Megaloblastic Anemias
DEFINITION:Megaloblastic anemias are caused by defects in DNA synthesis that lead to abnormalities of bone marrow and peripheral blood cells.
The term megaloblastic refers to a morphologic abnormality (mainly affecting the size and morphology) of the cell and it's nucleus
Causes of Megaloblastic Anemia
I. Cobalamin(vit B12) deficiencyA. Decreased ingestion: vegetarians.
B. Impaired absorption: small intestinal disease.
C.Impaired utilization.
II. Folate deficiency
A. Decreased ingestion:prolonged parenteral feeding,alcoholism.
B. Impaired absorption:small intestinal disease.
C. Impaired utilization:drug induced eg; sulfa drugs,methotrexate,phenytoin…
D. Increased requirement:pregnancy,hemolysis.
E. Increased loss:through urine.
III. Drugs — metabolic inhibitors
IV. Miscellaneous
A. Inborn errors
B. Unexplained disorders
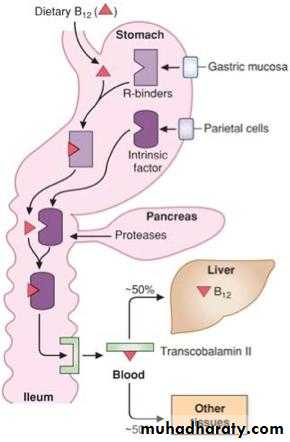
Cobalamine Metabolism
Cobalamine is an animal product.
Daily need=1microgram.
Dietary cobalamin enters the duodenum bound to R protein.
Pancreatic proteases degrade R protein–cobalamin complexes in the jejunum; cobalamin is bound to intrinsic factor only after this process occurs.
The intrinsic factor–cobalamin complex binds with receptors on ileal mucosal cells. Cobalamin then enters these cells and reaches the portal plasma, which contains three cobalamin binding proteins known as transcobalamin I, II, and III.
Vitamin B12 Absorption
Folate Metabolism
Folate is widely distributed in plants and and animal products.Daily need=50microgram.Enzymes in the small intestine convert the polyglutamate forms of folate to the monoglutamate and diglutamate forms, which are absorbed in the proximal jejunum.
Folate in plasma is present as 5-methyltetrahydrofolate in the monoglutamate form. it is taken up by receptors present on cells throughout the body.
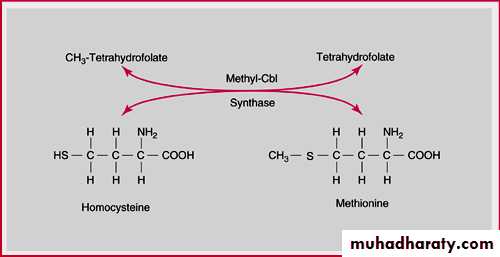
The 5-methyltetrahydrofolate is converted to tetrahydrofolate by the cobalamin-dependent enzyme methionine synthase before it can be converted to the polyglutamate form and take part in the other folate-dependent enzymatic reactions
Folate and Cobalamine metabolism
Clinical Manifestations of Megaloblastic Anemia
• Symptoms of slowly progressive anaemia• Jaundice(Cobalamine deficiency).
• Glossitis
• Stomatitis
• Gastrointestinal symptoms
• Orthostatic hypotension
• Weight loss
• Neuropsychiatric :in Cobalamine deficiency
• Paresthesia , Abnormal gait , Memory loss. Disorientation, Decreased or Increased reflexes,Romberg's sign.
• Spasticity, Babinski's sign, Psychosis, Slow Mentation.
Laboratory Investigations
1- Complete Blood Count &Blood Film:Macrocytosis (increased MCV),Neutropenia,Thrombocytopenia,
Neutrophil hypersegmentation, Reticulocytopaenia
2- Bone Marrow Aspirate &Biopsy:
Hypercellular, Megaloblastic morphology ,Giant bands &metamyelocytes.
3- Indirect Hyperbilirubinemia, elevated s.LDH.
4- Serum cobalamin: in cobalamine deficiency(normal, 200–900 pg/mL).
5- Serum folate: in folate deficiency(normal, 2.5–20 ng/mL).
6- Schilling Test for diagnosing the cause of Cobalamine malabsorption.
7- Gastric biopsy for pernicious anemia(cobalamine deficiency) and/or Small Intestinal Biopsy for malabsorption .
8- Anti-Intrinsic factor Ab& Anti-Parietal cell Ab in Pernicious
anemia(Cobalamine deficiency).
9- Elevated serum Methylmalonic acid in Cobalamine deficiency.
Macrocytes and Hypersegmented Neutrophil
Megaloblastic Bone Marrow
PERNICIOUS ANEMIAThe most common cause of cobalamin malabsorption is pernicious anemia.
