Pulpal diseases and related periapical pathosis
PULPAL DISEASESEtiology
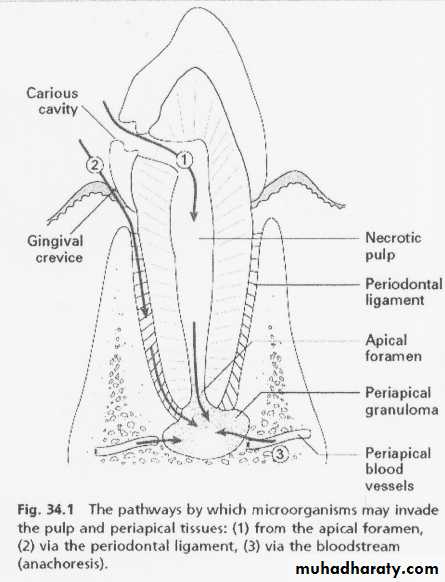
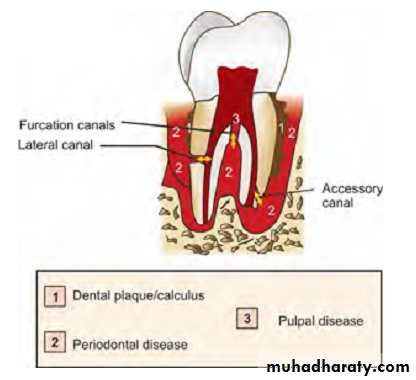
1. Bacteria and bacterial irritants: bacteria are a main cause of pulpal inflammation. Bacteria or their products may enter pulp through a break in dentin either from:
Caries
Accidental exposure
Fracture
Percolation around a restoration
Extension of infection from gingival sulcus
Periodontal pocket and abscess
Anachoresis (Process by which microorganisms get carried by the bloodstream from another source localize on inflamed tissue).
2. Traumatic
a) Acute trauma like fracture, luxation or avulsion of tooth.b) Chronic trauma including para-functional habits like bruxism.
3. Iatrogenic (Pulp inflammation for which the dentists own procedures are responsible is designated as Dentistogenic pulpitis). Various iatrogenic causes of
pulpal damage can be:
a. Thermal changes generated by cutting procedures, during restorative procedures, bleaching of enamel, electrosurgical procedures, laser beam, etc. can cause severe damage to the pulp if not controlled.
b. Orthodontic movement
c. Periodontal curettage
d. Periapical curettage
e. chemicals: A use of chemicals like temporary and permanent fillings, liners and bases and use of cavity desiccants such as alcohol.
4. Idiopathic
a. Agingb. Resorption: internal or external
5. Radiation therapy: Radiation therapy affect pulps of fully formed teeth in patients exposed to radiation therapy. The pulp cells exposed to ionizing radiation may become necrotic, there may occur vascular damage and the interference in mitosis of cells.
Progression of pulpal pathologies
Pulp reacts to above mentioned irritants as do other connective tissues. Degree of inflammation is proportional to intensity and severity of tissue damage. For example, slight irritation like incipient caries or shallow tooth preparation cause little or no pulpal inflammation, whereas extensive operative procedures may lead to severe pulpal inflammation. Depending on condition of pulp, severity and duration of irritant, host response, pulp may respond from mild inflammation to pulp necrosis. These changes may not be accompanied by pain and thus may proceed unnoticed.Pulpal reaction to microbial irritation
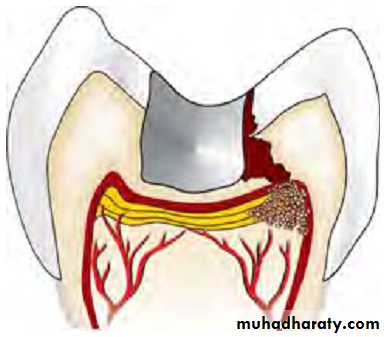
Carious enamel and dentin contains numerous bacteria↓
Bacteria penetrate in deeper layers of carious dentin
↓
Pulp is affected before actual invasion of bacteria via their
toxic byproducts
↓
Byproducts cause local chronic cell infiltration
↓
When actual pulp exposure occurs pulp tissue gets locally infiltrated by PMNs to form an area of liquefaction necrosis at the site of exposure
↓
Eventually necrosis spreads all across the pulp and periapical tissue resulting in severe inflammatory lesion.
