LARYNXVoice Box
Dr. Basil SaeedAssistant Professor
Anatomy
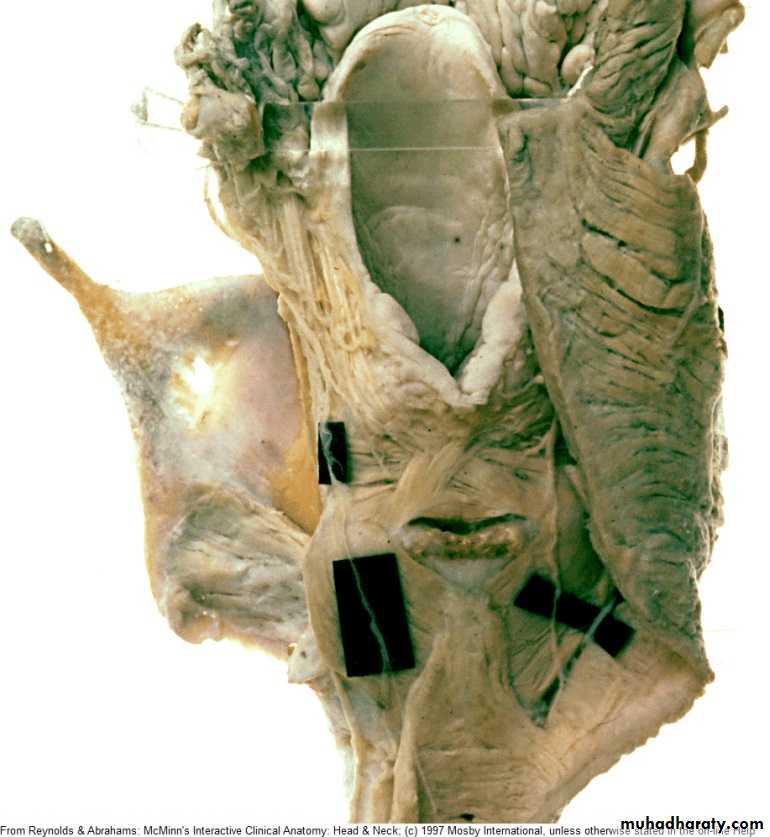
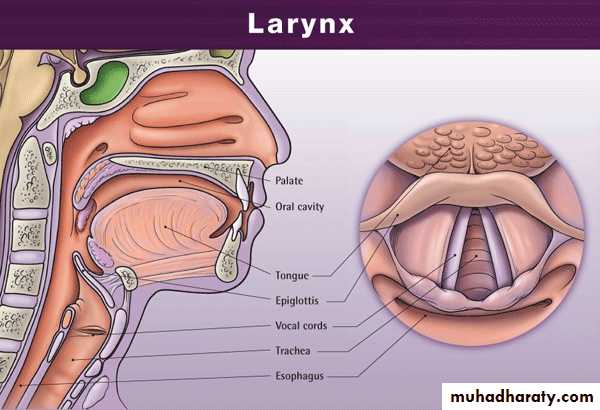
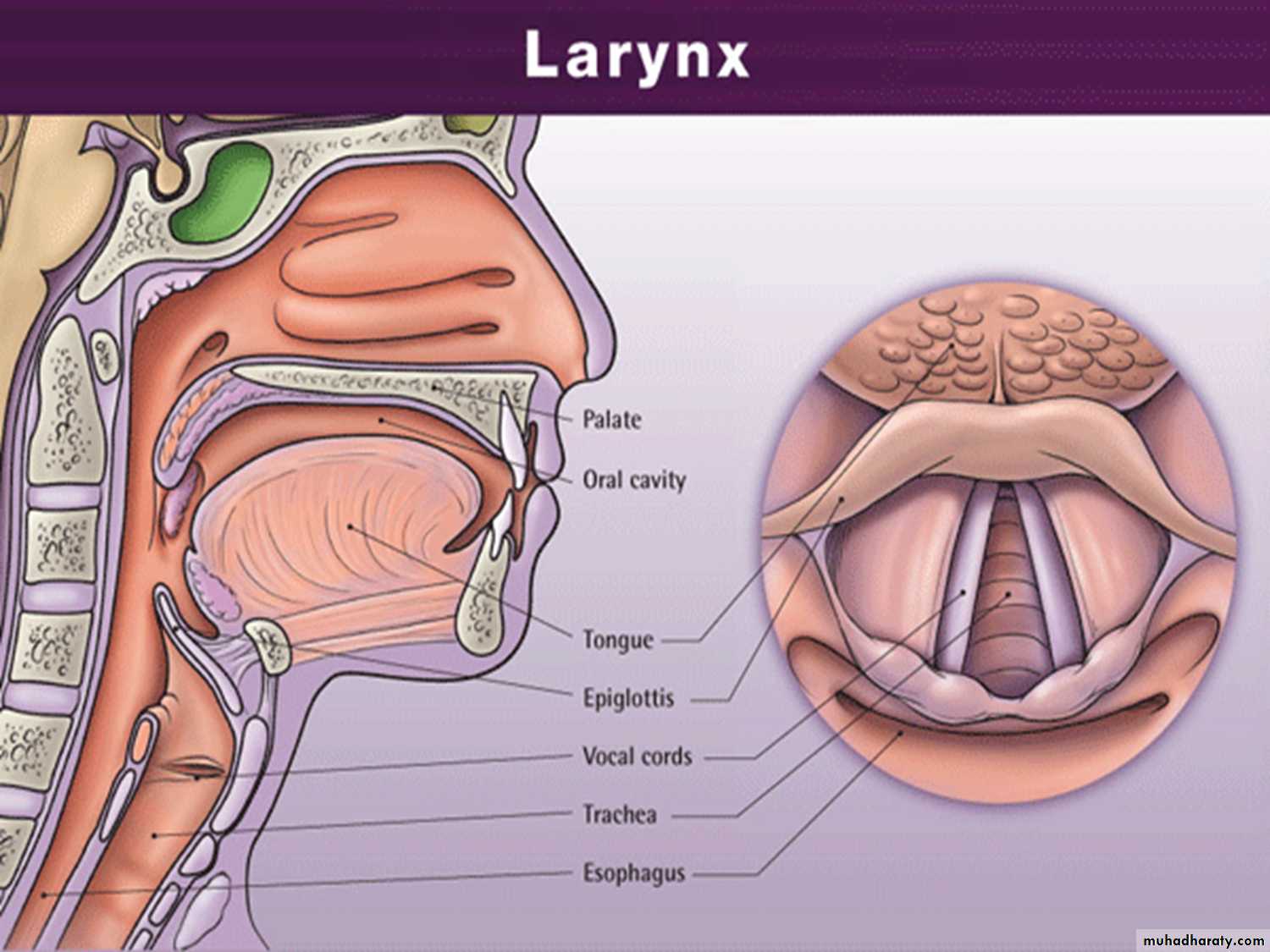
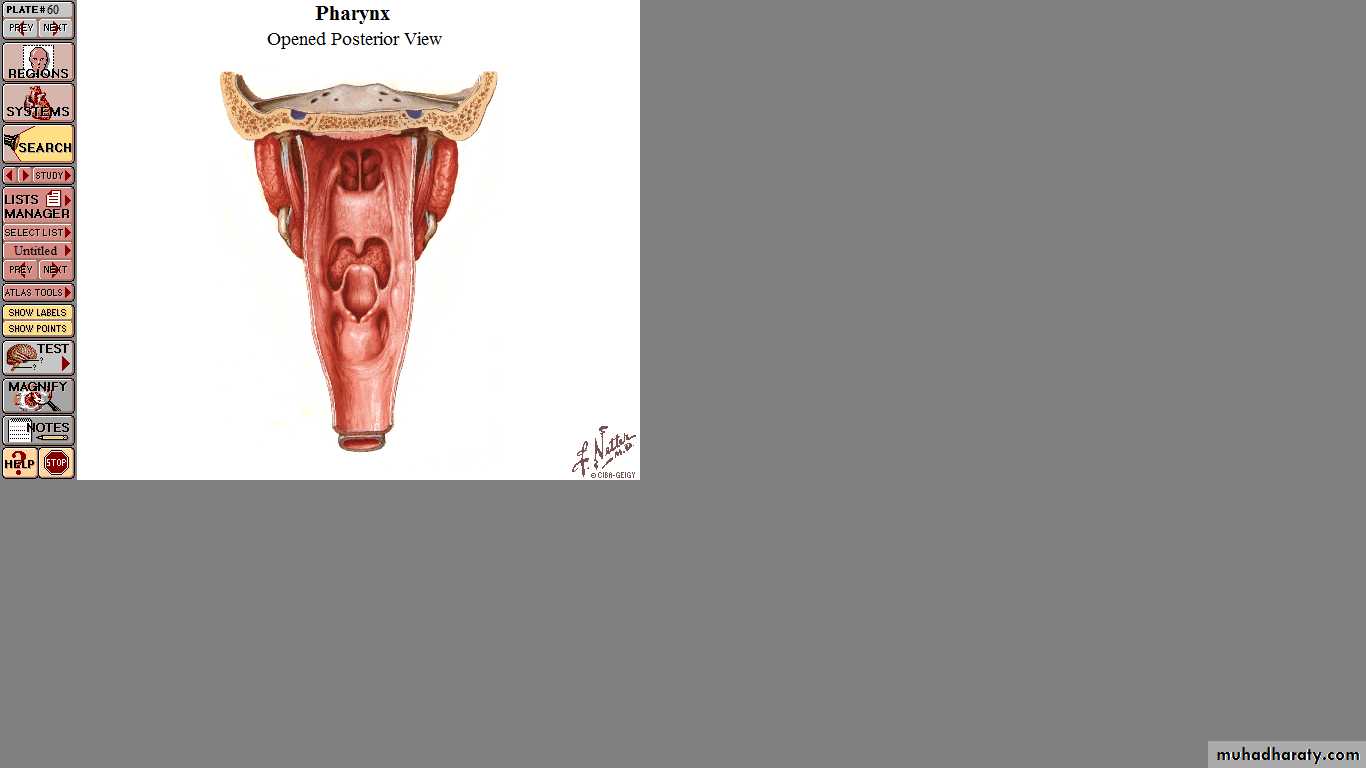
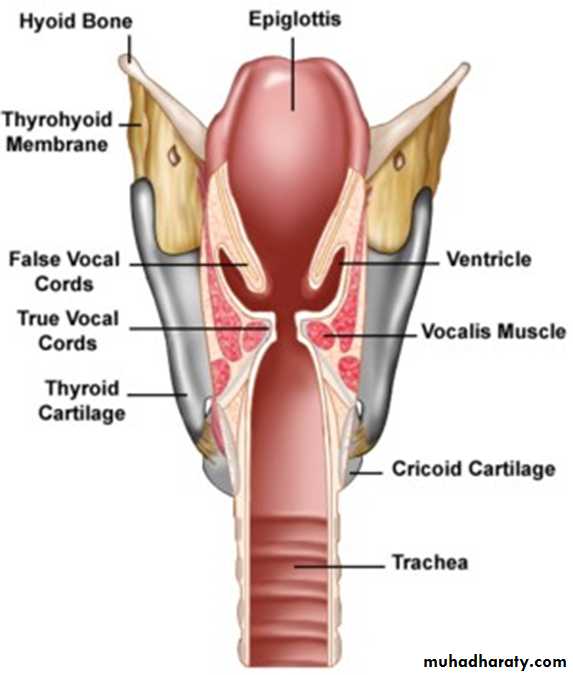
• - Situated in the midline of the neck, in front of the laryngopharynx from the level of the 3rd- 6th cervical vertebrae.It consist of a framework of cartilages, connected by ligaments, lined by a mucous
