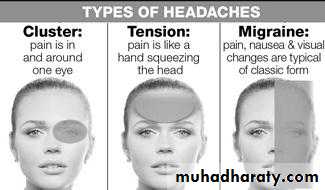
Revision from the previous lecture (Primary headache)
Note: The below revision were added by the students (its not included in lecture):Case: A 34-year-old Mexican male comes to the emergency department and complains of severe episodic headache, especially at night, for the past month. He also complains of unilateral, sharp, stabbing pain in the eye, which wakes him from sleep. The pain often starts suddenly just behind the right eye, and spreads to his face and temple region. It is not associated with nausea or visual disturbances, but is associated with watering of the eyes and nose, and with red eye. He had a similar episode one year ago, and it lasted for 2 months. Which of the following is the best treatment regimen for aborting the patient's pain during an acute attack?
Oral NSAIDs
Verapamil
Nasal sumatriptan
100% oxygen
Ergotamine
Explanation: The clinical presentation of this patient is classic for cluster headache. This is the only headache syndrome that is more common in men than in women. The pathophysiology is related to alterations in the circadian pacemaker, which may be due to hypothalamic dysfunction. Repetitive episodes of headache typically occur for weeks to months, followed by a period of remission. The attacks often occur at the same time of the day, and frequently awaken the patient from sleep. The headache is always unilateral, sudden in onset, severe, deep, excruciating, and continuous or explosive in quality. It generally starts as retro-orbital pain and later spreads to the hemicranium. It is not associated with nausea or vomiting, but is frequently associated with ipsilateral lacrimation, rhinorrhea, red eye, stuffy nose, pallor or even Horner's syndrome. Both abortive and prophylactic regimens are needed for an episode of cluster headache. Of all the regimens available, 100% oxygen is the most rapid-acting and effective in aborting the pain during an acute attack.
So the answer is D
23-year-old female presents with a headache that began acutely eight hours ago. She describes her headache as severe, unilateral, pulsating in quality, and associated with nausea and photophobia. She has vomited five times since its onset. She has had two other such episodes over the last two months, but this is the firsttime she has sought medical attention. Her neurological examination reveals normal muscle strength and no sensory loss. She has no fever or meningeal signs. Which of the following is the most appropriate initial management step?
Amitriptyline
Diazepam
Prochlorperazine
Propranolol
Sertraline
Explanation: This patient is most likely suffering from a migraine headache. Migraines are generally unilateral and have a pulsating quality. Attacks can last from 4 to 72 hours. Photophobia is commonly associated. Migraines are more common in younger female patients. In some cases there is an aura of neurologic symptoms that precedes the onset of the headache. In cases where the diagnosis is straightforward and there are no concerning features such as fever, meningeal signs, or focal neurologic symptoms, further work-up is generally not required.
Of the options given, the best initial treatment for this patient would be prochlorperazine. Intravenous antiemetics (chlorpromazine, prochlorperazine or metoclopramide) can be used as monotherapy or as adjuvant therapy in combination with NSAIDs or triptans for the treatment of acute migraine headaches. Prochlorperazine is an effective acute treatment for migraine and can be given in intravenous form, which is often necessary given these patients' tendency towards vomiting. Triptan medications are an effective migraine treatment, but must be started early on in the course of the migraine before symptoms become severe in order to be of benefit.
So the answer is C
Secondary headache from the previous lecture:
Meningitis
Intracranial Hemorrhage
Brain Tumor
Temporal arteritis
Idiopathic intracranial hypertention
4&5 will be discussed in this lecture
The new lecture
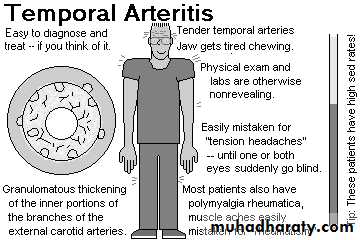
Secondary headache1-Temporal Arteritis
This disorder, also known as giant cell arteritis, is characterized by a subacute granulomatous inflammation (consisting of lymphocytes, neutrophils, and giant cells) that affects the external carotid arterial system, particularly the superficial temporal artery and the vertebral artery. Inflammation of the pain-sensitive arterial wall produces the headache. Thrombosis may occur in the most severely affected arteries.This syndrome, which affects women twice as frequently as men, it is uncommon before the age 50 and is frequently associated with malaise, myalgia, weight loss, arthralgia, and fever (the polymyalgia rheumatica complex).
The headache can be unilateral or bilateral, fairly severe, and boring in quality. It is characteristically localized to the scalp, especially over the temporal arteries. Scalp tenderness may be especially apparent when lying with the head on a pillow or brushing the hair. Pain or stiffness in the jaw during chewing (jaw claudication) is highly suggestive of giant cell arteritis and is due to arterial ischemia in the muscles of mastication, Involvement of the ophthalmic artery leads to permanent blindness in 50% of untreated patients; in half of these, blindness will become bilateral. The visual loss is most often sudden in onset.
