Dr. Athal Humo pediatric Lec 1
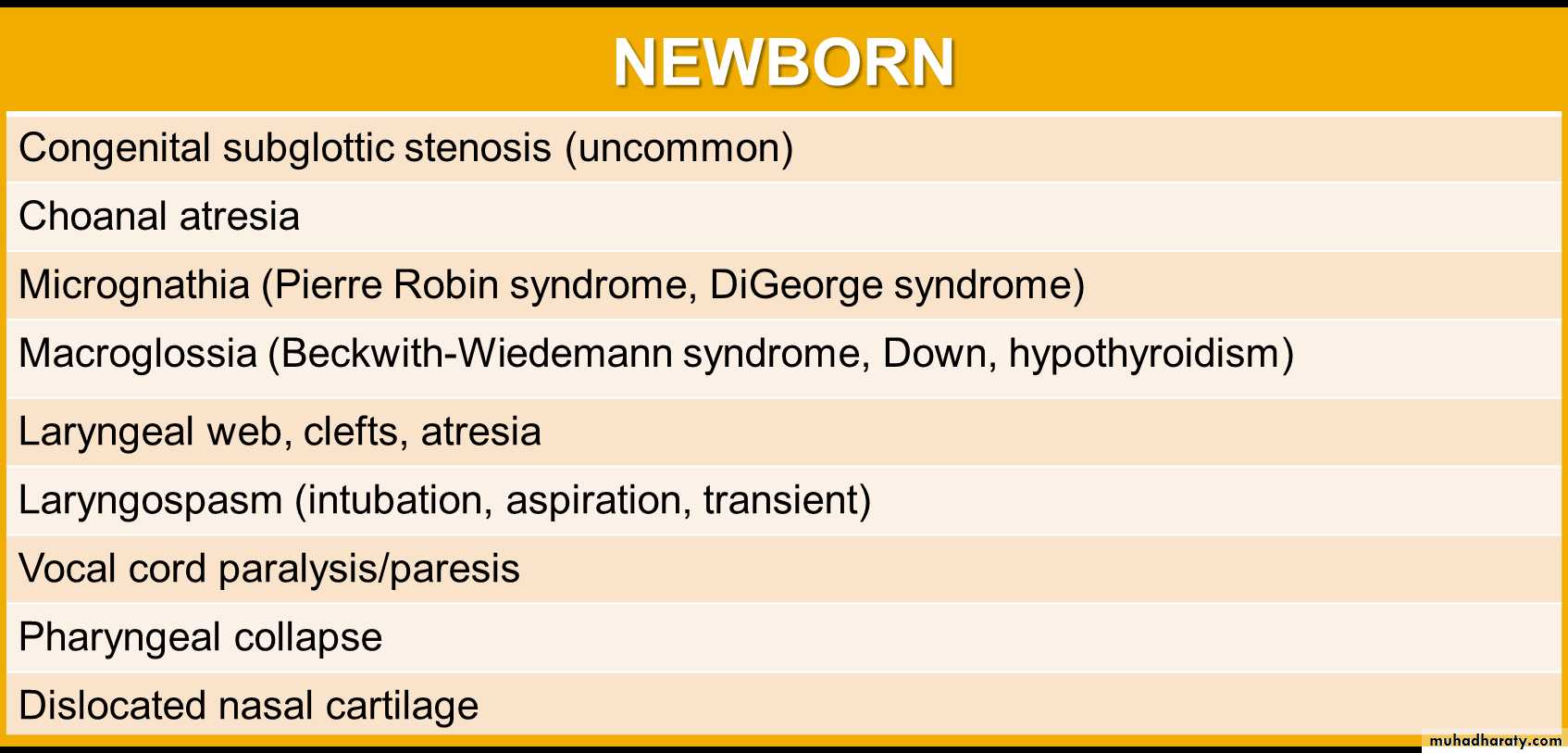
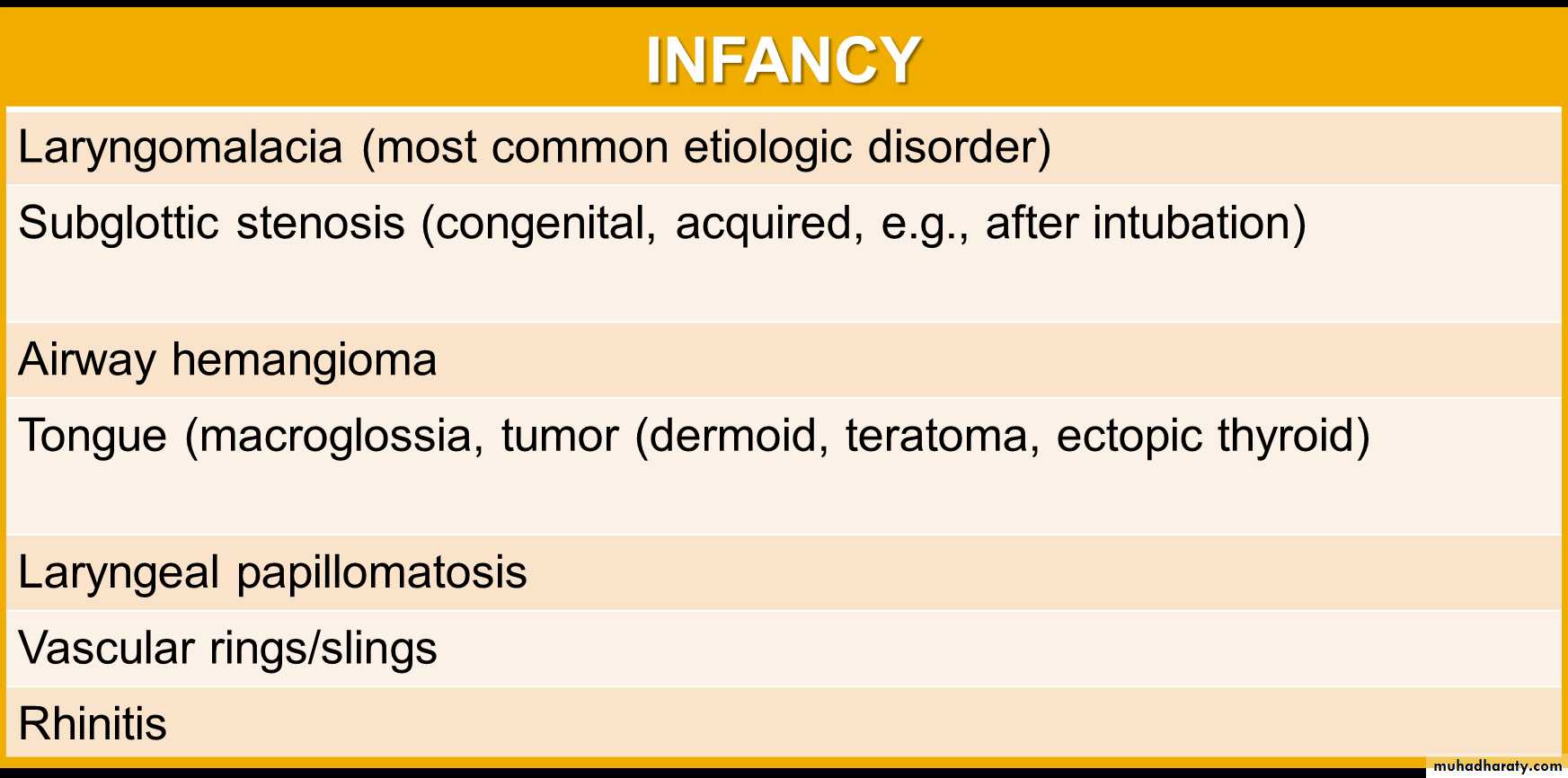
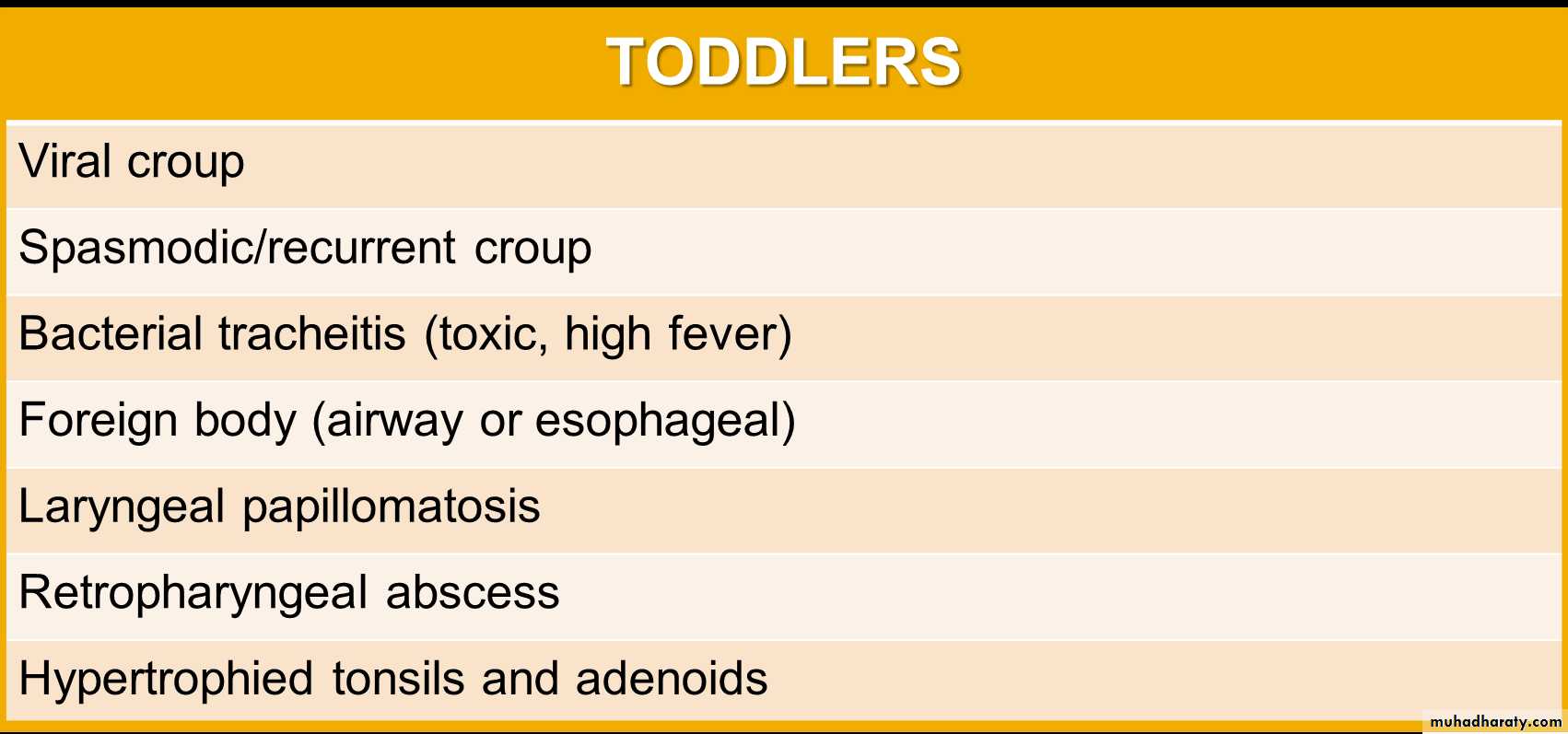
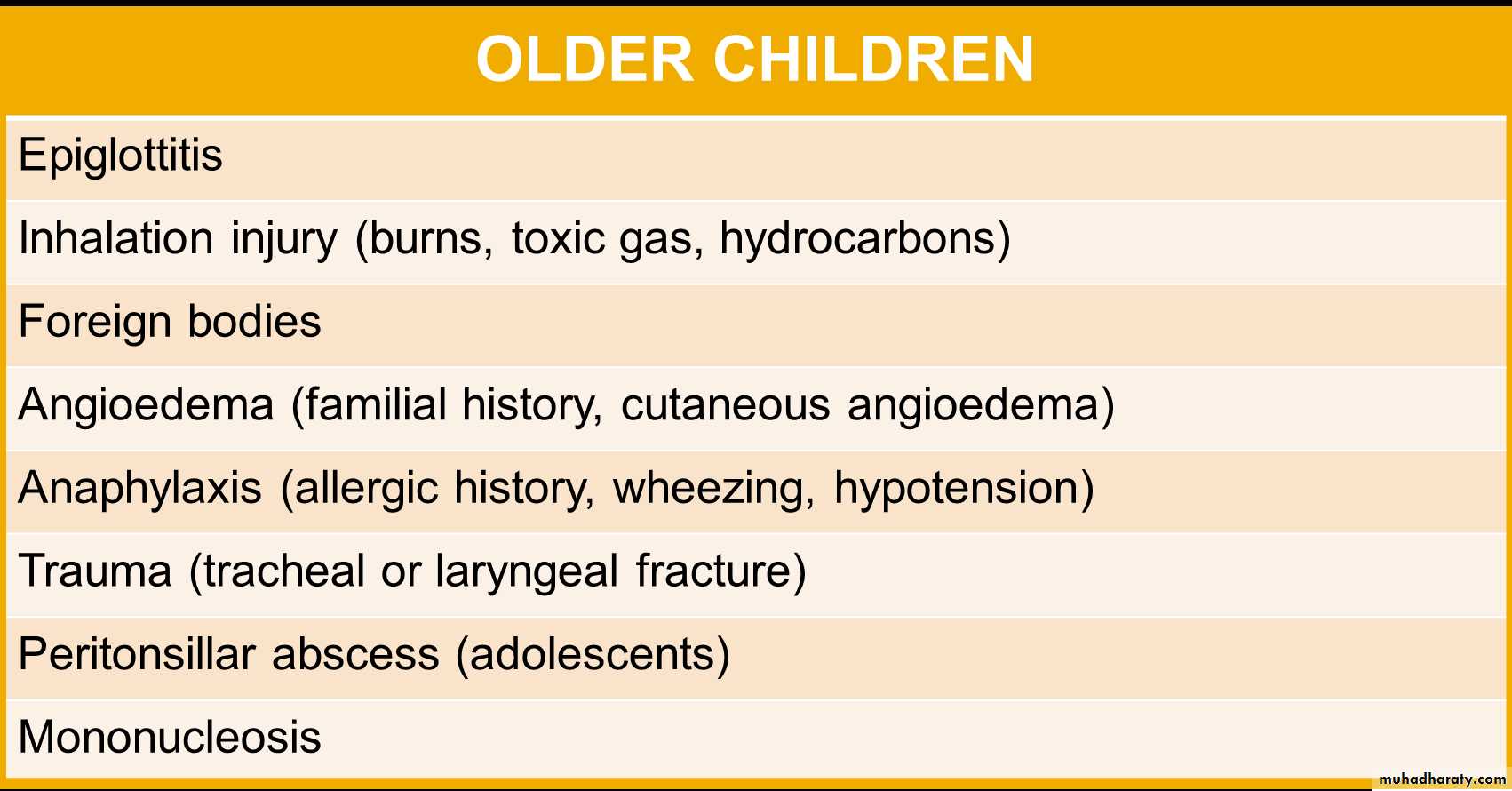
Upper Airway Obstruction (UAO)• UAO, is defined as blockage of any part of the airwaylocated above the thoracic inlet, can range fromnasal obstruction due to the common cold to lifethreatening obstruction of the larynx or upper trachea(subglottic space).ETIOLOGY• The differential diagnosis of airway obstruction varieswith patient age and can also be subdivided intosupraglottic and subglottic causesAge-Related Differential Diagnosis of Upper AirwayObstruction
CLINICAL MANIFESTATIONS• Upper airway obstruction is more pronounced duringinspiration.• The respiratory noise most commonly associated with upperairway obstruction is stridor, a harsh sound caused by thevibration of the airway structures mainly in inspiration.Occasionally stridor may also be present on exhalation.• Stridor often decreases during sleep due to lower inspiratoryflow rates and increase during feeding , excitement, & agitation.