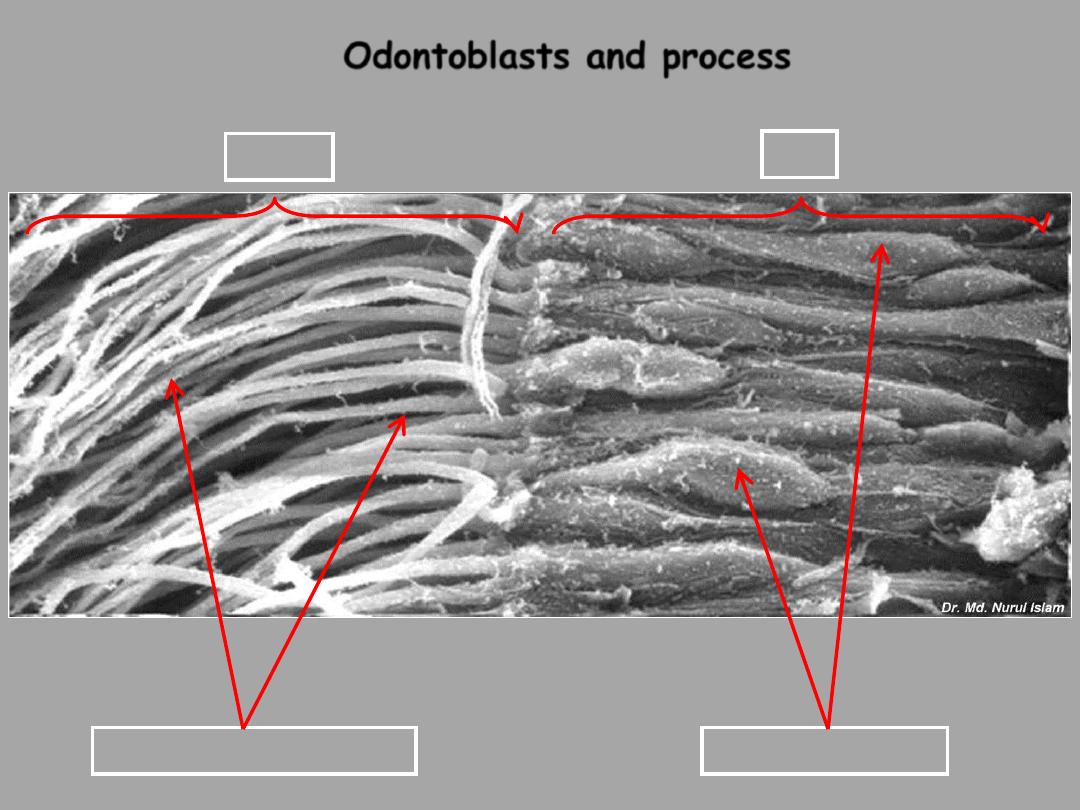
Odontoblasts and process
Odontoblast cells
Odontoblast extensions
Dentin
Pulp
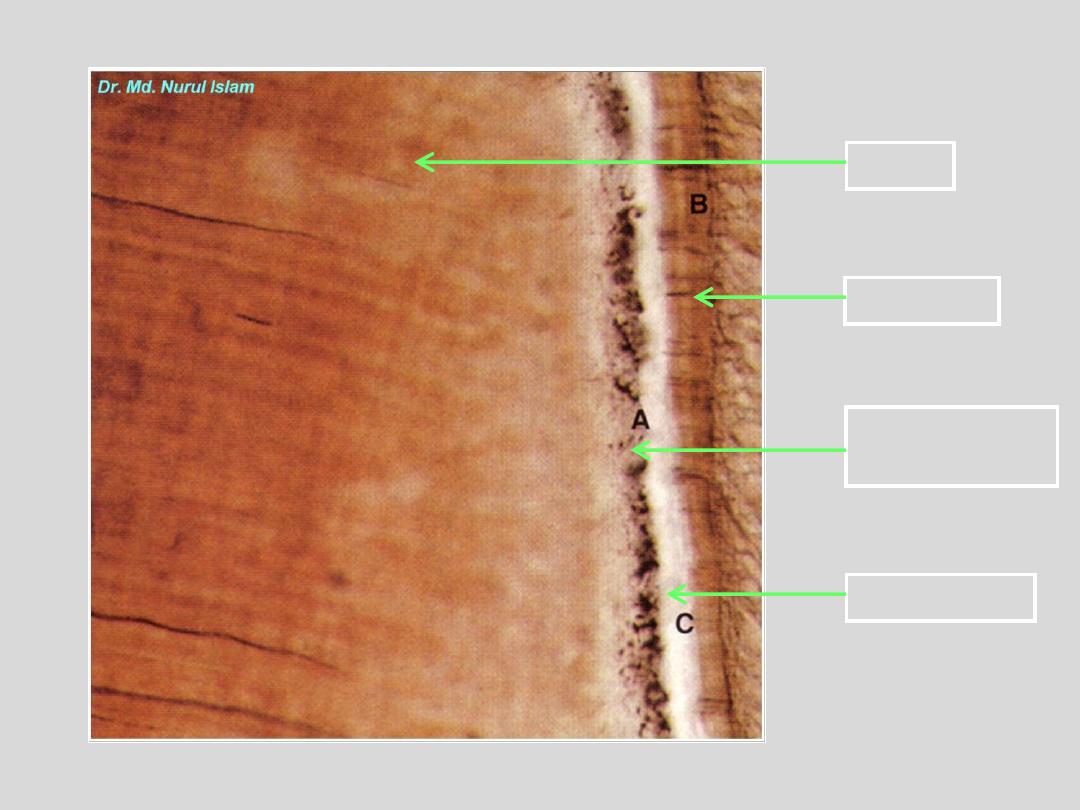
Dentin
Cementum
Granular layer
of Tomes
Hyaline layer

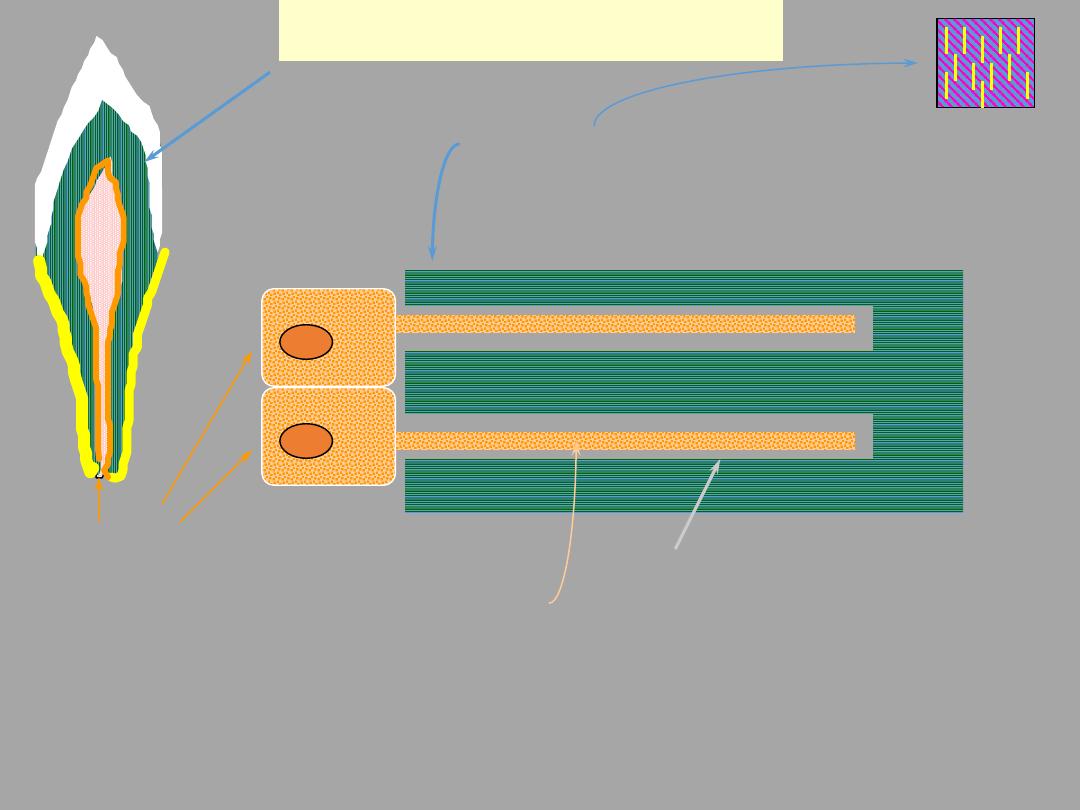
Amelogenesis is also a two-step process:
1.