Diagnostic aids for pulpal pathology
• Subjective symptoms—most common being pain• Objective symptoms
1. Visual and tactile inspection — 3Cs rule–
i. Color
ii. Contour
iii. Consistency
2. Thermal tests
i. Heat tests— isolation of tooth — use of:
– Warm air
– Hot water
– Hot burnisher
– Hot gutta-percha stick
ii. Cold tests:
– Ethyl chloride spray
– Ice pencils
– CO2 snow — temperature 18ºC
3. Electrical pulp testing
4. Radiographs
5. Anesthetic tests
6. Bite test
7. Cavity test
Recent advances in diagnostic aids for pulpal pathology
include:
Laser Doppler flowmetry
Pulp oximetry
Pulp conditions
Normal when there is a response to the stimulus provided by the sensibility test and this response is not pronunced or exaggerated,and it does not linger
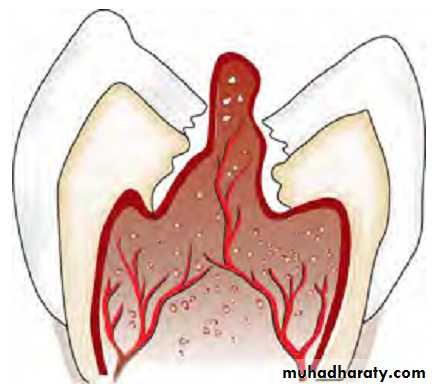
Pulpitis is present when there is an exaggerated response that produse pain. Pulpitis can be considered as reversible or irreversible, depending on the severity of pain and whether the pain lingers or not.
Pulp necrosis: the pulp tissuues are dead
Reversible pulpitis/hyperemia/hyperactive pulpalgia
Definition: Pulpal inflammation, the tissue is capable of returning to a normal state of health.Etiology: Pulpal irritation to external stimuli is related to dentin permeability. Under normal circumstances, enamel and cementum act as impermeable barrier to block the patency of dentinal tubules at dentinoenamel junction or dentinocemental junction.
When caries and operative procedures interrupt this natural barrier, dentinal tubules become permeable. So inflammation can be caused by any agent which is capable of injuring pulp.
It can be:
• Trauma
– Accident or occlusal trauma
• Thermal injury
– While doing tooth preparation
– Overheating during polishing of a restoration
• Chemical stimulus—Like sweet or sour foodstuff
• Following insertion of a deep restoration
Symptoms: Symptomatic reversible pulpitis is characterized by sharp pain lasting for a moment, commonly caused by cold stimuli. Pain does not occur spontaneously and does not continue when irritant is removed. Asymptomatic reversible pulpitis may result from incipient caries and is resolved on removal of caries and proper restoration of tooth.
Diagnosis
1. Pain: It is sharp but of brief duration, ceasing when irritant is removed.
2. Visual examination and history: It may reveal caries, traumatic occlusion and undetected fracture.
3. Radiographs: These show normal PDL and lamina dura.– Depth of caries or restoration may be evident.
4. Percussion test: It shows negative responses, i.e. tooth is not tender to percussion.
5. Vitality test: Pulp responds readily to cold stimuli. Electric pulp tester requires less current to cause pain.
Treatment
• No endodontic treatment is needed for this condition. The best treatment of reversible pulpitis is prevention.• Usually, a sedative dressing is placed, followed by permanent restoration when symptoms completely subside.
• Periodic care to prevent caries, desensitization of hypersensitive teeth and use of cavity varnish or base before insertion of restoration is recommended.
• If pain persists inspite of proper treatment, pulpal inflammation should be considered as irreversible and it should be treated by pulp extirpation.
Irreversible pulpitis
DefinitionIt is a persistent inflammatory condition of the pulp, symptomatic or asymptomatic, caused by a noxious stimulus. It has both acute and chronic stages in pulp.
Etiology
• Most common cause of pulpitis is bacterial involvement of pulp through caries
• Chemical, thermal, mechanical, traumatic injuries of pulp may induce pulp inflammation
• Reversible pulpitis when left untreated deteriorates into irreversible pulpitis.
Symptoms
• A rapid onset of pain, which can be caused by sudden temperature change, sweet or acidic food. Pain remains even after removal of stimulus
• Pain can be spontaneous in nature which is sharp, piercing, intermittent or continuous in nature
• Pain exacerbated on bending down or lying down due to change in intrapulpal pressure
• Presence of referred pain
• In later stages, pain is severe, boring, throbbing in nature which increases with hot stimulus. Pain is so severe that it keeps the patient awake in night. The relief of pain can be simply done by use of cold water. The patient may report dental office with jar of ice water.
Diagnosis
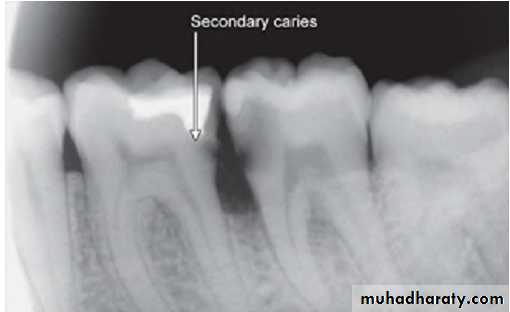
Visual examination and history: Examination of involved tooth may reveal previous symptoms. On inspection, one may see deep cavity involving pulp or secondary caries under restorations.