There is atrophy of the gastric parietal cells leading to the absence of IF and HCl secretion.There is association of pernicious anemia with other autoimmune diseases. There is a positive family history for about 30% of patients
The histologic appearance of the gastric mucosa (infiltration with plasma cells and lymphocytes) is suggestive of autoimmune-type lesions.
There is also a high incidence of anti-parietal cell IgG antibodies in the serum of 90% of patients with pernicious anemia.
Treatment of Megaloblastic Anemia
Cobalamine Deficiency:Hydroxycobalamine 1 mg i.m. daily for 10 days ,then once every one month for life.Iron is added for slow response. Hypokalemia may develop during therapy. Reticulocytosis at day 7 will indicate response.
Blood is given for severly symptomatic patients.
Folate Deficiency:
Oral Folic acid 5 mg/day for 3 weeks then weekly as maintenance.
Summary
Iron deficiency anemia is the most common cause of anemia.
Chronic blood loss is the most common cause of iron deficiency in adults and physiological increased demand in pregnants and children.
A hpochromic microcytic anemia with low serum ferritin, low serum iron and increased TIBC are diagnostic of iron deficiency anemia.
Oral iron therapy is the standard of care. Injectable iron is needed in special circumstances.
Megaloblastic anemia is caused by vit B12 or folate deficiency.
Neuropsychiatric manifestations are seen in vit B12 deficiency.
A macrocytic anemia with megaloblastic changes in bone marrow are the criteria to diagnose megaloblastic anemia.
Vitamin B12 replacement in pernicious anemia is continued indefinitely.
Oral folate is the standard of care for folate deficiency.
Anemia of Chronic Disease
EtiologyInfections, cancer, endocrine disorders (e.g. thyroid).
Inflammatory and rheumatologic disease.
Renal disease.
Pathophysiology
A mild hemolytic component is often present, red blood cell survival is moderately decreased.
Erythropoietin levels are normal or slightly elevated but are inappropriately low for the degree of anemia, erythropoietin level is low in renal failure
Iron cannot be removed from its storage pool in hepatocytes and RES cells.
Anemia of Chronic Disease
Diagnosis
RBC are usually normocytic normochromic if the anemia is mild, but may be microcytic normochromic, or even microcytic hypochromic,Hb rarely < 9 g/dL except in renal failure.
Serum iron, TIBC, and % saturation all normal or slightly reduced, serum ferritin is normal or increased.
Normal or increased iron stores in bone marrow, decreased “normal” sideroblasts.
Management
Resolves if underlying disease is treated.
Erythropoietin may normalize the hemoglobin value especially in chronic renal failure. Dose of erythropoietin required is lower for patients with renal disease
Case Presentation
A 50 year old female presented with one month history of progressive pallor, multiple ecchymoses ,epistaxis and attacks of fever and sore throat.Her clinical examination revealed severe pallor, multiple bleeding spots on her legs .
Blood counts revealed pancytopenia
What is your differential diagnosis?
1-Aplastic Anemia.
2-Acute leukemia.
3-Myelodysplasia.
Aplastic Anemia
EtiologyRadiation
Drugs
• anticipated (chemotherapy)
• idiosyncratic (chloramphenicol, phenylbutazone)
Chemicals
• benzene and other organic solvents
• DDT and insecticides
Post viral e.g. hepatitis B, parvovirus,HIV.
Idiopathic
• often immune (cell mediated)
Paroxysmal nocturnal hemoglobinuria
Marrow replacement
Congenital: Fanconi anemia, associated with dysmorphic features.
Abnormal Thumbs in Fanconi Anemia
Clinical Presentation of Aplastic Anemia
• Occurs at any age• Slightly more common in males.
• Can present acutely or insidiously.
• Features of anemia or neutropenia or thrombocytopenia (any combination).
• Thrombocytopenia as bruising, bleeding gums, epistaxis.
• Anemia as SOB, pallor and fatigue.
• Presentation of neutropenia ranges from infection in the mouth to septicemia.
Aplastic Anemia
Diagnosis1- CBC: Pancytopenia
• normochromic normocytic anemia.
• neutrophil count < 1.5 x 109/L.
• platelet count < 20 x 109/L.
• corrected reticulocyte count < 1%.
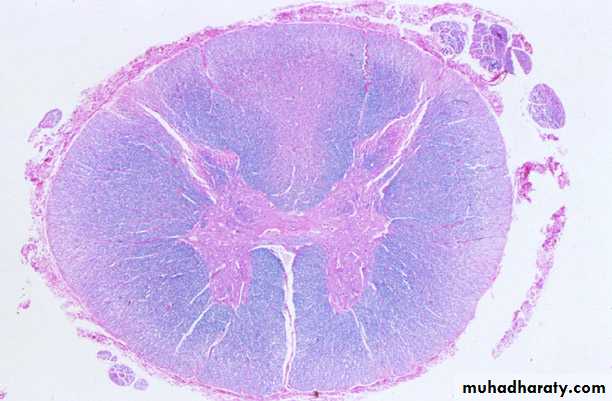
2- Bone marrow aspirate and biopsy
• aplasia or hypoplasia of marrow cells with fat replacement.
