Endocrine System Physiology
Dr. Yasir Al MallayahM.B.Ch.B, M.Sc., PhD
1
Introduction and Overview
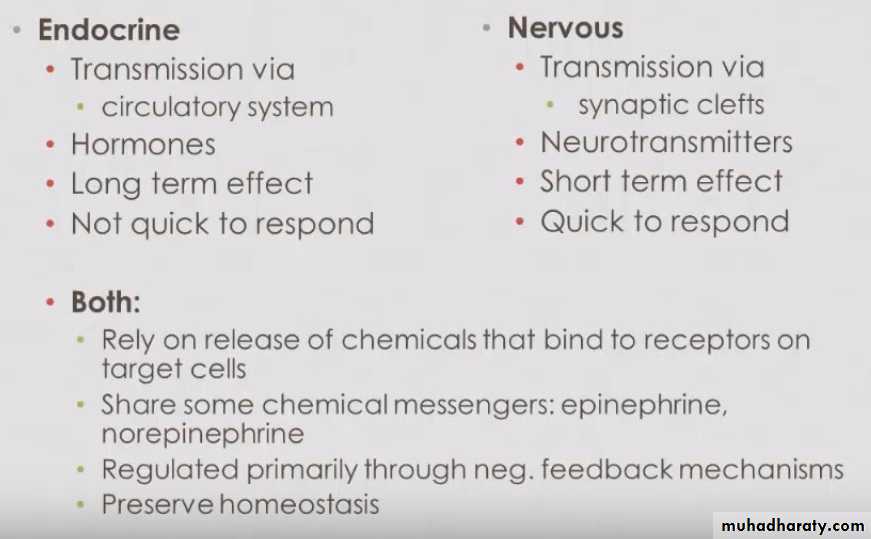
- It is one of the control systems, like the nervous system.2
General functions of the endocrine system
The endocrine system, in concert with the nervous system, is responsible for homeostasis.Growth, development, reproduction, blood pressure, concentrations of ions and other substances in blood, and even behavior are all regulated by the endocrine system.
Endocrine physiology involves the secretion of hormones and their subsequent actions on target tissues.
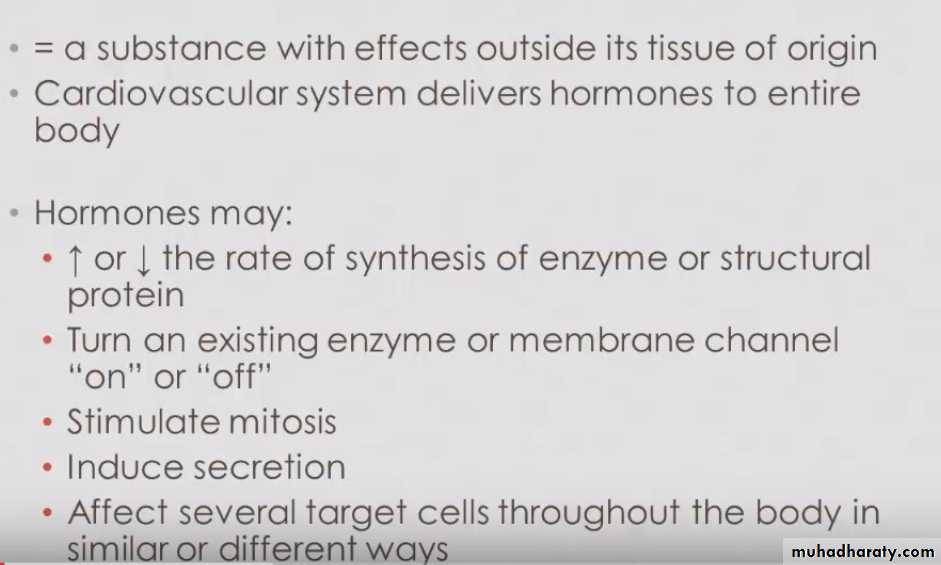
A hormone is a chemical substance that is classified as a peptide, steroid, or amine and they are secreted into the circulation in small amounts and delivered to target tissues, where they produce physiologic responses
3
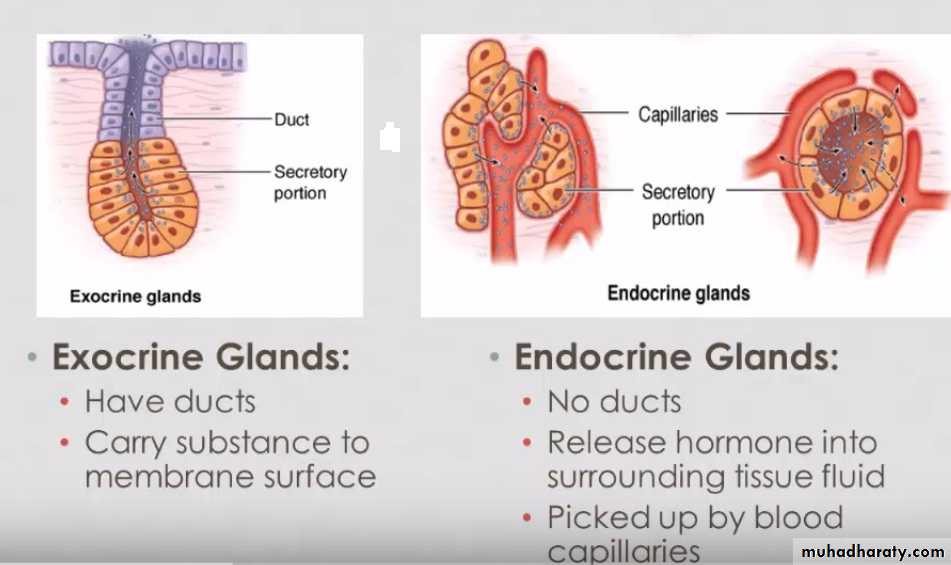
Endocrine Vs Exocrine glands
4
Endocrine glands
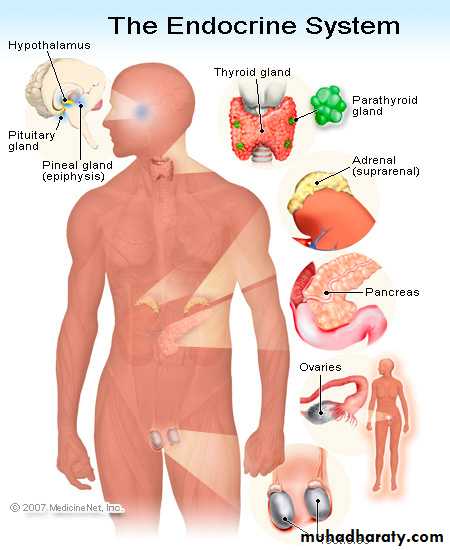
Endocrine glands may be strictly endocrine, such as the pituitary, thyroid, parathyroid, adrenal, pineal and thymus; or they may be organs that have hormone production as one of many functions, such as the pancreas, gonads, hypothalamus, kidneys, heart,…etc.5
Hormones
6
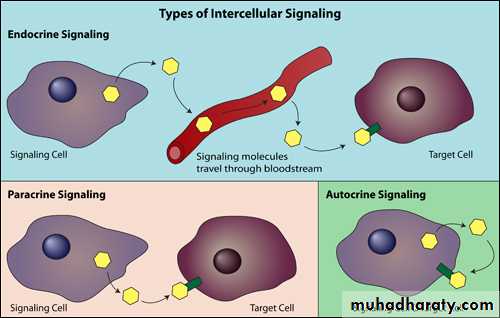
Endocrine Vs Autocrine & Paracrine
7
Classes of Hormones
I- Amino acid based:
1- Single amino acids
- small molecules
- synthesized from tyrosine or tryptophan
- include: thyroxin, epinephrine, norepinephrine, dopamine, melatonin.
II- Peptide hormones
- chains of amino acids
- include: TSH, LH, FSH, ADH, oxytocin, and GH
II- Lipid based:
1- Steroids : synthesized from cholesterol,
- Androgen, estrogen, progestins, corticosteroids, calcitriol
2- Eicosanoids ( paracrines or autocrines )
Prostaglandins (PGs), leukotrienes
Secreted by nearly all cell membranes, and involved in many functions including inflammation
8
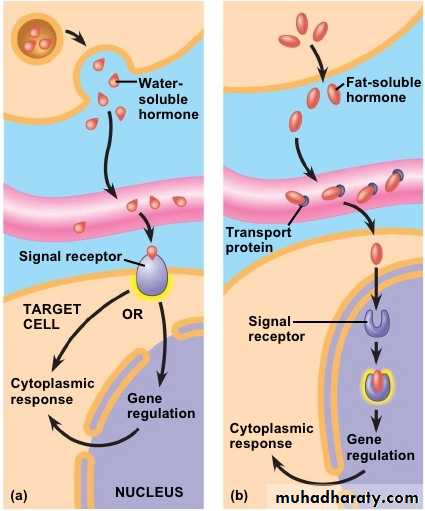
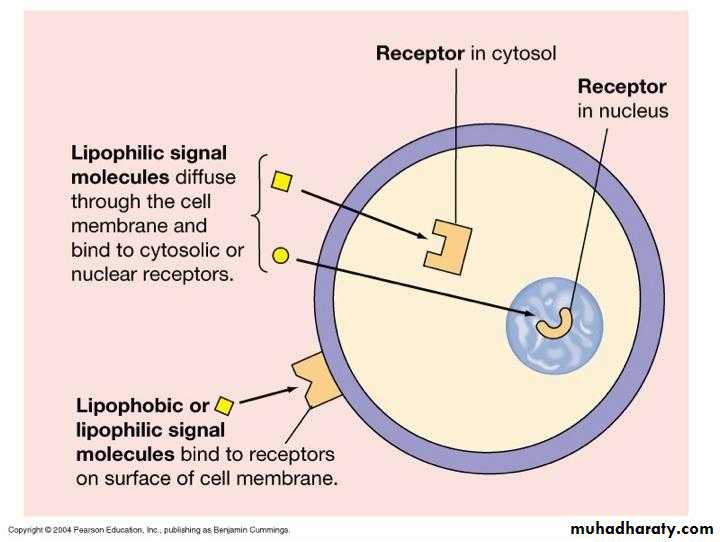
Hormone transport
A- Water soluble hormones
(Lipophobic)Amino acids and peptide hormones
Except thyroid hormones
B- Lipid soluble
(Lipophilic)
Steroid and thyroid hormones
9
Hormone activation of target cell
10
Hormone activation of target cell
11Mechanisms of Hormone Action
Hormones typically produce changes in membrane permeability or potential, stimulate synthesis of proteins or regulatory molecules, activate or deactivate enzymes, induce secretory activity, or stimulate mitosis.12
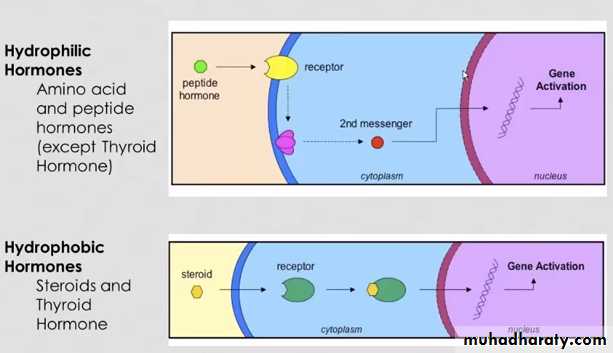
How water-soluble hormones exert their effects?
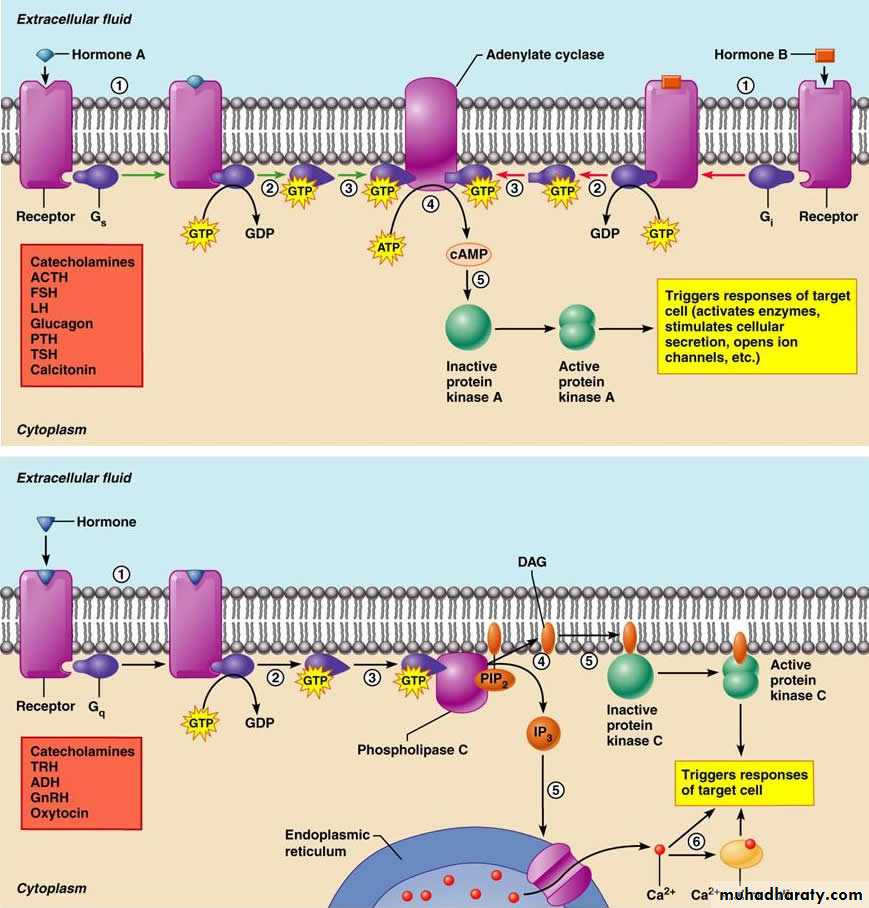
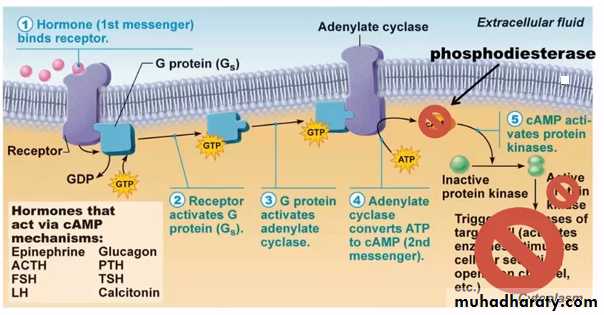
Water-soluble hormones (all amino acid-based hormones except thyroid hormone) exert their effects through an intracellular second messenger that is activated when a hormone binds to a membrane receptor.Second messenger systems, activated when a hormone binds to a plasma membrane receptor, activate G-proteins within the cell that alter enzyme activity.
13
How water-soluble hormones exert their effects?
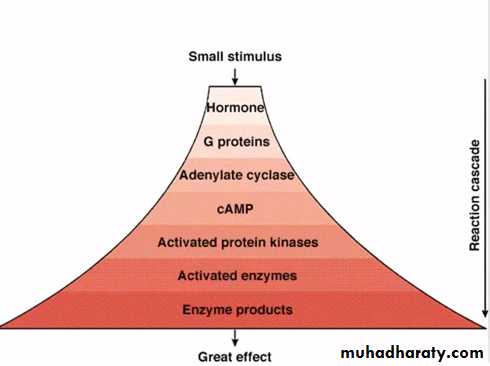
Hormone actions on target cells begin when the hormone binds to a membrane receptor, forming a hormone-receptor complex. In many hormonal systems, the hormone-receptor complex is coupled to effector proteins by guanosine triphosphate (GTP)-binding proteins (G proteins). The effector proteins usually are enzymes, either adenylyl cyclase or phospholipase C. When the effector proteins are activated, a second messenger, either cAMP or IP3 (inositol 1,4,5-triphosphate), is produced, which amplifies the original hormonal signal and orchestrates the physiologic actions.14
How water-soluble hormones exert their effects?