2. Radiographic findings:
– May show depth and extent of caries.– Periapical area shows normal appearance but a slight widening may be evident in advanced stages of pulpitis.
3. Percussion: Tooth is tender on percussion (due to increased intrapulpal pressure as a result of exudative inflammatory tissue).
4. Vitality tests:
i. Thermal test: Hyperalgesic pulp responds more readily to cold stimulation than for normal tooth, pain may persist even after removal of irritant.
As the pulpal inflammation progresses, heat intensifies the response because it has expansible effect on blood vessels. Cold tends to relieve pain because of its contractile effect on vessels, reducing the intrapulpal pressure.
ii. Electric test: Less current is required in initial stages. As tissue becomes more necrotic, more current is required.
Treatment
Pulpectomy (root canal treatment).
A clinical guide to determine the status of dental pulp in irreversible pulpitis:
A history of spontaneous bouts of pain which may last from a few seconds to several hours
Hot and cold fluids exacerbating the pain. In the latter stages, heat will be more significant and cold will relieve the pain
Pain radiating initially but once the periodontal ligament has become involved; the pain will be more localized by the patient
The tooth may become tender to percussion once the inflammation spreads to the periodontal ligament
A radiographically visible widening of the periodontal ligament may be seen.
Chronic pulpitis
It is an inflammatory response of pulpal connective tissue to an irritant. Here pain is absent because of diminished exudative inflammatory activity and corresponding decrease in intrapulpal pressure to a point below threshold limits of pain receptors. It can be of three types:a. Ulcerative/open form
b. Hyperplastic form
c. Closed form.
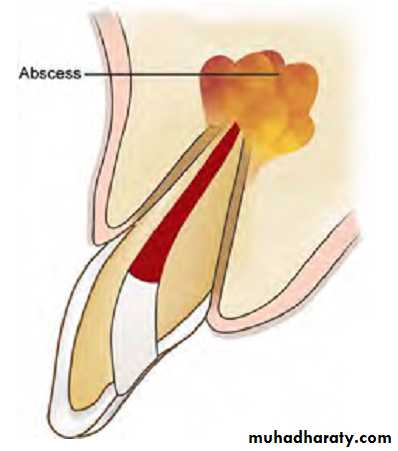
a. Ulcerative form is a chronic inflammation of cariously exposed pulp characterized by formation of an abscess at point of exposure (Fig. 3.20). Abscess is surrounded by granulomatous tissue. This condition is also known as pulpal granuloma.
b. Hyperplastic form is overgrowth of granulomatous tissue into carious cavity.
c. Closed form of chronic pulpitis may occur from operative procedures, excessive orthodontic forces, trauma or periodontal lesions. Here carious lesion is absent.
Etiology
Etiology is same as that of irreversible pulpitis. It is normally caused by slow and progressive carious exposure of pulp.Signs and Symptoms
• Pain is absent.• Symptoms develop only when there is interference with drainage of exudate
• Hyperplastic form of chronic pulpitis is seen in teeth of children and adolescents in which pulp tissue has high resistance and large carious lesion permit free proliferation of hyperplastic tissue. Since it contains few nerve fibers, it is non-painful but bleeds easily due to rich network of blood vessels.
Diagnosis
• Pain:It is usually absent.• Hyperplastic form shows a fleshy, reddish pulpal mass which fills most of pulp chamber or cavity. It is less sensitive than normal pulp but bleeds easily when probed.
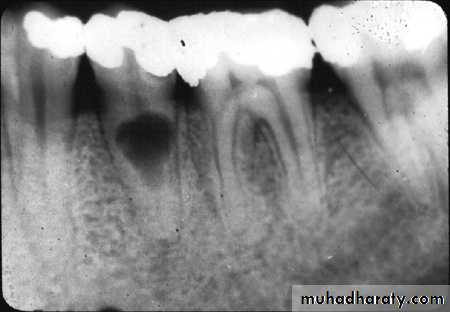
• Radiographic changes show:
– Chronic apical periodontitis in longstanding cases.
– In young patients, low grade longstanding irritation stimulates periapical bone deposition, i.e. condensing osteitis. Radiograph shows areas of dense bone around apices of involved teeth.
• Vitality Tests
– Tooth may respond feebly or not at all to thermal test, unless one uses extreme cold– More current than normal is required to elicit response by electric pulp tester.
Treatment
• Complete removal of pulp followed by its restoration should be the goal of treatment. In case of hyperplastic pulpitis, removal of polypoid tissue with periodontal curette or spoon excavator followed by extirpation of pulp should be done
• If tooth is in non-restorable stage, it should be extracted.