• Hoarseness suggests vocal cord involvement.DIAGNOSTIC STUDIES• Radiographic evaluation of a child with stridor may not be helpful. However,• Lateral views of the neck and nasopharynx can assess for adenoid hypertrophy &airway swelling.• AP views of the neck taken with the head in extension, the subglottic space should besymmetrical and the lateral walls of the airway should fall away steeply. Asymmetrysuggests subglottic stenosis or a mass lesion, while tapering suggests subglotticedema. However, these findings may be subtle.• Computed tomography (CT) scans of the upper airway can help delineate the site of theobstruction but may require sedation in younger children.• Flexible nasopharyngoscopy, which can be done without sedation, is extremely usefulin assessing airway patency, the presence of adenoid tissue, vocal cord, laryngomalaciaand other airway lesions,.• Bronchoscopy can be useful in assessing the subglottic space and intrathoracic largeairways, but this procedure requires deep sedation.
Adenoidal and Tonsillar Hypertrophy• The most common cause of chronic upper airwayobstruction in children is hypertrophy of the adenoidsand tonsils. The adenoids are lymphoid tissue arisingfrom the posterior and superior walls of thenasopharynx in the region of the choanae. Adenoidand tonsillar hyperplasia may be aggravated byrecurrent infection, allergy, and inhaled irritants.Clinical Manifestations:• Mouth breathing.• Snoring.• In some patients, obstructive sleep apnea.• Recurrent or persistent otitis media, because theeustachian tubes enter the nasopharynx at the choanaeand can be obstructed by enlarged adenoids.Diagnostic Studies:• Adenoidal hypertrophy is assessed by a lateralradiograph of the nasopharynx or by flexiblenasopharyngoscopy.Treatment• If the adenoids or tonsils are large and thought to besignificantly contributing to upper airway obstruction, then themost effective treatment is removal.• Because the adenoids are not a discrete organ but ratherconsist of lymphoid tissue, regrowth after adenoidectomy ispossible.• If the tonsils are large and the obstruction is severe, thenremoving the tonsils in addition to the adenoids may benecessary.
Choanal Stenosis (Atresia)• Choanal stenosis/atresia is a congenital problem that presentsin the neonatal period. It may be bilateral or unilateral and is arelatively rare cause of respiratory distress in newborns.