15Inactivation
Phosphdiesterase
Already present inside the cell16
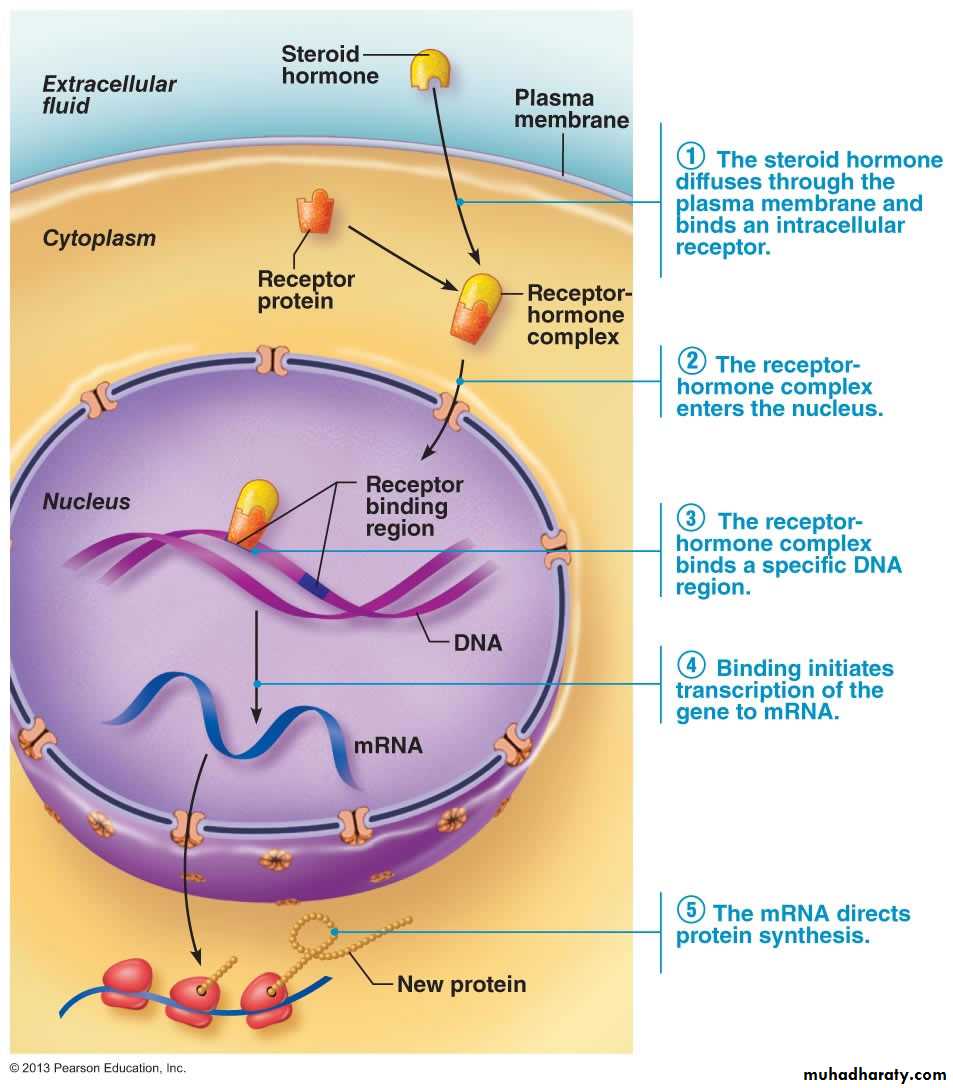
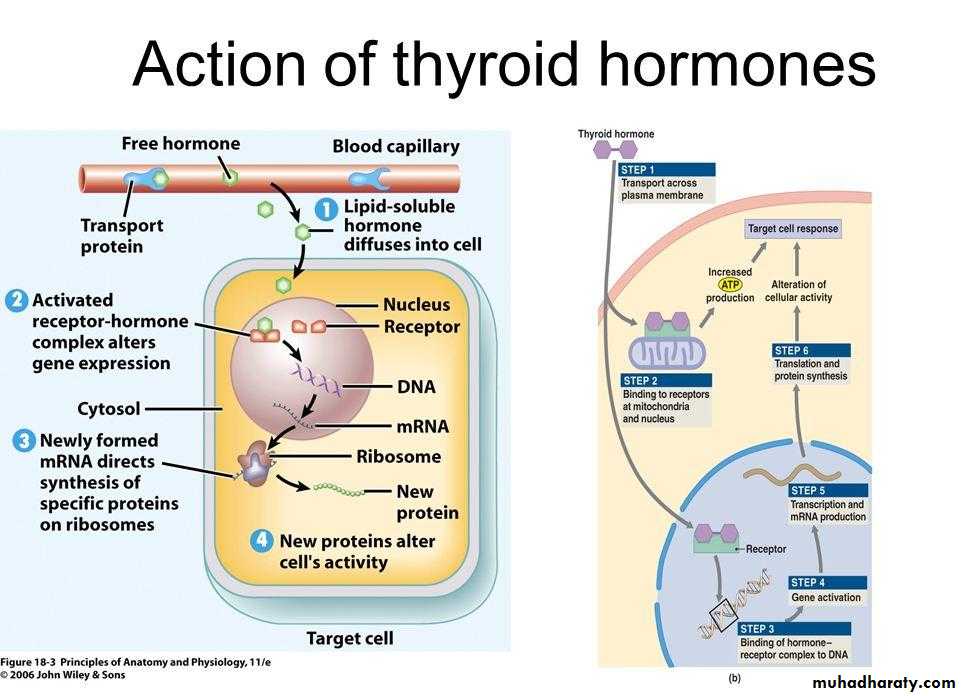
How lipid-soluble hormones exert their effects? Direct gene activation
Lipid-soluble hormones (steroids and thyroid hormone) diffuse into the cell, where they bind to intracellular receptors, migrate to the nucleus, and activate specific target sequences of DNA.Direct gene activation occurs when a hormone binds to an intracellular receptor, which activates a specific region of DNA, causing the production of mRNA, and initiation of protein synthesis.
17
Direct gene activation
18
Signal Amplification
19
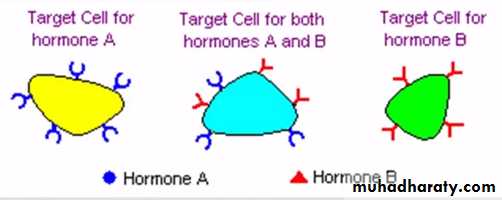
Target Cell Specificity
Cells must have specific membrane or intracellular receptors to which hormones can bind.20
Target Cell Response and Regulation of Hormone Receptors
Target cell response depends on three factors:1- Blood levels of the hormone,
2- Relative numbers of target cell receptors,
3- Affinity of the receptor for the hormone.
- Target cells can change their sensitivity to a hormone by changing the number of receptors or changing the affinity to hormones.
- Number of receptors may change in response to hormone level
1- Up-regulation: target cell receptors increase in number and/or increase affinity to hormone due to low blood level of that hormone.
2- Down-regulation: target cell receptors decrease in number and/or decrease affinity to hormone due to high blood level of that hormone.
21
Half-Life, Onset, and Duration of Hormone Activity
The concentration of a hormone reflects its rate of release, and the rate of inactivation and removal from the body.The half-life of a hormone is the duration of time a hormone remains in the blood, and is shortest for water-soluble hormones.
Target organ response and duration of response vary widely among hormones.
22
Interaction of Hormones at Target Cells
Permissiveness occurs when one hormone exerts its full effect when another hormone is present (reproductive hormones need thyroxin to properly stimulate development of reproductive organs), (thyroid hormone increase the number of epinephrine receptors on target cells).Synergism occurs when more than one hormone produces the same effects in a target cell, and their combined effects are amplified (glucagon + epinephrine together stimulate more glucose release from the liver than when each acts alone), that is combined effect is more than the sum of individual effects, (another example LH and estrogen on egg production)
Antagonism occurs when one hormone opposes the action of another hormone (glucagon antagonizes insulin).
Agonism (agonistic effect) when two hormones have similar effects, (epinephrine and norepinephrine)
Tropic (Trophic) effect: hormone stimulates development of another gland and secretion of its hormones (ex: TSH stimulates thyroid gland to make and release thyroid hormone)
23
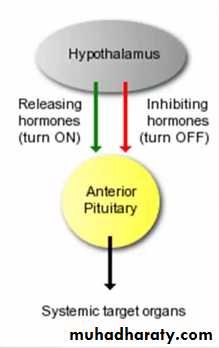
Control of Hormone Release
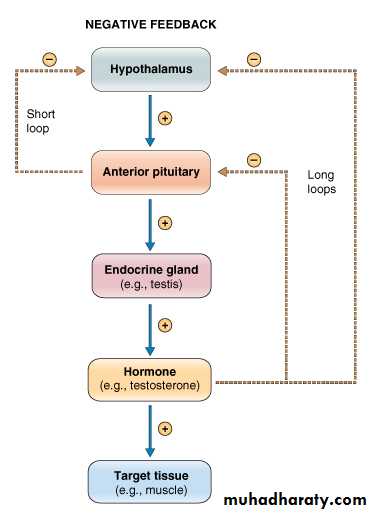
Most hormone synthesis and release is regulated through negative feedback mechanisms, which means some feature of hormone action, directly or indirectly, inhibits further secretion of the hormone24
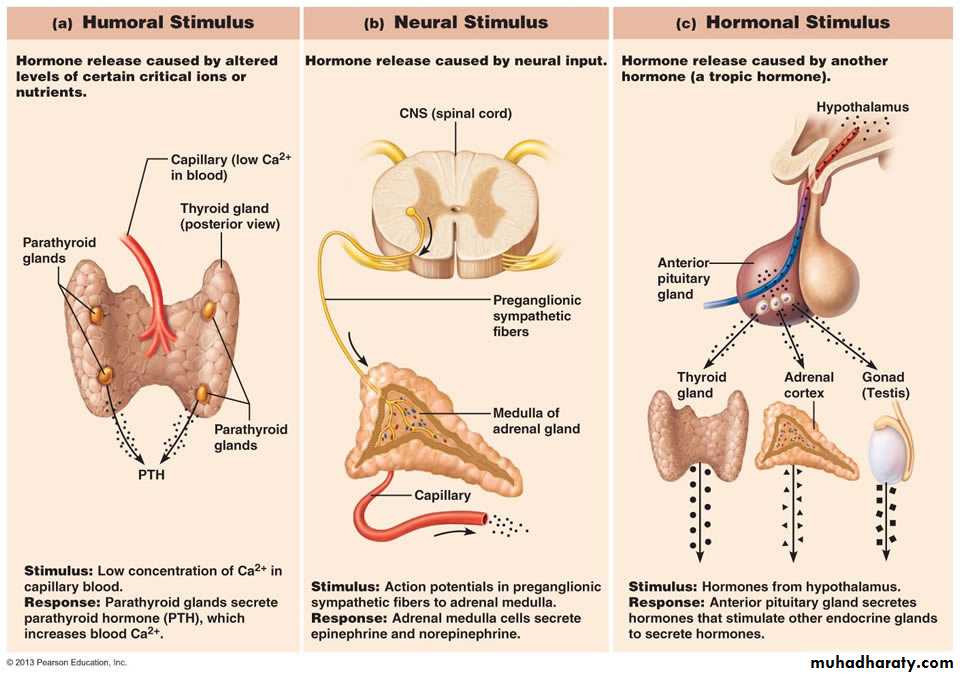
How endocrine glands are stimulated?Types of Endocrine Glands Stimuli
25
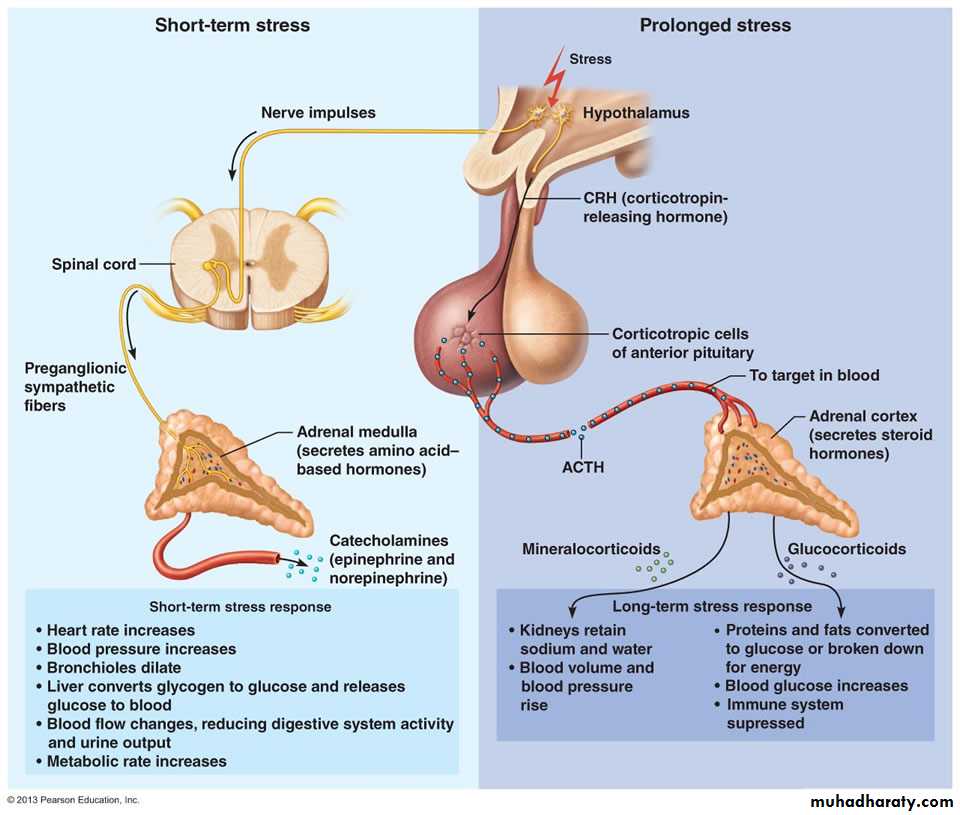
Neural Modulation of Hormone Levels
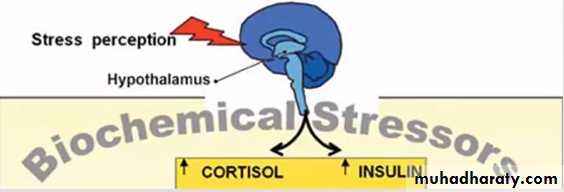
Nervous system modulation allows hormone secretion to be modified by the nervous stimulation in response to changing body needs.Example: during stress neural effects exceeds the negative feedback regulation of stress hormones secretion
26
27
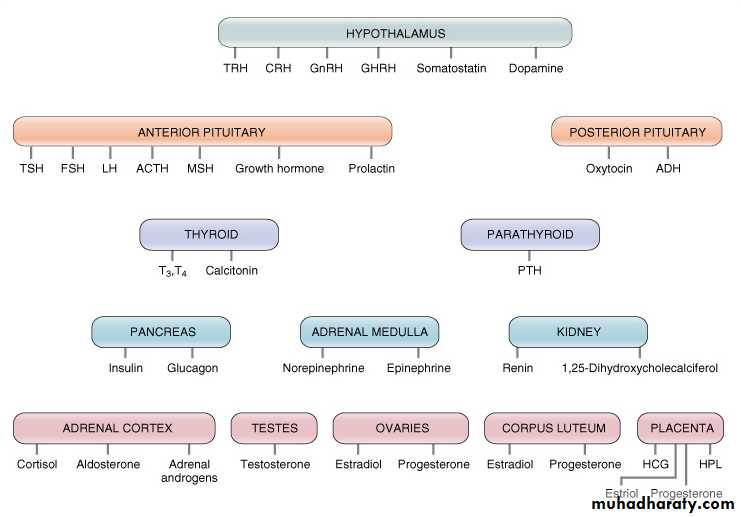
Endocrine glands and the hormones secreted by each gland
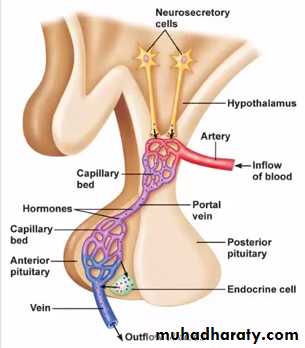
28Hypothalamic-Pituitary Axis
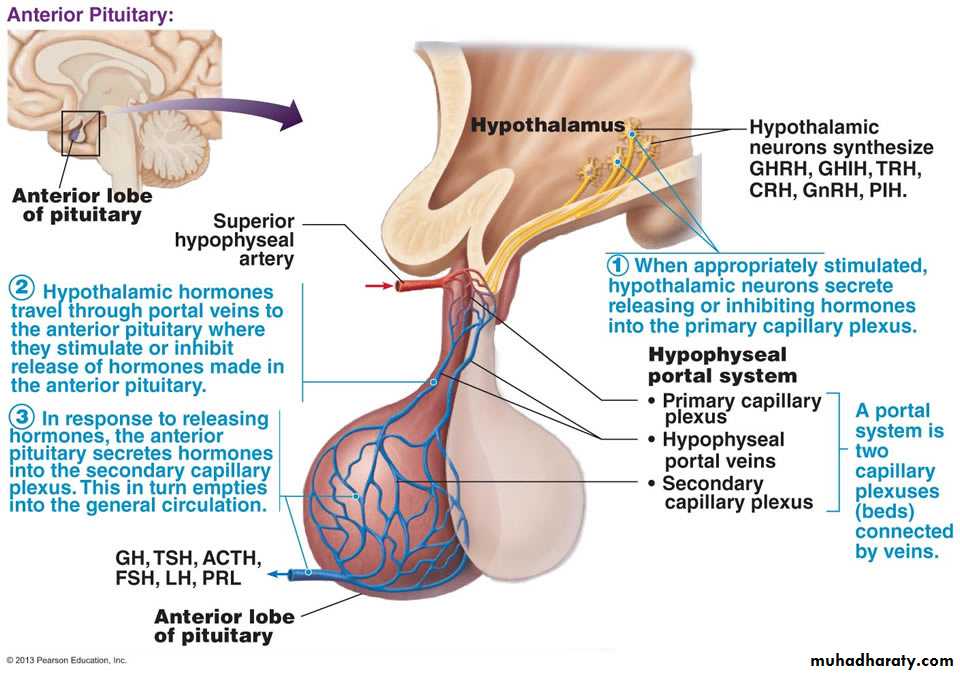
The Pituitary Gland (Hypophysis), also called “ Master gland”, it secretes 6 different hormones affecting virtually all systems of the body.The hypothalamus controls the secretion and release of anterior pituitary hormones via its release of tropic hormones.