Pulp necrosis
Pulp necrosis or death is a condition following untreated pulpitis. The pulpal tissue becomes dead and if the condition is not treated, noxious materials will leak from pulp space forming the lesion of endodontic origin. Necrosis may be partial or total, depending on extent of pulp tissue involvement.
Etiology
Necrosis is caused by noxious insult and injuries to pulp by bacteria, trauma, and chemical irritation.
Symptoms
• Discoloration of tooth—First indication of pulp death
• History from patient
• Tooth might be asymptomatic.Diagnosis
1. Pain: It is absent in complete necrosis.
2. History of patient reveals past trauma or past history of severe pain which may last for some time followed by complete and sudden cessation of pain.
3. Radiographic changes:Radiograph shows a large cavity or restoration
4. Vitality test: Tooth is nonresponding to vitality tests. But multirooted teeth may show mixed response because only one canal may have necrotic tissue.
5. Visual examination:Tooth shows color change like dull or opaque appearance due to lack of normal translucency
Treatment
Complete removal of pulp(R.C.T) followed by restoration or extraction of nonrestorable tooth.
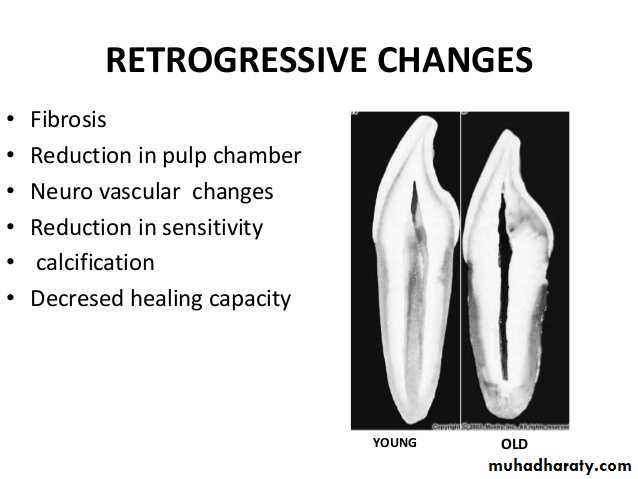
Pulp degeneration
It is generally present in older people. It may be the result of persistent mild irritation in the teeth of younger people. Usually pulp degeneration is induced by attrition, abrasion, erosion, bacteria, operative procedures, caries, pulp capping and reversible pulpitis.
It may occur in following forms:
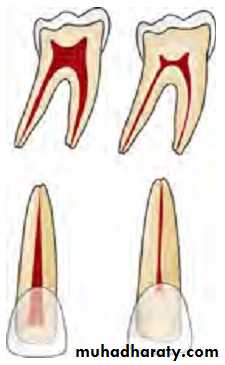
1. Atrophic degeneration and fibrosis
It is a decrease in size of pulp space which occurs slowly as tooth grows old
2. Calcifications
In calcific degeneration, part of the pulp tissue is replaced by calcific material. Mainly three types of calcifications are seen in pulp:Dystrophic calcification: occur by deposition of calcium salts in dead or degenerated tissue. The local alkalinity of destroyed tissues attracts the salts.
Diffuse calcification: They are generally observed in root canals. The deposits become long, thin and fibrillar on fusing.
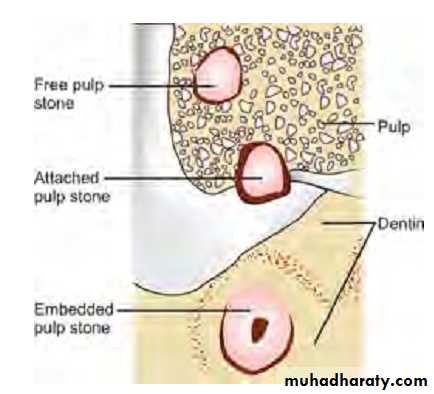
Denticles/pulp stones. These are usually seen in pulp chamber.
Classification
According to location:•Free
• Embedded
• Attached
According to structure:
•True• False
True denticles: It is composed of dentin formed from detached odontoblasts or fragments of Hertwig’s enamel root sheath which stimulate and undifferentiated cells to assume dentinoblastic activity.
False denticles: Here degenerated tissue structures act as nidus for deposition of concentric layers of calcified tissues.