Aplastic Bone Marrow Biopsy
Aplastic Anemia
ManagementRemoval of offending agents.
Supportive care (red cell and platelet transfusions, antibiotics).
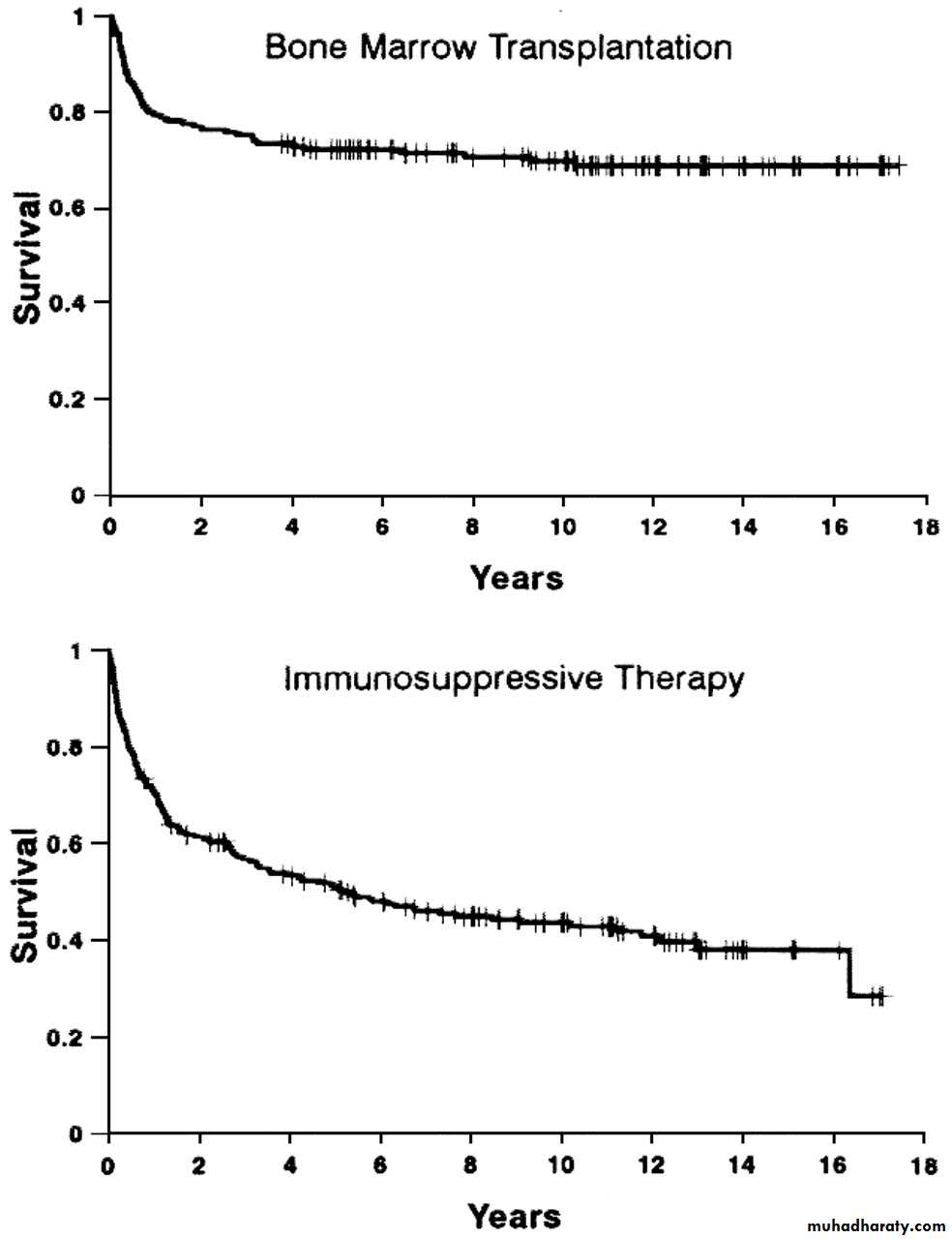
Antithymocyte globulin (50-60% of patients respond) for patients who are >45 years of age and those who have no donor for bone marrow transplant
Cyclosporin A,mainly useful for mild cases.
Allogeneic bone marrow transplantation for patients<45 y
• minimize blood products on presentation.
• only irradiated, leuko-depleted blood products should be used to minimize CMV transmission.