First step produces a partially mineralized matrix (~ 30%)
2.
Second step involves influx of additional mineral coincident
with removal of organic material and water to attain greater
than 96% mineral content
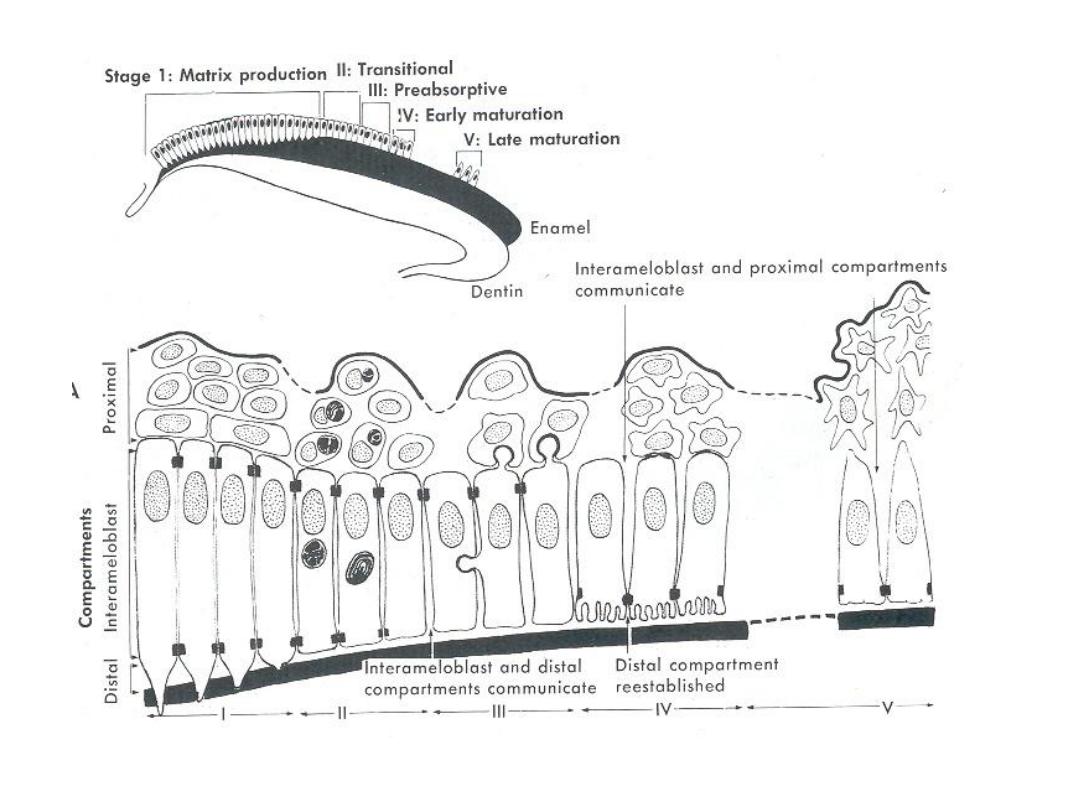
Amelogenesis
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
Amelogenesis
Amelogenesis begins after a few
m of dentin deposition at the
dentinoenamel junction
Ameloblasts goes through following functional stages:
1.
Morphogenetic. During this stage the shape of the crown is determined.
2.
Histodifferentiation. The cells of the inner dental epithelium is
differentiating into ameloblasts. The above two stages are the presecretory
stages, where the cells differentiate, acquire phenotype, change polarity,
develop an extensive protein synthesis machinery, and prepare to secrete an
organic matrix of enamel.
3. Secretory stage: Ameloblasts elaborate and organize the entire enamel
thickness. Short conical processes called Tomes´ processes develop at the
apical end of the ameloblasts. The main protein that accumulates is
amelogenin.
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
4. Maturation stage: Ameloblasts modulate and transport specific ions
required for the concurrent accretion of mineral. At this stage,
ameloblast becomes more active in absorption of the organic matrix
and water, which allows mineralization to proceed. After the
ameloblasts have completed their contributions to the mineralization
phase, they secrete an organic cuticle on the surface of the enamel,
which is called developmental or primary cuticle
5.
