Antiepileptic drugs((Anticonvulsant
The term epilepsy refers to a group of disorders characterized by excessive excitability of neurons within the CNS.This abnormal activity can produce a variety of symptoms, ranging from brief periods of unconsciousness to violent convulsions.
Epilepsy
Seizures are initiated by synchronous, high-frequency discharge from a group of hyperexcitable neurons, called a focus.Seizures result when discharge from a focus spreads to other brain areas, thereby recruiting normal neurons to discharge abnormally along with focus.
1. Phenytoin
2. Carbamazepine3. Phenobarbital
4.Valproic acid
5. Benzodiazepines: diazepam, lorazepam clonazepam.
6. Ethosuximide.
Antiepileptic Drugs:
At the concentrations achieved clinically, phenytoin causes selective inhibition of sodium channels.
As a result, entry of sodium into neurons is inhibited, and hence action potentials are suppressed.
Phenytoin:
Epilepsy. Phenytoin can be used to treat all major forms of epilepsy except absence seizures.
Cardiac Dysrrhythmias. Phenytoin is active against certain types of dysrrhythmias. Phenytoin is a second choice drug after lidocaine for treating digoxin-induced dysrrhythmias.
Therapeutic uses:
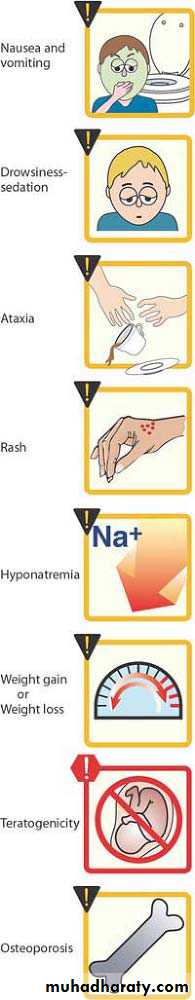
Effects on the CNS. Sedation, Nystagmus, ataxia, diplopia and cognitive impairmentGingival hyperplasia.
Skin rash.
Other adverse effects
a. Hirsutism
b. Interference with vitamin D metabolism may cause rickets and osteomalacia.
c. Interference with vitamin K metabolism can lower prothrombin levels, thereby causing bleeding tendencies in newborns.
Adverse Effects:
Phenytoin should be used during pregnancy only if the benefits of seizure control outweigh the risk to the fetus.Pregnancy:
Levels below 10 µg/ml are too low to control seizure; at levels above 20 µg/ml, signs of toxicity begin to appear. (Narrow therapeutic range).
When treatment with phenytoin is discontinued, dosage should be reduced gradually. Abrupt withdrawal may precipitate seizures
Plasma level
Carbamazepine (Tegretol) is a mainstay of epilepsy therapy.The drug is active against partial seizures and tonic clonic and other types of seizures but not absence seizures.
Carbamazepine
The mechanism of action of carbamazepine appears to be the same as that of phenytoin.Mechanism of action:
• 1. Epilepsy.2. Bipolar disorder (manic-depressive illness).
3. Trigeminal neuralgia. Neuralgia is a severe, stabbing pain that occurs along the course of a nerve. Carbamazepine can reduce neuralgia associated with the trigeminal nerves.
Therapeutic uses:
• 1. CNS effects. Nystagmus, blurred vision, diplopia, ataxia, vertigo and headace.
2. Hematologic effects. bone marrow suppression leading to leukopenia, anemia and thrombocytopenia. Fatal aplastic anemia3. Hyponatremia.
4. Dermatologic effects.
Adverse effects:
Carbamazepine may be teratogenic.In humans, the drug is associated with an increased risk of neural tube defect.
Pregnancy:Valproic acid appears to act by 3 mechanisms:
1. The drug shares the same mechanism asphenytoin and carbamazepine.
2. The drug suppresses calcium influx through calcium channels.
3. Augment the inhibitory influence of GABA by inhibiting its metabolism
Valproic acid (Depakene)
• 1.Broad spectrum antiepileptic agent
2. Bipolar disorder3. Migrain
Clinical uses:1.GIT effects.
2. Hepatotoxicity.
3. Other adverse effects.
a. skin rashes.
b. Weight gain.
C. Hair loss
d. Blood dyscrasias: leukopenia, thrombocytopenia, anemia
Adverse effects:
Gabapentin is an analog of GABA. However, it does not act at GABA receptors nor enhance GABA actions, nor is it converted to GABA.
Its precise mechanism of action is not known. .
Gabapentin:It is approved as adjunct therapy for partial seizures and for treatment of postherpetic neuralgia.
Good choice due to limited or no reported pharmacokinetic drug interactions
Continuous series of tonic clonic seizures that lasts for at least 20 to 30 minutes.An IV benzodiazepine, either lorazepam or diazepam, is used initially.
Once seizures have been stopped, phenytoin or phenobarbitone is given for long-term suppression.