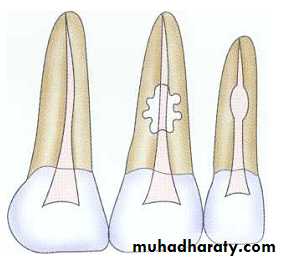
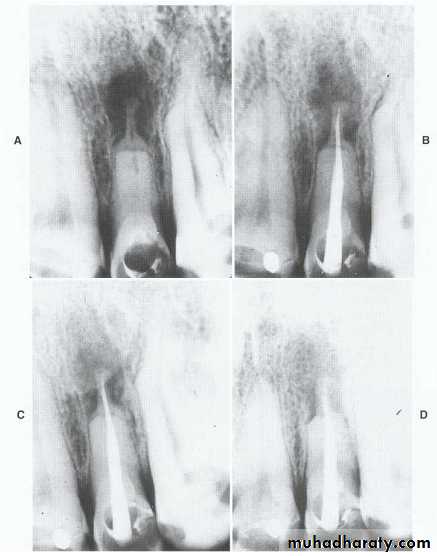
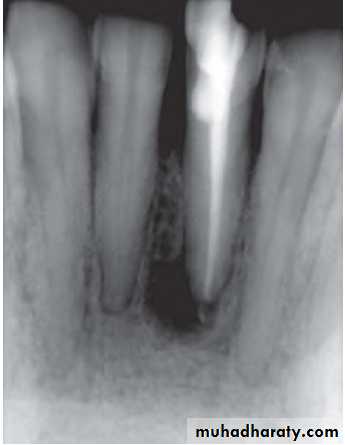
Internal root resorption
Internal resorption is initiated within the pulp cavity and results in loss of substance from dentinal tissue.Etiology
Exact etiology is unknown. Patient often presents with history of trauma, persistent chronic pulpitis, history of pulpotomy, crown preparation, force from orthodontic treatment, impacted teeth,…etc.
Symptoms
• Usually asymptomatic, recognized clinically through routine radiograph (especially in the root)• Pain occurs in cases of perforation of crown.
• “Pink Tooth” is the pathognomic feature of internal root resorption (especially in the crown).
Diagnosis
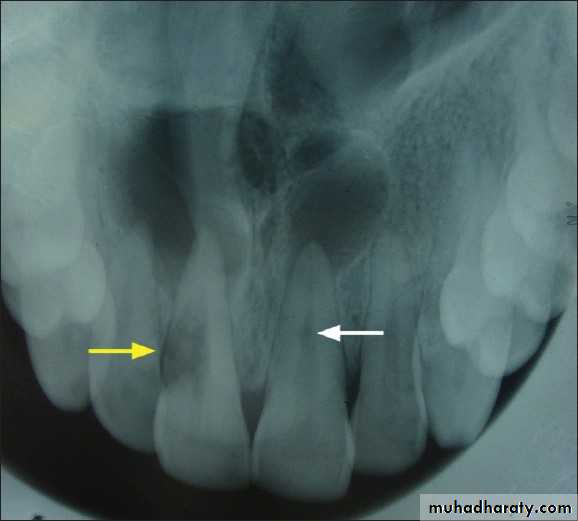
• Clinically:“Pink Tooth” appearance• Radiographic changes:
– Radiolucent enlargement of pulp canal
– Original root canal outline distorted
– Bone changes are seen only when root perforation into periodontal ligament takes place.
• Pulp tests: Positive, though coronal portion of pulp is necrotic, apical pulp could be vital
Treatment
• Pulp extirpation stops internal root resorption.
• Surgically treatment is indicated if conventional treatment fails.
External root resorption
In external root resorption, root resorption affects the cementum or dentin of the root of tooth. It can be:
• Apical root resorption
• Lateral root resorption
• Cervical root resorption.
Etiology:
The same as internal root resorption but here it is mostly associated with trauma to the teeth that injure the cementum. Other factors include:• Infected necrotic pulp
• Over instrumentation during root canal treatment
• Trauma
• Granuloma/cyst applying excessive pressure on tooth root
• Replantation of teeth
• Adjacent impacted tooth.
Bleaching.
Symptoms
• Asymptomatic during development
• When root is completely resorbed, tooth becomes mobile
• When external root resorption extends to crown, it gives “Pink tooth” appearance
• When replacement resorption/ankylosis occur, tooth becomes immobile with characteristic high percussion sound
Radiographic Features
• Radiolucency at root and adjacent bone• Irregular shortening or thinning of root
• Loss of Lamina dura.
Treatment
• Remove stimulus of underlying inflammation.• Nonsurgical endodontic treatment should be attempted before surgical treatment is initiated.
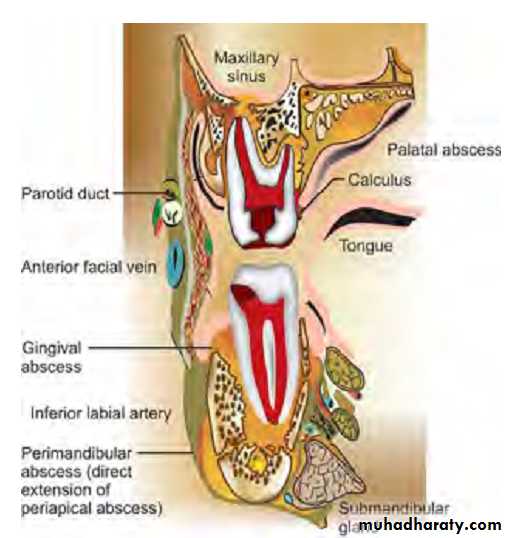
PERIAPICAL DISEASES
Etiology
Bacterial
- Untreated pulpal infection leads to total pulp necrosis. If left untreated, irritants leak into periapical region forming periapex pathologies. Severity of periapical inflammation is related to microorganisms in root canals and the length of exposure to infecting microorganisms.