Protection: The ameloblast are shorter and contact the stratum
intermedium and outer dental epithelium and fuse to form the
reduced dental (enamel) epithelium. The reduced enamel epithelium
remains until the tooth erupts. As the tooth erupts and passes
through the oral epithelium, the incisal part of the reduced dental
epithelium is destroyed but the epithelium present cervically
interacts with oral epithelium to become the junctional epithelium
Amelogenesis

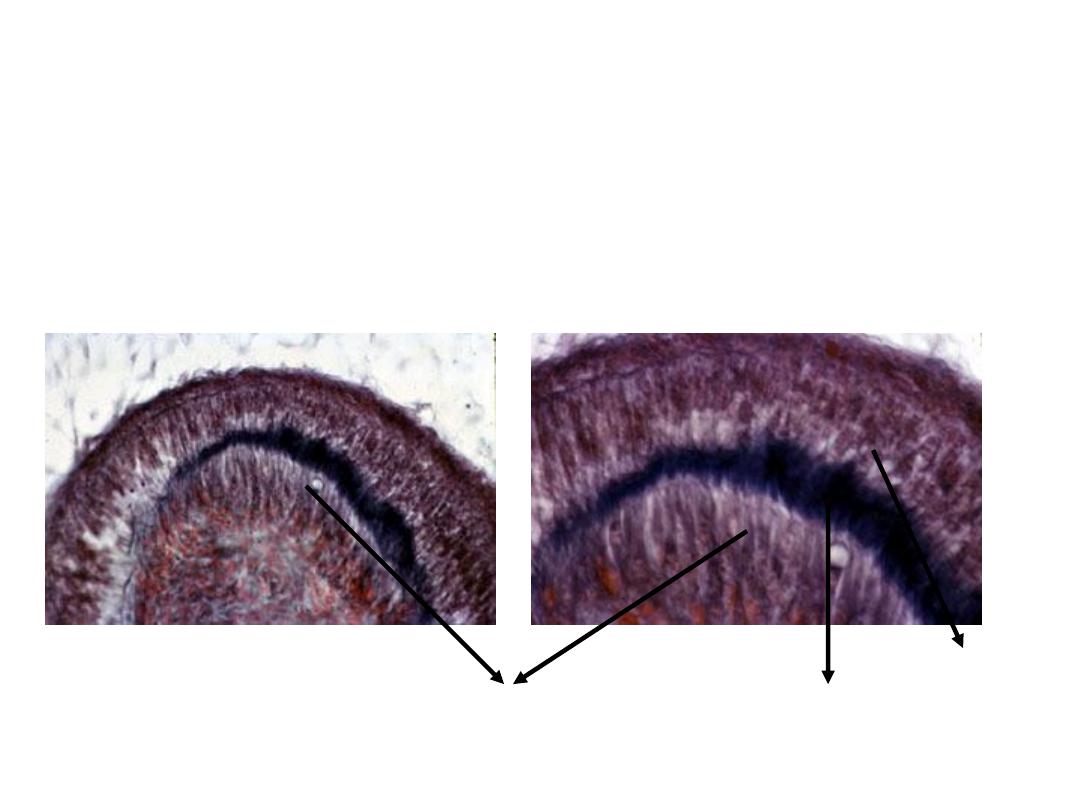
Amelogenesis Imperfecta
Hypomaturation
Hypoplastic
Hypocalcified
Summary of Tooth Development
(So Far)
1.
The epithelium is separated from the
dental papilla by an acellular zone
2.
Inner dental epithelial cells are elongated,
and the acellular zone is lost by
differentiation of odontoblasts
3.
Odontoblasts retreat toward the center
of the pulp, leaving behind dentin
4.
Ameloblasts begin to migrate outward and
leave behind formed enamel
Time Line of Human Tooth Development
(Table 5-2 in Text book)
Age
Developmental Characteristics
42 to 48 days
Dental lamina formation
55 to 56 days
Bud stage; deciduous incisors;
canines and molars
14 weeks
Bell stage for deciduous teeth; bud
stage for permanent teeth
18 weeks
Dentin and functional ameloblasts
in deciduous teeth
32 weeks
Dentin and functional ameloblasts
in permanent first molars
Incremental pattern of dentin
and enamel formation from
initiation to completion
Growth areas of developing crown.
Growth at cusp tip, intercuspal region,
and cervical region
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.
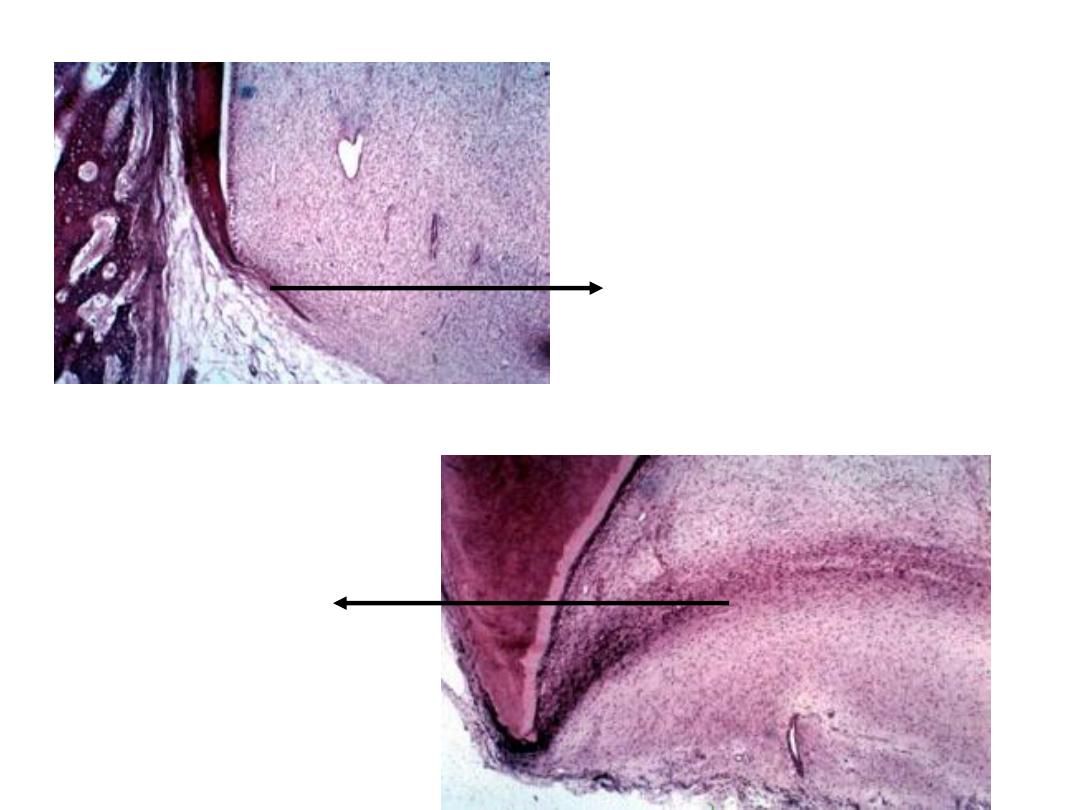
Root Formation
Development of root begins after the enamel and dentin formation has
reached the future cementoenamel junction
Epithelial cells of the inner and outer dental epithelium proliferate from the
cervical loop of the enamel organ to form the Hertwig’s epithelial root sheath.
