Epilepsy
Epilepsy is as a disorder of brain characterized by an ongoing liability to recurrent seizures. Epileptic seizure is defined as the transient clinical manifestations that result from an episode of epileptic neuronal activity.Epileptic neuronal activity is a specific dysfunction, characterized by abnormal synchronization, excessive excitation and/or inadequate inhibition, and can affect small or large neuronal populations
The clinical manifestations are sudden and usually brief. They include motor, psychic, autonomic and sensory phenomenon, with or without alteration in consciousness or awareness, and the symptoms depend on the part of the brain involved in the epileptic neuronal discharge, and the intensity of the discharge.
Seizure types:
Generalized seizures
Note by the students:
There are several nice videos on YouTube demonstrating the different types of seizure.
Note by the students:There are several nice videos on YouTube demonstrating the different types of seizure.
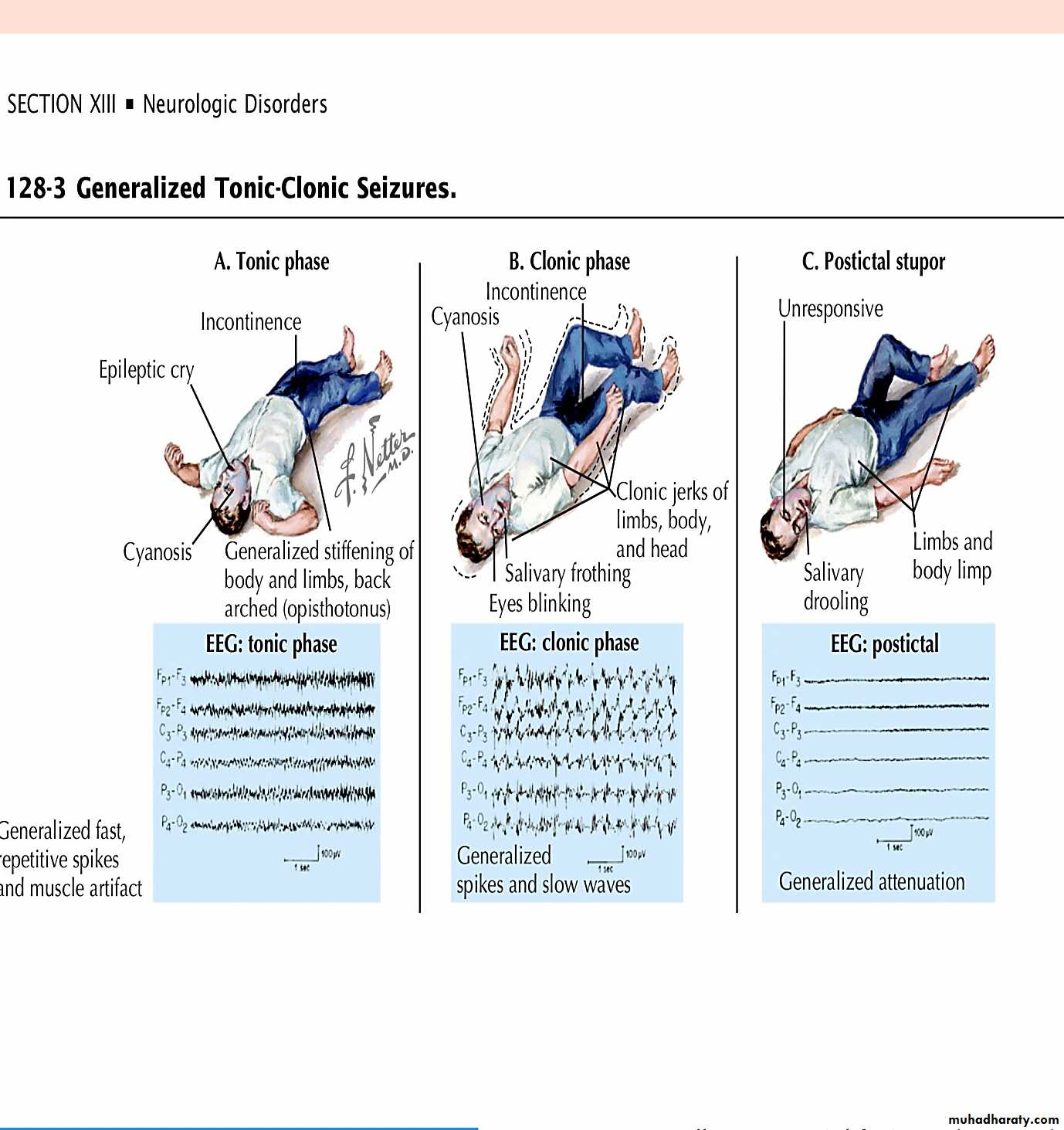
Tonic–clonicAbsence
Myoclonic
Clonic
Tonic
Atonic
2- Focal seizures
Without impairment of consciousness or awareness (simple partial)
Focal motor
Focal sensory
With impairment of consciousness or awareness (complex partial)
3- Secondarily generalized seizure
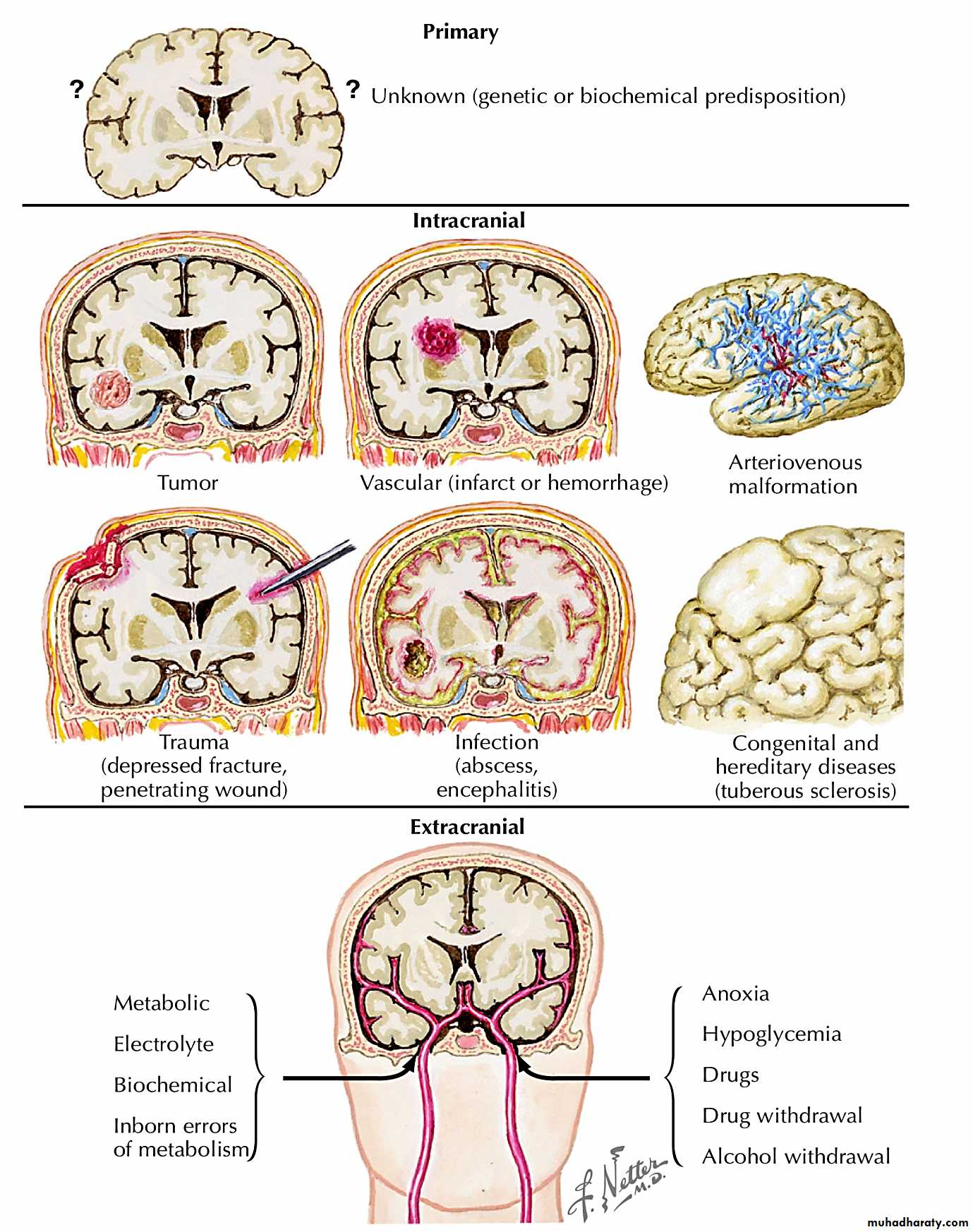
Note by the students there is a nice picture in the appendix (page 12) summarize some of the causes of seizure.
Note by the students there is a nice picture in the appendix (page 12) summarize some of the causes of seizure.
Causes of seizure:
Idiopathic
Genetic
Dysembryonic e.g. (Cortical dysgenesis)
Cerebral birth injury
Cerebral anoxia
Cerebrovascular disease (Intracerebral haemorrhage, infarction,)
Arteriovenous malformation
Tumors (primary and secondary)
Trauma (including neurosurgery)
Infective e.g. (Meningitis, Cerebral abscess, Encephalitis.)
