InflammationAcute &Chronic
Dr. Nadwa Subhi Al-azowINFLAMMATION
Inflammation is the response of living tissues to cell injury. Its purpose is to localize & eliminate the causative agent, to limit tissue injury & then to restore the tissue to normality or as close to normality as possible.Often beneficial, but sometime harmful.
Nomenclature: itis (after name of tissue) e.g.,
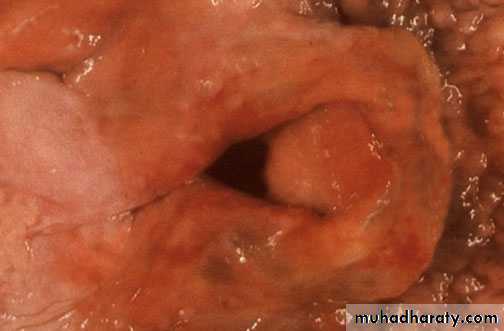
Appendicitis
Dermatitis
Cholecystitis
The cardinal signs of inflammation
● redness● heat
● swelling
● pain
● loss of function.
Causes of Inflammation:
1.Infections:e.g., bacterial, viral, parasitic fungal etc.2.Physical agents: e.g., heat, cold, radiation, etc
3.Chemical agents: e.g., acid, alkaline, drugs, etc.4.Hypersensitivity: e.g., rheumatic fever, ect.
5.Tissue necrosis: e.g., Ischemic necrosisMain Functions of Inflammatory response
1.Dilute,destroy and wall off injurious agents.2.Start process of healing.
Types of inflammation
1.Acute inflammation.
2.Chronic inflammation.
3-Acute on chronic inflammation.
Acute inflammation
Initial reaction of vascularized tissue to injury.
Neutrophils are predominant inflammatory cells in early stages (6 - 24 hours).Monocytes ( macrophages) predominate inflammatory cells in later stages (24 - 48 hours).
Vascular changes1) Change in caliber
Initially arteriolar vasoconstriction.Then arteriolar vasodilatation.
2) Increase permeability
Hallmark of acute inflammation.Result in marked outflow of fluid into interstitial tissue ( exudate).
Ending in increase blood viscosity & slowing of the circulation (stasis).
Mechanisms of increased vascular permeability
Endothelial cell contraction (venules)
Reversible due to histamine, bradykinin, leukotrienes.
Immediate transient response (15-30 min.).
Cytoskeletal reorganization, Junctional retraction, (venules & capillaries)
Reversible, due to interleukin 1 (IL-1), TNF & hypoxia.Direct endothelial injury (any vessel)
Irreversible, seen with severe injuries (burns or infections).Causes necrosis & detachment of endothelial cells.
Leukocyte-mediated endothelial injury (venules, pulmonary & glomerular capillaries)
Irreversible due to free radical & protease of leukocytes.Increased transcytosis (venules)
Reversible due to VEGF secretion.Causing widening & increased number of intracellular transcytoplasmic channels.
Leakage from new blood vessels
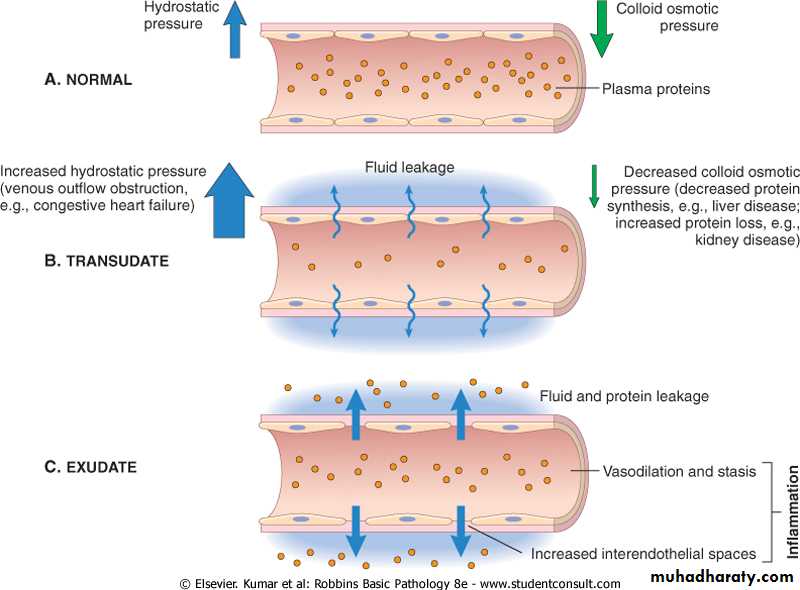
Edema: excess fluid in interstitial tissue or body cavities. May be either an exudate or transudate
Transudate: an extra vascular fluid with low protein content and a specific gravity of less than 1.012,essentially an ultra filtrate of blood plasma resulting from elevated fluid pressures or diminished osmotic forces in the plasma.