The root sheath determines if a tooth has single or multiple roots, is short or
long, or is curved ir straight
Hertwig’s epithelial
root sheath
http://www.usc.edu/hsc/dental/ohisto/
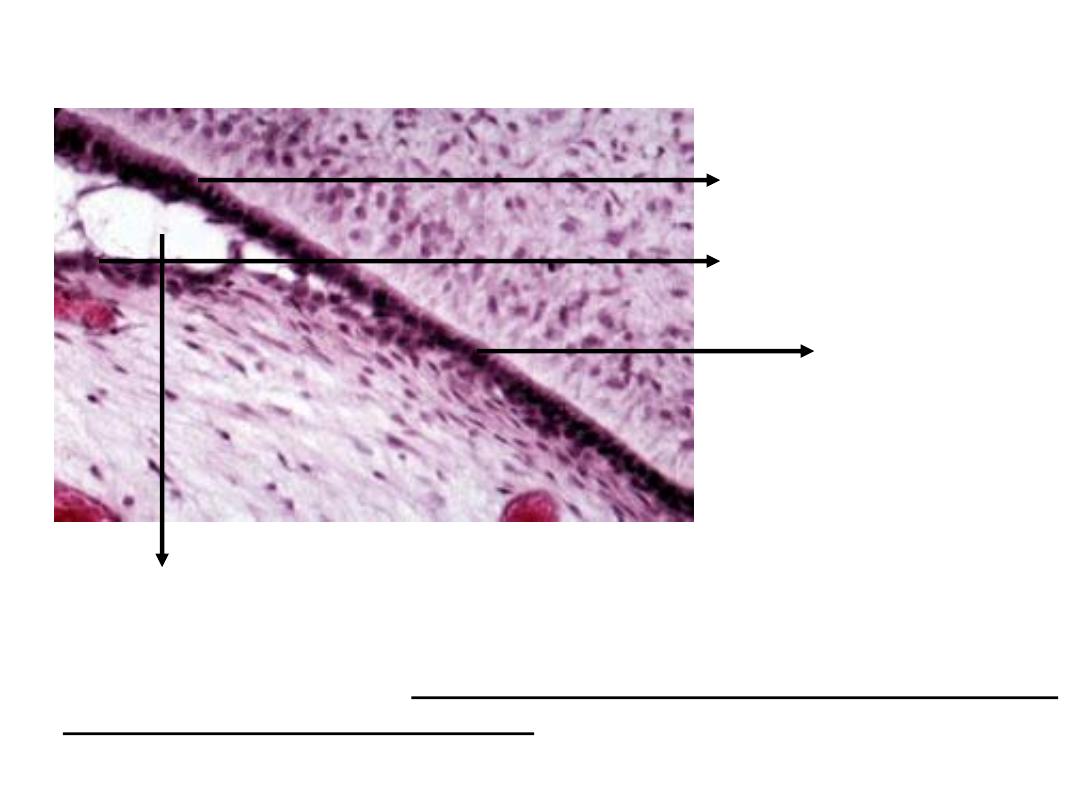
Hertwig’s epithelial
root sheath
Inner dental epithelium
Outer dental epithelium
Stratum intermedium
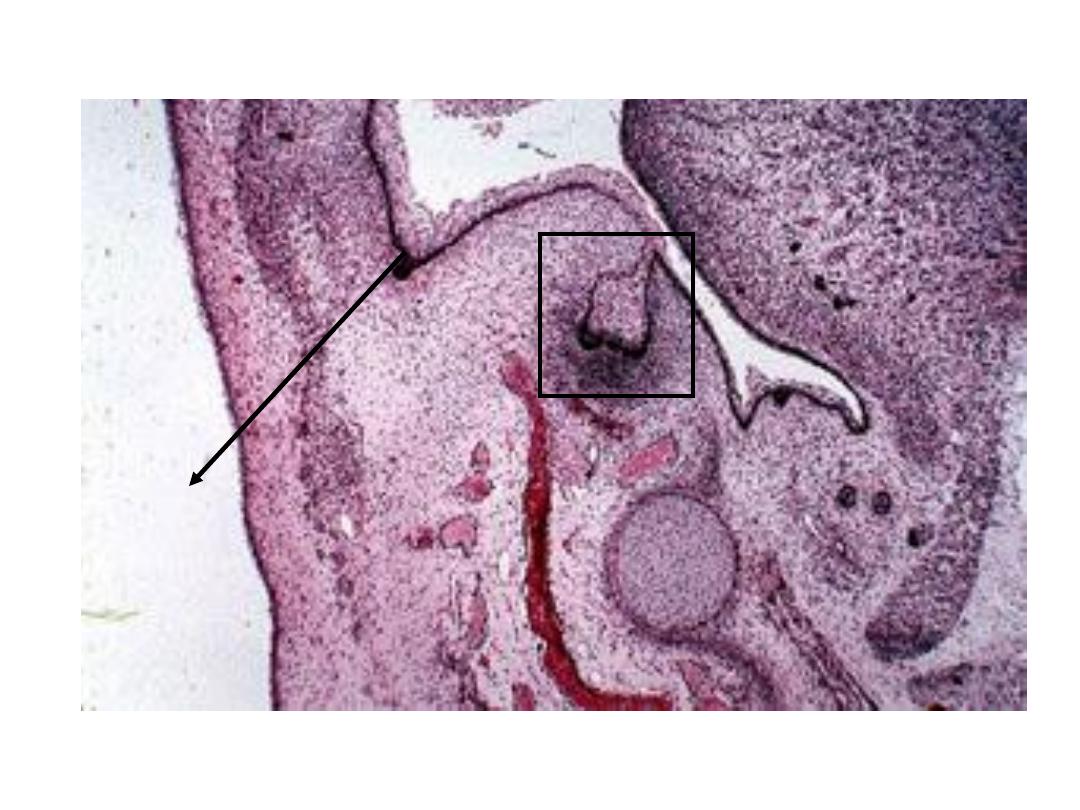
