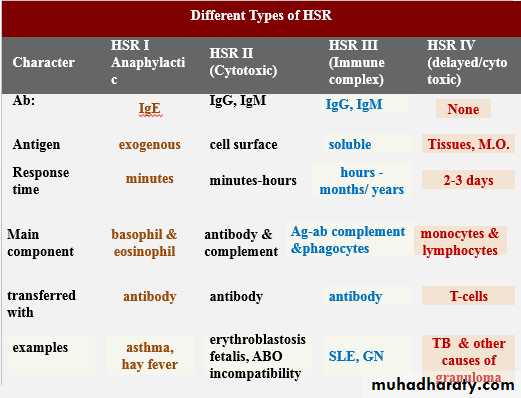
Type II HSR
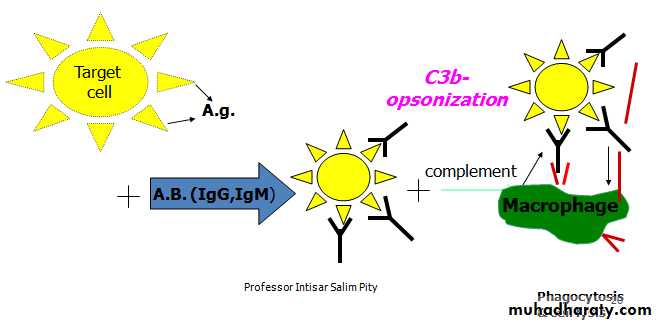
The antigen is on the surface of cells + Ab →→ Ag-Ab reaction may be one of three effects:1- Complement dependent HSR (opsonization & phagocytosis)
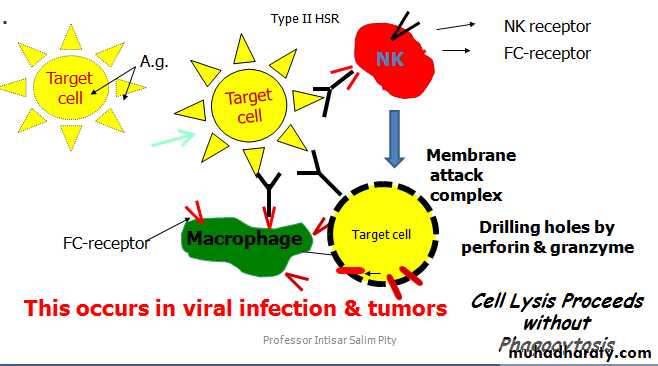
2- Antibody dependent cellular cytotoxicity
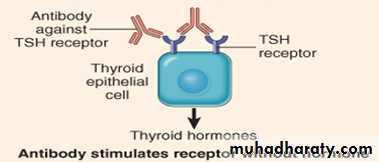
Antibody mediated cellular dysfunction 3-
Type II hypersensitivity
1. Complement dependent HS-reactions
Complement activation and lysis of the target cells after opsonization & phagocytosis. The complement here is C3b, the Ig is IgG, IgM
Clinical examples of HSR II
Complement dependent reactions
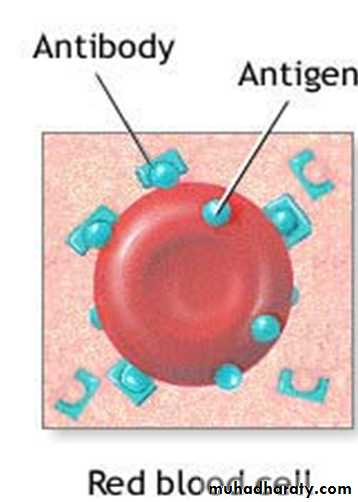
a- Autoimmune hemolytic anemia: There are auto-antibodies against the RBC-antigens. These auto-abs are of IgG or IgM type. Both can activate the complement and result in RBCs lysis or alternatively, IgG may opsonize the RBCs to be engulfed by the phagocytic cells in the spleen & liver.