membrane and moved by
muscles.
•
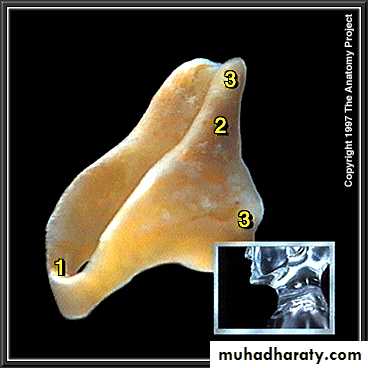
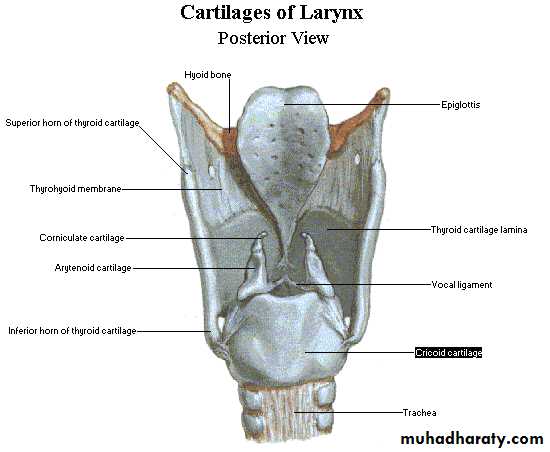
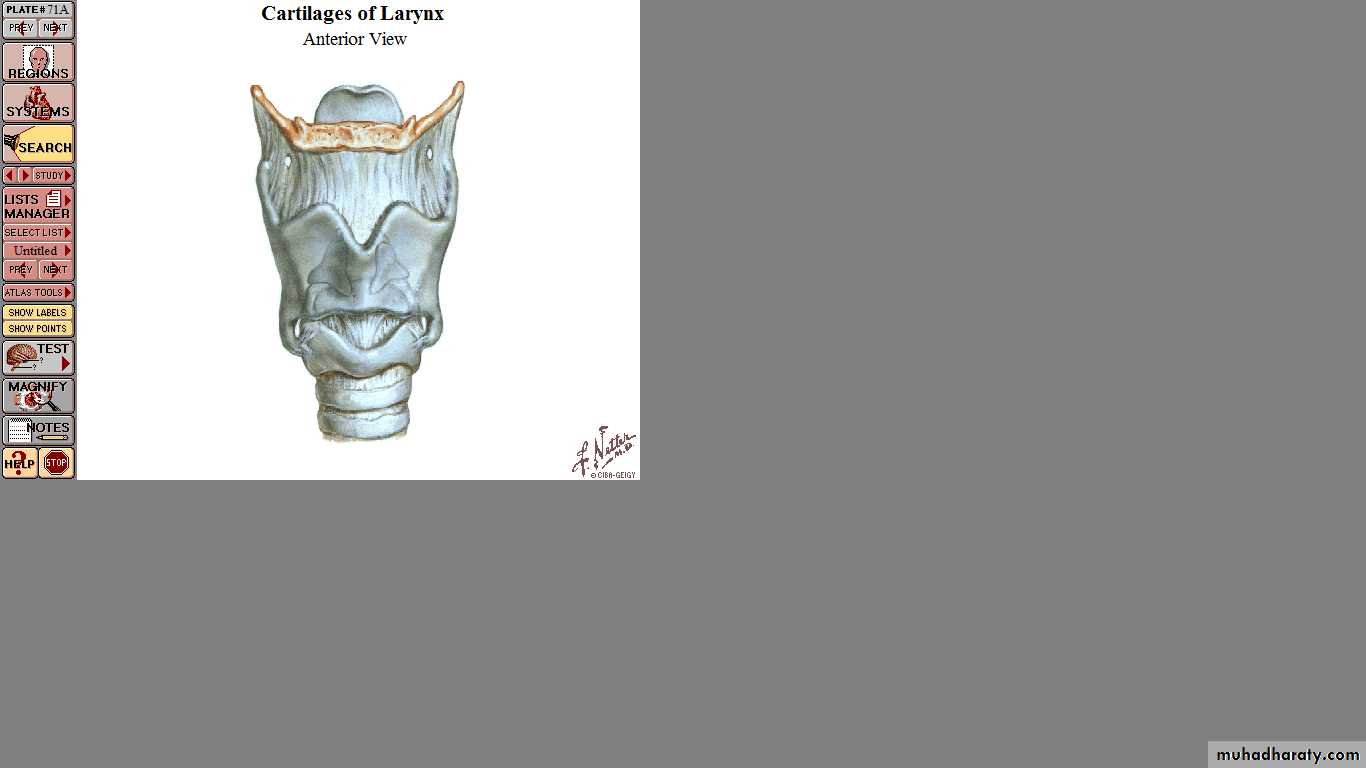
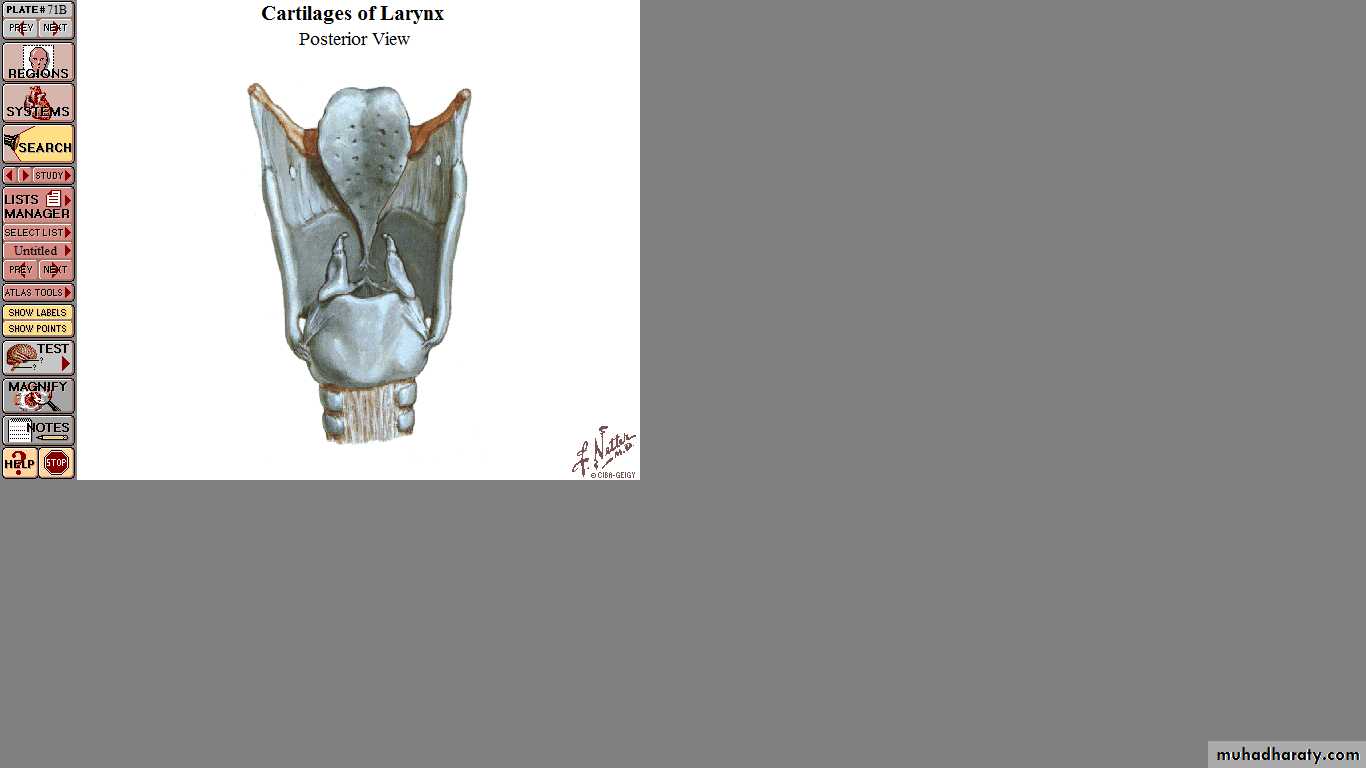
Unpaired Cartilages
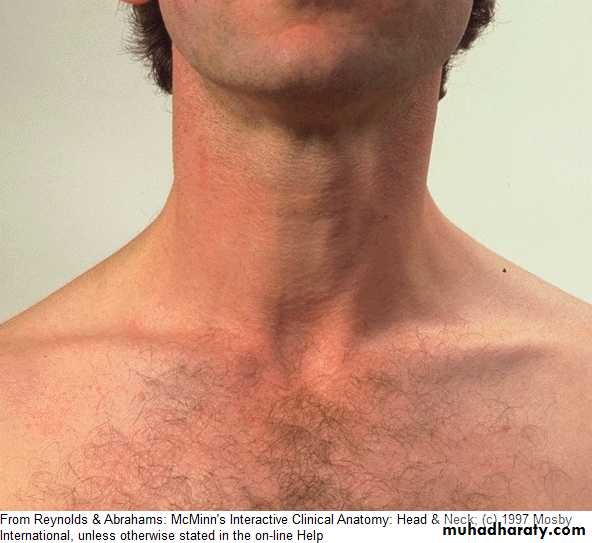
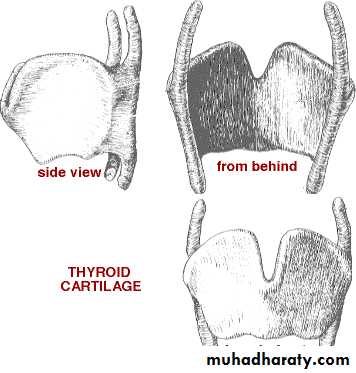
Thyroid CartilageThe largest cartilage.
Makes a prominence
In the front of the
Neck “Adam’s Apple”.
The two alae meet
anteriorly forming an
angle of 90 in males
and 120 in females.
