HeadacheDr.Ghayath
Headache account for up to 4% of medical office visits
Headache is caused by traction, displacement, inflammation, vascular spasm, or distention of the pain-sensitive structures in the head or neck.Isolated involvement of the bony skull, most regions of brain parenchyma does not produce pain
PAIN-SENSITIVE STRUCTURES WITHIN THE CRANIAL VAULT
These include the venous sinuses , arteries; the dura ; the trigeminal (V), glossopharyngeal (IX), and vagus (X) nervesEXTRACRANIAL PAIN-SENSITIVE STRUCTURES
These include the periosteum of the skull and other structuresApproach to the Differential Diagnosis
1-Location of PainUnilateral headache is an invariable feature of cluster headache and occurs in the majority of migraine attacks;
patients with tension headache report bilateral pain
Headache from intracranial mass lesions may be bioccipital and bifrontal pain when the intracranial pressure becomes elevated
Paranasal pain localized to one or several of the sinuses occure in sinusitis
2-Characteristics of Pain
Pulsating, throbbing pain is frequently ascribed to migraine
A steady sensation of tightness or pressure is also commonly seen with tension headache.
pain produced by intracranial mass lesions is typically dull and steadySharp, lancinating pain suggests a neuritic cause such as trigeminal neuralgia
4-Relieving factors
Migraine headaches are frequently relieved by darkness, sleep, vomiting, or pressing on the ipsilateral temporal artery, and their frequency is often diminished during pregnancy3-Precipitating Factors:
emotional stress, or fatigue; menses; hunger, chocolate containing phenylethylamine or cheddar cheese containing tyramine; oral contraceptive agents or other drugs such as nitrates and bright lights trigger for migraine.jaw claudication for giant cell arteritis
5-Associated Symptoms
Recent weight loss may accompany cancer, giant cell arteritisFever or chills may indicate systemic infection or meningitis
Visual disturbances suggest an ocular disorder eg. glaucoma,migraine
Nausea and vomiting are common in migraine
Photophobia may be prominent in migraine and acute meningitis or subarachnoid hemorrhage
Ipsilateral rhinorrhea and lacrimation during attacks typify cluster headache
• 6-Temporal pattern of head ache (Time)
• Headaches from mass lesions are commonly maximal on awakening also are sinus headaches:
• Headaches from mass lesions, however, increase in severity over time.
• Cluster headaches frequently awaken patients from sleep; they often recur at the same time each day or night in certain time in the year
• Tension headaches can develop whenever stressful situations occur and are often maximal at the end of a work day
• Migraine headaches are episodic and may be worse during menses
Primary headache
1-migrain2-Tension-Type headache
3-The trigeminal autonomic cephalalgias (TACs)
4- Primary Thunderclap headache
5-Hemicrania Continua
6-primary sex headache
7-hypnic headache
7-Prodromal Symptoms and Auras
such as scintillating scotomas or other visual changes, often occur with migraine• Secondary headache:
1-Meningitis2-Intracranial Hemorrhage
3-Brain Tumor
4-Temporal arteritis
5-Idiopathic intracranial hypertention
Migraine
