* Branched chain AA
ValineLeucine
Isoleucine
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
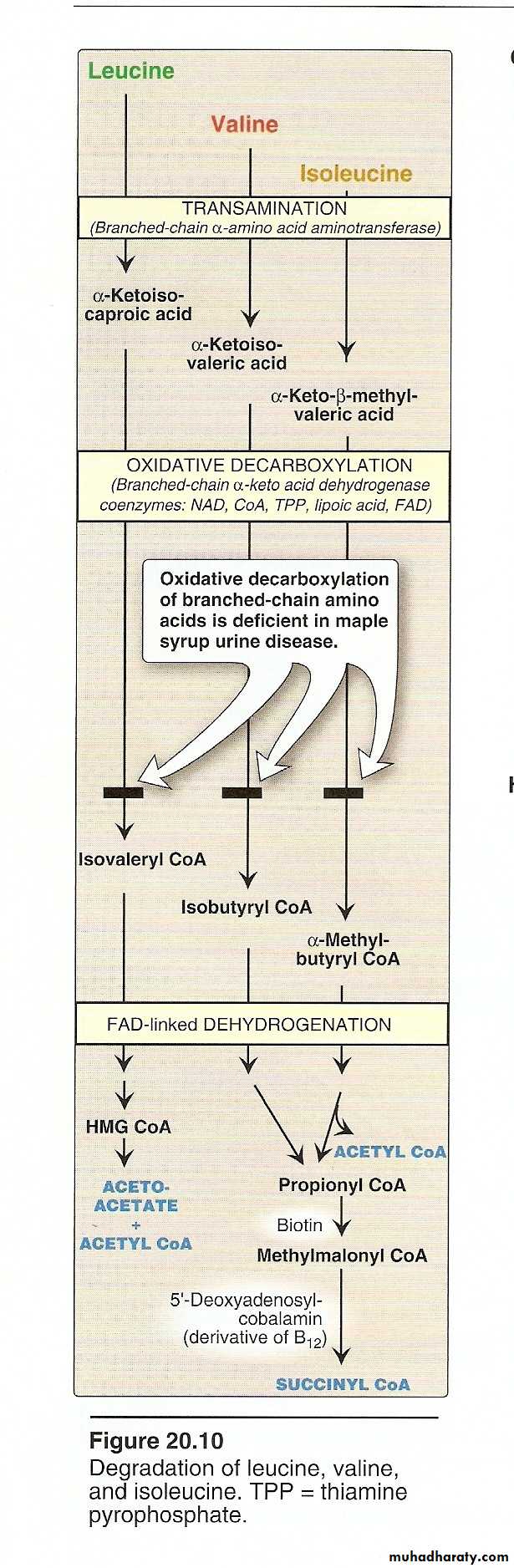
Valine,leucine and isoleucine are branched chain essential amino acids.
These three AA initially undergo a common pathway and then diverge to result in different end product.
Based on their product they are either glycogenic or ketogenic
Valine-------------glycogenic
Leucine------------ketogenic
Isoleucine-----------both glycogenic&ketogenic
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
The first three metabolic reactions are common to the branched chain amino acids
1. Transamination.
2. Oxidative decarboxylation.
3. Dehydrogenation.
Transamination: the 3AA undergo transamination to form their respective ketoacids.
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• Schematic presentation of metabolic pathways of Br. Chain Amino Acids
End result
Valine--------propionyl CoA--------GlucoseLeucine-------Acetyl CoA+Acetoacetate
Isoleucine------- Propionyl CoA + Acetyl CoA
Valine--------Glycogenic
Leucine------- Ketogenic
Isoleucine------Both
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Metabolic Disorders of Branched Chain A.A.
Maple Syrup Urine Disease
Autosomal recessive disease.
Block in the metabolism of leucine, Isoleucine.
The oxidative decarboxylation of αketoacids do not occur.
Branched chain ketoacids accumulate in the urine.
Occurs at the end of the Ist week of life.
.
• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Intolerance to milk.
Mental retardation.
Smell of the urine is just like burned sugarDiagnosis by urine chromatography.
Harmful untreatable disease.Extensive brain damage in those who survive.