29
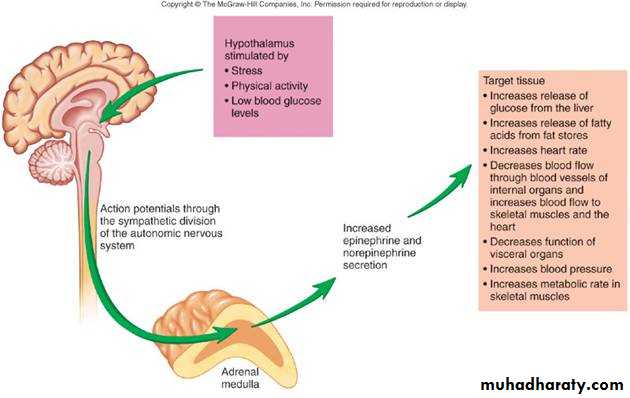
The Hypothalamus
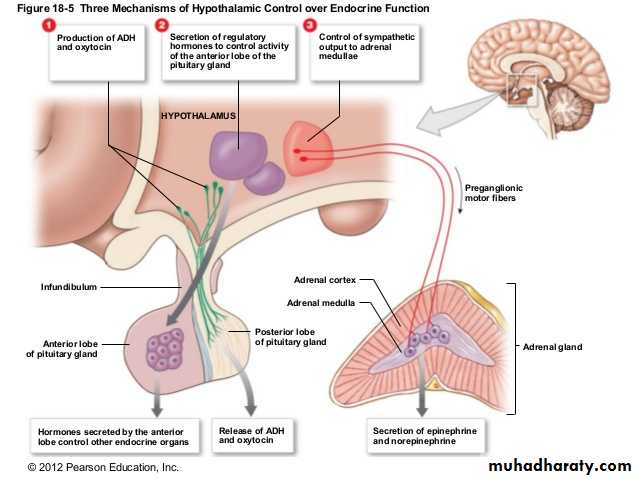
Hypothalamic control over the endocrine function is accomplished by three mechanisms:
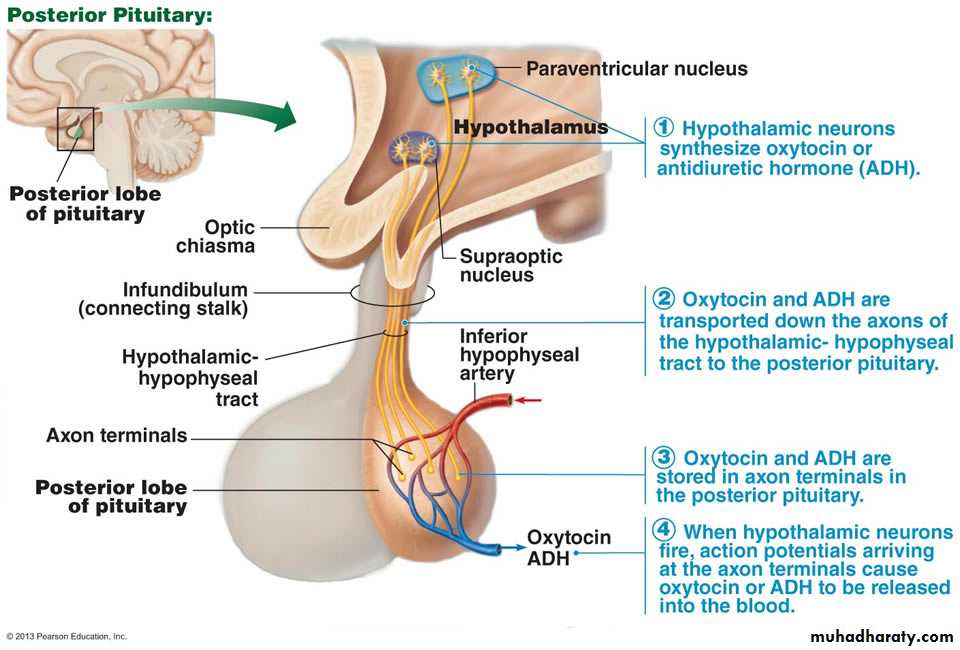
1- Production of ADH and Oxytocin.
2- Secretion of regulatory hormones that control Ant. Pit. hormones
3- Control the sympathetic outflow to the adrenal medulla
30
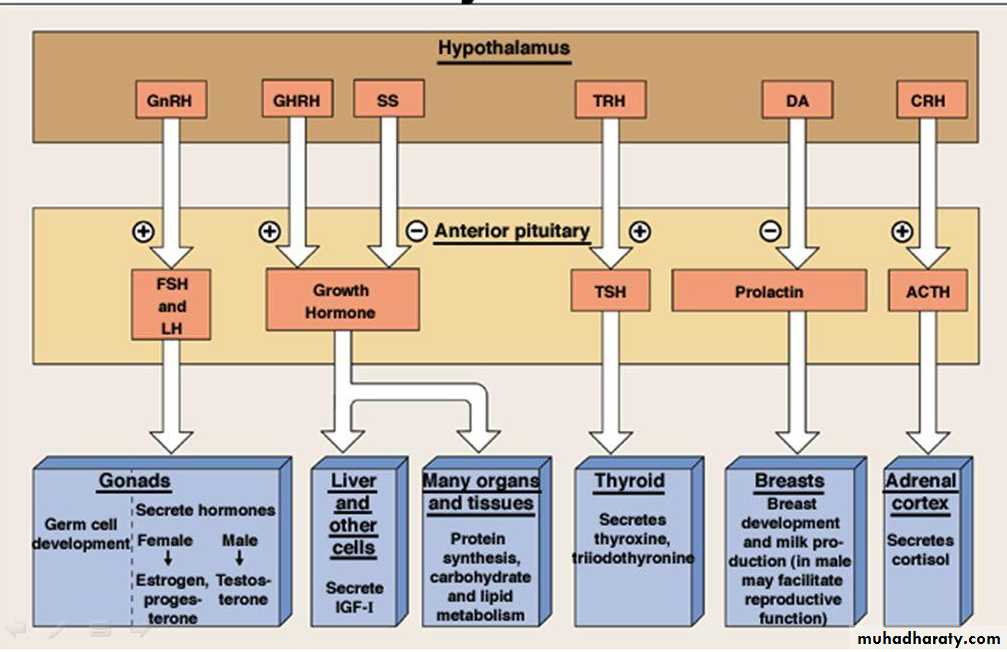
The hypothalamus releases the following Regulatory Hormones that stimulate the release of different hormones from the ant.pit. (adenohypophysis):
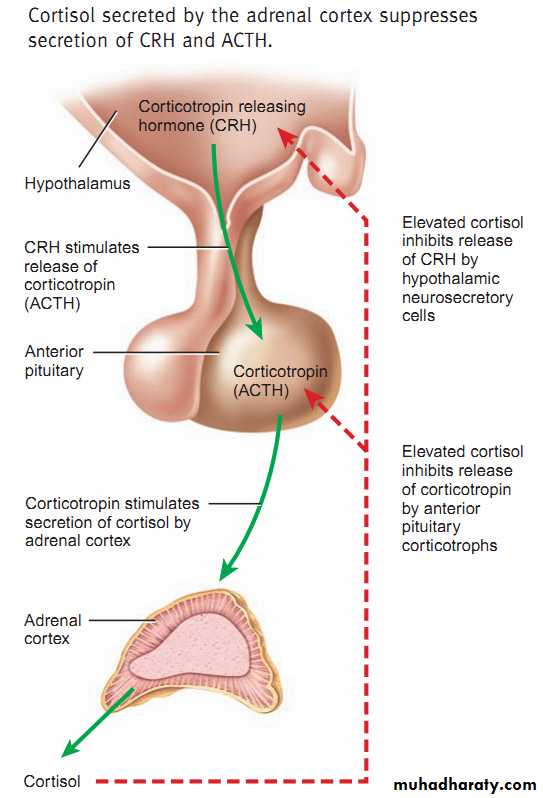
1- Corticotropin Releasing Hormone (CRH causes the release of ACTH)
2- Thyrotropin Releasing Hormone (TRH causes the release of Thyroid Stimulating Hormone TSH)
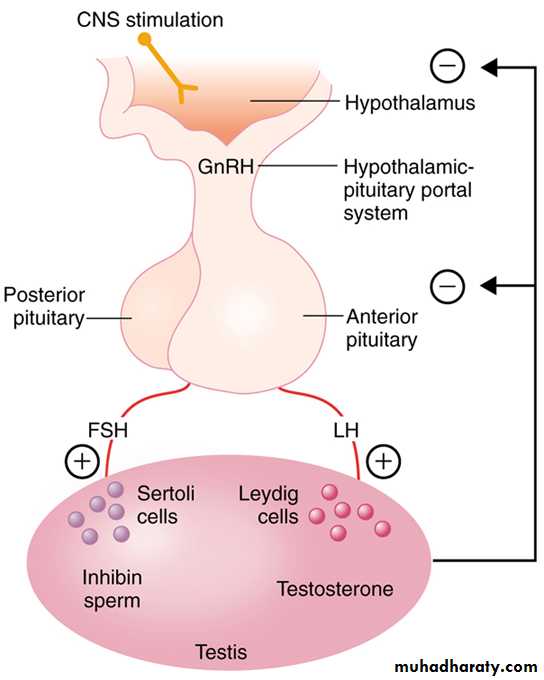
3- Gonadotropin Releasing Hormone (GnRH causes release of LH and FSH.)
4- Growth Hormone RH & Growth Hormone Inhibitory H (SS)
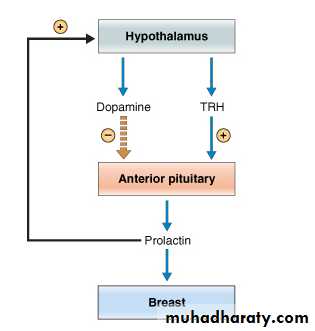
5- Prolactin IH (dopamine)
The Hypothalamus
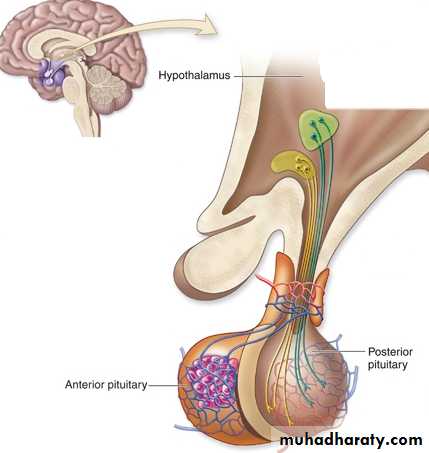
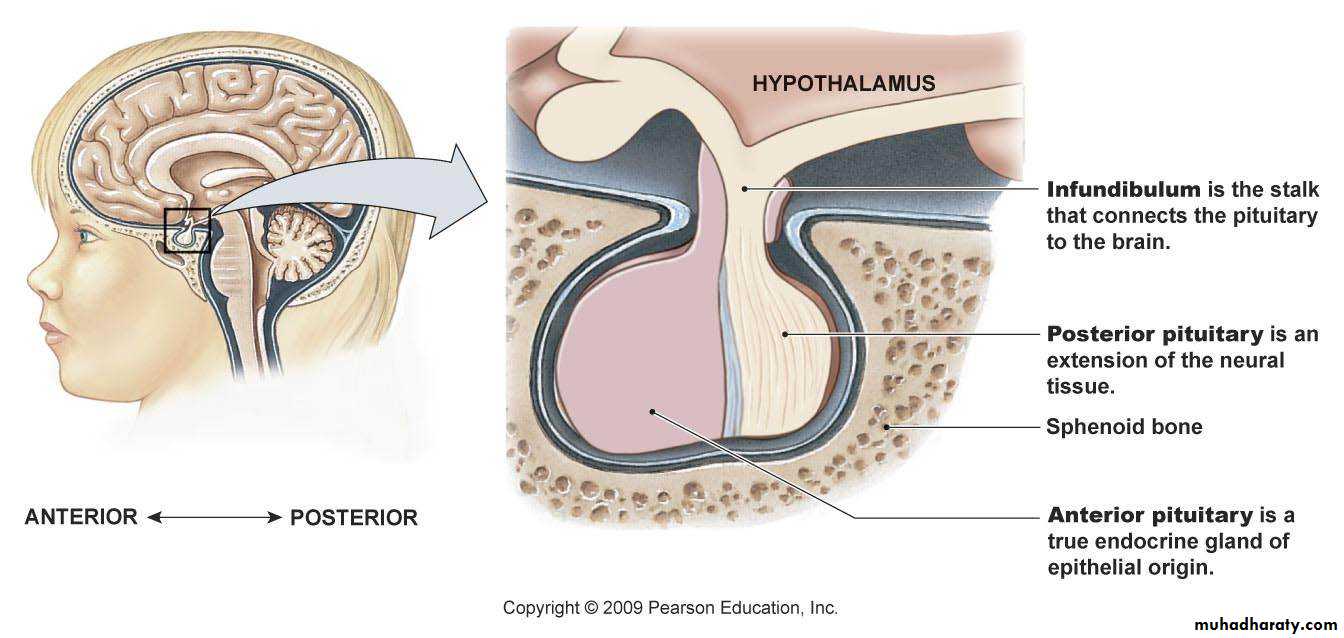
31The pituitary gland is connected to the hypothalamus via a stalk, the infundibulum, and consists of two lobes: the anterior pituitary, or adenohypophysis, and the posterior pituitary, or neurohypophysis.
32
33
The Posterior Pituitary (Neurohypophysis)
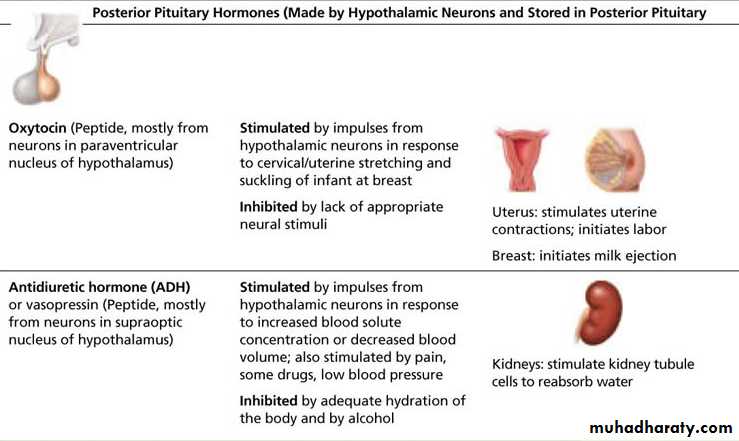
Two neurohormones are synthesized by the hypothalamus and secreted by the posterior pituitary:1- Antidiuretic hormone (ADH) or Vasopressin
Acts on kidney tubules to promote increased water reabsorption .
Its release is stimulated by: low blood volume or low blood pressure , high osmolality, and sometimes pain.
Its release is inhibited by adequate hydration, also inhibited by alcohol consumption.
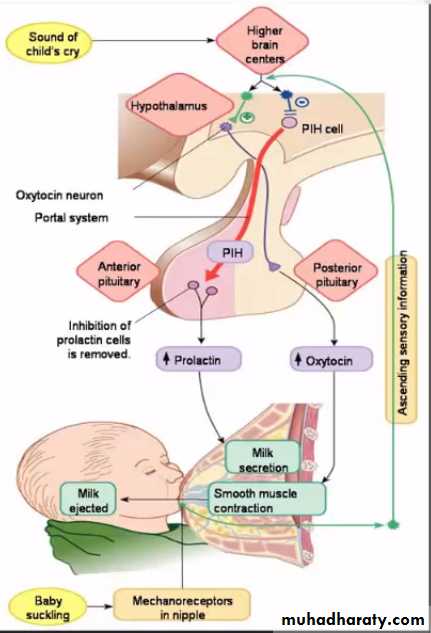
2- Oxytocin: Which acts on the smooth muscle of the uterus and breast to cause uterine contractions during childbirth and contraction of mammary myoepithelial cells, resulting in milk expulsion (let-down reflex) during nursing. Oxytocin also promotes pair-bonding between mother and child.