Migraine is generally an episodic headache often with sensitivity to light, sound or movement, nausea or vomiting accompanying the headache , and may occur with or without aura. While migraine is often hemicranial, it is bilateral in about 40% of adults, Two-thirds to three-fourths of cases of migraine occur in women; the onset is early in life more than 90% before age 40
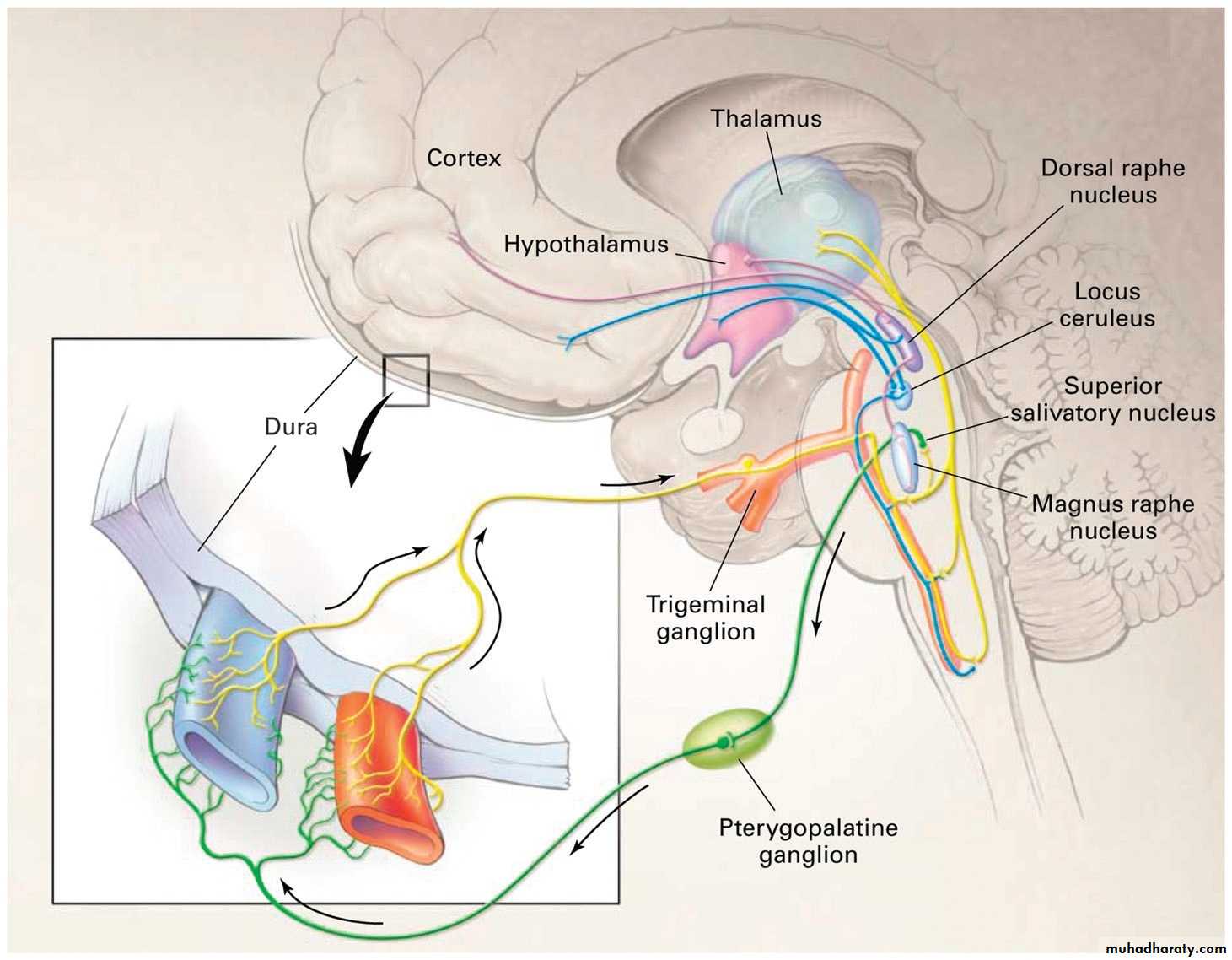
MIGRAINE PATHOPHYSIOLOGY
The cause of migraine is unknown but there is increasing
evidence that the aura is due to dysfunction of ion channels causing a spreading front of cortical depolarisation (excitation) followed by hyperpolarisation (depression of activity). This process (the ‘spreading depression’) spreads over the cortex at a rate of about 3 mm/minute, corresponding to the aura’s symptomatic spread. The headache phase is associated with vasodilatation of extracranial vessels. Activation of the trigeminovascular system is probably important.• Genetics of Migraine
• The aggregation of migraine within families has long been recognized, although consistent mendelian patterns of inheritance have not been found among the collective group of familial migraineurs. Presumably this reflects a variety of inheritance patterns, and possibly multiple genes interacting with environmental factors in the multigenic/multifactorial pattern characteristic of migrain .but a rare subtype of migraine with aura, familial hemiplegic migraine, has a straightforward autosomal dominant pattern• Migraine triggers
• include exertion, dietary factors (including delaying a meal), sleep disturbances, hormonal influences(menstruation) ,medication(especially oral contraceptive agents and vasodilators such as nitroglycerin), bright lights, sounds, alcohol , stormy weather or barometric pressure changes and certain foods( tyramine-containing cheeses; meat, such as hot dogs, chocolate containing phenylethylamine ..• Migraine Without Aura(COMMON MIGRAINE)
• Description: Recurrent headache disorder manifesting in attacks lasting 4 to 72 hours. Typical characteristics of the headache are unilateral location, pulsating quality, moderate or severe intensity, aggravation by routine physical activity, and association with nausea and/or photophobia and phonophobia.Diagnostic Criteria(Migraine Without Aura)
A. At least 5 attacks fulfilling criteria B through DB. Headache attacks lasting 4 to 72 hours (untreated or unsuccessfully treated)
C. Headache has at least two of the following characteristics:
1. Unilateral location
2. Pulsating quality
3. Moderate or severe pain intensity
4. Aggravation by routine physical activity (eg, walking or climbing stairs)
D. During headache at least one of the following:
1. Nausea and/or vomiting
2. Photophobia and phonophobia
E. Not attributed to another disorder
• Migraine with aura (CLASSIC MIGRAINE)
• Description: Typical aura consisting of visual and/or sensory and/or speech symptoms. Gradual development, duration no longer than 1 hour and complete reversibility characterize the aura. which is associated with a headache fulfilling criteria for migraine without aura.
• management
• Nonpharmacologic Management• Migraine can often be managed to some degree by a variety of nonpharmacologic approaches. Most patients benefit by the identification and avoidance of specific headache triggers. A regulated lifestyle is helpful including a healthful diet, regular exercise, regular sleep patterns, avoidance of excess caffeine and alcohol.