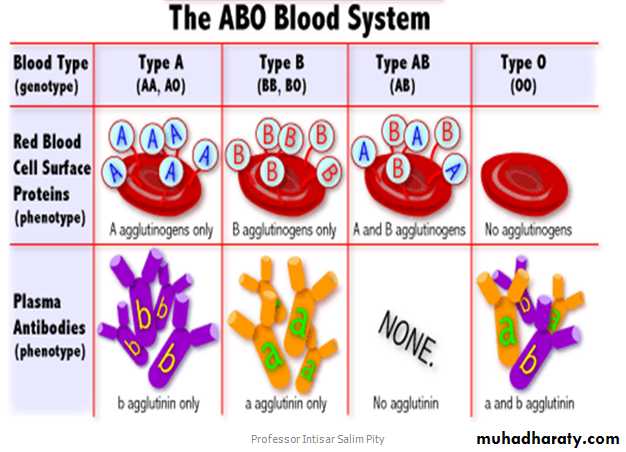
b- Mismatched blood transfusion
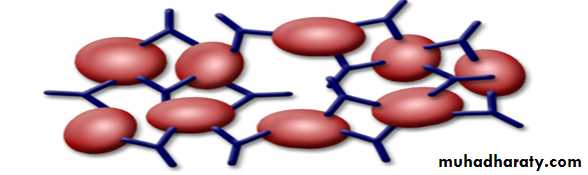
Mismatched blood transfusion can result in a severe and life threatening hemolysis. For example, giving a blood of group A to a recipient of blood group B, then the anti A antibodies in the serum of the recipient will agglutinate and damage the transfused RBCs of the donor.
c- Erythroblastosis fetalis, only occurs in cases of Rh-ve mother & Rh+ve foetus). The maternal anti-D (anti-Rh) antibodies, which are of IgG type pass through the placenta and destroy the fetal RBCs. (Unusual in the first pregnancy & the antibodies developed after previous exposure to D-antigen, i.e. Rh+ve blood)
2. Antibody dependent cellular cytotoxicity in which the antibody molecule provides a link between the natural killer cell (or macrophage) and the Ag on the surface of the target cell without phagocytosis & without activation of complement →Drilling holes by perforin & granzyme .
3. Ab- mediated cellular dysfunction
a. Sometimes antibodies are formed against specific receptor & block its effect.b. Hashimoto thyroiditis: Ab formed are against TSH receptor of thyroid epithelial cells, locking the site of TSH action, resulting in hypothyroidism.
c. Grave’s disease: Here the antibodies formed against TSH receptor of thyroid epithelial cells themselves act as TSH leading to continuous thyroid stimulation with a resultant thyrotoxicosis.
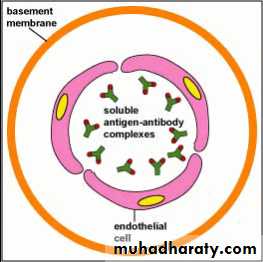
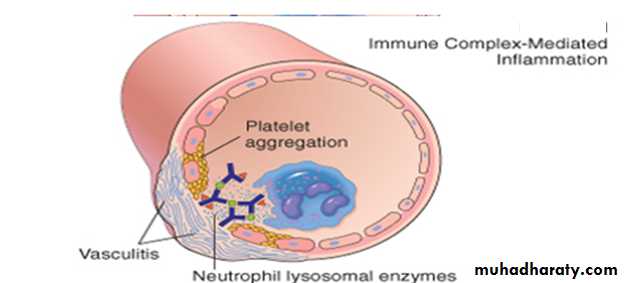
Type III HSR (Complex HSR)
Characterized by immune complex formation either locally in certain tissue or circulating in the blood & deposition in various tissues.