• Neonates are generally obligate nose breathers, so obstructionof nasal passages can cause significant respiratory distress.• Inability to easily pass a small catheter through the nostrilsshould raise the suspicion of choanal atresia.• The diagnosis is confirmed by CT scan and by inspecting thearea directly with a flexible nasopharyngoscope.• An oral airway may be useful in the short term, but thedefinitive treatment is surgery
Acute Epiglottitis• It is a medical emergency because of the risk ofsudden supraglottic airway obstruction.• This illness is now rare and usually caused by groupA streptococcal or staphylococcus aureus infectionsor H. influenza type B in unimmunized patients.Clinical Manifestation• Characterized by an acute rapidly progressive course.• Often, the otherwise healthy child suddenly develops a sore throat andfever. Within a matter of hours, the patient appears toxic, swallowing isdifficult, and breathing is labored.• Drooling is usually present and the neck is hyperextended in anattempt to maintain the airway. The patients typically have a preferencefor sitting, often with the head held forward, the mouth open, and thejaw thrust forward (sniffing position).• A brief period of air hunger with restlessness may be followed byrapidly increasing cyanosis and coma.• Stridor is a late finding and suggests near-complete airwayobstruction.• Complete obstruction of the airway and death can ensue unlessadequate treatment is provided.• The barking cough typical of croup is rare. Usually, no other familymembers are ill with acute respiratory symptoms.Diagnosis• Lateral radiograph reveals thickened and bulging epiglottis (thumbsign) and swelling of the aryepiglottic folds.• Anxiety-provoking interventions such as phlebotomy, intravenousline placement, placing the child supine, or direct inspection of theoral cavity should be avoided until the airway is secure.• The diagnosis is confirmed by direct observation of the inflamedand swollen supraglottic structures and swollen, cherry-redepiglottitis, which should be performed only in prepared operatingroom to place an endotracheal tube or perform a tracheostomy ifneeded.Treatment• Antibiotic therapy: as 3rd generation cephalosporine &chloramphenicol.• Endotracheal intubation: to maintain the airway. Clinicalrecovery is rapid, and most children can be extubated safelywithin 48 to 72 hours.