Diagnosis
The diagnosis is made by biopsy of affected temporal arteries, which are characteristically thickened and nonpulsatile as well as dilated and tender. The temporal arteries may be affected in a patchy manner, and serial sections may be necessary to demonstrate histologic vasculitis. The erythrocyte sedimentation rate (ESR) is almost invariably elevated. Consideration of this diagnosis demands prompt evaluation to avoid visual loss. Initial therapy is with prednisone, 40-60 mg/d orally. The dose is decreased, usually after 1-2 months, depending upon the clinical response. The sedimentation rate returns rapidly toward normal with prednisone therapy and must be maintained within normal limits as the drug dose is tapered.
Treatment
Therapy should not be withheld pending biopsy diagnosis and should be continued despite negative biopsy findings if the diagnosis can be made with confidence on clinical grounds. Tapering of prednisone therapy requires 1-2 years. Although dramatic improvement in headache occurs within 2-3 days after institution of therapy, the blindness is usually irreversible.
Note: the picture above were added by the students (its not included in the lecture)
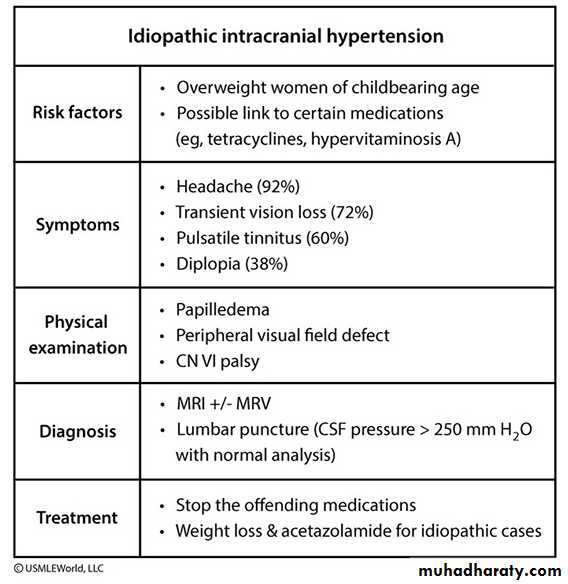
2- Idiopathic Intracranial Hypertension (pseudotumor cerebri)
Idiopathic intracranial hypertension is characterized by a diffuse increase in intracranial pressure causing headache, papilledema, visual loss, and diplopia (as a result of abducent nerve palsy). Although intracranial hypertension can accompany many disorders ,most cases are idiopathic. In the idiopathic variety, women are affected much more commonly than men, with a peak incidence in the third decade. Most patients are obese.Diffuse headache is almost always a presenting symptom ,moderate to severe papilledema is seen in almost all. Visual loss from increased intracranial pressure may occure.
Disorder associated with IIH
Endocrine dysfunction (e.g., obesity, withdrawal from steroid therapy, amenorrhea, oligomenoriha )
Vitamin and drug therapy (e.g., hypervitaminosis A and 13 cis-retinoic acid; tetracycline, minocycline, nalidixic acid,steroid and contraceptive drugs)
Pathophysiology
Supuse to be due to decrease absorption of CSF.
Diagnosis
The diagnosis depends the following
1-headache and papillodema
2-No localizing symptoms or signs other than a 6th nerve palsy.
3-Normal neuroimaging ( Brain CT Scan)
4-Lumbar puncture showing elevated opening pressure (>250 mm/H2O) but normal CSF fluid analysis.