- Anachoresis also accounts for microbial infection in teeth.
- Microorganisms may invade pulp from periodontal pocket and accessory canals
Trauma
• Physical trauma to tooth, or operative procedures which results in dental desiccation or significant heat transfer causes sufficient damage to pulp and its blood supply.• Persistent periapical tissue compression from traumatic occlusion leads to apical inflammatory response.
Factors Related to Root Canal Procedures
Several complications can arise from improper endodontic technique which can cause periapical diseases:1. It is impossible to extirpate pulp without initiating an inflammatory response because a wound is created.
2. Using strong or excessive amounts of intracanal medicaments between appointments may induce periapical inflammation.
3. Improper manipulation of instruments within root canal or over instrumentation can force dentinal debris, irrigating solution and toxic components of necrotic tissue in the periapex.
4. Overextended endodontic filling material may induce periapical inflammation by directly inducing foreign body reaction
Periapical lesions may include:
Acute apical periodontitis (AAP)Acute apical periodontitis is defined as painful inflammation of the periodontium as a result of trauma, irritation or infection, through the root canal, regardless of whether the pulp is vital or nonvital. It is an inflammation around the apex of a tooth. The distinctive features of AAP are microscopic rather than roentgenographic, symptomatic rather than visible.
Etiology
a. In vital tooth, it is associated with occlusal trauma, high points in restoration or wedging or forcing object between teeth.
b. In nonvital tooth, AAP is associated with sequelae to pulpal diseases.
c. Iatrogenic causes can be over instrumentation of root canal pushing debris and microorganisms beyond apex, overextended obturation and root perforations.
Signs and Symptoms
• Tooth is tender on percussion
• Dull, throbbing and constant pain
• Pain occurs over a short period of time
• Negative or delayed vitality test
• No swelling
• Pain on biting
• Cold may relieve pain or no reaction
• Heat may exacerbate pain or no reaction
• No radiographic sign; sometimes widening of periodontal ligament space.
Treatment
Management of acute apical periodontitis:• Endodontic therapy
• To control postoperative pain following initial endodontic therapy, analgesics are prescribed
• Use of antibiotics, either alone or in conjunction with root canal therapy is not recommended
• If tooth is in hyperocclusion, relieve the occlusion
• For some patients and in certain situations, extraction is an alternative to endodontic therapy.
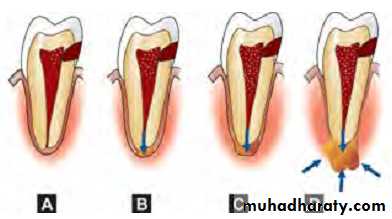
Acute apical abscess
It is a localized collection of pus in the alveolar bone at the root apex of the tooth, following the death of pulp with extension of the infection through the apical foramen into periradicular tissueIt is a localized collection of pus in the alveolar bone at the root apex of the tooth, following the death of pulp with extension of the infection through the apical foramen into periradicular tissue.Etiology
• Most common cause is invasion of bacteria from necrotic pulp tissue.• trauma, chemical or any mechanical injury resulting in pulp necrosis.
• Irritation of periapical tissue by chemical or mechanical treatment during root canal treatment.