• CMV negative blood for CMV negative patients.
MYELODYSPLASTIC SYNDROMES (MDS)
PathophysiologyA group of clonal bone marrow stem cell disorders characterized by one or more cytopenias.
Ineffective hematopoiesis despite presence of adequate numbers of progenitor cells (bone marrow is usually hyper-cellular).
Dysplastic changes affect all the hematopoietic cell lines due to abnormal maturation and differentiation which include abnormal size , nuclear shape and cytoplasmic granules
The blood elements are dysfunctional.
There is increased liability for transformation to AML.
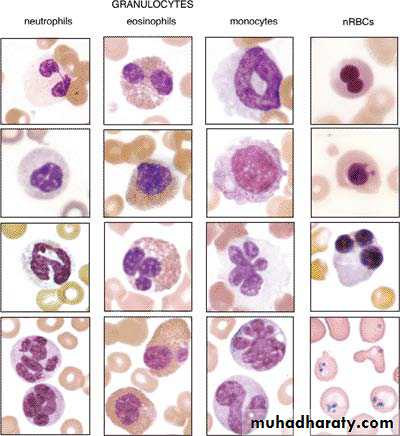
Dysplastic nuclear features in circulating cells. Composite image taken from several cases of myelodysplastic syndrome showing dysplastic nuclear features seen in circulating granulocytes and nucleated RBCs. The right lower figure shows numerous Pappenheimer bodies.
MDS
Types
Refractory anemia (RA).
Refractory anemia with ring sideroblasts (RARS).
Refractory anemia with excess blasts (RAEB).
Refractory anemia with excess blasts in transformation (RAEB-T).
Chronic myelomonocytic leukemia (CMML).
MDS
• Clinical Presentation
• Related to bone marrow failure, most common in elderly, usually > 70 and post-chemotherapy or radiation
• Usually insidious in onset: fatigue, weakness, pallor, infections, bruising and rarely weight loss, and hepatosplenomegaly
• Diagnosis
• 1- Anemia ± thrombocytopenia ± neutropenia
• RBC: variable morphology with decreased reticulocyte count.
• WBC: decrease in granulocytes and abnormal function.
• Platelet: either too large or too small and thrombocytopenia.
• 2- Bone marrow : dysmyelopoiesis in bone marrow precursors
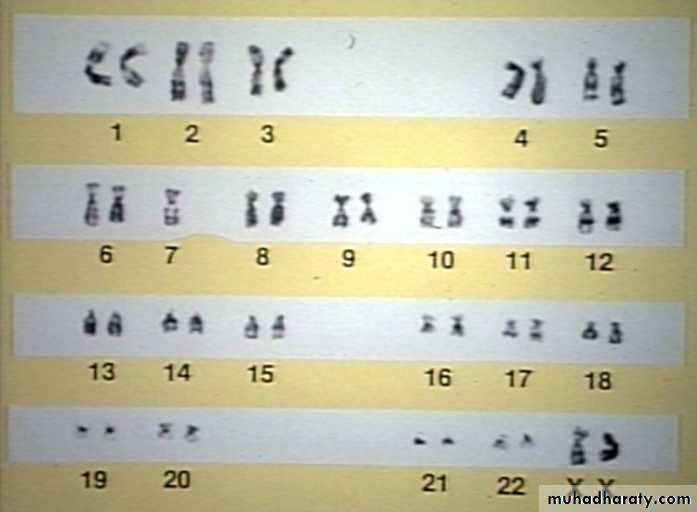
• 3- Chromosomal Abnormalities:5,7,8 ,others
MDS
• Management
• 1- Symptomatic (transfusion, antibiotics)
• 2- Growth factors: Erythropoietin,G-CSF.
• 3- Cytotoxics for RAEB & RAEB-T&CMML
• 4- Bone marrow transplant for young patients with advanced disease.
• 5- Immune modulating and differentiating agents .
Summary
Anemia of chronic disease may be confused with iron deficiency anemia, but the serum ferritin is normal.Anemia of chronic disease is usually mild except in chronic renal failure were it responds well to erythropoietin injections.
Aplastic anemia presents with anemia ,repeated infections and bleeding tendency due to pancytopenia and hypocelluar marrow.
Idiopathic aplastic anemia is best treated with allogeneic bone marrow transplantation for patients younger than 45 years old.
Idiopathic aplastic anemia of older patients is treated with antithymocye globulin and ciclosporin A.
Supportive treatment is essential for aplastic anemia.
Myelodysplastic syndrome is a group of disorders affecting bone marrow stem cells that result in dysplastic changes, di or pancytopenia and tendency to transform into AML.
Patients need supportive treatment. Chemotherapy and bone marrow transplantation are reserved for fit patients with transformation into AML.