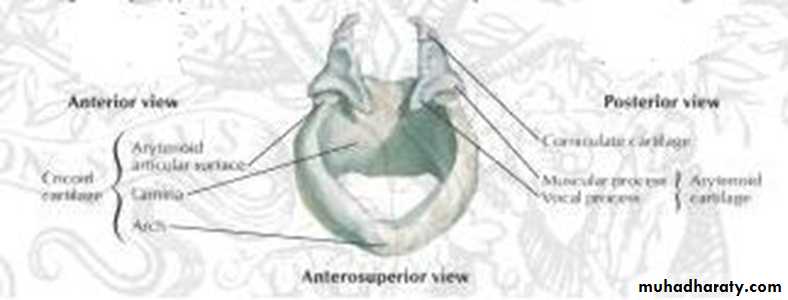
Cricoid Cartilage:
The only complete ring in the respiratory tract. Resembles a signet ring and lies below the thyroid cartilage.Connected anteriorly with the thyroid cartilage by cricothyroid membrane.
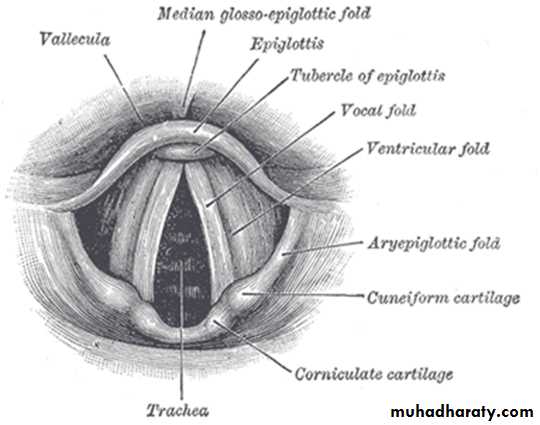
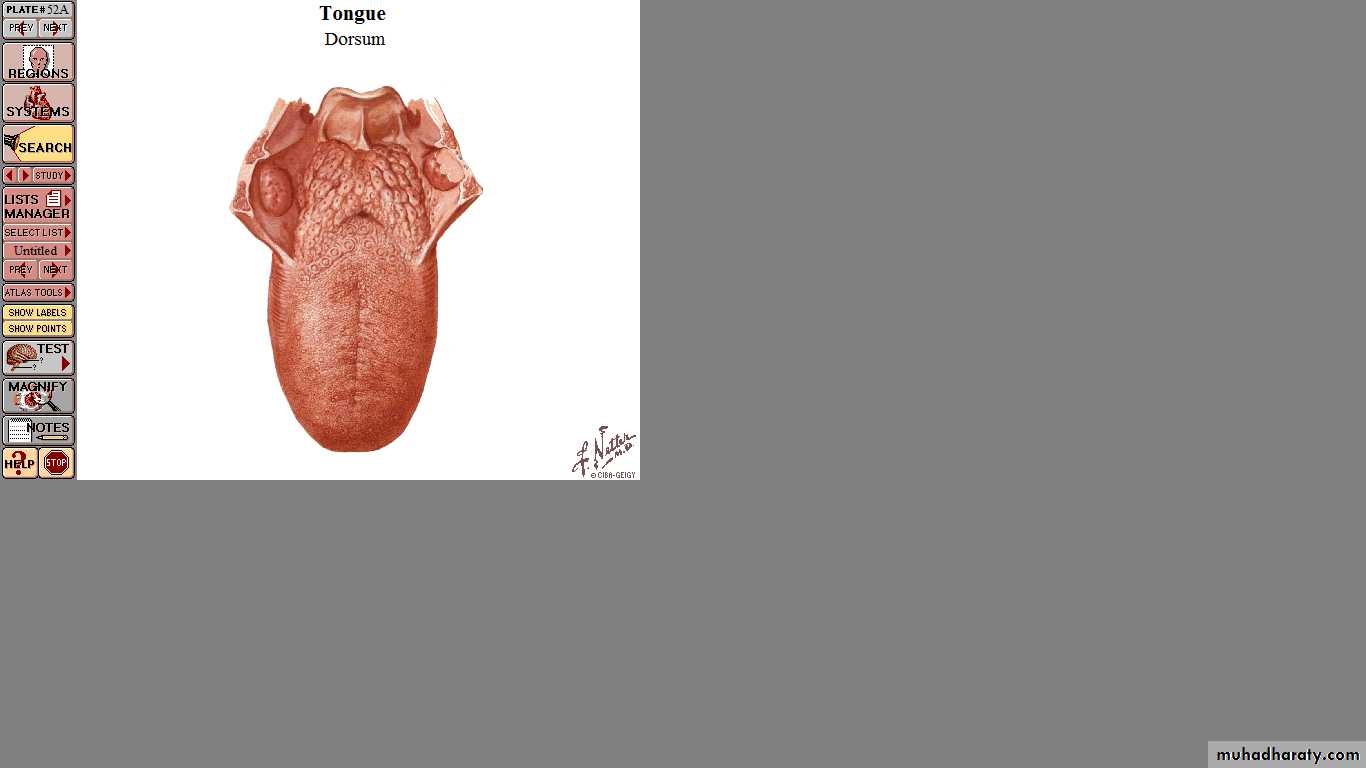
Epiglottis
A leaf-shaped piece of cartilage which is attached both to the base of the tongue and to the upper part of thyroid cartialge.