Oxytocin is also released during orgasm, and its release is inhibited by lack of appropriate neural stimuli.
Like ADH, oxytocin release is also inhibited by alcohol.
34
35
Diabetes Insipidus (DI)
Disease that results from low or lack of ADH.
Causes:
1- Low or lack of ADH production by the hypothalamus (Central DI)
2- Inability of the kidneys to respond to ADH (nephrogenic DI);
Symptoms: Excess urine production ( kidneys can’t concentrate urine), Polyuria, and excess water intake Polydipsia.
Differentiated from diabetes mellitus, that no glucose in urine and no hyperglycemia.
36
The Posterior Pituitary(Summary of hormones)
37
The Anterior Pituitary( Adenohypophysis )
38
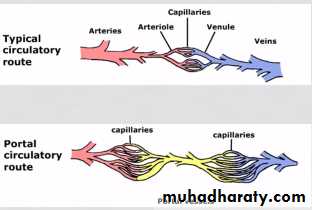
Hypothalamo Hypophyseal Portal System
Two portal systems in the body
1- Hepatic portal system2- Hypothalamo Hypophyseal Portal System
39
The Six Classical Anterior Pituitary Hormones
40
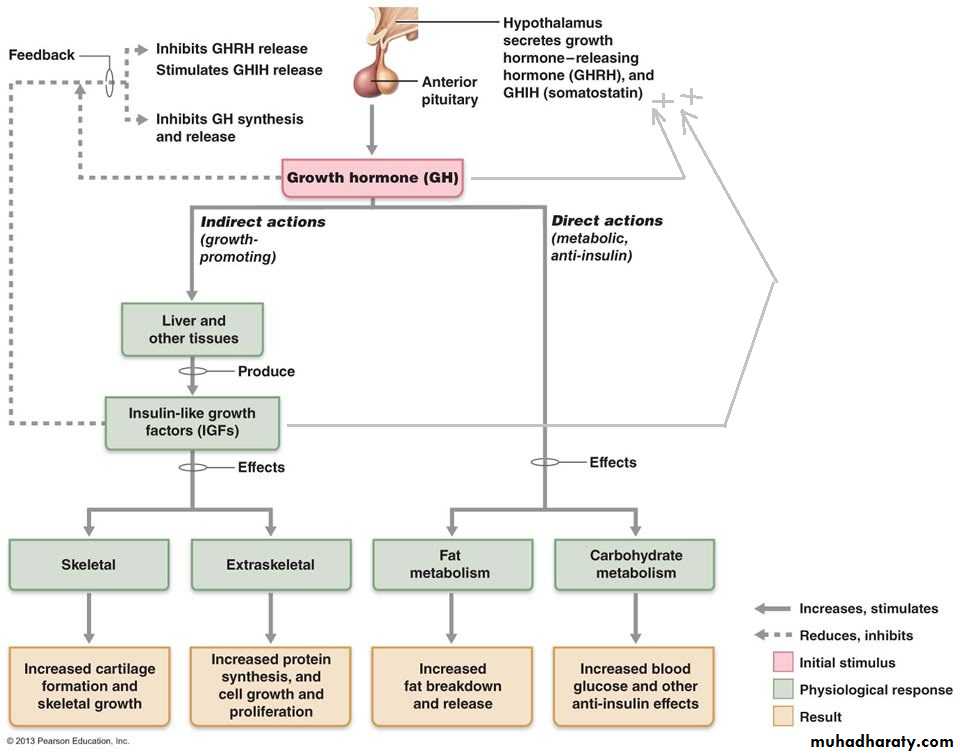
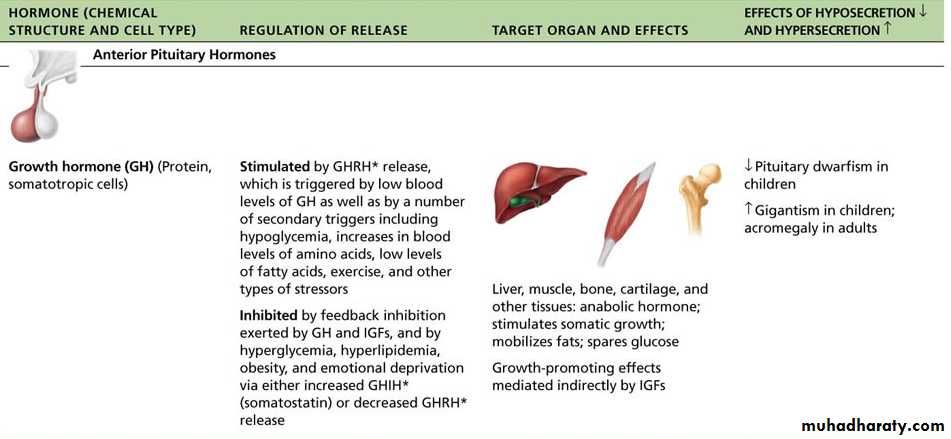
Growth hormone (GH)
GHRH, secreted from the hypothalamus, is the stimulus for GH release. The stimulus for GHRH release is low blood levels of GH as well as hypoglycemia, low blood levels of fatty acids, and high blood levels of amino acids.GH is a polypeptide and it is a stress hormone that raises the concentration of glucose and free fatty acids.
GH has both direct and indirect effects:
1- Direct effects are glucose-sparing (anti-insulin): mobilization of fatty acids for fuel (lipolysis), inhibition of insulin activity which decrease glucose utilization by most tissues, release of glucose from liver to blood (glycogenolysis), and stimulation of amino acid uptake by cells.
2- Indirectly (through insulin-like growth factors, IGFs) which are produced mostly by the liver. IGFs stimulate body cells growth and proliferation through new protein synthesis, also stimulate increase cartilage formation and skeletal growth.
41
42
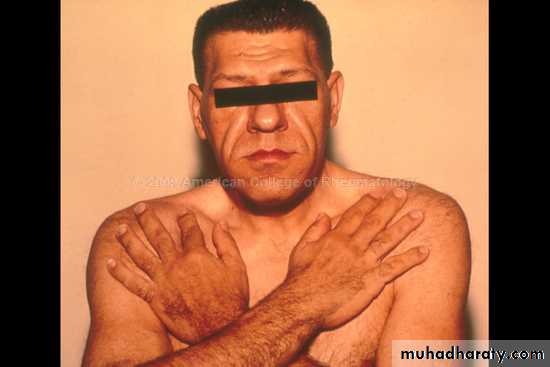
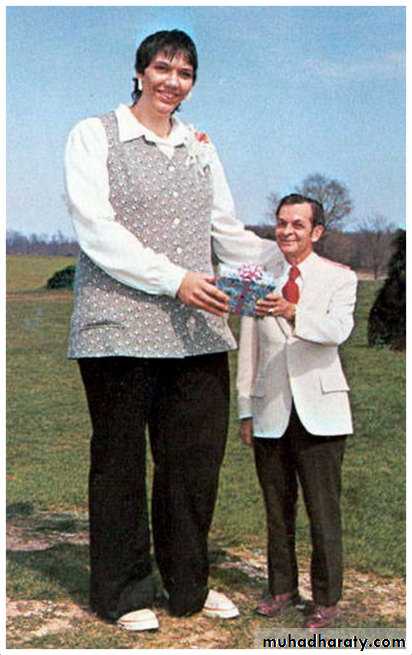
GH Imbalance
Hyposecretion of GH results in pituitary dwarfism in children.Hypersecretion of GH in childhood results in gigantism.
Hypersecretion of GH in adulthood causes acromegaly (increase in size of flat bones after epiphyseal plates of long bones have been sealed).
43
Acromegaly Vs Gigantism
44Pituitary dwarf Vs Achondroplasia
45GH Summary
46
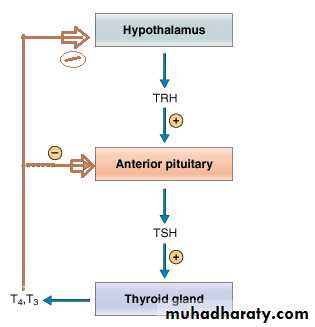
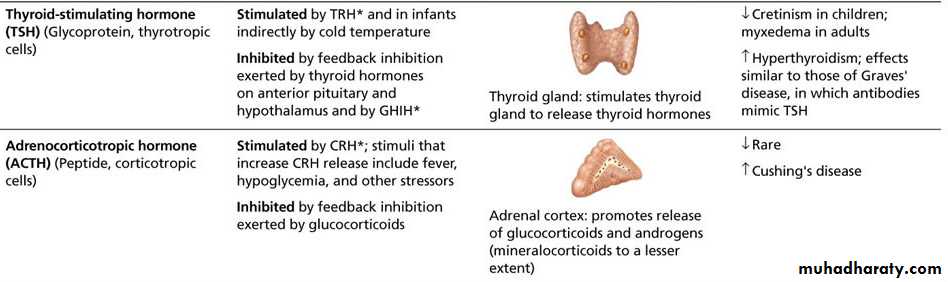
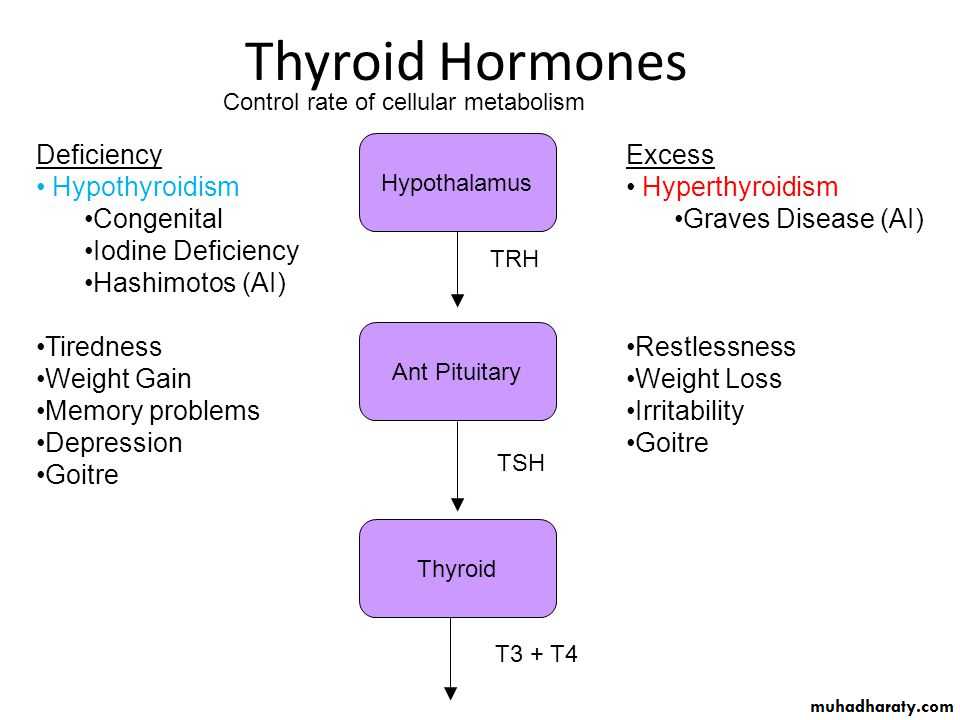
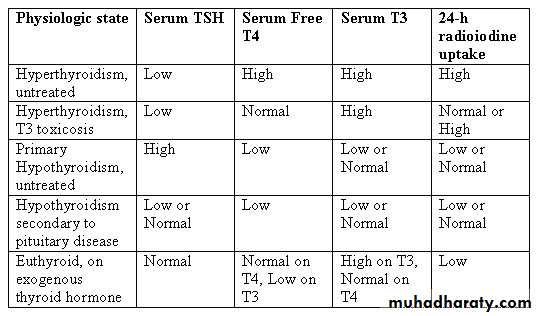
Thyroid stimulating hormone (TSH)
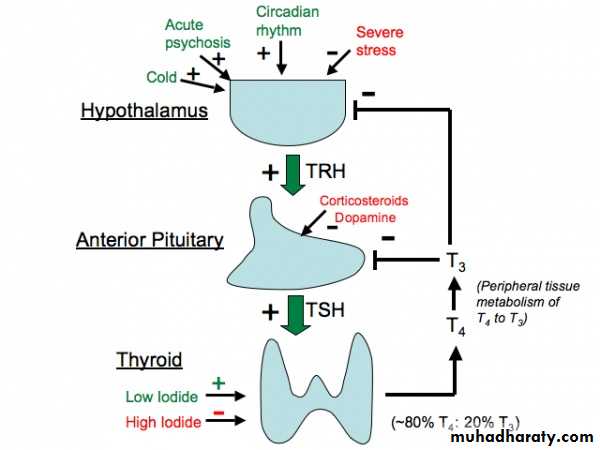
TSH is a tropic hormone that stimulates normal development and secretion of the thyroid gland. Thyroid releasing hormone (TRH) from the hypothalamus stimulates TSH release;Thyroid hormone (Thyroxin) exerts negative feedback control of both TRH and TSH.
47
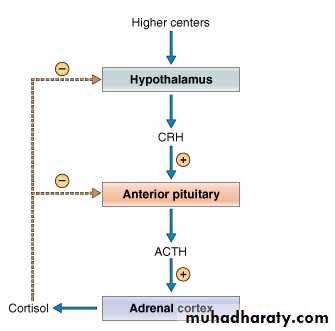
Adrenocorticotropic Hormone (ACTH)
- Adrenocorticotropic hormone (ACTH) is a tropic hormone stimulates the adrenal cortex to release glucocorticoid hormones (e.g. cortisol)
CRH, ACTH, Glucocorticoids levels cycle through the day being highest level in the morning. ( circadian or diurnal rhythm) .
Fever, hypoglycemia, and stress can also affect CRH, ACTH, Glucocorticoids levels
48
TSH & ACTH summary
49
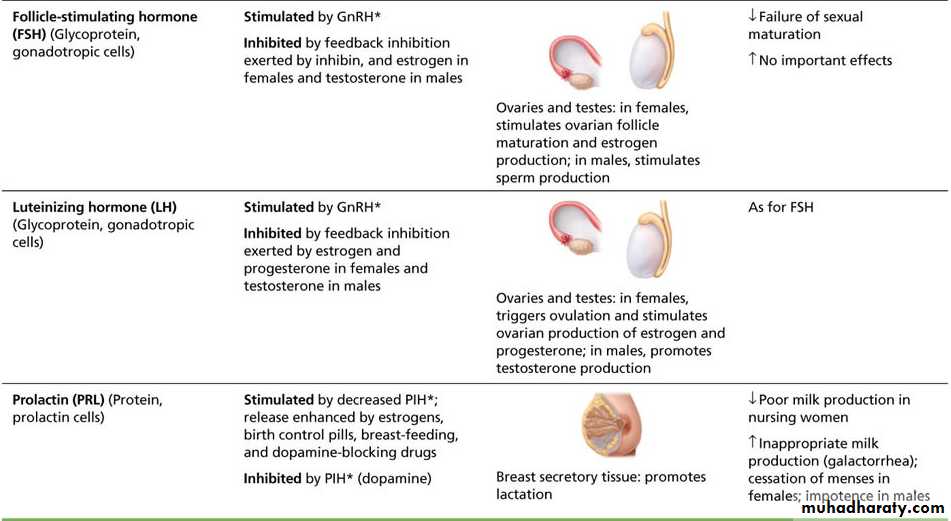
Gonadotropins (FSH and LH)
- Follicle-stimulating hormone (FSH) is a tropic hormone that stimulates gamete production (sperms or ova).- Luteinizing hormone (LH) is a tropic hormone that promotes ovulation in females and production of gonadal hormones.
- Gonadotropins release is regulated by GnRH from the hypothalamus.
50
Prolactin (PRL)
It is not tropic hormoneIt stimulates mammary gland development and milk production in females and may enhance testosterone in males.
Regulation
Prolactin Inhibiting Hormone (PIH)(dopamine) from hypothalamus.
