Drug Interactions
(Drug-Drug Interactions)Drug – Drug interaction:
It is the modification of the effect of one drug (the object drug )By
The prior or concomitant administration of another (precipitant drug).
Risk Factors for Drug Interactions
High Risk Patients
Elderly, young, very sick, multiple disease multiple drug therapy, Renal, liver impairment
High Risk Drugs
Narrow therapeutic index drugs e.g.(digoxin , warfarin , theophylline recognized enzyme inhibitors or inducers
Site of interaction:
Outside the body. Inside the body.
Outside the body:
Reaction of IV drugs resulting in solutions after mixing that are not longer safe for the patient alter stability(change the PH) or structure leading to:
Loss of drug activity
Formation of precipitates.
Development of toxic product
Penicillin and aminoglycoside should never be placed in the same infusion fluid because of formation of inactive complex.
Protamine zinc insulin + soluble insulin lead to reduces the immediate effect of the dose.
With calcium – ceftriaxone precipitates in the lung and kidneys premature neonates.
Drug Interactions Inside the body
Pharmacokinetics drug interactions
Pharmacodynamics drug interactions
Pharmacokinetics drug interactions
Involve the effect of a drug on another from the point of view that includes :
Absorption
Distribution
Metabolism
Excretion
Interaction at the site of absorption
1. Formation of drug Chelates or complexes.2. Altered gut Flora
3. Altered GIT Motility.
4. Altered PH
5. Drug induced Mucosal damage
6. Malabsorption caused by other drugs
7. Interaction other than in the Gut
1. Direct chemical interaction . in the gut and formation of drug Chelates or complex
Calcium (milk), iron, anti acid (Al or Mg hydroxide) +Tetracyclin insoluble complex
levothyroxine ,digoxine and some acidic drugs e.g warfarine +
Colestyramine decrease their absorption
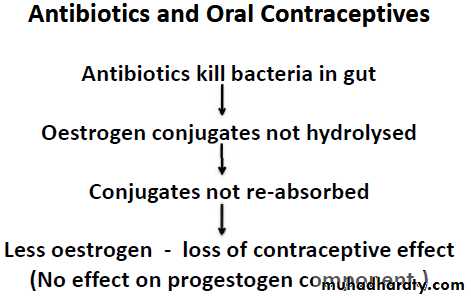
2. Altered intestinal bacterial flora
Antibiotics kill a large number of the normal flora of the intestine Antimicrobials may potentiates Oral anticoagulant by reducing bacterial synthesis of vitamin K, in 10% 0f patients receiving Digoxin…..40% or more of the administered dose is metabolized by the intestinal flora Increase digoxin conc. and increase its toxicity
3. Altered gut motility
Slowing of gastric emptying such as antimuscarinic drugs and opiate analgesics anticholinergics + acetaminophenImpact: delay in absorption of acetaminophen
OR
Accelerated by drugs e.g metclopromide which hasten gastric emptying
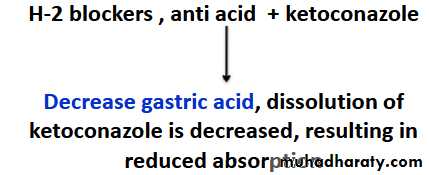
4. Altered PH.
The non-ionized form of a drug is more lipid soluble and more readily absorbed from GIT than the ionized form does.
Therefore, These drugs must be separated by at least 2h in the time of administration.
5. Drug-induced mucosal damage:
Colchicine (which cause local Mucosal damage) can decrease absorption of poorly absorbed drugs e.g. (digoxin, phenytoin)
6-Malabsorption caused by other drugs
Orlistat (Xenical) Inhibits pancreatic lipases , preventing hydrolysis of ingested fat)
Orlistat (Xenical) + fat soluble vitamins (A,D,E,K)
malabsorption of Fat-soluble vitamins
7. Interaction other than the gutAddition of vasoconstrictors e.g adrenalin to local anesthetics delay absorption and prolong local anesthesia
Effect of drug distribution
Displacement from plasma protein bindingIt depends on the affinity of the drug to plasma protein.