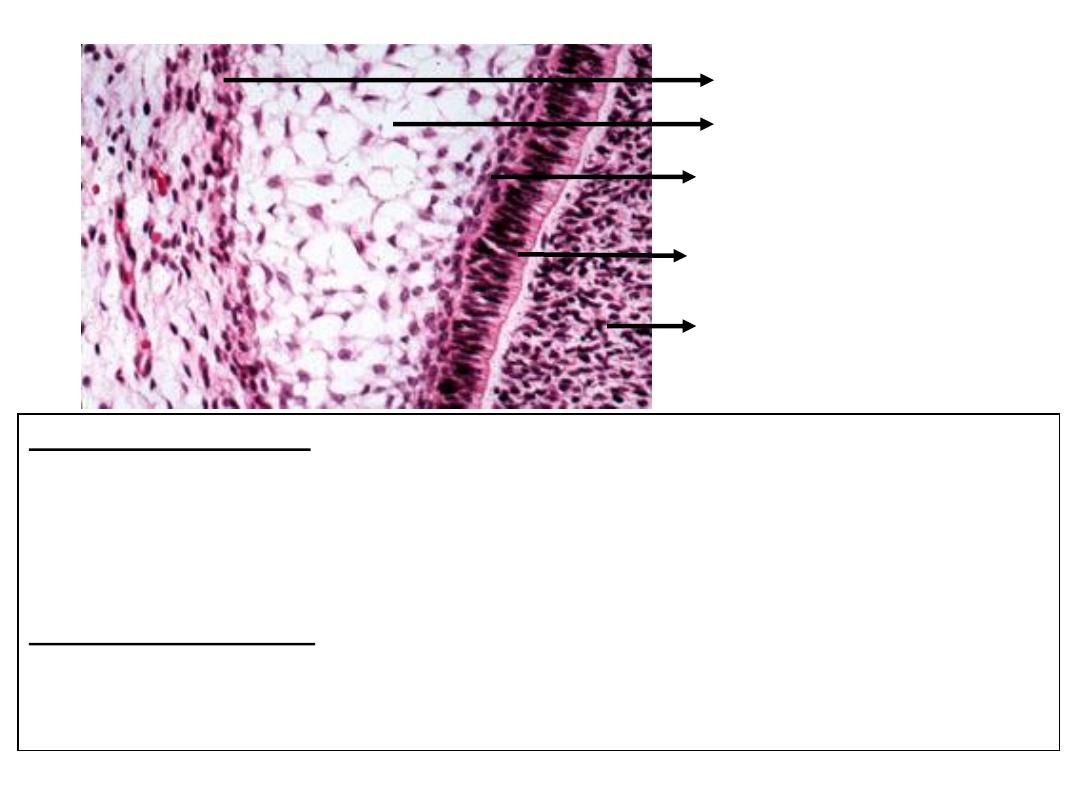
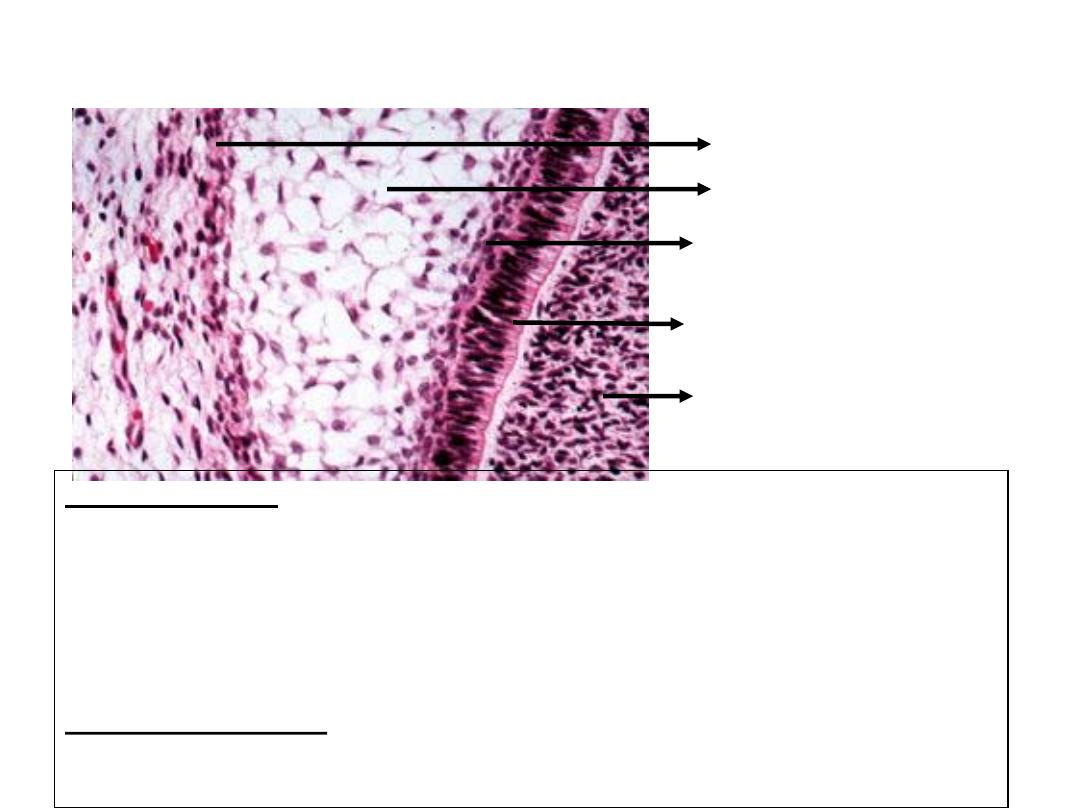
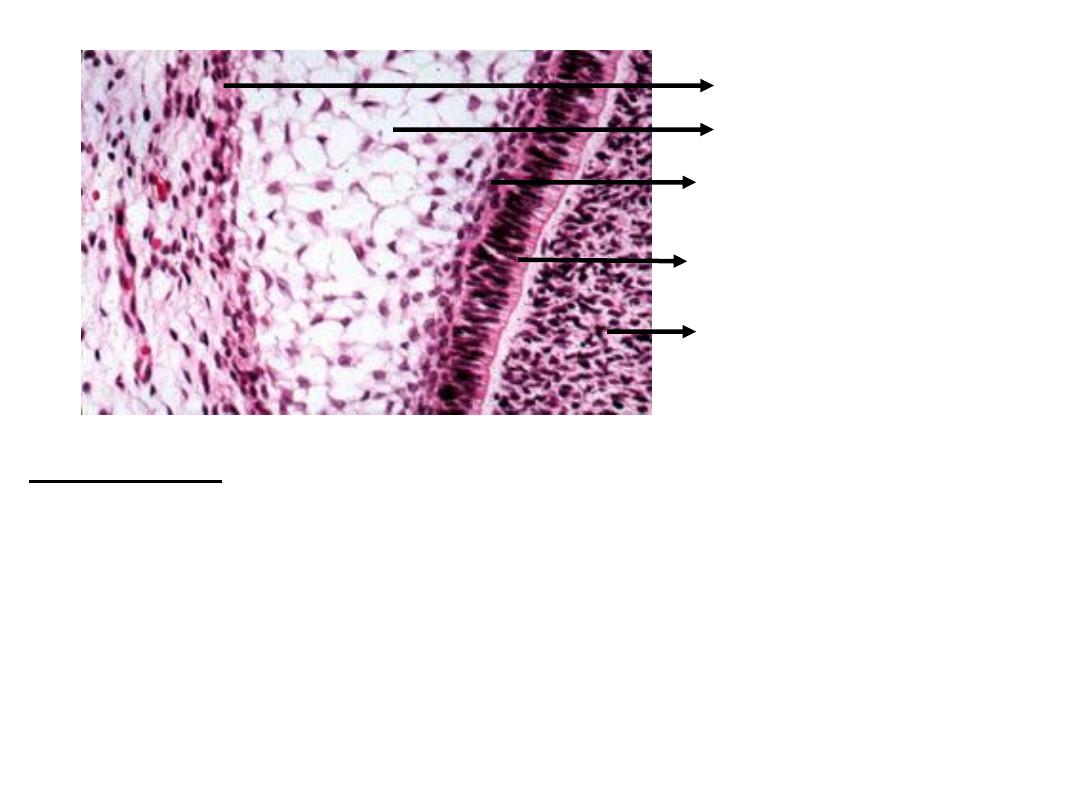
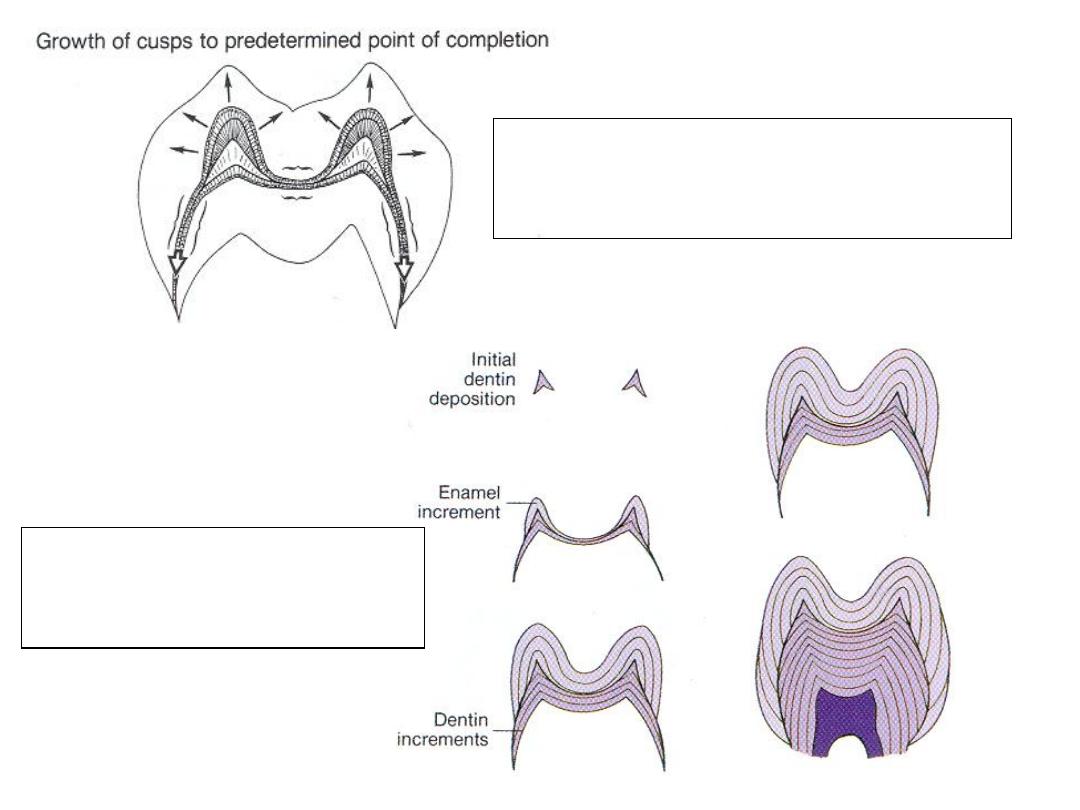
Eventually the root sheath will fragment to form several discrete clusters
of epithelial cells known as epithelial cell rests of malassez. These will persist in