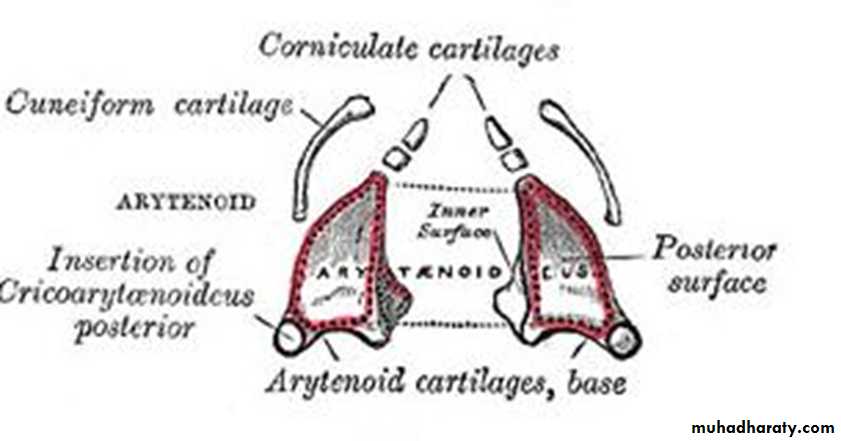
Paired Cartilages
Arytenoid Cartilages:Pyramidal in shape
The base articulates
with cricoids cartilage.
Anterior projection
((vocal process))
Lateral projection
((muscular process))
The aryepiglottic folds connect the arytenoids with the base of epiglottis and form the upper edge of the laryngeal inlet.
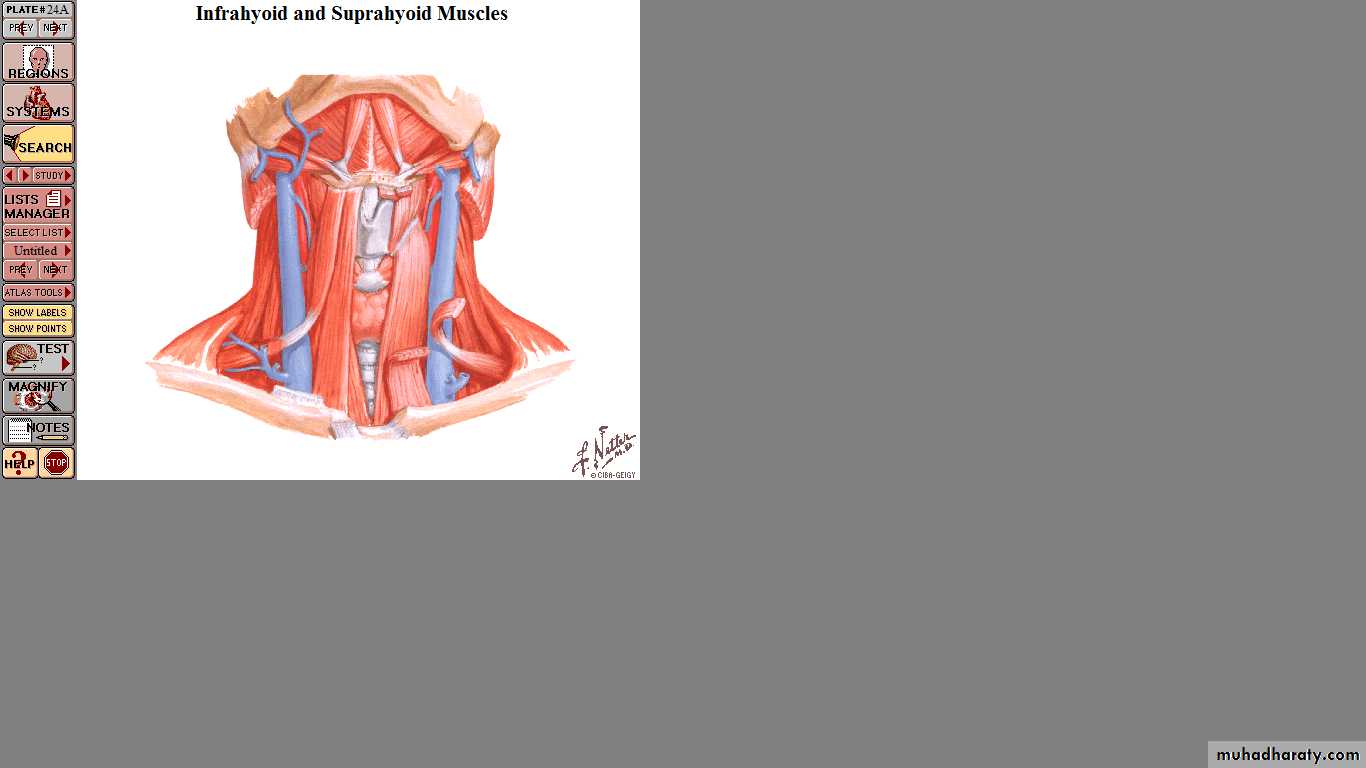
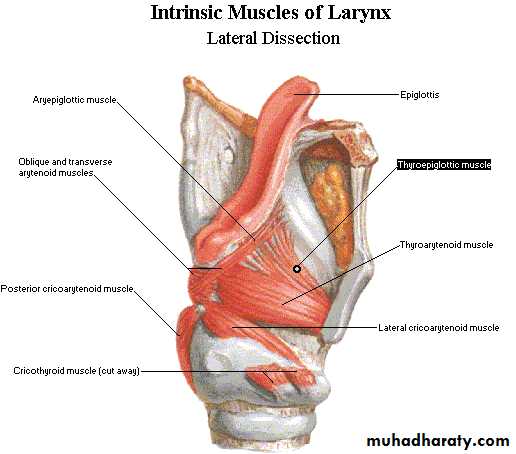
Laryngeal Muscles
Extrinsic: between the larynx and neighboring structures.The strap muscles of the neck (sternothyroid and thyrohyoid muscles).
The pharyngeal muscles (stylopharyngeus, palatopharyngeus and inferior constrictor muscles).
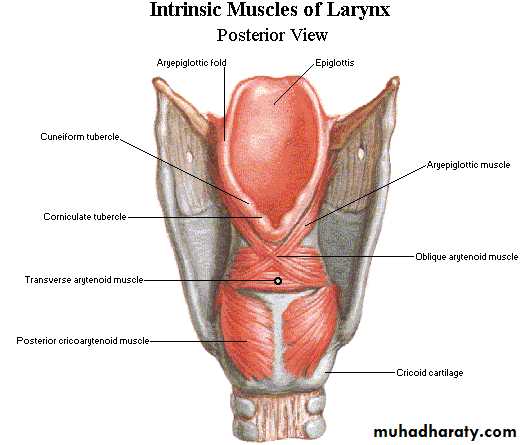
Intrinsic
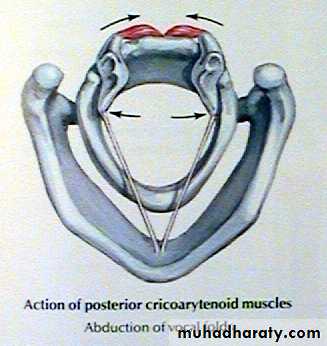
Abductors of the vocal cords: posterior cricoarytenoid.