• Acute Attack Therapies for Migraine
• Mild migraine attacks can usually be managed by oral agents; Severe migraine attacks may require parenteral therapy. Most drugs effective in the abortive treatment of migraine are members of one of three major pharmacologic classes: NSAID, 5-HT1B/1D receptor agonists, and dopamine receptor antagonists.
• Acute (Abortive) Treatment
• Simple Analgesics:• Acetaminophen, aspirin, caffeine
• NSAIDs: Naproxen, Ibuprofen. etc…
• 5-HT1 Agonists:
• Oral :eg. Ergotamine, Sumatriptan, Zolmitriptan
• Nasal: Dihydroergotamine, Sumatriptan, Zolmitriptan
• Parenteral: Dihydroergotamine
• Subcutaneos: Sumatriptan
• Dopamine Antagonists:oral and parantral mainly for vomiting eg. Chlorpromazine &Metoclopramide
• When to Use Migraine Prevention
• Three or more headache episodes per month• Significant interference of headache with daily activity
• Acute medications ineffective, contraindicated, or overused
• Adverse effects from acute medications
General Principles of Preventive Treatment
Start with a low dose and increase slowly
Use an adequate trial of 2 to 3 months
Consider preventive medication combinations in refractory patients
Taper when headaches are controlled
• Classes of Migraine Preventives
• Antiepileptic drugs:eg.topiramatate , Divalproex sodium,• Antidepressants:tricyclic eg. Amitriptyline, Nortriptyline
• Beta-adrenergic blockers:eg. Propranolol, Timolol maleate
• Calcium channel antagonists: eg. Verapamil
Antiserotonin/Antihistamine:eg. Cyproheptadine
Pure Menstrual Migraine
Migraine without aura that occurs exclusively on (ie, days -2 to +3)of menstruation in at least two of three menstrual cycles.No migraine occurs at other times of the cycle.
• TENSION-TYPE HEADACHE
The term tension-type headache (TTH) is commonly used to describe a chronic head-pain syndrome characterized by bilateral tight, band like discomfort or pressure at the vertex. It is of constant character and generalised,but often radiates forwards from the occipital region. The pain typically builds slowly, fluctuates in severity, and may persist more or less continuously for many days. The headache may be episodic or chronic (present >15 days per month).A useful clinical approach is to diagnose TTH in patients whose pain is not localized, not throbbing, not aggravated by activity, and not severe no significant nausea, no vomiting, no more than one photophobia or phonophobia
Pathophysiology
Tension headache is incompletely understood. Emotions
and anxiety are common precipitants and there is sometimes
an associated depressive illness. Anxiety about the headache itself may lead to continuation of symptoms and patients often become convinced of a serious underlying condition. Muscular spasms may worsen this in some patients
MANAGEMENT OF TENSION-TYPE HEADACHE
The approach to the management of TTH involves a combination of lifestyle, physical, and pharmacologic measures recommendations for regulation of sleep, meals, and exercise are generally quite valuable. Stress management techniques and other steps toward trigger avoidance may be of great benefit. Behavioral therapies are the most frequentlyrecommended techniques including relaxation therapy
• Acute Therapies for Tension-Type Headache
• Acetaminophen• Aspirin
• Ibuprofen
• Ketoprofen
• Naproxen
• Diclofenac
• Caffeine
• Pharmacologic Preventive Therapies for Tension-Type Headache
• Amitriptyline• Mirtazapine
• Venlafaxine
Trigeminal Autonomic Cephalalgias:
• 1-Cluster headache
• Cluster headache syndrome occurs much more frequently in men than in women. Cluster headaches characteristically begin at a later age than migraine, with a mean age at onset of 25 years. There is rarely a family history of such headaches.
The syndrome presents as clusters of brief, very severe, unilateral, constant, nonthrobbing headaches that last from 15 minutes to 2 hours. Unlike migraine headaches, cluster headaches are always unilateral, and usually recur on the same side in any given patient. The headaches commonly occur at night, awakening the patient from sleep, and recur daily, often at nearly the same time of day, for a cluster period of weeks to months. Between clusters, the patient may be free from headaches for months or years. The headache may begin as a burning sensation over the lateral aspect of the nose or as a pressure behind the eye Ipsilateral conjunctival injection, lacrimation, nasal stuffiness, and Horner syndrome are commonly associated with the attack . Episodes are often precipitated by the use of alcohol or vasodilating drugs, especially if used during a cluster siege.
• Treatment:
• Abortive treatment : subcutaneous or intranasal sumatriptan or Zolmitriptan nasal spray (5 or 10 mg), 100% oxygen (8-10 L/min for 10-15 minutes), or dihydroergotamine• Preventive treatment:
• Short term prevention for subsequent attacks : prednisone at the beginning of a cluster cycle: 40-80 mg/d orally for 1 week discontinued by tapering the dose over the following week.
• Long term prevention : verapamil or lithium carbonate