Death occurs at the end of Ist year.• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
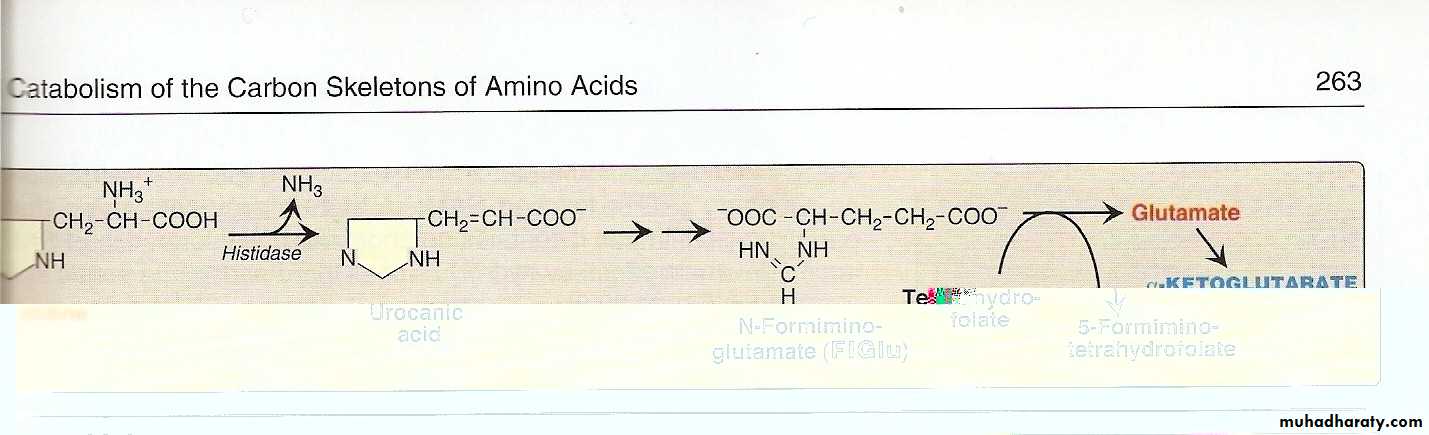
Histidine:
Usually metabolized through histidase which act on histidine to split off ammonia and form urocanate.
• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Histidine on decarboxylation ,gives the histamine which regulate HCl secretion by gastric mucosa
Histidinemia: due to defect histidase.
High level of histidine.
Mentally retarded with defect in speech
Harmful untratable
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
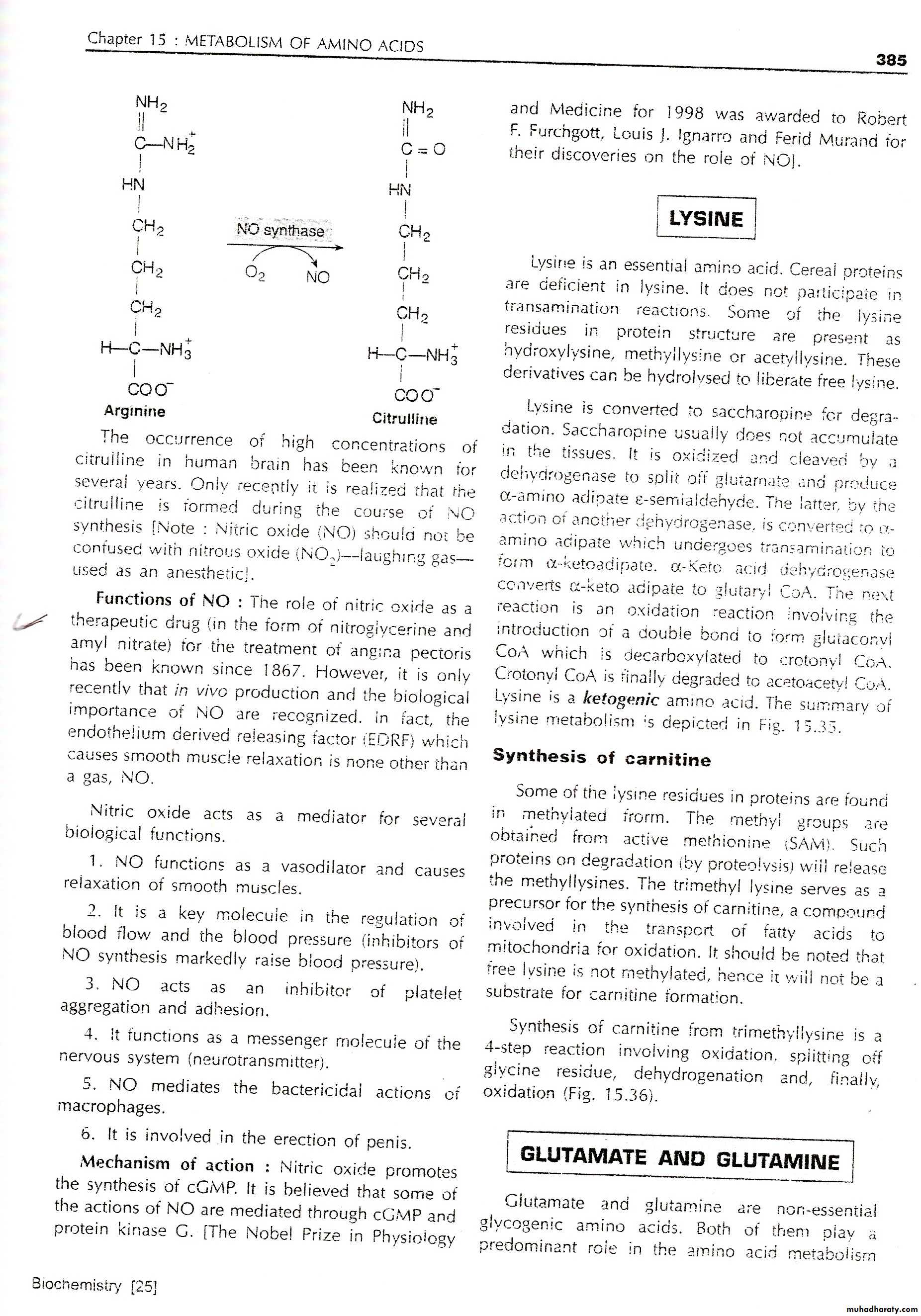
Arginine:
Arginine is cleaved by arginase to give urea and produce ornithine
Hyperargininemia is inborn error of metabolism of arginine due to the defect in the enzyme arginase.
Nitric oxide(NO): arginine is the substrate for the production of nitric oxide(NO)by the enzyme nitric oxide synthase
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• Function of NO
• It acts as endothelial derived releasing factor (EDRF) and cause smooth muscle relaxation. (General)
• NO functions as a vasodilator and muscle relaxant.
• It is the key molecule in the regulation of blood flow and the blood pressure.
• NO acts as inhibitor of platelets aggregation and adhesion.
• It functions as a messenger molecule of the nervous system (neurotransmitter).
• NO mediate the bacterial action of macrophages.
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Aminoaciduria
Excessive excretion of A.A. in urine.
2Types:
1.Overflow Aminoaciduria.
2.Renal Aminoaciduria.
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Renal Aminoaciduria:
Defective in reabsorption of AA while the renal threshold is normal.
• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Overflow A.A. presented to the glomerulous over the renal threshold( above the reabsorptive ability of the tubules) either due to overproduction or due to accumulation of A.A