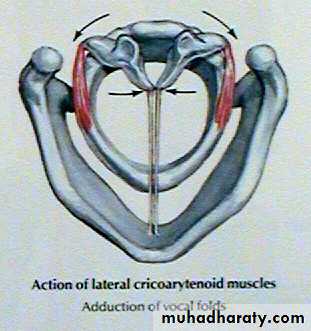
Adductors of the vocal cords:
1. Lateral cricoarytenoid muscle.
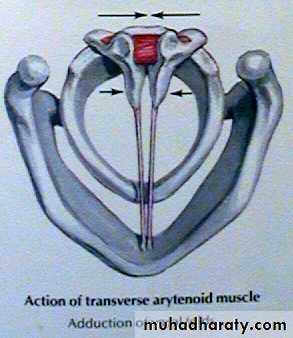
2. Interarytenoid muscle (Transverse arytenoid).
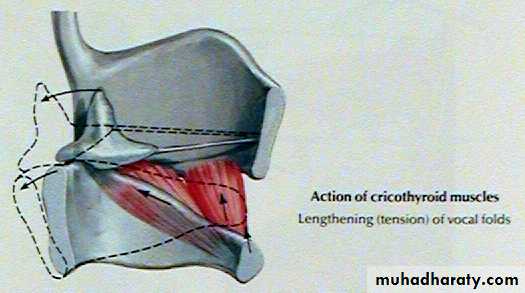
3. Cricothyroid muscle.
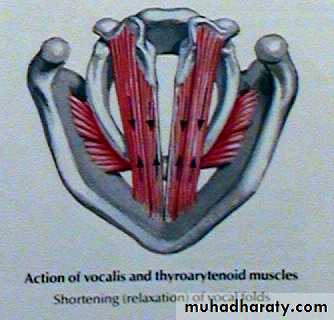
4. Thyroarytenoid muscle (vocalis).
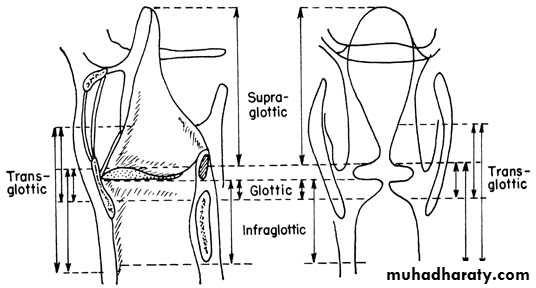
Laryngeal Cavity
The supraglottis fromthe inlet to the lower
part of the laryngeal
ventricle
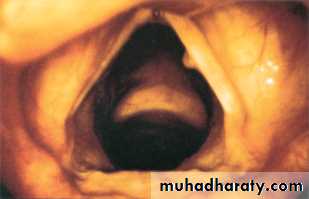
The glottis
comprises the vocal cords
and arytenoids.
The subglottis
below the cords.
The vocal cords are two fold-like structures extending from the thyroid cartilage to the vocal process of the arytenoid cartilage.
The covering epithelium of vocal cords is closely bound to the underlying structure and the blood supply is poor, hence the pearly white appearance.
The epithelium lining the larynx is ciliated columnar type except over the vocal cord where it is stratified squamous type.
Blood Supply
The region above the vocal cord is supplied by the laryngeal branch of the superior thyroid artery.Below the cords is supplied by the laryngeal branch of the inferior thyroid artery.
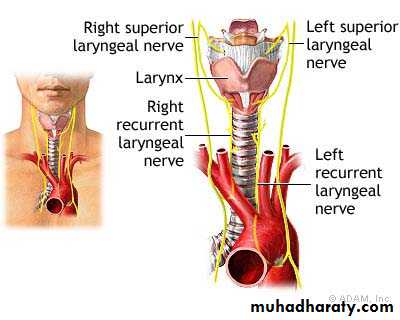
Nerve Supply
Sensory: Above the vocal cords is supplied by the internal laryngeal nerve, whereas below the vocal cords, the mucous membrane is supplied by the recurrent laryngeal nerve.
Motor: The recurrent laryngeal nerve,
except the cricothyroid muscle the external laryngeal nerve.
Lymphatic Drainage
The vocal cords have no lympahtic drainage and acts as a watershed dividing the supraglottis from the subglottis.The supraglottis drains to the upper deep cervical chain.
The subglottis drains to the prelaryngeal, pretracheal and the lower deep cervical chain.
Functions of the Larynx
1. Protection of the lower air passages by:Approximation of the aryepiglottic folds assisted by the epiglottis.
The apposition of the false cords.
The closure of the vocal cords.
Reflex cessation of respiration.
Cough reflex.
2. Phonation: voice is produced by vibration of the vocal cords and the sound is amplified by the resonating chambers of the mouth, pharynx, nose and chest.
3. Respiration: reflex adjustment of the glottis by abduction during inspiration and adduction during expiration.
4. Fixation of the Chest to increase the intrathoracic pressure.
Symptoms of Laryngeal diseases
Disorders of voiceHoarseness of voice: a rough, husky voice resulting from any abnormality in the vocal cords. There is change of voice from high to low pitch, and may even ends with aphonia.
Causes
* Congenital: laryngeal web.
* Inflammatory: acute and chronic laryngitis.
* Neoplastic: papilloma laryngeal carcinoma.
* Traumatic: external injury and intubation.
* Neurological: Vocal cord palsy (adductor).
* Vocal abuse: Vocal cord nodules and polyps.
Stridor:
Noisy breathing produced by turbulent air flow through a narrowed air passages.
Stridor is a physical sign and not a disease.
Causes
*Congenital: laryngomalacia and subglottic stenosis.
*Trauma: thermal, chemical and surgical.
*Foreign body: larynx or trachea.
*Infective: epiglottitis and croup.
*Neoplastic: papilloma, laryngeal carcinoma.
*Neurological: bilateral vocal cord palsy (abductor).
Sore throat
Cough: dry and irritating cough may reflect laryngitis or a F.B.Haemoptysis: may be due to infection or neoplastic causes.
Laryngomalacia
Most common laryngeal congenital abnormality.It is characterized by excessive flaccidity of supraglottis which is sucked in during inspiration producing stridor.
The condition manifests at birth or soon after and usually disappears by 2 years of age. Characterized by stridor which is classically inspiratory, worse when the baby is active and relieved by prone position.
•
On Exam.
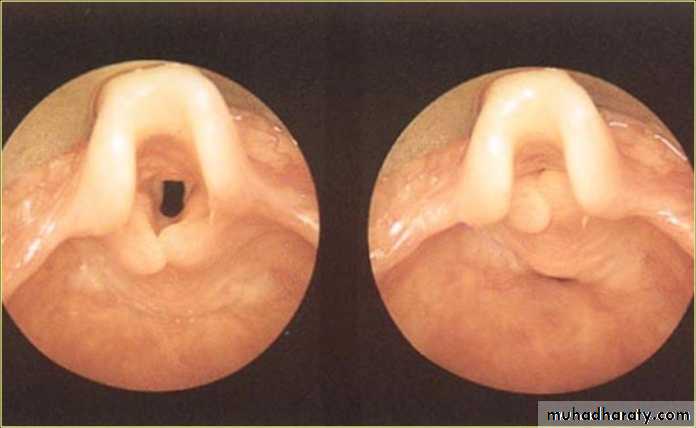
The diagnosis is made at endoscopy with the child breathing spontaneously.Classical appearance include an omega-shaped epiglottis, short aryepiglottic folds and loose redundant mucosa over the arytenoids.
On inspiration, the cartilages are sucked inwards obstructing the airway.
Treatment
Parental reassurance.
Tracheostomy in severe cases.
Acute LaryngitisADULTS
An acute superficial inflammation of the laryngeal mucosa.
Aetiology:
Infection: Its most frequently caused by adeno or influenza viruses but secondary bacterial infection may supervene. Acute laryngitis occurs as part of respiratory tract infection or as an isolated disease.
Trauma: Vocal abuse or endoscopic manipulation.
Irritation: Inhaled fumes, smoking .
Clinical Picture
Hoarseness of voice or aphonia, sore throat.Dry and irritative cough.
Generalized symptoms: malaise and fever.
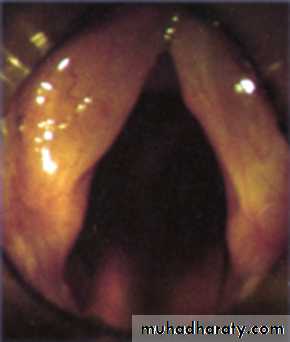
On examination: Indirect and fibroptic laryngoscopy reveals:
Redness and oedema of the larynx.
The vocal cords are covered with mucous and pus.
Treatment:
Bed rest and vocal rest.
Avoidance of tobacco and irritating agents.
Steam inhalation.
Systemic antibiotics if there is secondary bacterial infection.
Acute Laryngitis
An acute superficial inflammation of the laryngeal mucosa.
Aetiology:
Infection: Its most frequently caused by adeno or influenza viruses but secondary bacterial infection may supervene. Acute laryngitis occurs as part of respiratory tract infection or as an isolated disease.