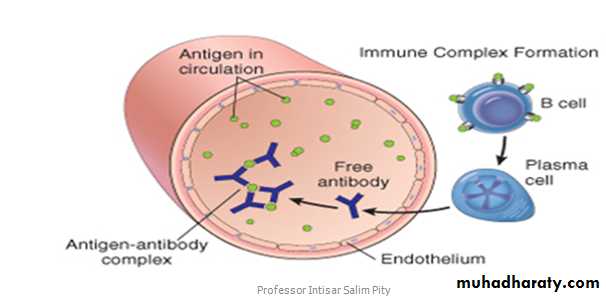
1. Binding of the antibodies (IgG, IgM) to the soluble antigen forming antigen-antibody complexes will activate the complement components (C3a, C4a, C5a, C5b).
2. Ag-ab complexes + activated complements in neutrophil emigration & cause vasodilatation and increased vascular permeability (i.e. acute inflammation). The end result will be tissue (endothelial) damage.
The process of inflammation of the wall of blood vessels is called vasculitis → Endothelial destruction → stimulates formation of thrombosis → may occlude the vessel lumen → tissue ischemia & necrosis of the organ or tissue supplied by that BV.
Clinical examples of localized HSR III
● Acute post-streptococcal glomerulonephritis which develops 1-2 weeks following throat infection. The streptococcal antigens pass into the blood, then antibodies develop against them and react to form the ag-ab complexes which precipitate on the basement membrane of the glomerular capillaries. These complexes will activate complement components and cause the inflammation (vasculitis) & endothelial damage. The patient presents clinically with hematuria and oliguria.Examples of systemic HSR III
A- Serum sicknessB- SLE
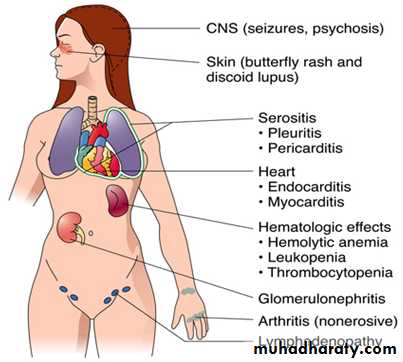
Systemic lupus erythematosus
● It results from auto-antibodies against nuclear components (DNA, histones, etc.). These are normally sequestered inside the nucleus where they are hidden from the antibodies, but they are released following tissue injury; e.g., a viral infection and are quickly bound by the patient own antibodies.● The antigen-antibody complexes will deposit in the basement membranes of the glomeruli, lungs, joints, skin, lymph nodes…etc, where they induce complement fixation, inflammation & tissue damage
Clinical Features of Systemic Lupus Erythematosus
Type IV hypersensitivity
● Type IV hypersensitivity is characterized by cell-mediated response rather than antibodies.● Specifically T lymphocytes are involved in the development of the sensitivity, hence called cell-mediated hypersensitivity.
● T lymphocytes (CD4+) are activated by a variety of non-degradable agents like bacteria, fungi and protozoa…etc.
Delayed HSR (Type IV HSR)
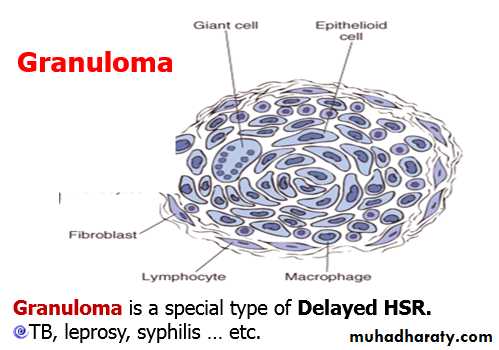
The antigen-specific CD4+ T cells will be activated → secretion of a variety of effector molecules (cytokines) → macrophage accumulation, activation & modification to epithelioid cells → granuloma.
Many epithelioid cells may unite together to form giant cells.
B- Cellular cytotoxicity:
This reaction is mediated by the cytotoxic CD8 +ve T-lymphocytes which recognized antigen on target cells.E.g.:
1- graft rejection
2- virus infection
3- tumor immunity
The cytotoxic CD8 +ve T-lymphocytes kill the target cells by perforin & granzyme.
End