SYSTEMIC LUPUS ERYTHEMATOSUS
Connective Tissue DiseasesEpidemiology and natural history
It is widely agreed that lupus is approximately 10–20 times more common in women than men.F:M is 9:1There is also little dispute that the overwhelming majority of lupus patients will develop their disease between the ages of 15 and 40.
Although, in the early part of the century, lupus was considered a serious and frequently fatal disease, perceptions of it have changed considerably.
There is now widely available tests for measuring antinuclear antibodies have eased identification of milder cases.
The introduction of corticosteroids and immunosuppressive drugs, dialysis, and renal transplantation has improved the chances of survival in the more serious cases.
However, as will be discussed, lupus continues to cause considerable morbidity and 10–20 per cent of patients succumb from either the disease, a side-effect of its treatment, or both within 15 years of follow-up
SLE
Pathophysiology
SLE-PathophysiologyThe cause of SLE is incompletely understood but genetic factors play an important role.
There is a higher concordance in monozygotic twins and associations with multiple polymorphisms in the HLA locus on chromosome 6 have been identified.
In a few instances, SLE is associated with inherited mutations in complement components C1q, C2, and C4; in the immunoglobulin receptor or in the DNA exonuclease .
Recent studies have identified common polymorphisms that predispose to SLE, including a gene which encodes an integrin; agenes which are involved in interferon signalling; and a gene which is involved in B-cell signalling.
From an immunological standpoint, the characteristic feature of SLE is the production of autoantibodies.
SLE-Pathophysiology
These have specificity for a wide range of targets but many are directed against antigens present within the cell or within the nucleus. This has led to the suggestion that patients with SLE have defects in apoptosis or in the clearance of apoptotic cells, which causes inappropriate exposure of intracellular antigens on the cell surface, leading to polyclonal B- and T-cell activation and autoantibody production.This is supported by the fact that environmental factors that cause flares of lupus, such as ultraviolet (UV) light, pregnancy and infections, increase oxidative stress and/or stimulate apoptosis .
Whatever the underlying cause, immune complex formation is thought to be an important mechanism of tissue damage in active SLE, leading to widespread vasculitis and organ damage.
SLE
Clinical Features
Non-specific featureslymphadenopathy, especially in the axillae, which persists long after patients have gone into remission.
Patients with active lupus may experience weight loss and, on occasion, nausea.
Most of these general features will improve when treatment is commenced.
Musculoskeletal involvement
Arthralgia occurs in about 90 per cent of patients with SLE. The joint pain is polyarticular and frequently symmetrical, .It is accompanied in about half the patients by early morning stiffness. Very often, the patient's symptoms outweigh the objective signs and major synovial effusions are rare.
Furthermore, unlike patients with rheumatoid arthritis, the deformities are usually related to an intense tenosynovitis and less frequently to synovial hypertrophy, with or without bone erosion. These deformities in the hands are known as Jaccoud's arthropathy which is generally a reversible subluxation.
Musculoskeletal involvement
Myalgia, muscle weakness, and tenderness have been reported in upto 60 per cent of lupus patients, although a true myositis is confined to about 5 per cent of these patientsTreatment with corticosteroids and chloroquine may cause a myopathy, but in the main the myalgia experienced by lupus patients seems to be a complication of adjacent joint involvement