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Renal Aminoaciduria:
Defective in reabsorption of AA while the renal threshold is normal.
Specific
Overflow------------
Non specific
Renal------------- Specific
Non specific• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Overflow Specific: inherited diseases of AA metabolism presented to the glomerulous in a large amounts above the renal threshold.
Phenylketonuria
Tyrosinemia
Homocystinuria
Maple syrup Disease
• A
• m• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Overflow non specific: AA presented to the glomeruli are different AA not related to each other over the renal threshold excreted in large amount in urine .
Chronic Hepatitis
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Renal SpecificAA:defective reabsorption
Group of AA related to each other share in their structures.
Hartnup disease defective absorption of tryptophan in the intestine)& (defective reabsorption in the tubules)
Cystinuria(group of related AA (cysteine glycine arginine
• A• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
Renal non specific: loss of more than one AA not related to each other due to defective reabsorption ability.
Fanconi Syndrome
Acquired condition due to defect in renal tubules usually multiple , (Generalized aminoaciduria).
Phosphate, Glucose, Bicarbonate Loss)
(Proximal renal tubular acidosis)
It may be inherited or secondary to other conditions
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
In general(my be regarded as a role)
All AA that are specific due to inherited disorders while all AA that are non specific are acquired due to diseases process.
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
31
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
32
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
34
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M
• A
• m
• I
• n
• o
• A
• c
• I
• d
• S
• M
• E
• T
• A
• B
• O
• L
• I
• S
• M