adults within the periodontal ligament
http://www.usc.edu/hsc/dental/ohisto/
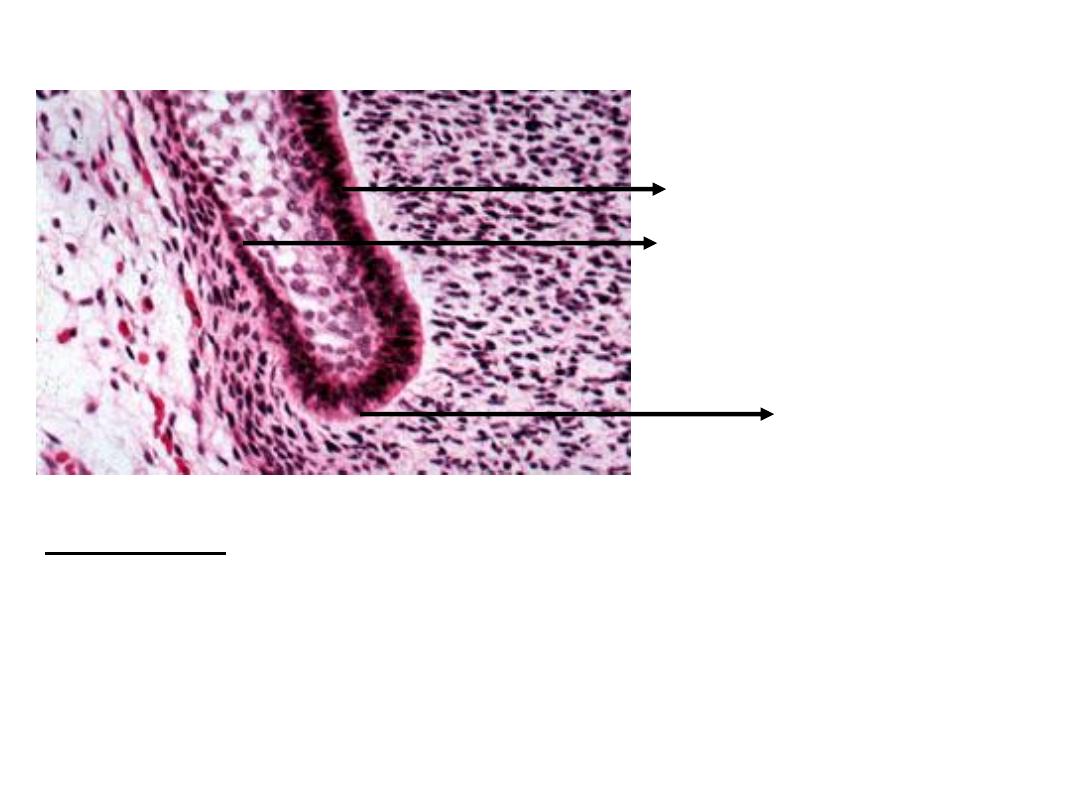
The epithelial rests appear as small clusters of epithelial cells which
are located in the periodontal ligament adjacent to the surface of
cementum. They are cellular residues of the embryonic structure
known as Hertwig's epithelial root sheath.