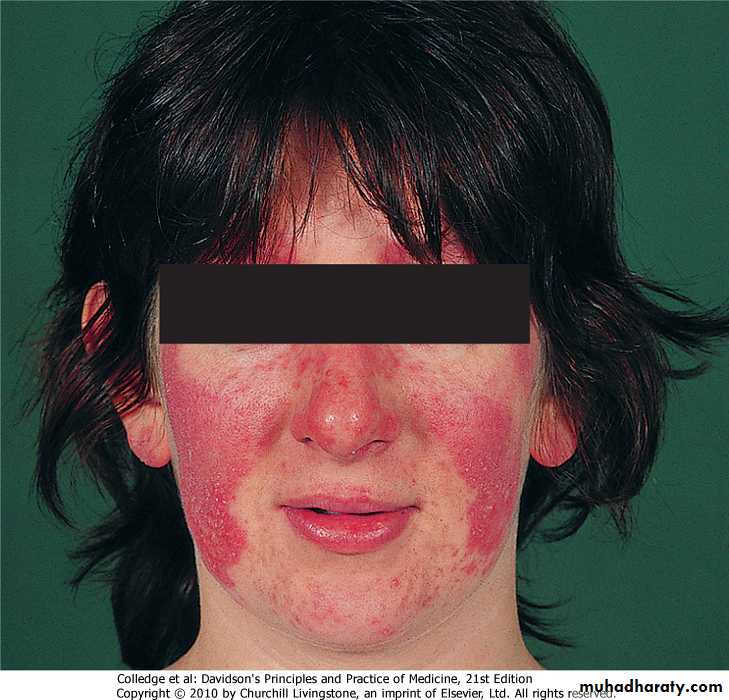
Dermatological involvement
• Common (20–50% approximately)• Butterfly rash
• Chronic discoid lesion• Photosensitivity
• Non-scarring alopecia
Non-specific maculopapular lesions
• Purpura/petechiae
• Less common (5–20% approximately)
• Mucous membrane lesions
• Leg ulcer
• Urticaria
• Subcutaneous nodules
• Diffuse hyperpigmentation
• Occasional (<5%)
• Periorbital oedema
• Bullae
• Jaundice
• Panniculitis
• Severe scarring alopecia
• Psoriaform lesions
• Pruritis
Cardiovascular involvement
Cardiovascular involvement1. Pleuritic pain/pleuritis
2. Pleural effusions .These are usually small volume, straw coloured, white cell count 3–5000/mm 3 mostly mononuclear cells and lymphocytes, glucose levels approximate to those in the blood (unlike RA in which the levels are lower), ANA may be detected, protein content varies from 2.75 to 6.4 g%3. CXR and lung function tests (and autopsy findings!) invariably indicate a greater degree of pulmonary involvement than is evident clinically
4. Interstitial fibrosis, pulmonary vasculitis, and interstitial pneumonitis are found in upto one-fifth of the patients
5. Pulmonary hypertension is unusual and has been linked to the presence of antiphospholipid antibodies
Major pulmonary manifestations in lupus
Renal involvement-WHO classification of SLE glomerulonephritis
Renal involvement-WHO classification of SLE glomerulonephritis
Neuropsychiatric syndromes observed in SLE
Haematopoietic involvementnormochromic, normocytic anaemia, the 'anaemia of chronic disease', is present in upto 70 per cent of lupus patients
Coombs' positive haemolytic anaemia. Much less frequently, a microangiopathic haemolytic anaemia with disseminated intravascular coagulation has been described.
Leucopaenia (<4 × 10 9 /l) and lymphopaenia (<1.5 × 10 9 /l) are the most frequent abnormalities of the white blood cell count in lupus patients.
leukocytosis is rare in lupus in the absence of infection or major corticosteroid therapy.
Gastrointestinal disease
Gastrointestinal diseases include mouth ulcers, dysphagia, anorexia, nausea, vomiting, haemorrhage, and abdominal painHepatomegaly, which can be detected in upto one-fourth of patients with lupus, is usually a minor degree of enlargement only and rarely accompanied by major abnormalities in liver function tests. Splenomegaly is found in approximately 10 per cent of the patients, though again the spleen is rarely greatly enlarged
Revised American Rheumatism Association criteria for systemic lupus erythematosus
FeaturesCharacteristics
Malar rash
Fixed erythema, flat or raised, sparing the nasolabial folds
Discoid rash
Erythematous raised patches with adherent keratotic scarring and follicular plugging
Photosensitivity
Rash due to unusual reaction to sunlight
Oral ulcers
Oral or nasopharyngeal ulceration, which may be painless
Arthritis
Non-erosive, involving two or more peripheral joints
Serositis
Pleuritis (history of pleuritic pain or rub, or pleural effusion) or pericarditis (rub, ECG evidence or effusion)
Revised American Rheumatism Association criteria for systemic lupus erythematosus
Features
Characteristics
Renal disorder
Persistent proteinuria > 0.5 g/day or cellular casts (red cell, granular or tubular)
Neurological disorder
Seizures or psychosis, in the absence of provoking drugs or metabolic derangement
Haematological disorder
Haemolytic anaemia or leucopenia2 (< 4 × 109/L), or lymphopenia2 (< 1 × 109/L), or thrombocytopenia2 (< 100 × 109/L) in the absence of offending drugs
Immunological disorder
Anti-DNA antibodies in abnormal titre or presence of antibody to Sm antigen or positive antiphospholipid antibodies
Antinuclear antibody (ANA) disorder
Abnormal titre of ANA by immunofluorescence