Rising estrogen levels prior to menstruation causes increase PRL secretion and (breast tenderness)
Nursing (lactation): stimulates its release
TRH : stimulates PRL release
51
52
FSH, LH & PRL summary
53
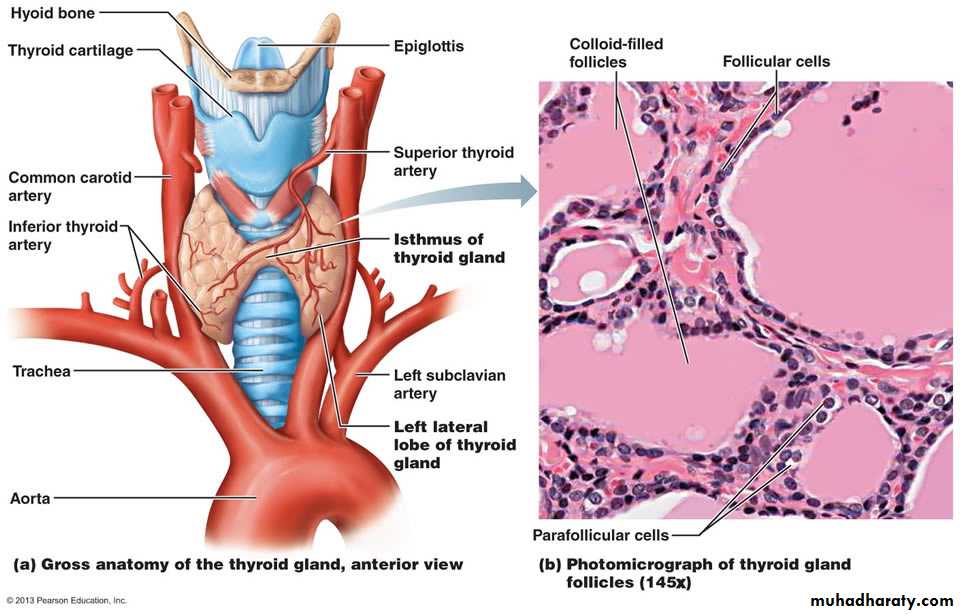
The Thyroid Gland
Hormones: T4 Thyroxin, T3 Triiodothyronin and Calcitonin
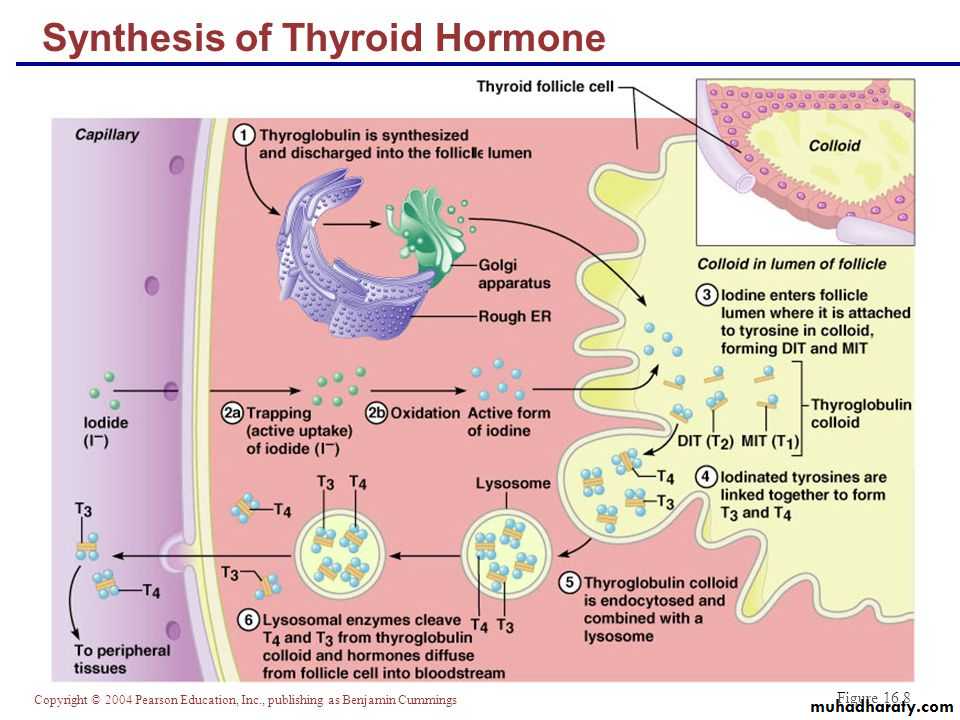
54Iodine is essential for synthesis of T4 and T3
55Thyroid Hormones
Thyroid hormone consists of two amine hormones: thyroxin (T4) and triiodothyronine (T3), that act on all body cells to increase basal metabolic rate and body heat production.While not strictly necessary for life, thyroid hormones have profound effects on many essential physiologic processes, such as development, growth and metabolism, and deficiency in thyroid hormones is not compatible with normal health.
56
Physiologic Functions of Thyroid Hormones
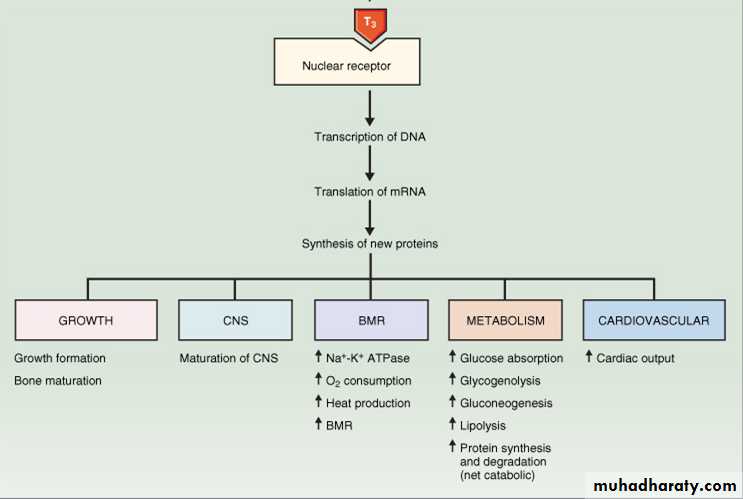
1- Metabolism: Thyroid hormones stimulate diverse metabolic activities in most tissues, leading to an increase in basal metabolic rate. One consequence of this activity is to increase body heat production, which seems to result from increased oxygen consumption and rates of ATP hydrolysis. It binds to mitochondria and increase the synthesis of enzymes involved in ATP productionLipid metabolism: T3,T4 stimulate fat mobilization, leading to increased concentrations of fatty acids in plasma. They also enhance oxidation of fatty acids in many tissues. Finally, plasma concentrations of cholesterol and triglycerides are inversely correlated with thyroid hormone levels , so one diagnostic point of hypothyroidism is increased blood cholesterol concentration.
Carbohydrate metabolism: Thyroid hormones stimulate almost all aspects of carbohydrate metabolism, including enhancement of insulin-dependent entry of glucose into cells and increased gluconeogenesis and glycogenolysis to generate more free glucose. Also increase the synthesis of enzymes involved in glycolysis.
57
2- Growth and development: Thyroid hormones are clearly necessary for normal growth (stimulate GH & IGF), so growth-retardation observed in thyroid deficiency in children.
Normal levels of thyroid hormone are essential for the development of the fetal and neonatal brain.
3- Central nervous system: Thyroid hormones are essential for both CNS development and function, TH amplify the effects of sympathetic NS (increase the number of adrenergic receptors especially on blood vessels); (Permissive effect).
4- Cardiovascular system: Thyroid hormones increases heart rate, cardiac contractility and cardiac output. They also promote vasodilation, which leads to enhanced blood flow to many organs.
5- Reproductive system: Normal reproductive behavior and physiology is dependent on having essentially normal levels of thyroid hormone. Hypothyroidism in particular is commonly associated with infertility.
(Permissive effect).
58
59
60
Thyroid hormones secretion is regulated by TSH (anterior pituitary), TRH (hypothalamus)
1- TRH binds to specific receptors and mediates TSH release via G-protein activation;2- TSH binds to its receptors and stimulates thyroid hormone production and release by using cAMP and G-protein mechanism.
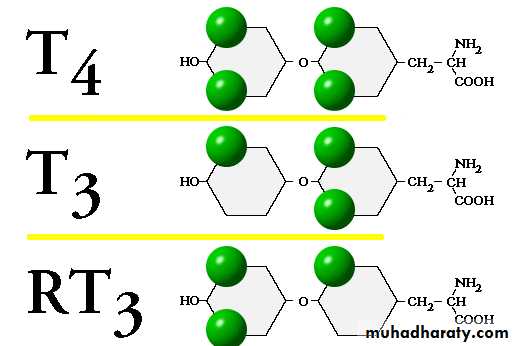
3- The active form of thyroid hormone is T3, which is mainly produced in peripheral tissues from T4 (by deiodination). T3 binds to specific nuclear receptors to mediate most of its effects.
4- Thyroid hormones then diminish TSH and TRH production through a negative feedback mechanism
61
Thyroid hormones regulation
62
Transport of Thyroid Hormones in Plasma
T4 (and to less extent, T3) bind several serum proteins, mainly:1- Thyroid binding globulin (TBG) present in relatively low concentrations, but with high affinity for T4, binds about 2/3 of T4 and T3.
2- Transthyretin (old name was thyroid-binding prealbumin)
3- Albumin.
- Only about 0.02% of T4 (and 0.2% of T3) are free in plasma
- Only the free thyroid hormone that is the active form.63
Thyroid Hormones Metabolism
About 90% of the thyroid hormones released is in the form of T4 which is an inactive form and must be converted to T3.10% of released hormones is T3 (active form)
T3 and T4 once released into the blood they bind to carrier plasma proteins (mostly TBG)
In the liver, around 60% of the inactive T4 is converted to T3. Another 20% gets converted to reverse T3 which is inactive and excreted from the body. The last 20% is converted to T3S (T3 Sulphate) and T3AC (triiodo-thyro-acetic acid) which are inactive forms of T3.
T3S and T3AC are then converted into the active form of T3 by bacteria located in the gastrointestinal tract. It can then be used by the cells of the body to fuel metabolism.
64
Most of the T3 of the body is produced from the conversion of T4 to T3 that takes place outside the thyroid gland in the body’s tissues, T4 is converted to T3 by an enzyme called 5′-deiodinase, which is found in many tissues of the body.
Peripheral conversion of T4, not only produce T3, but also reverse T3 (RT3).
T4 has a small amount of activity at the target cells
T3 is four times more active than T4
RT3 has no activity at all.
65
Thyroxin (T4)
T4 is considered as a prohormone , a precursor of T3.T4 serves as a steady, constant supply of the more active T3.
T4 is a highly lipophilic hormone, and binds serum proteins much more than its active form, T3.
T4 synthesis starts when the thyroid gland actively traps substantial amounts of the micronutrient iodine. There is a specific ATP-requiring pump that can maintain a concentration of iodine in the thyroid follicular cell that is 30 to 100(+) times the plasma level. (This apical transporter protein is called Pendrin )
Apart from pendrin, thyroid cells also contain a second iodide transporter called "NIS", the sodium iodide symporter ).
66
Triiodothyronin T3
Tissue effects of T3 include:
Increased expression of Na/K ATPase;
Increased sarcolemmal calcium uptake
Increased beta adrenergic receptor levels in myocardium;
increased hepatic production of sex steroid binding globulin;
Bone: (cartilage ossification, maturation of epiphyses, chondrocyte maturation; - thyroid hormone has a direct effect on bone, and indirect effects through GH release and IGF-1 action);
Neuronal: cortical growth, axonal and dendritic growth, myelination; T3 is vital for normal brain development, and fetal TSH secretion starts by about 11-12 weeks. The auditory and visual sensory systems appear particularly dependent on T3
Renal: increased renal plasma flow and GFR
67
Thyroid Disease States
Disease is associated with both inadequate production and overproduction of thyroid hormones. Both types of disease are relatively commonHypothyroidism may result from
1- Inadequate TRH release,
2- Inadequate TSH release,
3- Dysfunction of the thyroid gland itself, inadequate dietary iodine, or autoimmune destruction (Hashimoto's autoimmune thyroiditis).
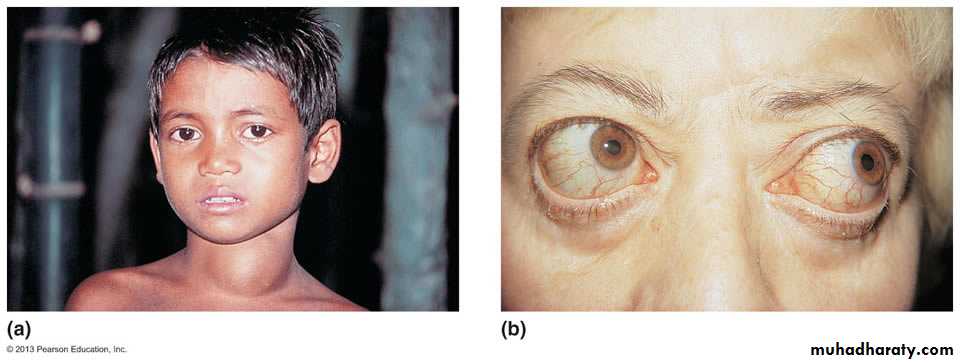
Full blown hypothyroidism in adults is known as myxedema (mucous swelling). If myxedema results from lack of iodine the thyroid gland continues to make thyroglobulin but can't iodinate it, resulting in an enlarged thyroid, or colloidal/endemic goiter (Figure a)
Hypothyroid in infants leads to Cretinism, if undetected early can lead to severe mental retardation.
68
Hyperthyroidism
The most common cause of hyperthyroidism is an autoimmune disease (Graves' disease) in which anti-TSH receptor antibodies bind to TSH receptors on the thyroid and stimulate continuous thyroid hormone release. The feedback mechanism is short-circuited because the production and release of thyroid hormone is not dependent on TSH.Exopthalmos may occur, indicating edema and fibrosis of tissue behind the eyes (Figure b)
69
70
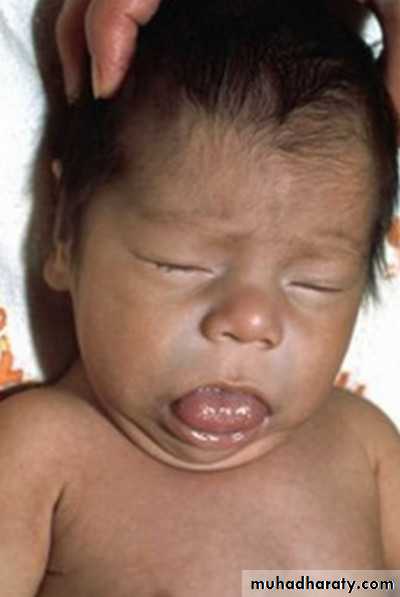
When hypothyroidism occurs in the perinatal period and is untreated, it results in an irreversible form of growth and mental retardation called cretinism.
The infant is floppy, big tongue, poor feeding, constipation, prolonged jaundice, dwarf and deaf-mute
71
Thyroid Function Tests
72
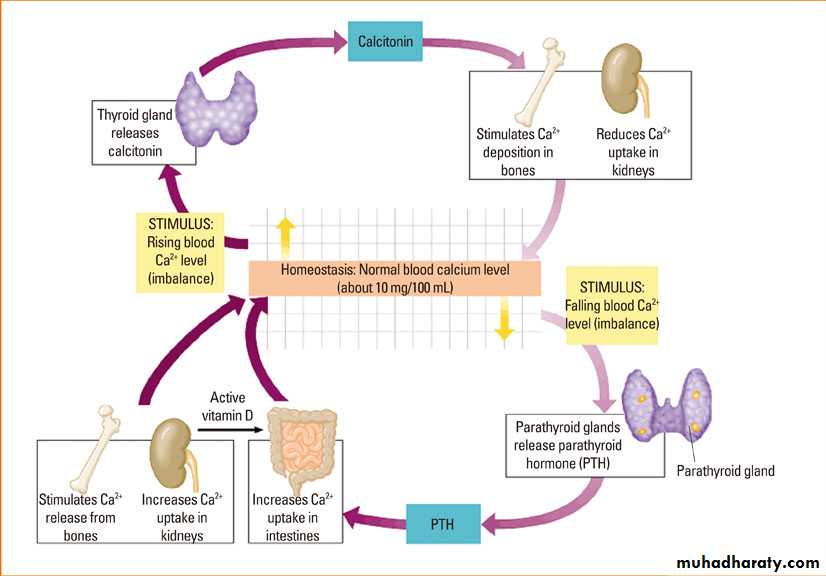
Calcitonin
Produced by parafollicular or "C" cellsIt is a peptide hormone
Act on bone tissue by inhibiting osteoclast activity and stimulating Ca2+ uptake and incorporation into the bone matrix, so it increases bone density (bone sparing effect) and lower blood calcium.