Croup (Laryngotracheobronchitis)• Croup, or laryngotracheobronchitis, is the most commoninfection of the middle respiratory tract.• The most common causes of croup are parainfluenza viruses(types 1, 2, and 3) and respiratory syncytial virus.• Croup is most common in children 6 months to 3 years of age,with a peak in fall and early winter. It typically follows acommon cold.CLINICAL MANIFESTATIONS• The manifestations of croup are a harsh barking cough,hoarseness, inspiratory stridor, low-grade fever, andrespiratory distress that may develop slowly or quickly.• Signs of upper airway obstruction, such as labored breathingand marked suprasternal, intercostal, and subcostalretractions, may be evident on examination.• Wheezing may be present if there is associated lower airwayinvolvement.LABORATORY AND IMAGING STUDIES• Anteroposterior radiographs of the neck show thediagnostic subglottic narrowing of croup known asthe steeple sign.• Many rapid tests (PCR or antigen) are available forparainfluenza viruses and RSV.PA view of the upper airway shows the so-called steeple sign, thetapered narrowing of the immediate subglottic airway (arrows)
TREATMENT• Oral or intramuscular dexamethasone reduces symptoms, theneed for hospitalization, and shortens hospital stays.Dexamethasone phosphate (0.6 to 1 mg/kg) may be givenonce intramuscularly or dexamethasone (0.6 to 1 mg/kg) onceorally. Alternatively, prednisolone (2 mg/kg per day) may begiven orally in two to three divided doses.• For significant airway compromise, administration ofaerosolized racemic epinephrine reduces subglottic edemaby vasoconstriction, temporarily producing marked clinicalimprovement. Aerosol treatment may need to be repeatedevery 20 minutes (for no more than 1 to 2 hours) in severecases.• Children should be kept as calm as possible to minimizeforceful inspiration. One useful calming method is for a childwith croup to sit in the parent's lap. Sedatives should be usedcautiously and only in the intensive care unit. Cool mistadministered by face mask may help prevent drying of thesecretions around the larynx.• Hospitalization is often required for:o Children with stridor at rest.o Children receiving aerosol treatment should be hospitalized or observedfor at least 2 to 3 hours because of the risk of rebound airway obstruction.
Bacterial Tracheitis• It is a rare but serious superinfection of the tracheathat may follow viral croup and is most commonlycaused by S. aureus.