Trauma: Vocal abuse or endoscopic manipulation.
Irritation: Inhaled fumes, smoking or alcohol abuse.
Clinical Picture
Hoarseness of voice or aphonia, sore throat.Dry and irritative cough.
Generalized symptoms: malaise and fever.
On examination: Indirect and fibroptic laryngoscopy reveals:
Redness and oedema of the larynx.
The vocal cords is covered with mucous and pus.
Treatment:
Bed rest and vocal rest.
Avoidance of tobacco and irritating agents.
Steam inhalation.
Systemic antibiotics if there is secondary bacterial infection.
Acute laryngotracheabronchitis( Croup)
Inflammatory condition of the larynx, trachea and bronchi.Causative organism is usually parainfluenza virus. Secondary bacterial infection is common and makes the condition worse.
Clinical Picture
It affects children 6 months to 3 years of age. There is frequently a preceding nasal or pharyngeal infection followed by:
Dry croupy or barking cough with hoarseness.
Inspiratory stridor and dyspnea.
Constitutional symptoms: fever.
On Examination:
Oedema and redness of the larynx.
Tenacious exudation and crusting over the larynx.
Investigation:
Anteroposterior X-ray of the neck shows subglottic narrowing (steeple sign).
Treatment
Reassurance and rest.Oxygen.
Adequate hydration.
Humidification of the inspired air.
Systemic antibiotics to overcome the secondary bacterial infection.
Steroids: using hydrocortisone or dexamethasone to reduce the inflammatory oedema.
Nebulized salbutamol or adrenaline administrated via a nebulizer is a bronchodialator
If signs of respiratory obstruction develop then intubation or tracheostomy is indicated.
Acute Epiglottitis
Serious condition.Affects young children 2-7 years of age, but it is less common and more dangerous than croup.
Aetiology: Haemophilus influenzae type B infection.
Clinical Picture
The onset is sudden and lethal airway obstruction can develop within hours.Sore throat and upper respiratory tract infection.
Inspiratory stridor develops rapidly and may end in sudden death.
Painful and difficult swallowing, so the child leans forward and drools saliva.
Muffled voice and cry.
High fever with toxaemia.
Triad of drooling, dysphagia, and distress.
The epiglottis is swollen,
red cherry color.No tongue depressor,
as this
may end in fatal total
obstruction.
Fiberoptic laryngoscopy.
It is better done in operation theater where facilities for intubation or tracheostomy are available.
Team of: Otolaryngologist, Pediatrician, and Anesthetist.
Investigation
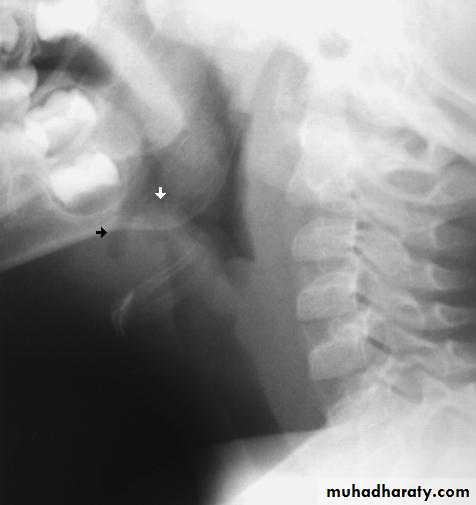
Lateral X-ray of the neck may show swollen epiglottis (thumb sign).Treatment
Once the diagnosis is suspected the child must be admitted to the hospital and intubation or tracheostomy should be kept in mind.Antibiotics: I.V. amoxycilin is the drug of choice, but the emergence of penicillin resistant strains, third generation cephalosporines (Ceftriaxone) by paranteral route are best used.
Intubation and tracheostomy is required in 60% of cases.
Chronic Laryngitis
A chronic inflammatory reaction of the larynx in which the laryngeal mucosa undergoes irreversible inflammatory changes. It may be diffused or localized.Etiology
Infection: repeated attacks of acute laryngitis or focal sepsis in the teeth, tonsils and sinuses.
Faulty use of the voice.
Excessive smoking and alcoholism.
Pollution by dust and irritant fumes.
Gastroesophageal reflux.
Clinical Picture
Hoarseness and tiredness of voice.
Irritation and raw sensation in the throat. A frequent desire to clear the throat is common.
Dry and irritating cough.
On Exam.
Indirect and fiberoptic laryngoscopy: Hyperaemia and oedema of the vocal cords. Excessive viscid secretions may be seen which results from increased activity of the mucous glands.
Laryngoscopy is indicated if hoarseness persists for more than
3 weeks to exclude malignancy.Treatment
Treat the predisposing factorsa. Elimination of focal sepsis in the teeth, tonsils and sinuses.
b. Voice rest and speech therapy.
c. Elimination of irritant factors as tobacco, fumes and alcoholism.
Medical treatment
Steam inhalation and application of laryngeal sprays.
Mucolytics (solvodin) when the secretions are thick and tenacious.
Antibiotics if there is secondary bacterial infection .
Surgical treatment
Microlaryngoscopy: For diagnostic purposes Endoscopic stripping of the vocal cords in resistant cases: when there is vocal cord edema.
Vocal Cords Nodules
They are bilateral, small, grayish, white,localized thickening of the vocal cords
situated at the junction of the anterior
third and posterior 2/3 of the vocal cord.
In this area maximum vibration occurs followed by fibrosis and traumatic scarring.
Aetiology:
Misuse of the voice or bad voice production with straining. It is commonly seen in singers, teachers and actors affecting women more than men.
Symptoms:
Hoarseness of voice.
Voice fatigue.
On Examination:
The site of nodule is at the junction of the anterior third and posterior 2/3 of the vocal cord.
Treatment
Small Voice rest and speech therapy.
Large Endoscopic excision followed by voice rest.
Laryngeal Polyp
Smooth unilateral glistering mass attached to the vocal cord due to accumulation of fluid in the sub-epithelial space.Aetiology: Vocal abuse, heavy smoking and allergy.
Clinical Picture:
Hoarseness of voice.
A large polyp may result in choking spills and stridor.
On Examination:
Indirect laryngoscopy and fibroptic endoscopy: sessile or pedunculated mass arising from the vocal cord near the anterior commissure, but it can be seen anywhere in the larynx.
Treatment
Endoscopic excision followed by voice rest and speech therapy. Histological examination is necessary to exclude malignancy.
Intubation Granuloma
AetiologyIt results from injury to vocal process of
arytenoids due to rough intubation, use of large tube or propounded intubation.
Pathology
Mucosal ulceration is followed by granuloma formation over the exposed cartilage.
Clinical picture
Patients are referred few days or weeks after an operation with hoarseness of voice. Stridor is rare.On Examination:
Endoscopy reveals a large fleshy granuloma arising from the vocal process of arytenoids.
Treatment
Voice rest and endoscopic removal preferably with LASER.
Tumors of the Larynx
Benign
EpithelialPapilloma
Connective tissue
Angioma• Fibroma
ChondromaMalignant
• Epithelial
Squamous cell carcinoma
Connective tissue
• Sarcoma• Lymphoma
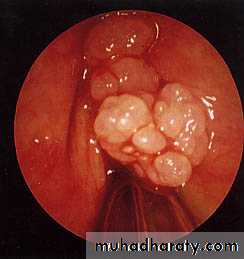
PapillomaThey can be divided into juvenile and adult onset types. They are known for recurrence after removal.
Juvenile: They are multiple often involving infants and young children. They are not premalignant and tend to disappear after puberty.
Adult onset: Usually its single and arises from the free edge of the vocal cord in adults. It may undergo malignant changes.
Juvenile Papilloma
Etiology: Virus HPV .
Clinical Picture:
Hoarseness of the voice.
Stridor from interference with the laryngeal intet.
On Exam.
The papilloma commonly seen at the anterior aspect of the vocal cords.
Treatment
Endoscopic excision using LASER because of the precision in removal and less bleeding. Histological examination is necessary to exclude malignant changes.Interferon therapy is being tried to prevent recurrence.
Tracheostomy in severe cases.
Tumors of the Larynx
BenignEpithelial
Papilloma
Connective tissue
Angioma
• Fibroma
ChondromaMalignant
• Epithelial
Squamous cell carcinoma
Connective tissue
• Sarcoma• Lymphoma
Carcinoma of the Larynx• The larynx is the most common site for carcinoma in the upper aero digestive tract occurring most often in men between 50-70 years of age.
• Histology:
• Microscopically 85-95% of laryngeal
• tumors are squamous cell
• carcinoma
Etiology
Heavy smoking and alcoholism.Cigarette smoke contains hydrocarbons which are carcinogenic.