73
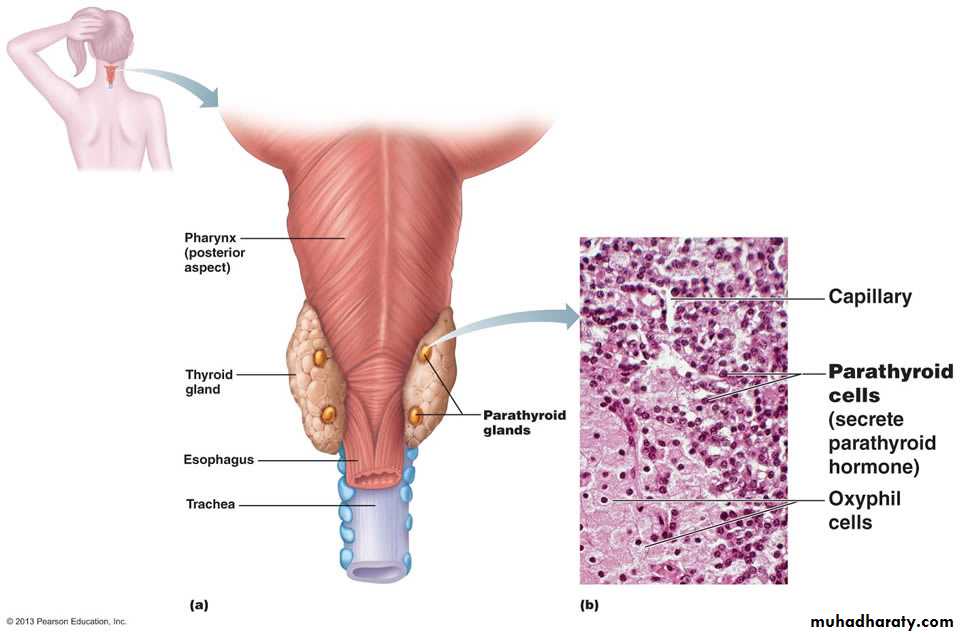
The Parathyroid Glands
The parathyroid glands contain chief cells that secrete parathyroid hormone, or parathormone (PTH).74
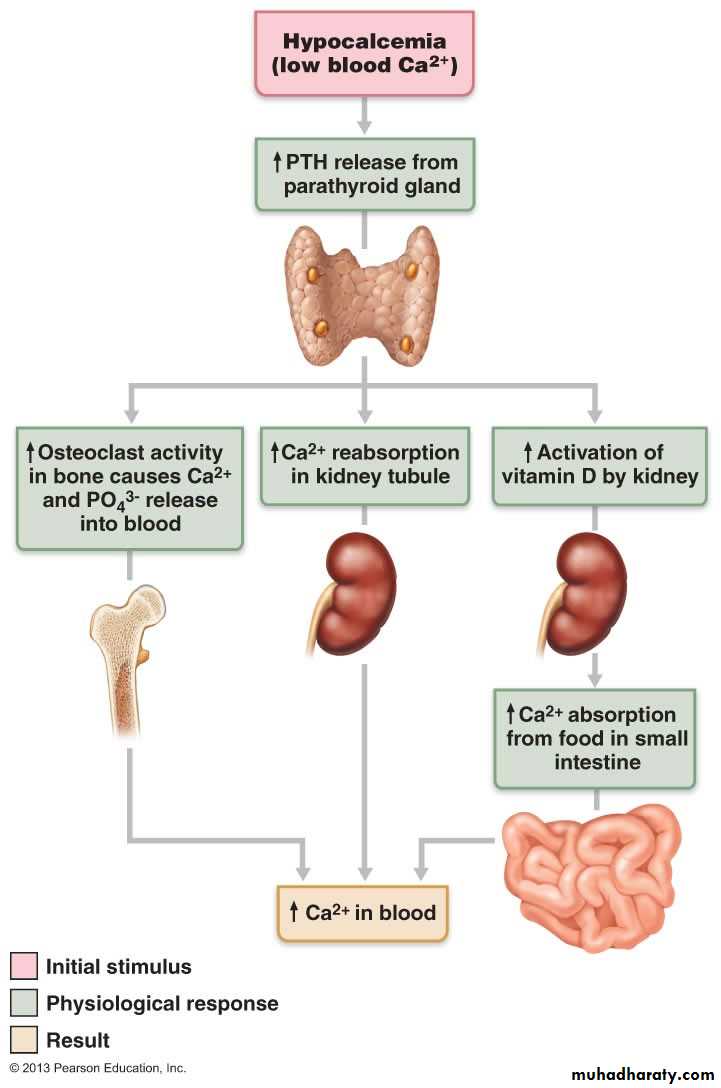
Parathormone (PTH)
PTH increases blood calcium levels by1- Accessing stored Ca++,
It stimulates osteoclasts so mobilizing Ca++ and PO43+ from bone.
2- Increasing absorption of Ca++,
It increases Ca++ absorption by stimulating renal activation of vitamin D3 which enhances intestinal absorption of Ca++
3- Inhibiting loss of Ca++ ,
It stimulates Ca++ reabsorption at the kidney and also stimulates the excretion of PO43+
75
76
Calcium Homeostasis
77
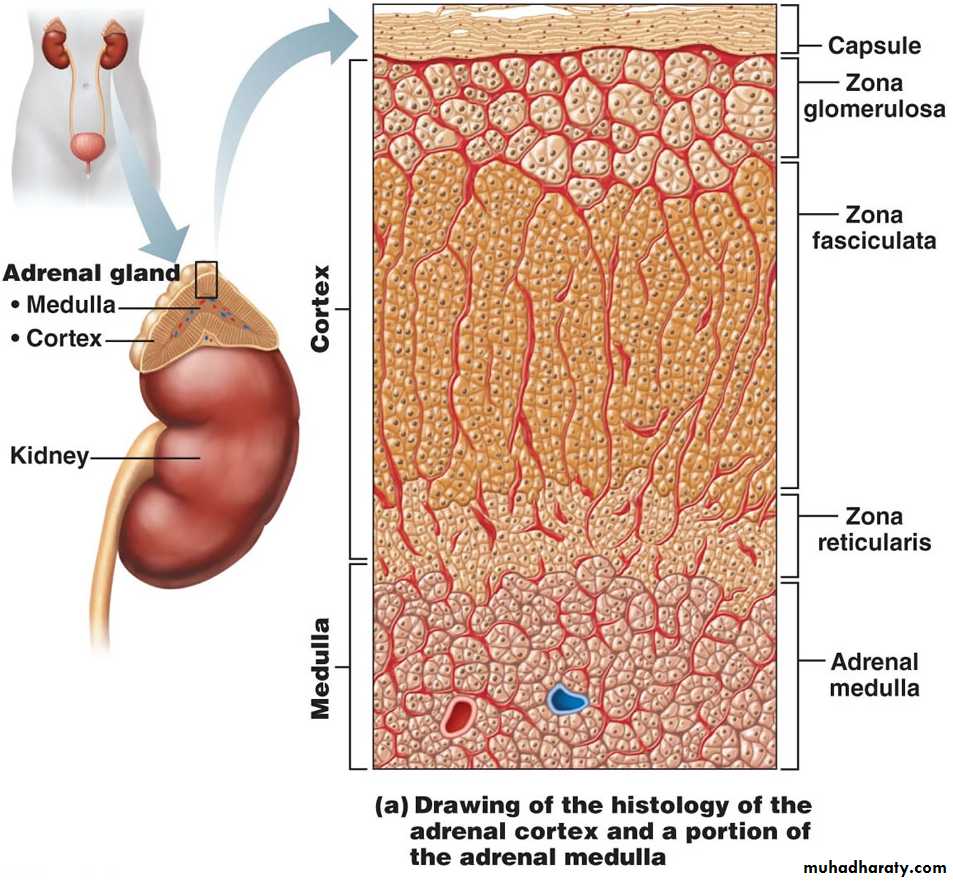
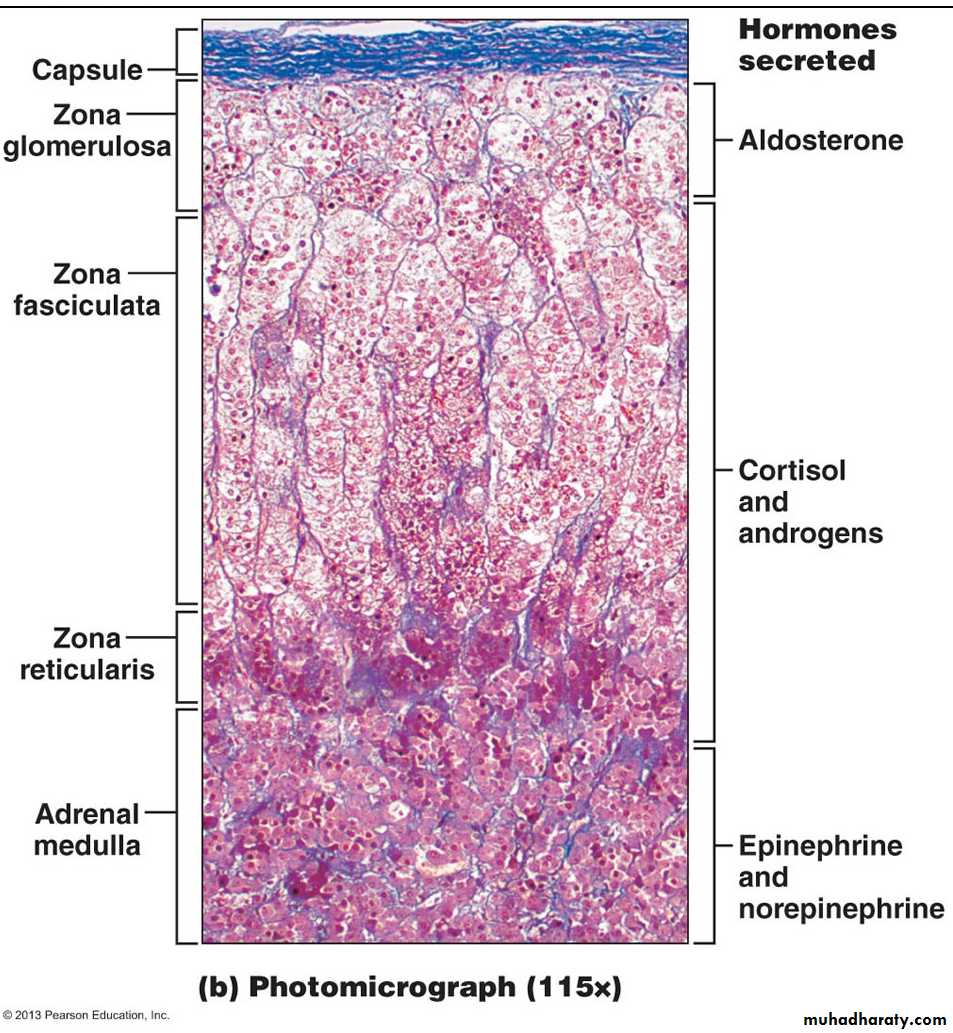
The Adrenal (Suprarenal) Glands
The adrenal glands, or suprarenal glands, consist of two regions: an inner adrenal medulla and an outer adrenal cortex, the two regions behave like two endocrine glands.Adrenal Medulla : secretes Epinephrine (Adrenalin) and Norepinephrine (Noradrenalin); considered as part of the ANS.
Adrenal Cortex : produces corticosteroids from three distinct regions: the zona glomerulosa, the zona fasciculata, and the zona reticularis.
Corticosteroids
Mineralocorticoids (Aldosterone) which regulate electrolytes of ECF.
Glucocorticoids (Cortisol) which accelerate the rate of glucose synthesis and glycogen formation
78
79
80
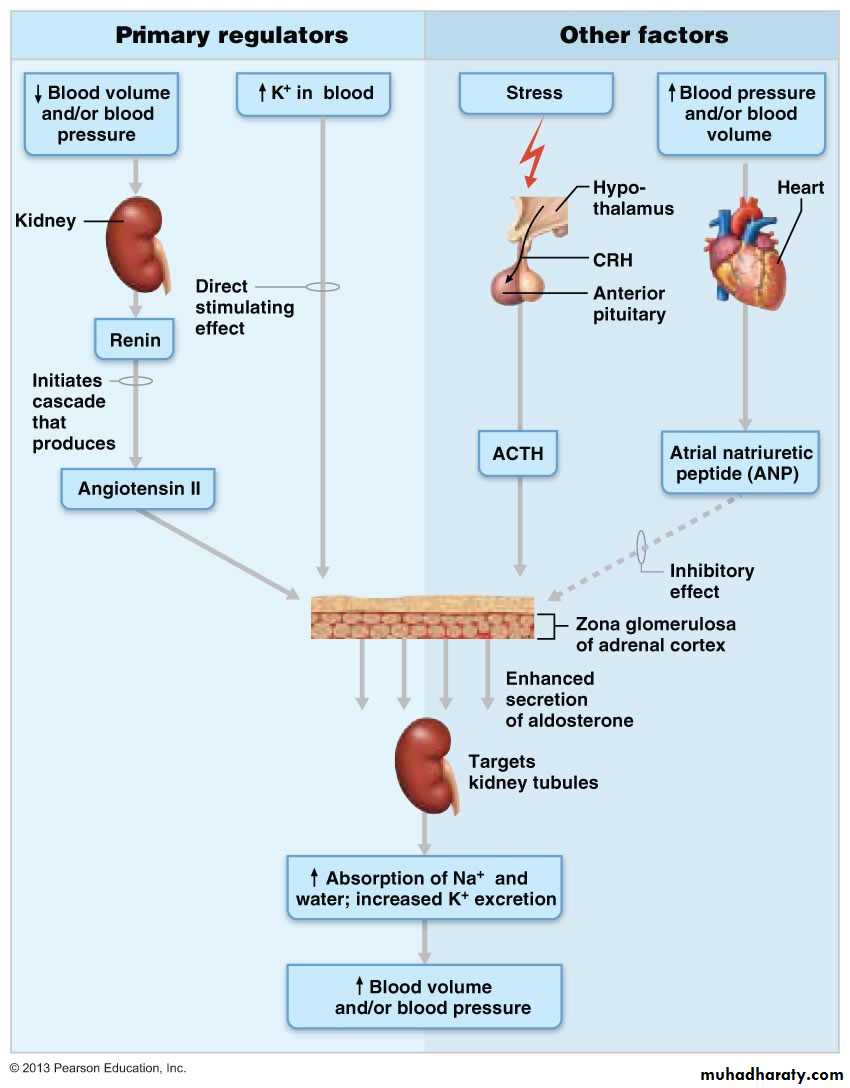
Mineralocorticoids (Aldosterone)
Mineralocorticoids, mostly aldosterone secreted by glomerulosa, They are essential for regulation of electrolyte concentrations of extracellular fluids (Na+ & K+).Action of aldosterone:
1- Na retention : decrease excretion of Na from kidneys, saliva, sweat and gastric juices
2- Water retention
3- K secretion and excretion
Regulation:
1- High plasma K stimulates its secretion
2- High levels of ACTH during stress will cause more aldosterone release.
3- Cardiovascular related control
a- Renin-Angiotensin-Aldosterone system or mechanism (angiotensin II stimulates the release of aldosterone).
b- Atrial natriuretic peptide (ANP): decreases aldosterone release.
81
82
Zona Fasciculata and Reticularis
Fasciculata: primarily glucocorticoids are released in response to stress through the action of ACTH. Glucocorticoids, like cortisol, are glucose sparing stress related hormones.Reticularis: primarily gonadocorticoids are mostly weak androgens, which are converted to testosterone and estrogens in the tissue cells.
83
Glucocorticoids (Cortisol)
Target: most cells of the bodyFunctions: (glucose sparing and stress related hormone)
Energy metabolism
Keep blood glucose levels constant
Maintain blood pressure by acting as vasoconstrictors
Under stress :
- Gluconeogenesis (formation of glucose from fat and proteins)
Glucose sparing effect
- Anti-inflammatory (anti-immune) effect
84
85
Regulation
ACTH and CRHUnder stress , CNS overrides inhibition of cortisol on CRH
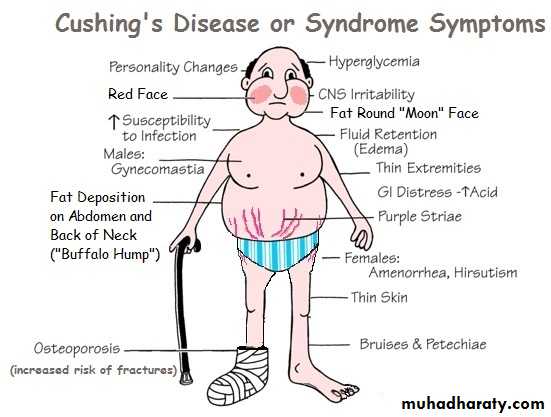
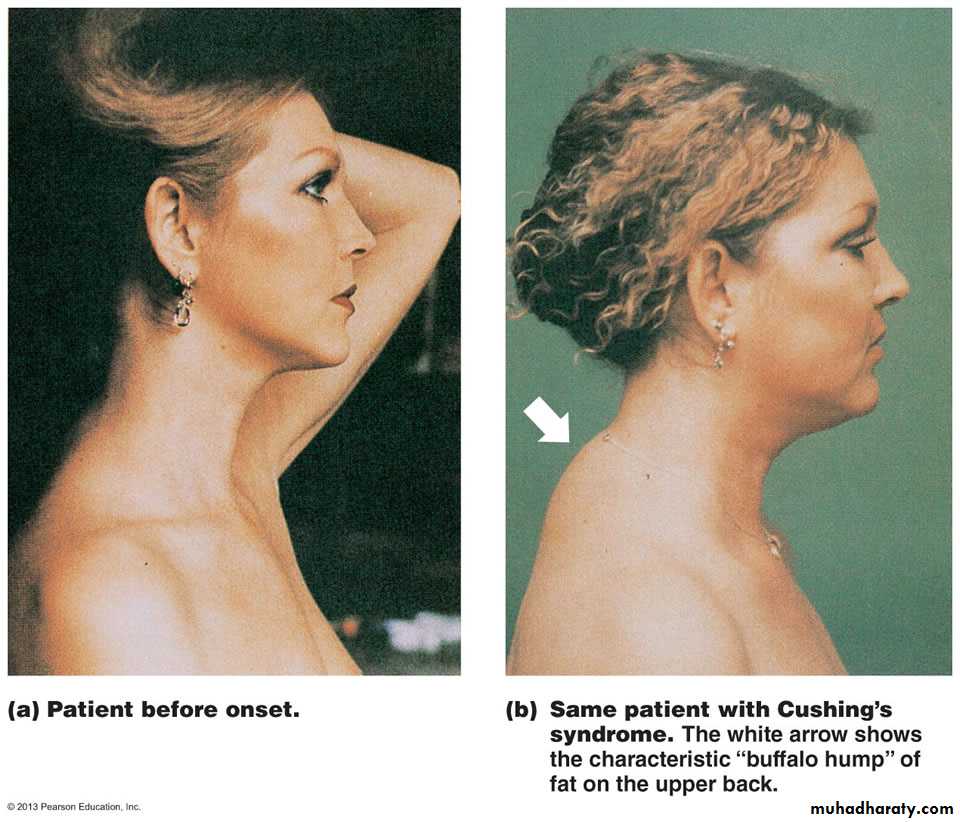
Excess Glucocorticoids
Cushing's syndrome/disease is caused by an excess of glucocorticoids.Causes:
- Adrenal gland tumor or hyperplasia (glucocorticoid producing tumor)
- ACTH producing tumor
- Long term administration of glucocorticoids.