The most likely bound drugs is capable to displace others.
The free drug is increased.
Sodium valproates displaces phyentoin from its binding site on plasma
albumin in addition to inhibit its metabolism
Displacement from tissue bindings
Binding Quinidine with digoxin and cause increase concentration of free digoxin in addition to impair renal excretion
Altered drug metabolism
The effect of one drug on the metabolism of the other is well documented.The liver is the major site of drug metabolism CYP450 family is the major metabolizing enzyme in phase I (oxidation process).
Effect on drug metabolism
Enzyme induction : the drug called (inducer) a drug may induce the enzyme that is responsible for the metabolism of another drug or even itself e.g: carbamazepine (antiepileptic drug ) increases its own metabolism phenytoin increases hepatic metabolism of Oral
Contraceptives Leading to decreased level Reduced action and Unplanned Pregnancy
Phenobarbital + warfarin metabolism of warfarin (danger of thrombosis)
Enzyme inhibition:
It is the decrease of the rate of metabolism of a drug by another one.This will lead to the Increase of the concentration of the target drug and leading to the increase of its toxicity .
Cimetidine + Theophylline
cimetidine reduces the clearance of theophyllinecausing an increase in adverse effects
Inducer (carbamazepine) + Inhibitor (verapamil)
The effect of the Inhibitor will be predominantMost important enzyme Inhibitors
1. Cimetidine.2. Erythromycine.
3. Quinolones.
4. Sodium valproate.
5. Allopurinol.
Alterations in renal clearance
• Increase in Renal Blood Flow
• Inhibition of Active Tubular Secretion
• Alterations in Tubular Reabsorption
Increase in Renal Blood Flow
hydralazine + digoxinhydralazine increases the renal clearance of digoxin
• Active tubular secretion:It occurs in the proximal tubules.
The drug combines with a specific protein to pass through the proximal tubules.
When a drug has a competitive reactivity to the protein that is responsible for active transport of another drug this will reduce such a drug excretion increasing its conce.
probenecid + penicillin
Decreases tubular secretion of pecicillin• Passive tubular Reabsorption
Acidification of urine increases reabsorption and decreases excretion of weak acids, and, in contrast, decreases reabsorption of weak bases.Alkalinization of urine has the opposite effect.
In some cases of overdose, these principles are used to enhance the excretion of weak bases or acids
e.g. sodium bicarbonate + salicylates(weak acid) decrease reabsorption and Increase excretion of salicylates
Pharmacodynamics Interaction
Pharmacodynamics are related to the pharmacological activity of the interacting drugs .
Both drugs act on the target site of clinical effect.
Synergism
Summation or Additive
Potentiation
Antagonism
Results of drug interactions:
Synergism : occurs when the effects of 2 drugs having the same action or increase the action of another drugs
1-Summation(Additive):
Ex. β-adrenoceptor blocker + thiazide additive anti hypertension effect 1+ 1 = 2
2-Potentiation:
When one drug Increase the action of another 1 + 1 = more than 2
Ex. Trimethprim + sulfamethaxazole
Antagonism
When the action of one drug opposes the action of another.
1 + 1 = 0 (or 0.5)
Ex. Histamine and Adrenaline on bronchi (physiological antagonism)
Flumazenil and diazepam they compete reversibly for the same drug
Receptor (competitive antagonism)
Interactions directly on Receptor or body system
Actions on receptors
Beneficial interaction naloxone for morphin over dose (opiod receptor) Unwanted interaction atenolol + cold remedies containing ephedrine or Phenylephrine loss of antihypertensive effect
Action on body system
NSAIDs especially indomethacin + α adrenoicepter blocker lead to loss some antihypertensive efficacy by inhibition of production of vasodilator prostpglandins by the kidney leading to sodium retentionOnset of drug interaction
• It may be seconds up to weeks• For example in case of enzyme induction, it needs weeks for protein synthesis
• while enzyme inhibition occurs rapidly.
END