Features of acute apical abscess:
• Tooth is nonvital• Pain
– Rapid onset
– Readily localized as tooth becomes increasingly tender to percussion
– Slight to intense throbbing pain
– Marked pain to biting
• Swelling
– Palpable, fluctuant
– Localized sense of fullness
• Mobility
May or may not be present
• Tooth may be in hyperocclusion
• Radiographic changes: small change to large periapical radiolucency
Symptoms
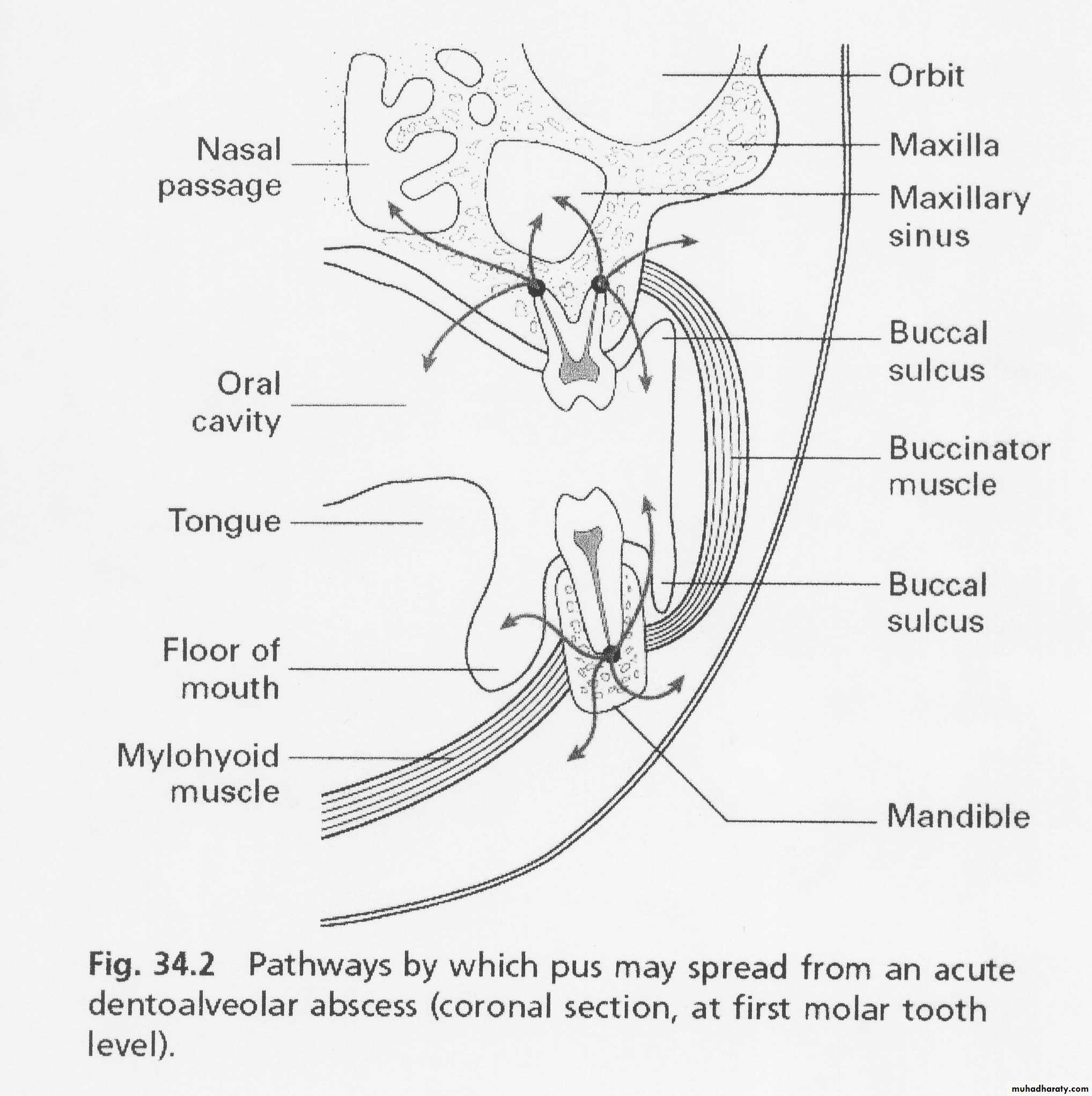
In early stage, there is tenderness of tooth which is relieved by continued slight pressure on extruded tooth to push it back into alveolus. Later on throbbing pain develops with diffuse swelling of overlying tissue. Tooth becomes more painful,
elongated and mobile as infection increases in latter stages. Patient may have systemic symptoms like fever, increased WBC count. Spread of lesion towards a surface may take place causing erosion of cortical bone or it may become diffuse and spread widely leading to formation of cellulitis. Location of swelling is determined by relation of apex of involved tooth to adjacent muscle attachment.
Diagnosis
• Clinical examination• Initially locating the offending tooth is difficult due to the diffuse pain. Location of the offending tooth becomes easier when tooth gets slightly extruded from the socket.
• Pulp vitality tests give negative response
• Tenderness on percussion and palpation.
• Tooth may be slightly mobile and extruded from its socket.
• Radiography helpful in determining the affected tooth as it shows a cavity or evidence of bone destruction at root apex.
Management of an Acute Apical Abscess
• Drainage of the abscess should be initiated as early as possible. This may include:a. Non-surgical endodontic treatment (Root canal therapy)
b. Incision and drainage
c. Extraction
• Considerations regarding the treatment should be dependent on certain factors:
a. Prognosis of the tooth
b. Patient preference
c. Strategic value of the tooth
d. Economic status of the patient
• In case of localized infections, systemic antibiotics provide no additional benefit over drainage of the abscess
• In the case of systemic complications such as fever, lymphadenopathy, cellulitis or patient who is immunocompromised, antibiotics should be given in addition to
drainage of the tooth
• Relieve the tooth out of occlusion in hyperocclusion cases
• To control postoperative pain following endodontic therapy, nonsteroidal anti-inflammatory drugs should be given
Phoenix abscess
Phoenix abscess is defined as an acute inflammatory reaction superimposed on an existing chronic lesion, such as a cyst or granuloma; acute exacerbation of a chronic lesion.