Cushing's syndrome is characterized by elevated blood glucose, loss of muscle and protein from bone, and hypertension and edema due to salt and water retention. Anti-inflammatory effects can cause increased susceptibility to disease and poor wound healing.
The signs include "moon" face (due to edema), and redistribution of fat to the back of the neck (buffalo hump) and abdomen.
86
87
88
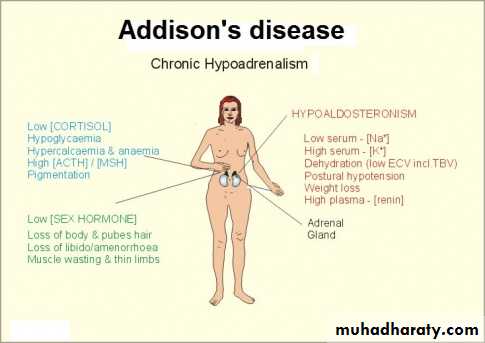
Glucocorticoid (Cortical) Insufficiency
Addison's disease is a disease of cortical insufficiency,(hyposecretion of adrenal cortex hormones)
Resulting in weight loss, hypoglycemia ,hyponatremia, and hyperkalemia (due to low aldosterone).
The patient complain of dizziness, fatigue and there will be severe dehydration and hypotension.
Disruption of the feedback mechanism that controls POMC (Pro-opio-melanocortin) release may result in over production of MSH and a general bronzing/darkening of the skin.
Treatment: corticosteroids replacement therapy
8990
Adrenal Medulla
The adrenal medulla contains chromaffin cells that synthesize and release epinephrine and norepinephrine (stimulus is acetylcholine released by preganglionic sympathetic fibers).
Considered as part of the ANS
91
Stress Response
92
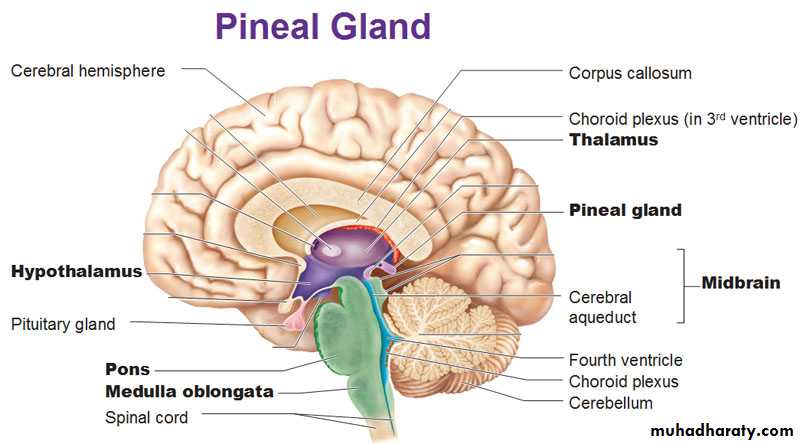
The pineal gland is located behind the third cerebral ventricle in the midline (between the two cerebral hemispheres) of the brain, its weight about 0.10 gram
93
Pineal Gland Function
Hormone: Melatonin (derivative of the amino acid tryptophan)1- Sleep-wake cycles (Diurnal cycle)
- Peaks at night, lowest at noon
- Its secretion increases soon after a person is placed in the dark and decreases soon after exposure to light.
The hypothalamus (which controls the biological clock) has high number of melatonin receptors.
2- Influences sexual development ( may have antigonadotropic effect in children)
Its production is high in infancy and childhood and declines with age, and abnormally high level of melatonin in children is associated with delayed sexual development.
3- Melatonin has been used to treat conditions such as depression, insomnia, and jet lag, but its efficacy for these purposes is controversial.
94
The Pancreas
95
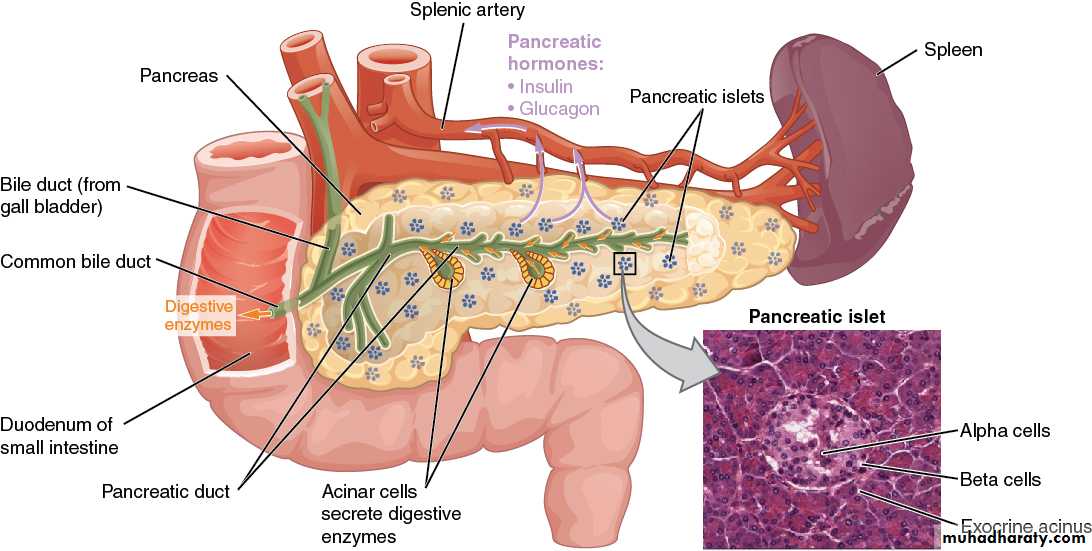
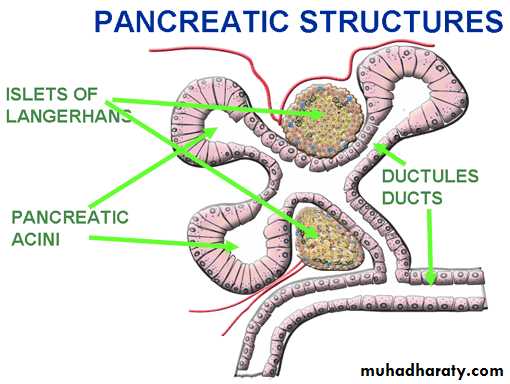
The pancreas has two glandular functions
A- Exocrine gland (Acini)Secrete digestive enzymes and it is part of the GIT.
B- Endocrine gland
(Islets of Langerhans)96
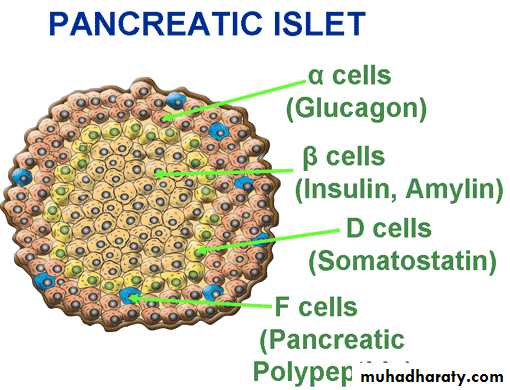
1- alpha cell produces glucagons
2- beta cells secrete both insulin and amylin.3- D cells, which secrete somatostatin
4- F cells that produce pancreatic polypeptide.
97
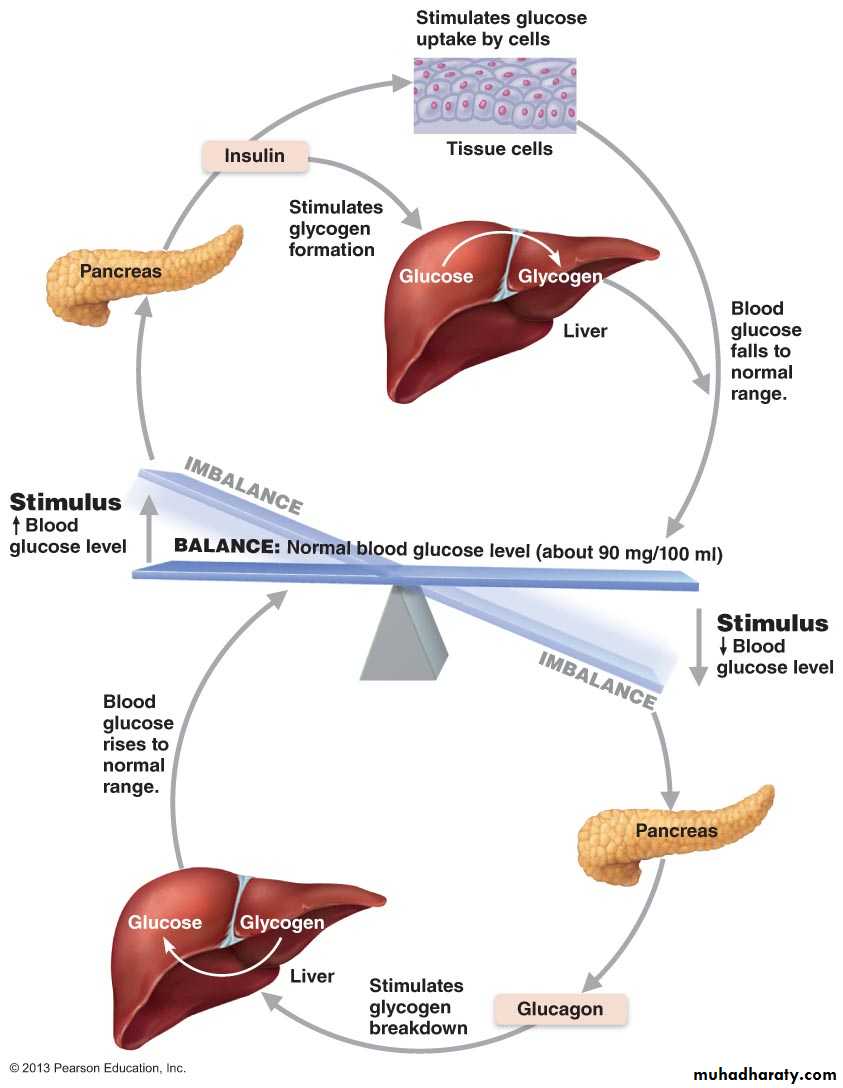
Insulin
Introduction:It is synthesized and secreted by the β cells, lowers blood sugar levels by
1- Enhancing membrane transport of glucose into body cells,
2- Inhibiting glycogenolysis,
3- Inhibiting gluconeogenesis.
(Brain, kidney and liver don't need insulin to take up glucose from blood.)
Insulin is an anabolic hormone and will stimulate not only glucose uptake but also storage in the form of glycogen (glycogenesis), fat (lipogenesis) and amino acid incorporation into proteins (inhibits amino acid breakdown by liver to form new glucose molecules - gluconeogenesis).
Stimuli for insulin release are primarily high blood glucose levels but insulin release is also potentiated by rising blood levels of amino acids and fatty acids and release of acetylcholine by parasympathetic neurons (all of these things happen after a meal).
98
Insulin, hormone of the “ Firsts”
- First hormone to be isolated from animal and administered therapeutically to humans.First hormone to have its primary and tertiary structure determined.
First hormone to have its mechanism of action elucidated
First hormone to be measured by radioimmunoassay
First hormone known to be synthesized from a larger precursor (prohormone)
First hormone to be synthesized using recombinant DNA technology
99
Structure and Synthesis of Insulin
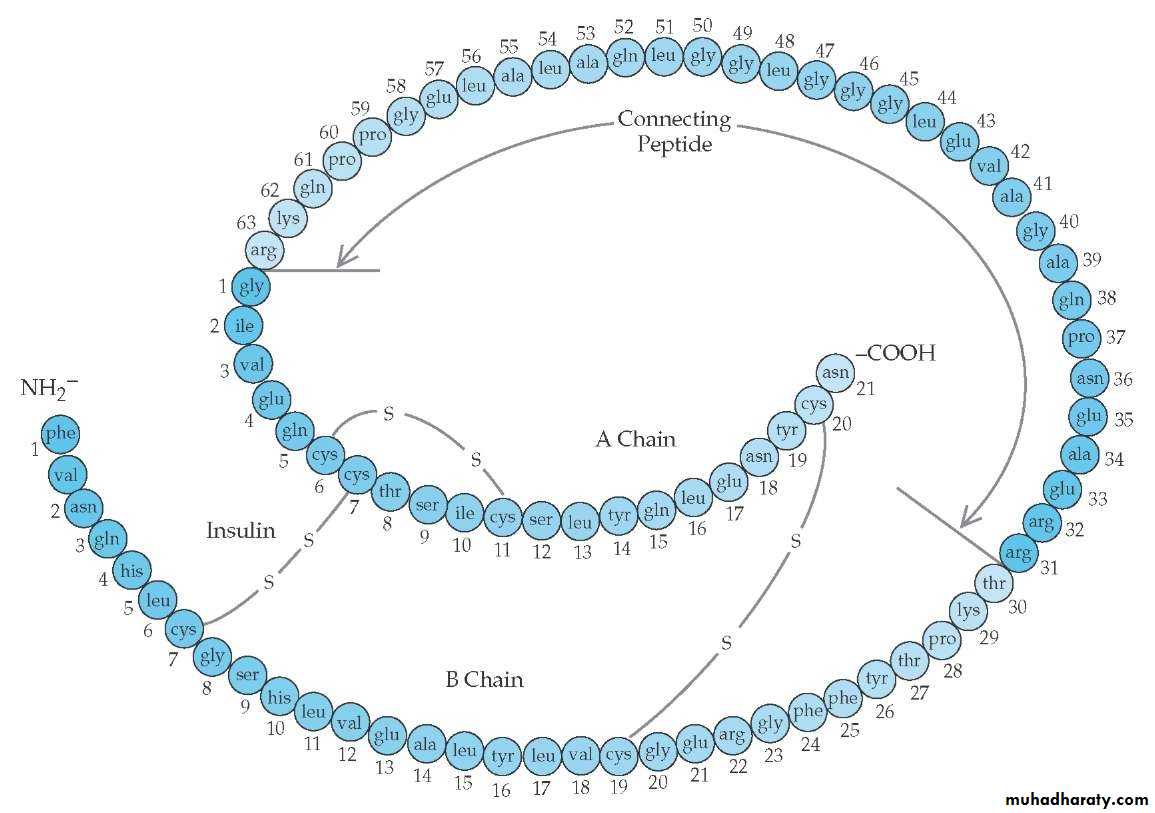
Peptide hormone consist of two straight chains, A chain (21 a.a) and B chain (30 a.a). Two disulfide bridges link the A chain to the B chain, and a third disulfide bridge is located within the A chain.The synthesis of insulin is directed by a gene on chromosome 11. The mRNA directs ribosomal synthesis of preproinsulin, which contains four peptides: a signal peptide, the A and B chains of insulin, and a connecting peptide (C peptide). The signal peptide is cleaved early in the biosynthetic process (while the peptide chains are still being assembled), yielding proinsulin which is then packaged in secretory granules on the Golgi apparatus. During this packaging process, proteases cleave the connecting peptide, yielding insulin.