Epithelial Cell Rests of Malassez
http://www.usc.edu/hsc/dental/ohisto/
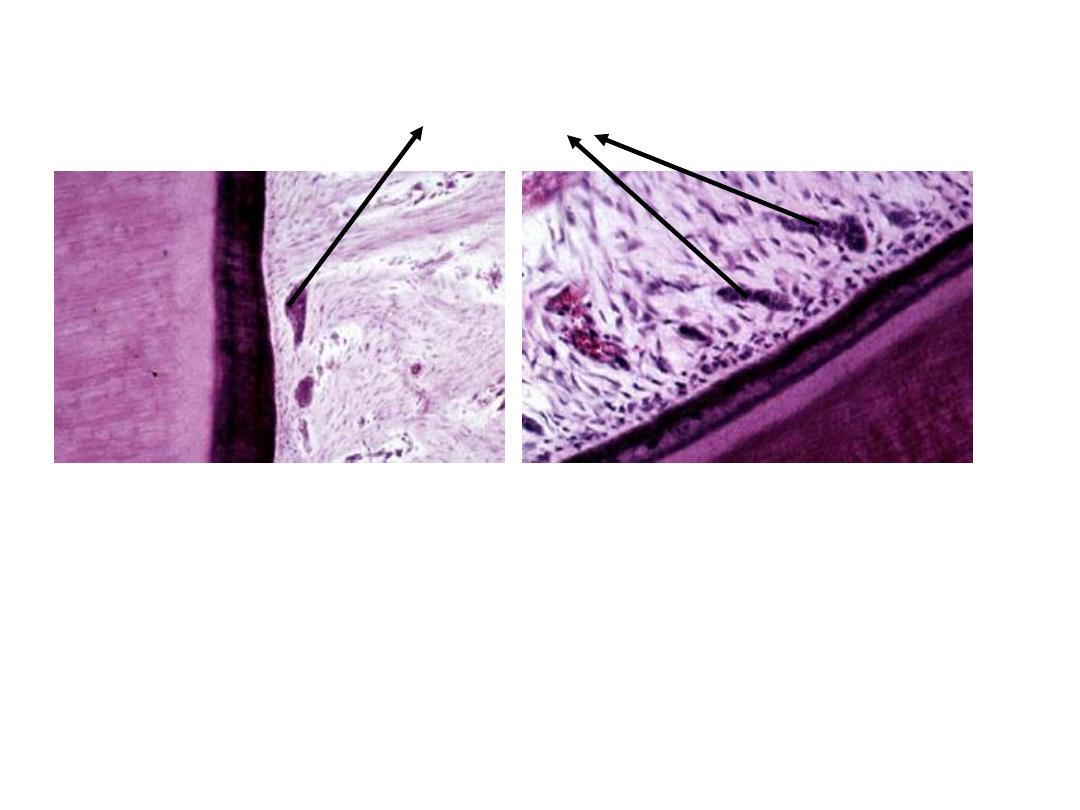
Primary apical formen
Epithelial diaphragm: the proliferating
end of the root sheath bends at a near
45-degree angle. The epithelial
diaphragm will encircle the apical
opening of the dental pulp during root
development
http://www.usc.edu/hsc/dental/ohisto/
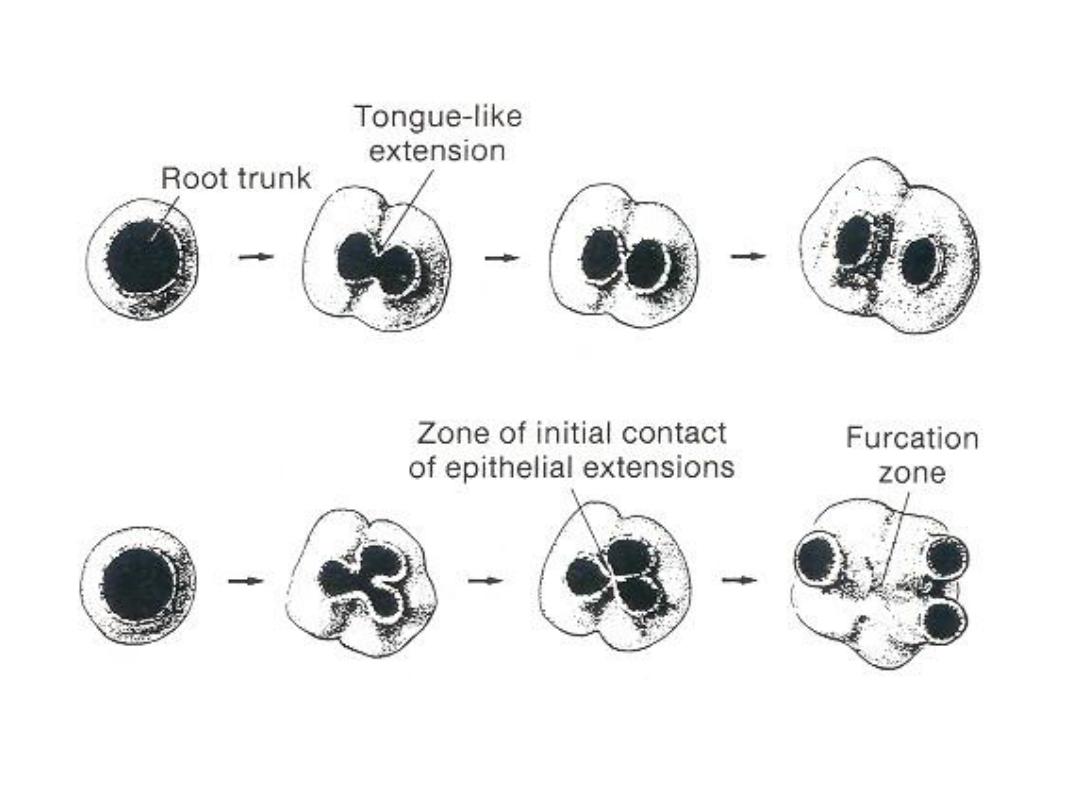
Secondary apical foramen form as a result of two or three tongues of
epithelium growing inward toward each other resulting in multirooted teeth
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000
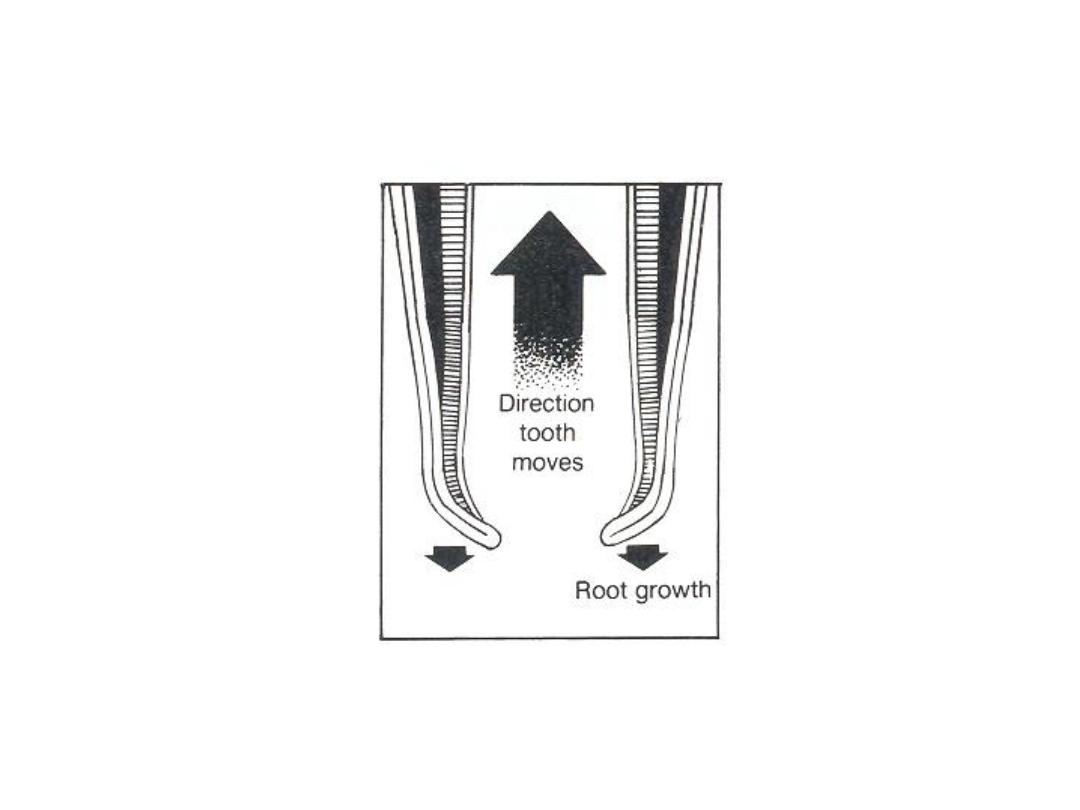
Direction of root growth versus eruptive movement of tooth
Essentials of Oral Histology and Embryology,
Ed: James Avery, 2
nd
edition. 2000.