Etiology
Chronic periradicular lesions such as granulomas are in a state of equilibrium during which they can be completely asymptomatic. But sometimes, influx of necrotic products from diseased pulp or bacteria and their toxins can cause the dormant lesion to react. This leads to initiation of acute inflammatory response.
Symptoms
• Clinically often indistinguishable from acute apical abscess• At the onset—tenderness of tooth and elevation of the tooth from socket
• Tenderness on palpating the apical soft tissue.
Diagnosis
• Associated with initiation of root canal treatment most commonly• History from patient
• Pulp tests show negative response
• Radiographs show large area of radiolucency in the apex created by inflammatory connective tissue which has replaced the alveolar bone at the root apex
• Phoenix abscess should be differentiated from acute alveolar abscess by patient’s history, symptoms and clinical tests results.
Treatment
• Establishment of drainage• Once symptoms subside—complete root canal treatment.
Periapical granuloma
Periapical granuloma is one of the most common sequelae of pulpitis. It is usually described as a mass ofchronically inflamed granulation tissue found at the apex of nonvital tooth.
Etiology
Periapical granuloma is a cell mediated response to pulpal bacterial products. Bacterial and toxins cause mild irritation of periapical tissues. This leads to cellular proliferation and thus granuloma formation.Clinical Features
• Most of the cases are asymptomatic but sometimes pain and sensitivity is seen when acute exacerbation occurs• Tooth is not sensitive to percussion
• No mobility
• Soft tissue overlying the area may/may not be tender
• No response to thermal or electric pulp test
• Mostly, lesions are discovered on routine radiographic examination.
Radiographic Features
• Mostly discovered on routine radiographic examination• The earliest change in the periodontal ligament is found to be thickening of ligament at the root apex
• Lesion may be well circumscribed or poorly defined
• Size may vary from small lesion to large radiolucency exceeding more than 2 cm in diameter.
• Some amount of root resorption has been reported.
Treatment
Main objective in treatment is to reduce and eliminate offending organisms and irritants from the periapical area.
• In restorable tooth, root canal therapy is preferred
• In non-restorable tooth, extraction followed by curettage of all apical soft tissue.
Radicular cyst
The radicular cyst is an inflammatory cyst which results because of extension of infection from pulp into the surrounding periapical tissues.Etiology
• Caries• Irritating effects of restorative materials
• Trauma
• Pulpal death.
Clinical Features
• The cyst is frequently asymptomatic and sometimes it is discovered when periapical radiographs are taken of teeth with nonvital pulps• Incidence - Males are affected more than females.
• Age - Peak incidence in third or fourth decades.
• Site - Highest in anterior maxilla
- In mandibular posterior teeth, separate small cysts arise from each apex of multi-rooted teeth.
• Slowly enlarging swelling sometimes attains a large size.
• As the cyst enlarges in size, the covering bone becomes thin in size and exhibits springiness due to fluctuation.
• In maxilla, palatal expansion is mainly seen in case of maxillary lateral incisor.
• The involved tooth/teeth usually found to be nonvital, discolored, fractured or failed root canal.
Radiographic Features
Radiographically radicular cyst appears as round, pear or ovoid shaped radiolucency, outlined by a narrow radiopaque margin
Treatment
Different options for management of residual cyst are:• Endodontic treatment
• Apicoectomy
• Extraction (severe bone loss)
• Enucleation with primary closure
• Marsupilization (in case of large cysts).
Chronic alveolar abscess
Chronic alveolar abscess is also known as suppurative apical periodontitis which is associated with gradual egress of irritants from root canal system into periradicular area leading to formation of an exudate.Etiology
It is similar to acute alveolar abscess. It also results from pulpal necrosis and is associated with chronic apical periodontitis that has formed an abscess. The abscess has penetrated through bone and soft tissue to form a sinus react stoma on the oral mucosa.Symptoms
• Generally asymptomatic• Detected either by the presence of a sinus tract or on routine radiograph
• In case of open carious cavity—drainage through root canal sinus tract prevents swelling or exacerbation of lesion
Diagnosis
Chronic apical abscess may be associated with asymptomatic or slightly symptomatic tooth. Patient may give history of sudden sharp pain which subsided and has not reoccurred. Clinical examination may show a large carious exposure, a restoration of composite, acrylic, amalgam or metal, or discoloration of crown of tooth.It is associated symptoms only if sinus drainage tract become blocked. Vitality tests show negative response because of presence of necrotic pulps.