Combination of alcohol and smoking increases the risk 15 folds compared to each factor alone (2-3 folds).
Radiation exposure.
Asbestos, mustard gas exposure.
GERD.
Human papilloma virus.
Classification
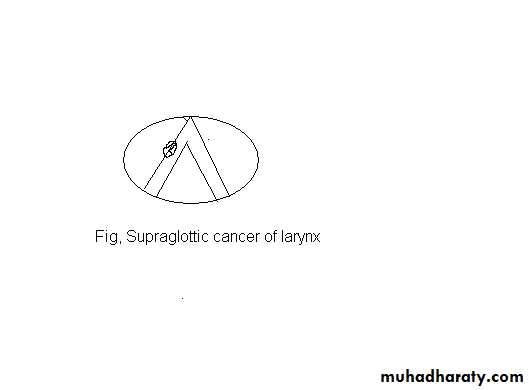
Supraglottis:It includes the epiglottis, aryepiglottic folds, arytenoids, false cords and the ventricles.
The supraglottis has a rich lymphatic drainage and a high proportion of these tumors spread to upper and middle jugular lymph nodes.
Hoarseness of voice is a late symptom, therefore these tumors often diagnosed late and carries a bad prognosis.
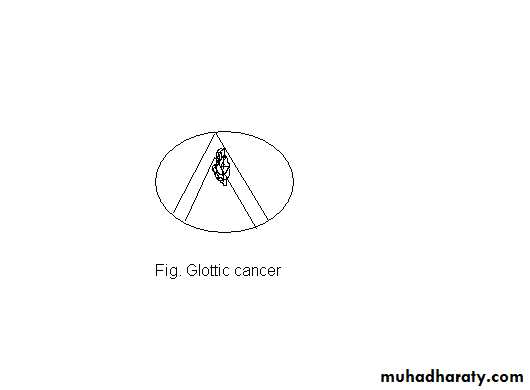
Glottis:
Vocal cords and the anterior and posterior commissures. The vocal cords have no lymphatic drainage and hoarseness of voice is an early symptom, therefore these tumors have an excellent prognosis.Subglottis:
Up to lower border of cricoid cartilage. It is the rarest region to be affected. Lymphatic mertastasis go to prelaryngeal, paratracheal and lower jugular lymph nodes.Hoarseness of voice is a late symptom and the patient may initially presents with stridor.
The prognosis is poorer than carcinoma of the glottis and supraglottis.
TNM classification and staging
Laryngeal carcinoma is classified according to the TNM staging system:T1: Tumuor is limited to one region.
T2: Tumuor affecting two adjacent regions.
T3: Fixation of the vocal cord.
T4: Tumour outside the larynx.
Staging- Nodes
• N0
• No cervical lymph nodes positive
• N1
• Single ipsilateral lymph node ≤ 3cm
• N2a
• Single ipsilateral node > 3cm and ≤6cm
• N2b
• Multiple ipsilateral lymph nodes, each ≤ 6cm
• N2c
• Bilateral or contralateral lymph nodes, each ≤6cm
• N3
• Single or multiple lymph nodes > 6cm
Staging- Metastasis
• M0• No distant metastases
• M1
• Distant metastases present
TNM classification and staging helps to determine:
The extent, the treatment modality and the prognosis.
Clinical Picture
Hoarseness of voice: Any patient with hoarseness of voice for more than 3 weeks without improvement, laryngoscopy is indicated.
Dyspnea and stridor.
Referred otalgia: Is a late symptom seen in mainly in supraglottic lesions.
Dysphagia: Late symptom, indicating invasion of the pharynx and commonly seen in supraglottic lesions.
Swelling of the neck: It may reflect direct penetration of the tumor outside the larynx or secondary lymphatic metastases.
Examination
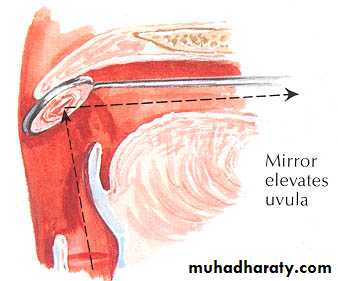
Indirect laryngoscopy for the shape, color and mobility of vocal cords.Fiberoptic endoscopy.
Examination of the neck for the shape of the larynx and lymph nodes.
Any patient with hoarseness of two weeks duration or longer must undergo visualization of the vocal cords.
Investigations
Radiography1 -Chest X-ray for pulmonary metastasis or mediastinal lymphnodes.
2 -CT scan and MRI assist in delineating the lesion.
Direct laryngoscopy and biopsy to prove the diagnosis
Spread of Laryngeal carcinomaDirect spread from one region to another and spread outside the larynx.
Lymphatic spread: common in supraglottic lesions and rare in glottic tumors.
Metastasis takes place to level (II-IV) lymph nodes or to paratracheal lymph nodes in subglottic tumors.
Distant metastases: mostly to the lung.
Treatment
Carcinoma in situ: Transoral CO2 LASER.- Early cancers T1 and T2 lesions are usually treated with either primary radiation or surgical excision. Both offer the 85-95% cure rate.
Radiotherapy has the advantage of preserving voice and it is indicated for small tumors with no cervical lymph nodes. Evidence of poor response to DXT or recurrence is an indication for suregry.
Surgery by LASER or partial laryngectomy.
Surgery has a shorter treatment period, saves radiation for recurrence, but may have worse voice outcomes.
Advanced laryngeal cancers (T3-T4) are often handled by multimodality therapy. Surgery with postoperative radiation.
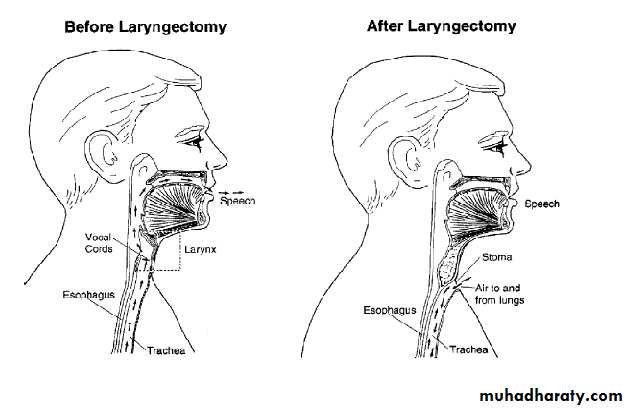
Surgery is usually: total laryngectomy±Neck dissection if nodes are palpable.
Organ preservation therapy by induction Chemotherapy followed by radiotherapy.
Voice rehabilitation after total laryngectomy
Oesophageal speech.Artificial larynx.
Tracheoesophageal valve.
Electrolarynx
Tracheo-oesophageal speech
Prognosis
• 5 year survival
• Stage I
• >95%
• Stage II
• 85-90%
• Stage III
• 70-80%
• Stage IV
• 50-60%
Tracheostomy
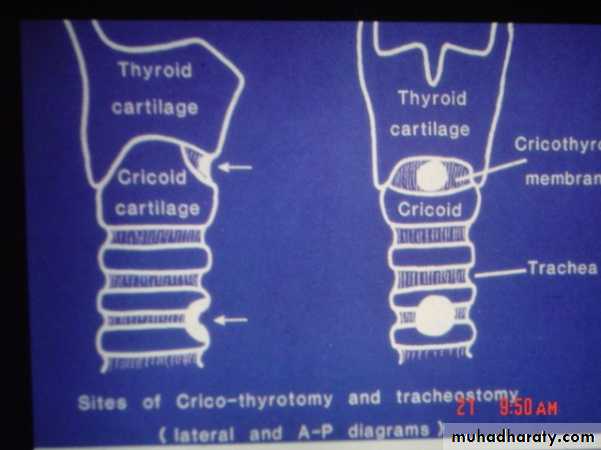
Surgical anatomy of the tracheaThe trachea is a fibromuscular tube supported by 20 hyaline cartilages which are opened posteriorly.
The soft tissue posterior wall is in contact with the oesophagus.
About 7-8 cartilaginous rings constitute the cervical portion.
Neck extension draws more rings to the cervical portion
The trachea begins at the 6th cervical vertebra.
The trachea is more superficial at its upper end, it became deeper as it passes downward and backward so that at the manuberum it is one inch from surface.In adults it is 12-16 cm long and 13-16 mm wide in women and 16-20 mm wide in men.
It is slightly to the right of the midline and divides at the carina into the right and left bronchi.