Exudate
Due to increase vascular permeability induced by chemical mediators and due to the direct damage of the vessels.It is consist of:
1.Fluid rich in plasma proteins.2.Fibrin.
3.Cells: Neutrophils, Macrophages, eosinophils, few lymphocytes & red blood cells.
4.Debris.
Vascular changes and fluid leakage during acute inflammation lead to Edema in a process called Exudation
Transudate
result of hydrostaticor osmotic imbalance
ultra filtrate of plasma
Low protein content
specific gravity < 1.015
Exudate
result of inflammation
vascular permeability
high protein content.
specific gravity >1.020
What are the function of EXUDATE?
It is in continuous turnover and have the following useful functions:1.It dilutes toxins.
2.It contains fibrin which localize infection.
3.It carries oxygen, nutrients to the inflammatory cells.
4.It carries Drugs, antibodies against bacteria.
It may have harmful effects e.g. causing life-threatening hypersensitivity reactions, or relentless and progressive organ damage from chronic inflammation and subsequent fibrosis ( e.g. rheumatoid arthritis, atherosclerosis).
Leukocyte activation: series of WBC responses that follow binding of chemotactic factors to their receptors on the cell membrane.
This result in
Secretion of chemical mediators, degranulation & oxidative burst.Arachidonic acid metabolism.
Increase number & affinity of adhesion molecules.
Chemotaxis.
Leukocyte cellular events in acute inflammation
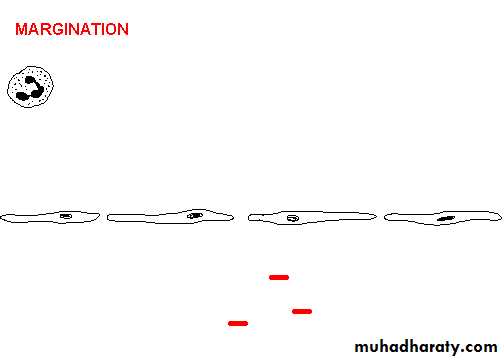
1) Margination (pavement) & rollingWith slowing of the circulation, leukocytes accumulate along vascular endothelial surface (Margination or Pavement).
Then they tumble on the endothelial surface, transiently sticking on the way (rolling) using selectins adhesion molecules.
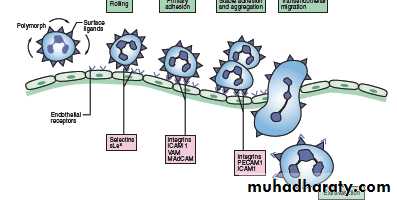
2) Adhesion & transmigration
More firm & stable sticking of leukocytes to endothelial surface (adhesion) using integrins adhesion moleculeThen leukocytes pass between endothelial cells along the intercellular junction (transmigration) using PCAM-1
3) Chemotaxis & activation
Chemotaxis: WBC locomotion towards site of injury along a chemical gradient due to action of chemotaxins.Types of chemotaxins:
Exogenous: bacterial products
Endogenous:
C5a (complement factor)
LTB4 (lipo-oxygenase pathway)
IL-8 (Cytokines)
PAF
4) Phagocytosis & degranulation
Affecting neutrophils & macrophages.Three steps
1-Recognition & attachment
facilitated by coating of microorganisms by serum proteins called OPSONINS. Mainly IgG & C3b that bind to Fc & C receptors on the WBC.
2-Engulfment
through formation of pseudopodia, phagosome, phagolysosome.
3-Killing or degradation
through formation of free radicals (Superoxides, hydrogen peroxide (H2O2) & hydrochloride (HOCL) ).
H2O2-MPO-halide system is the most bactericidal system .
oxygen independent pathway.
5) Release of leukocyte products
These include:
Lysosomal enzymes (protease).Oxygen-derived active metabolites (free radicals).
Products of arachidonic acid metabolism (lipo-oxygenase & cyclo-oxygenase products) .Diapedesis
Passage of RBCs through the defect created by the WBCs.It is a passive process.