Tratment
removal of 20-40 mL CSF may transiently relieve headacheCarbonic anhydrase inhibitor (acetazolamide 1-2 g/d)
furosemide 40-60 mg twice daily
lumboperitoneal or ventriculoperitoneal shunting may be needed to protect vision and decrease headache
Note: the table below were added by the students (its not included in the lecture)
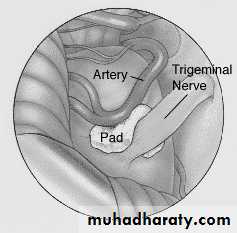
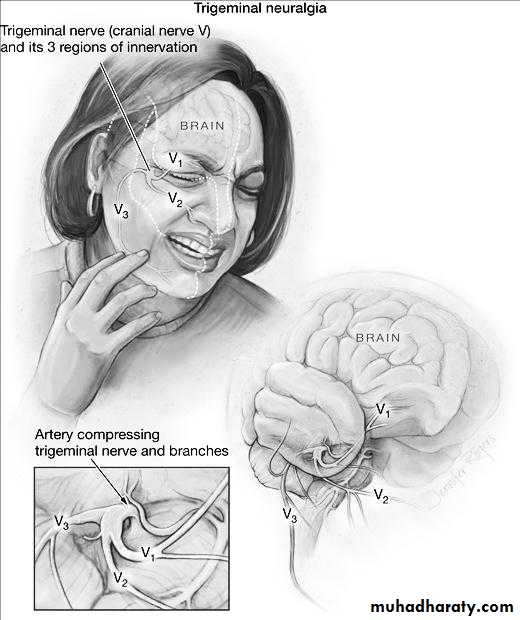
3- TRIGEMINAL NEURALGIA (Tic Douloureux)
Trigeminal neuralgia is characterized by excruciating paroxysms of pain in second and third division of trigeminal nerve (the lips, gums, cheek, or chin) and, very rarely, in the distribution of the ophthalmic division of the fifth nerve. The pain seldom lasts more than a few seconds or a minute or two but may be so intense that the patient winces, hence the term tic. The paroxysms, experienced as single jabs or clusters, tend to recur frequently, both day and night, for several weeks at a time ,they may occur spontaneously or with movements of affected areas.An essential feature of trigeminal neuralgia is that objective signs of sensory loss cannot be demonstrated on examination. Trigeminal neuralgia is relatively common. Middle-aged and elderly persons are affected primarily, and 60% of cases occur in women. Rarely, similar pain may occur in multiple sclerosis or brainstem tumors, and these possibilities should thus be considered in young patients and in all patients who show neurologic abnormalities on examination which indicated for brain MRI.
Pathophysiology
Demylination or Compression of the trigeminal nerve root by a blood vessel, most often the superior cerebellar artery or on occasion a tortuous vein, is the source of trigeminal neuralgia in a substantial proportion of patients.
Treatment
Antiepileptic drugsCarbamazepine and oxycarbamazepin has been the first line drug for TN and it is effective or partially effective in 70% of cases
phenytoin, 200-400 mg/d orally, may be effective alone or in combination with carbamazepine if a second drug is necessary.
2- Surgery
Posterior fossa microvascular decompressive surgery has been used in drug-resistant cases
Gasserian ganglion ablative techniques These techniques involve selective ablation of part of the trigeminal ganglion
Gamma knife radio-surgery High doses of focused irradiation are directed at the root of the trigeminal n. exit zone or the nerve itself.
Note: the picture above were added by the students (its not included in the lecture)
The following are indications for imaging in headache:signs and symptoms of elevated intracranial pressure (eg, papilledema)
Meningismus
partial seizure
nocturnal headaches that awaken the patient from sleep
increase in pain with coughing, sneezing or change in body position
sudden onset headaches that reach maximum intensity in 2 to 3 minutes
headache associated with mental status changes or decreased alertness
any new headache in an HIV-positive patient
Thunderclap headache
Sudden onset severe headache ‘‘the worst headache of my life” reaching maximum intensity in less than 1 minute.causes include:
Subarachnoid or Intracerebral hemorrhages
Cervico-cephalic arterial dissection eg. Vertebral or caroted
Cerebral venous thrombosis
Acute hypertension
Acute low CSF pressure
End
Note: the case below were added by the students (its not included in the lecture)
A 27 -year-old white female comes to the office and complains of a headache for the last two weeks. She characterizes the headache as intermittent, "feels like a dull ache", 5/10 in severity, and associated with nausea and vomiting. She is afebrile and never had such a headache before. She has no visual complaints. She is a non-smoker and drinks alcohol only on weekends. Her only drugs are oral contraceptive pills (OCPs). Her menses are regular, and she has never conceived. She has no family history of similar problem. Her pulse is 80/min, temperature is 37.1C, blood pressure is 120/75mmHg and respirations are 15/min. She is 5 feet 10 inches tall, and her weight is 210 lbs. The neurological examination is non-focal, and there are no signs of meningeal irritation. Funduscopy reveals papilledema. MRI of the brain is normal. Which of the following complications is likely to develop if this patient is left untreated?Seizures
Blindness
Intracranial bleed
Paralysis
Urinary incontinence
Explanation: Suspect benign intracranial hypertension (pseudotumor cerebri) in a young obese female with a headache that is suggestive of a brain tumor, but with normal neuroimaging and elevated CSF pressure. Neurologic signs are usually absent, except for papilledema, visual field defects and sometimes sixth (VI) nerve palsy. There may be a history of exposure to provoking agents such as glucocorticoids or vitamin A. Oral contraceptive pills have also been associated with this disorder. The pathology involves impaired absorption of CSF by the arachnoid villi. The treatment includes weight reduction and acetazolamide (if weight reduction fails). When medical measures fail or visual field defects are progressive, shunting or optic nerve sheath fenestration is done to prevent blindness, which is the most significant complication of this otherwise benign disorder.
So the answer is B