Soon after root formation begins, tooth begins to erupt until it reaches
its final position
While roots are forming, the supporting structures of tooth also
develop – periodontal ligament and cementum
As the root sheath fragments, the dental follicle cells will penetrate between
the epithelial cells and lie close to the newly formed root dentin
These cells will differentiate into cementoblasts, which will make cementum
Fibers of the periodontal ligament, which will also form from the cells of the
dental follicle will get anchored in the organic matrix of the cementum which
will later get mineralized
Tooth eruption and Development of
supporting structures
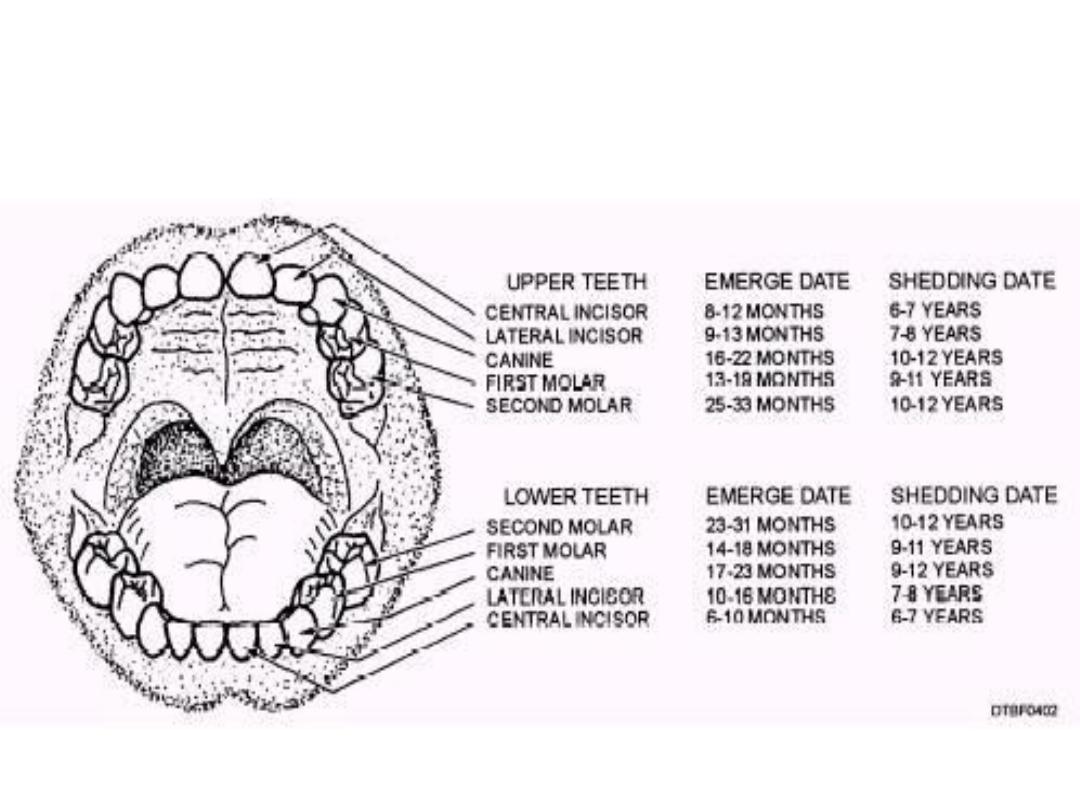
Figure :Average periods for emergence and exfoliation of primary teeth
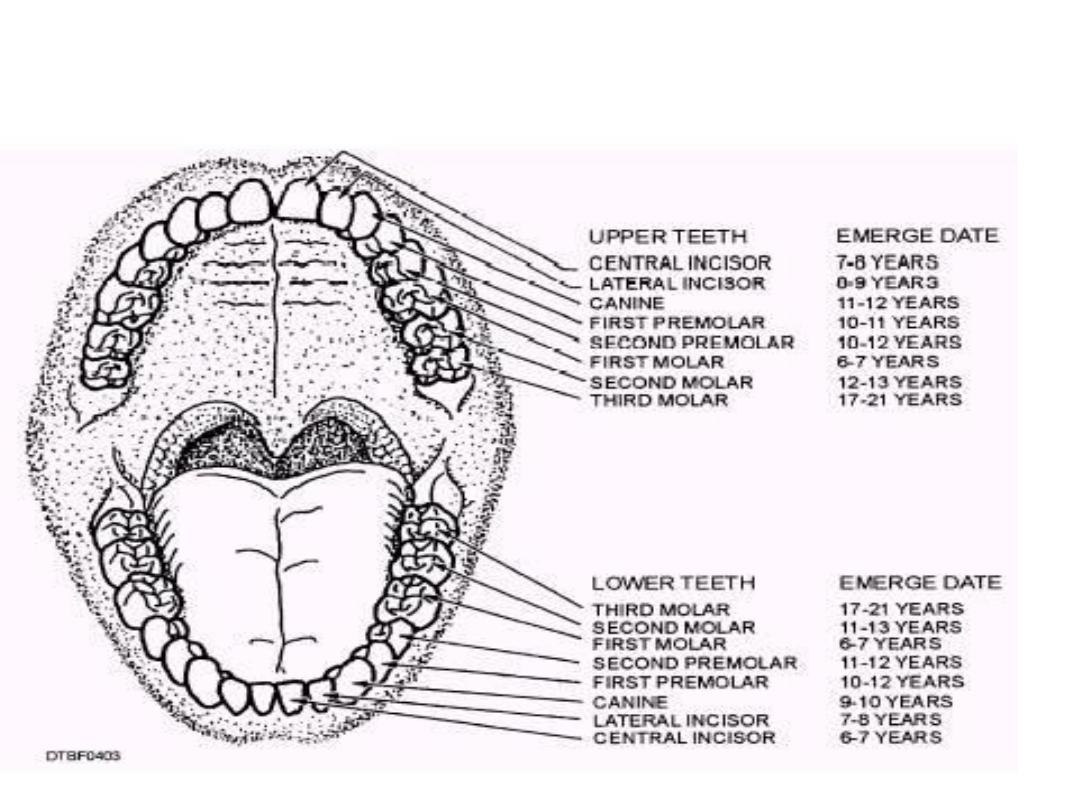
Figure: Average periods of emergence of permanent teeth.