Laryngomalacia (Floppy Larynx)• Laryngomalacia is most common cause of stridor in infants. It isdue to exaggerated collapse of the glottic structures, especially theepiglottis and arytenoid cartilages, during inspiration, but its precisecause is not known.• It may be due to decreased muscular tone of the larynx andsurrounding structures or to immature cartilaginous structures.• Inspiratory stridor beginning at or shortly after birth should raise thesuspicion of laryngomalacia. It usually does not result in muchrespiratory distress, but occasionally it is severe enough to causehypoventilation (CO2 retention), hypoxemia, and difficulty withfeeding.Clinical Manifestations• The primary sign of laryngomalacia is inspiratorystridor with little to no expiratory component. Thestridor is typically loudest when the infant is feedingor active and decreases when the infant is relaxed,supine, or the neck is flexed. Exacerbated by viralrespiratory infections & GERD.• Laryngomalacia normally peaks by 3 to 5 months ofage and resolves between 6 and 12 months of age.Diagnostic Studies• In typical cases, no need for investigation.• In severe or atypical cases, the patient should undergoflexible nasopharyngoscopy/laryngoscopy to assess thepatency and dynamic movement (collapse) of the larynxand surrounding structures.Treatment• In most cases, no therapy is required for laryngomalacia. Theinfant should be observed closely during times of respiratoryinfection for evidence of respiratory compromise, althoughmost infants with laryngomalacia tolerate infections fairly well.• Infants with severe laryngomalacia that results inhypoventilation, hypoxia, or growth failure may benefit from asurgical procedure (aryoepiglottoplasty) or, in extreme cases, atracheostomy to bypass the upper airway.
Subglottic Stenosis• Subglottic stenosis is the narrowing of tracheaimmediately below the vocal cords.• It may be:• Congenital• Acquired: due to prolonged or repeatedendotracheal intubation.Clinical Manifestations• Subglottic stenosis can present as stridor that is frequentlybiphasic (on both expiration and inspiration). However, thestridor is usually more prominent on inspiration.• Subglottic stenosis may also be associated with a barky coughsimilar to that noted with croup.• Respiratory infections can cause subglottic edema,exacerbating the clinical manifestations of subglottic stenosis.Diagnostic Studies• Definitive diagnosis requires endoscopic evaluation,either by flexible or rigid bronchoscopy.Treatment• Mild subglottic stenosis can be managed conservatively andmay improve sufficiently with airway growth alone.• Severe cases require surgical intervention.
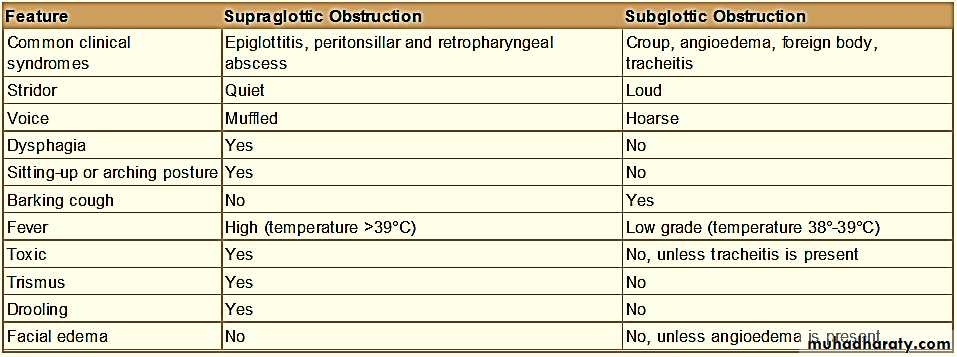
Others causes of UAO• hemangioma, usually presents before 6 months of age. Thetreatment of hemangiomas is controversial, but laser therapy andcorticosteroids (both direct injection and systemic) have been usedwith moderate success. If the obstruction is severe, tracheostomytube is needed.• Juvenile laryngeal papillomatosis .• Vocal Cord Paralysis, Paralysis may be unilateral or bilateral and ismore often caused by damage to the recurrent laryngeal nerve thanby a central lesion. Peripheral nerve injury can be caused by trauma(neck traction during delivery of infants or thoracic surgicalprocedures). Central causes as hydrocephalus.• Foreign body, should considered in any infant or child capable ofingesting small objects who develops acute onset of stridor.Differentiating Supraglottic from Subglottic Causes of Airway Obstruction