100
Insulin and the cleaved connecting peptide are packaged together in secretory granules, and when the β cell is stimulated, they are released in equimolar quantities into the blood.
The secretion of the connecting peptide (C peptide) is the basis of the test for β-cell function.
Insulin is metabolized in the liver and kidney by enzymes that break disulfide bonds. The A chains and B chains are released, now inactive, and are excreted in the urine
Structure and Synthesis of Insulin (continue..)
101102
Regulation of Insulin Secretion
Factors Affecting Insulin SecretionStimulatory factors
Inhibitory factors
Increase blood glucose
Decrease blood glucose
Increased amino acids in blood
Fasting
Increased fatty acids and ketoacids
Exercise
Glucagon
Somatostatin
Cortisol
Alpha adrenergic agonists
Glucose-dependent insulinotropic peptide (GIP)
Drugs: Diazoxide
Potassium
Vagal stimulation (Ach)
Obesity
Drugs: sulphonylurea e.g. tolbutamide103
Mechanism of Insulin Secretion by Pancreatic β Cells
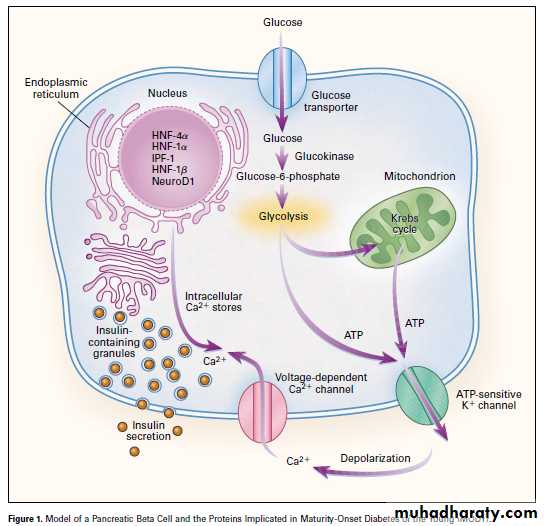
1- The β-cell membrane contains GLUT 2, a specific glucose transporter that moves glucose from the blood into the cell by facilitated diffusion .2- Once inside the cell, glucose is phosphorylated to glucose-6-phosphate by glucokinase , and glucose-6-phosphate is subsequently oxidized . ATP, one of the products of this oxidation step, appears to be the key factor that regulates insulin secretion.
3- ATP closes ATP-sensitive K+ channels. When ATP levels inside the β cell increase, the K+ channels close , which depolarizes the β-cell membrane .
4- Depolarization opens voltage-sensitive Ca2+ channels. Ca2+ channels, also in the β-cell membrane, are regulated by changes in voltage; they are opened by depolarization and closed by hyperpolarization. So, Ca2+ flows into the β cell down its electrochemical gradient and the intracellular Ca2+ concentration increases.
104
5- Increased intracellular Ca2+ causes insulin secretion. Increases in intracellular Ca2+ concentration cause exocytosis of the insulin-containing secretory granules. Insulin is secreted into pancreatic venous blood and then delivered to the systemic circulation.
C peptide is secreted in equimolar amounts with insulin and is excreted unchanged in the urine. Therefore, the excretion rate of C peptide can be used to assess and monitor endogenous β-cell function.
Mechanism of Insulin Secretion by Pancreatic β Cells
105Mechanism of Insulin Secretion by Pancreatic β Cells
106Note : Oral glucose is a more powerful stimulant for insulin secretion than intravenous glucose.
The reason for this difference is that oral glucose stimulates the secretion of glucose-dependent insulinotropic peptide (GIP), a gastrointestinal hormone that has an independent stimulatory effect on insulin secretion (adding to the direct effect of glucose on the β cells). Intravenous glucose does not cause the release of GIP, and thus only acts directly.
107
Mechanism of Action of Insulin
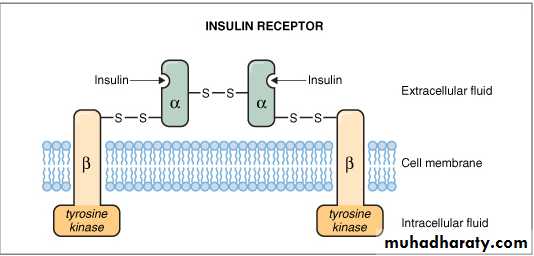
Insulin receptor composed of two α subunits and two β subunits . The α subunits lie in the extracellular domain, and the β subunits span the cell membrane. A disulfide bond connects the two α subunits, and each α subunit is connected to a β subunit by a disulfide bond. The β subunits have tyrosine kinase activity.108
Insulin action on target cells
1- Insulin binds to the α subunits of insulin receptor, producing a conformational change in the receptor. The conformational change activates tyrosine kinase in the β subunit, which phosphorylates itself in the presence of ATP. In other words, the β subunit autophosphorylates.2- Activated tyrosine kinase phosphorylates several other proteins or enzymes that are involved in the physiologic actions of insulin including protein kinases, phosphatases, phospholipases, and G proteins. Phosphorylation either activates or inhibits these proteins to produce the various metabolic actions of insulin.
109
3- The insulin-receptor complex is internalized (i.e., taken in) by its target cell by endocytosis. The insulin receptor is either degraded by intracellular proteases, stored, or recycled to the cell membrane to be used again. Insulin down-regulates its own receptor by decreasing the rate of synthesis and increasing the rate of degradation of the receptor.
Down-regulation of the insulin receptor is in part responsible for the decreased insulin sensitivity of target tissues in obesity and type II diabetes mellitus.
In addition to the previously described actions, insulin also binds to elements in the nucleus, the Golgi apparatus, and the endoplasmic reticulum. Thus, insulin stimulates gene transcription, similar to the actions of somatomedins, IGF-1 and IGF-2.
Insulin action on target cells (continue)
110
The Hormone of Abundance
Insulin is known as the hormone of "abundance" or plenty. When the availability of nutrients exceeds the demands of the body, insulin ensures that excess nutrients are stored as glycogen in the liver, as fat in adipose tissue, and as protein in muscle.These stored nutrients are then available during subsequent periods of fasting to maintain glucose delivery to the brain, muscle, and other organs
111
Actions of Insulin
1- Increase glucose uptake into cells, resulting in lowering blood glucose level (hypoglycemic action).- Stimulates glycogen formation in the liver and muscles (glycogenesis)
- Inhibits glycogenolysis
- Inhibits gluconeogenesis
2- Decreases blood fatty acid and ketoacid concentrations.
- Inhibits mobilization and oxidation of fatty acids (Inhibits lypolysis)
- Increases the storage of fatty acids (stimulates fat deposition)
3- Decreases blood amino acid concentration , (Anabolic action)
- Increases amino acid and protein uptake by target tissue cells.
- Increases protein synthesis, and inhibits protein degradation
4- Promotes K+ uptake into cells by increasing the activity of the Na+-K+ ATPase
5- Insulin also appears to have a direct effect on the hypothalamic satiety center independent of the changes it produces in blood glucose concentration
112
Pathophysiology of Insulin
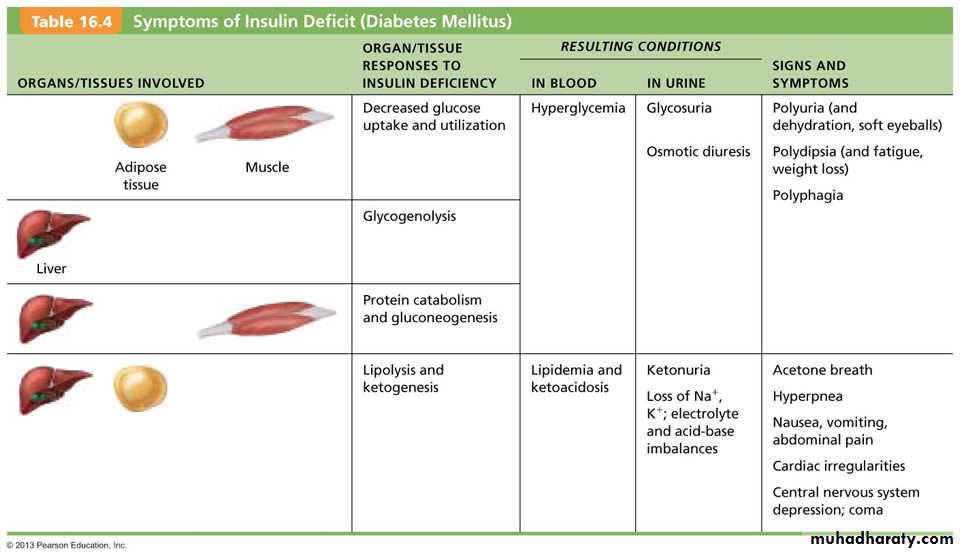
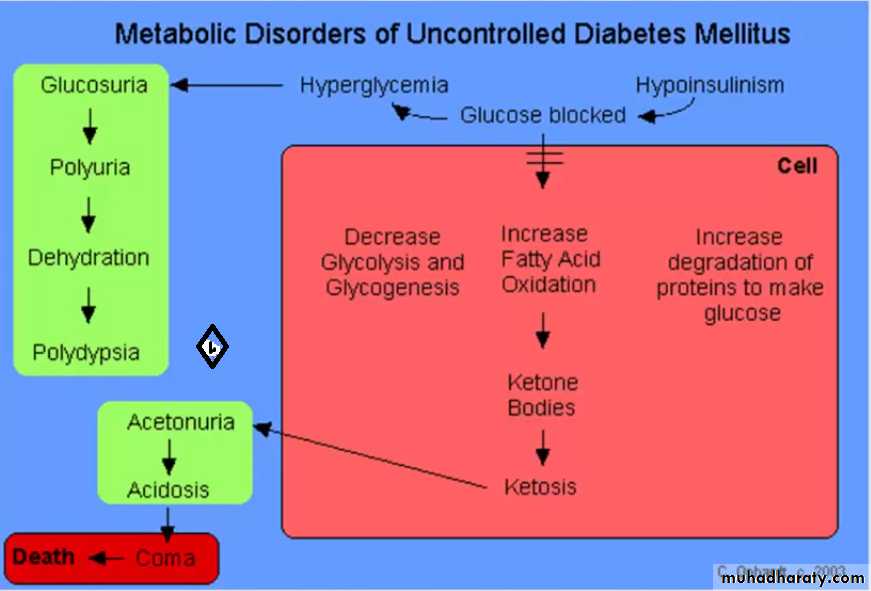
Insulin-dependent diabetes mellitus, or type I diabetes mellitus, is caused by destruction of β cells, often as a result of an autoimmune process. When pancreatic β cells do not secrete adequate amounts of insulin, there are serious metabolic consequences: Carbohydrate, fat, and protein metabolism all will be disturbed.Type I diabetes mellitus is characterized by the following changes:increased blood glucose concentration from decreased uptake of glucose into cells, decreased glucose utilization, and increased gluconeogenesis;
increased blood fatty acid and ketoacid concentration from increased lipolysis of fat, increased conversion of fatty acids to ketoacids, and decreased utilization of ketoacids by tissues;
increased blood amino acid concentration from increased breakdown of protein to amino acids. There also is loss of lean body mass (i.e., a catabolic state) and loss of adipose tissue.
113
Non-insulin-dependent diabetes mellitus, or type II diabetes mellitus
It is often associated with obesity. It exhibits some, but not all, of the metabolic derangements seen in type I diabetes mellitus. Type II diabetes mellitus is caused by down-regulation of insulin receptors in target tissues and insulin resistance. Insulin is secreted normally by the β cells, but at normal concentrations, it cannot activate its receptors on muscle, liver, and adipose tissue; thus, insulin is unable to produce its usual metabolic effects. Typically, the blood glucose concentration is elevated in both fasting and postprandial (after eating) states114
115
116
GLUCAGON
Glucagon is synthesized and secreted by the α cells of the islets of Langerhans. In most respects (i.e., regulation of secretion, actions, and effect on blood levels), glucagon is the "mirror image" of insulin. Thus, while insulin is the hormone of "abundance," glucagon is the hormone of "starvation." In contrast to insulin, which promotes storage of metabolic fuels, glucagon promotes their mobilization and utilization.117
Regulation of Glucagon Secretion
Both glucose and insulin inhibit the synthesis of glucagon.The major factor stimulating the secretion of glucagon is decreased blood glucose concentration,
Glucagon secretion also is stimulated by the ingestion of protein, specifically by the amino acids arginine and alanine. The response of the α cells to amino acids is blunted if glucose is administered simultaneously (partially mediated by the inhibitory effect of insulin on glucagon secretion). Thus, glucose and amino acids have offsetting or opposite effects on glucagon secretion (in contrast to their effects on insulin secretion, which are complementary).
Glucagon secretion is also stimulated by Cholecystokinin (CCK), which is secreted from the gastrointestinal tract when protein or fat is ingested,
Fasting and intense exercise, are stimulatory
Some of the stimulatory effects on glucagon secretion are mediated by activation of sympathetic α-adrenergic receptors
118
Actions of Glucagon
The mechanism of action of glucagon on its target cells begins with hormone binding to a cell membrane receptor, which is coupled to adenylyl cyclase via a Gs protein. The second messenger is cAMP, which activates protein kinases that phosphorylate various enzymes; the phosphorylated enzymes then mediate the physiologic actions of glucagon.A- Increased blood glucose by : 1- stimulating glycogenolysis and inhibiting glycogen formation from glucose, 2- increases gluconeogenesis (formation of glucose from amino acids).
B- Increases blood fatty acid and ketoacid concentration. Glucagon increases lipolysis and inhibits fatty acid synthesis (shunts substrates toward gluconeogenesis).
The ketoacids β-hydroxybutyric acid and acetoacetic acid are produced from fatty acids.
119
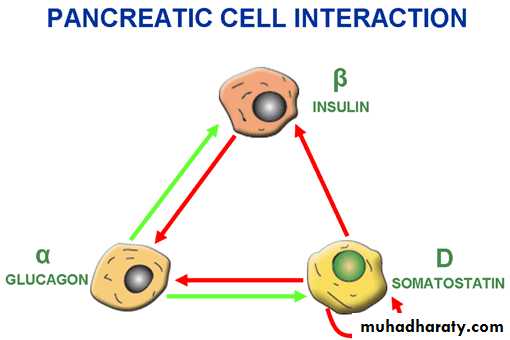
SOMATOSTATIN
Pancreatic somatostatin, a polypeptide with 14 amino acids, is secreted by the δ cells (D cells) of the islets of Langerhans. (The gastrointestinal counterpart of somatostatin has 28 amino acids and shares many of the physiologic actions of the pancreatic hormone.) Secretion of somatostatin is stimulated by the ingestion of all forms of nutrients ( glucose, amino acids, and fatty acids), by several gastrointestinal hormones, by glucagon, and by β-adrenergic agonists. Secretion of somatostatin is inhibited by insulin (via an intraislet paracrine mechanism).Pancreatic somatostatin inhibits secretion of insulin and glucagon via paracrine actions on the α and β cells. Thus, somatostatin is secreted by the δ cells in response to a meal, diffuses to the nearby α and β cells, and inhibits secretion of their respective hormones. Apparently, the function of somatostatin is to modulate or limit the responses of insulin and glucagon to ingestion of food.
120
Paracrine Interactions within Islets of Langerhans
121
122
The Thymus
The thymus producesThymopoietin,
Thymic factor,
Thymosin,
They are essential for the development of T-lymphocytes and the immune response.
123
Other Hormone-Producing Tissues
Adipose tissue: ProducesLeptin, which acts on the CNS to produce a feeling of satiety; secretion is proportional to fat stores.
Adiponectin, which enhances insulin activity,
Resistin, an insulin antagonist. Secretion of resistin is proportional to fat stores; secretion of adiponectin is inversely proportional to fat stores.
Adiponectin levels are low in type II diabetes, suggesting higher levels may help reverse the insulin resistance characteristic of type II diabetes.
The atria of the heart contain specialized cells that secrete atrial natriuretic peptide (or factor, or hormone - ANP or ANF or ANH) resulting in decreased blood volume, blood pressure, and blood sodium concentration.
ANP inhibits aldosterone secretion and antagonizes its activity at the kidney.
124
The gastrointestinal tract contains enteroendocrine cells throughout the mucosa that secrete hormones to regulate digestive functions.
The placenta secretes estrogens, progesterone, and human chorionic gonadotropin, which act on the uterus to influence pregnancy.
The kidneys produce erythropoietin, which signals the bone marrow to produce red blood cells.
Osteoblasts in bone produce osteocalcin, which stimulates pancreatic beta cells to divide and secrete more insulin. It also inhibits fat storage and stimulates adipocytes to produce adiponectin. Insulin promotes conversion of inactive osteocalcin to active osteocalcin.
The skin produces cholecalciferol, an inactive form of vitamin D3.