The carina lies under the junction of the sternum at the level of the 4th thoracic vertebra
MANAGEMENT OF THE OBSTRUCTED AIRWAY
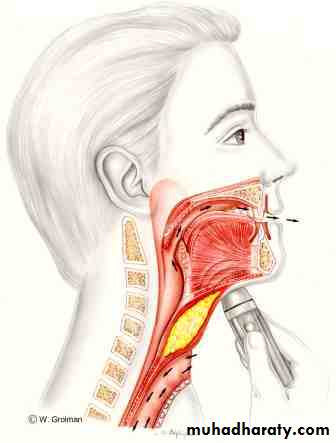
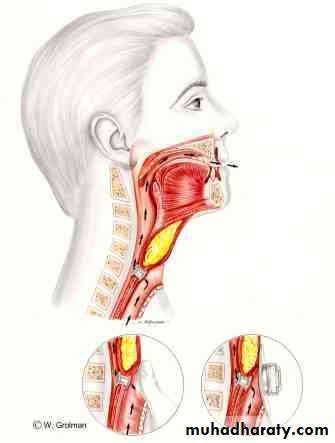
I. Laryngotomy (Cricothyroidotomy)
An opening through the cricothyroid membrane.
Indications
Sudden laryngeal obstruction when intubation is impossible and facilities for tracheostomy are not available.
Technique
It is performed without anaesthesia by transverse incision to open the cricothyroid membrane.
An elective tracheostomy is performed within a few hours if the obstruction is still present.
Complications
• Haemorrhage.
• Surgical emphysema.
Laryngeal stenosis
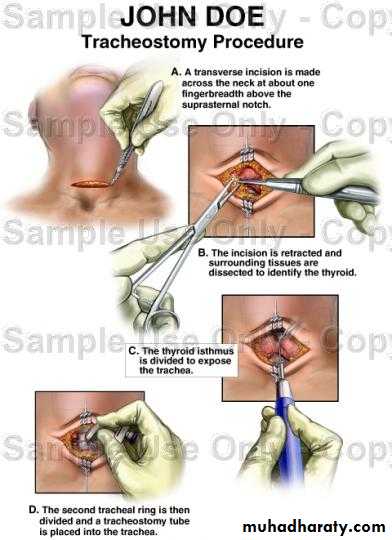
Tracheostomy
The creation of surgical opening into the trachea and converting it into a stoma on the skin surface.Types
1- Emergency tracheostomy: Its usually done under local anaesthesia in conditions such as acute respiratory failure, or large laryngeal tumor presenting with stridor.
2- Elective temporary tracheostomy: This is performed as planned procedure, usually under GA.
3- Permanent tracheostomy: The trachea is brought to the surface as a permanent mouth to the respiratory tract as following total laryngectomy.
Indications
I. Emergency
• Relief of upper airway obstruction.
• Congenital, Inflammatory lesions, Laryngeal tumors, Impacted F.B., Trauma, and Bilateral abductor paralysis.
Signs of upper airway obstruction
• Accessory Muscle use, Pallor, diaphoresis, restlessness, Tachycardia, Cyanosis and altered conscious state, Intercostal recession, Nasal Flaring, Exhaustion
• Bradycardia – most dangerous sign
2. Respiratory insufficiency: severe head and chest injuries, drug intoxication.
Tracheostomy aids respiration by:
a-Reduction of the dead space.
b-Reducing resistance to airflow.
c. The ability to use mechanical ventilator.
3. Respiratory difficulty due to secretions (bronchial toilet): coma, CVA and neurological lesions.
II. Elective: in cases of major head and neck surgery to maintain the airway and to protect it against hemorrhage.
Postoperative Management
• Nursing: constant attention is essential for the first 24 hours. The patient should have a paper to write and a bell to get assistance.• Care of the tube:
• Frequent tube suctioning and humidification of inspired air to prevent blockage.
• The safest way is to stitch it to the skin with a silk to prevent tube slippage.
• If cuffed tube is used, it should be periodically deflated to prevent pressure necrosis of the trachea.
• The first tube change can be done 3-4 days after surgery when the tract is fully formed.
Complications
• 1- Haemorrhage.• 2- Aprea: a result from sudden discharge of CO2 and the obstruction has been bypassed. It is managed by allowing the patient to breath a mixture of 95% O2 and 5% CO2.
3. Displacement of the tracheostomy tube caused by: Thick neck. Short tracheostomy tube. Postoperative oedema and haemorrhage causing broadening of the distance between the skin surface and the anterior tracheal wall.
4. Obstruction of the tracheostomy tube: this occurs if there is lack of humidification or poor toilet. It is treated by changing the tube.
5. Surgical emphysema: Too tight suturing of the wound. Small tracheostomy tube. Patient on positive pressure ventilation.
6. Pneumothorax: Due to injury to apical pleura. It is common in children and in low tracheostomy procedures.
7. Infection: wound, Chest
8. Subglottic stenois: especially if the cricoid cartilage is injured.
PARALYSIS OF THE LARYNX
I. Organic
• Central lesions: since the larynx is presented on both sides of the cortex, it requires bilateral symmetrical lesions to produce laryngeal paralysis. e.g. C.V.A., intracranial tumors and bulbar palsy.
• Peripheral lesions
• Congenital: Second most common cause of stridor in infants.
• Tumours: carcinoma of the lung, oesophagus, larynx, hypopharynx and mediastinal metastasis.
• Trauma: surgical trauma of thyroidectomy and chest surgery. The left R.L.N. being more affected by tumours and trauma than the right owing to its longer course.
• Neurological lesions: C.V.A, multiple sclerosis and head injury.
• Inflammatory lesions: Pulmonary or mediastinal T.B. and diphtheria toxins.
• Idiopathic: no cause could be found although infectious mononucleosis and influenza viruses have been suggested as aetiological agents.
II. Functional:
Occurs in emotionally unstable individuals, particularly in young women.
Investigations
• History.• Examination: mirror or rigid laryngoscopy, fiberoptic exam is important to visualize larynx in normal anatomic state.
• Examination also includes postnasal space, neck and chest.
• Imaging studies:
1. Chest X-ray.
2. CT scan of skull base, neck and thorax down to aortic arch.
3. MRI of brain.
• Sputum analysis for cytology.
• Fasting glucose, ESR and viral titres.
• Panendoscopy including oesophagoscopy and bronchoscopy.
Management
Main strategies:
• Treat the cause.
• Observation for 6-12 months after injury.
• Speech &/or swallow therapy
• Early surgical intervention
• Temporary – augmentation with filler.
• Permanent – medialization surgery.
• Abductor paralysis: unilateral or bilateral.
• Adductor paralysis: unilateral or bilateral.Unilateral Abductor Paralysis
Position: The paralyzed cord lies near the midline (paramedian position).Aetiology: The most common cause is damage to the R.L.N. by:
• Left bronchogenic carcinoma, aortic aneurysm and cardiac surgery.
• Surgical trauma of thyroidectomy.
Clinically: the voice and respiration remain near normal and the condition may be unsuspected.
Treatment
• Treat the cause: if it is occurred after thyroidectomy, then the neck should be urgently explored and any ligature involving the R.L.N. should be removed.
• Speech therapy: the voice problem is minimal and the other cord usually compensates by speech therapy.
Unilateral Adductor Paralysis
Position: the paralyzed cord lies in lateral position.
Aetiology: It is the result of damage to the vagus or both the superior and R.L.N.
1. Thyroid surgery is the most common cause.
2. Rarely, lesions of medulla, posterior cranial fossa and jugular foramen can cause it.
Clinically: the patient will be aphonic at the onset, but later the opposite cord will cross the midline and the voice will begin to return. Respiration is normal but aspiration of food and saliva can occur.
Treatment: 1. Treat the cause.
2. Speech therapy.
3. If there is no compensation after 6-12 months teflon paste injection in the paralyzed cord.
Bilateral Abductor Paralysis
Position: Both cords lie near the midline (paramedian).Aetiology: It is most often caused by
• Damage to both R.L.N. at thyroidectomy, for this all thyroid surgery should be preceded by laryngoscopy.
• It is also seen as a complication of postcricoid cancer and carcinoma of the cervical oesophagus.
Clinically: the quality of voice is good but sooner or later every patient will have stridor.
Treatment
Sudden onset → Intubation or tracheostomy and urgent exploration of the neck is indicated in thyroidectomy.
less urgent cases: Observation.
The final decision for treatment is taken after 6-12 months because compensation is possible at this period. If no improvement:
• Permanent tracheostomy with a speaking valve.
Arytenoidectomy and/or cordectomy
Bilateral Adductor Paralysis
Position: Both cords lie in lateral position.
Aetiology: It is commonly functional and most frequently encountered in hysterical females.
Clinically: the voice is weak and the patient uses a whisper. The most important single diagnostic feature is when the patient is asked to cough, there is good adduction of the cords.
Treatment: Psychotherapy and speech therapy.