Inflammatory e.g. (Vasculitis)
Drugs e.g. (Antibiotics, Psychotropic agents)
Alcohol (especially withdrawal)
Toxins e.g. Organophosphates (sarin)
Metabolic disease e.g. Hypocalcaemia Hypomagnesaemia, Hypoglycemia, Hyponatremia, Renal failure, Liver failure
Trigger factors for seizures
Sleep deprivation
Missed doses of anti-epileptic drugs in treated patients
Alcohol (particularly withdrawal) Recreational drug misuse
Physical and mental exhaustion
Flickering lights, including TV and computer
Intercurrent infections and metabolic disturbances
Uncommon: loud noises, reading, hot baths
Investigations
From where is the epilepsy arising?Standard EEG
Sleep EEG
What is the cause of the epilepsy?
Structural lesion?
CT, MRI
Metabolic disorder?
Urea and electrolytes
Liver function tests
Blood glucose
Serum calcium, magnesium
Inflammatory or infective disorder?
Full blood count
Chest X-ray
Collagen disease
CSF examination
Comparison between seizure and pseduoseizure
Pseduoseizure
SeizureCommon, emotional and stress-related
RarePrecipitating cause
1
Rare
Common
When alone or asleep
2
Longer
Usually short
Duration
3
Asynchronous flailing of limbs; pelvic thrusting; opisthotonos
Tonic, clonic ,tonic clonic synchronous small amplitude jerks
Body movement
4
May bite tongue usually anterior, throw self to ground, Directed violence
Tongue biting usually lateral side , fall
Injury
5
Variable, often inconsistent with seizure type
Complete loss in generalized tonic–clonic; may be incomplete in complex partial
Consciousness
6
Usually closed
Usually open
Eye
7
Rare
Common
Incontinence
8
Management
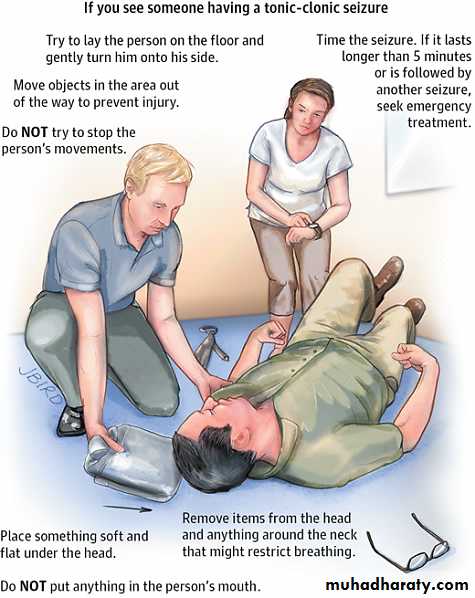
It is important to explain the nature and cause of seizures to patients and their relatives, and to instruct relatives in the first aid management of seizures.
Note by the students: There are nice videos on YouTube demonstrating how to administer First Aid for patient having seizure for e.g.:
Every day First Aid: Seizure (epilepsy) uploaded by British Red Cross
Note by the students: There are nice videos on YouTube demonstrating how to administer First Aid for patient having seizure for e.g.:
Every day First Aid: Seizure (epilepsy) uploaded by British Red Cross
How to administer first aid for seizures
Move person away from danger (fire, water, machinery, furniture).After convulsions cease, turn person into ‘recovery’ position (semi-prone).
Ensure airway is clear but do NOT insert anything in mouth (tongue-biting occurs at seizure onset and cannot be prevented by observers).If convulsions continue for more than 5 mins or recur without person regaining consciousness, summon urgent medical attention
Do not leave person alone until fully recovered (drowsiness and confusion can persist for up to 1 hr.)
Many people with epilepsy feel stigmatized and may become unnecessarily isolated from work and social life. It should be emphasized that epilepsy is a common disorder that affects 0.5–1% of the population, and that full control of seizures can be expected in approximately 70% of patients.
Anticonvulsant therapy
Anticonvulsant drug treatment (anti-epileptic drugs, or AEDs) should be considered after more than one unprovoked seizure. The decision to start treatment should be shared with the patient, to enhance compliance. A wide range of drugs is available. These agents either increase inhibitory neurotransmission in the brain or alter neuronal sodium channels to prevent abnormally rapid transmission of impulses. In the majority of patients, full control is achieved with a single drug.
Guidelines for anticonvulsant therapy
Start with one first-line drug
Start at a low dose; gradually increase dose until effective control of seizures is achieved or side-effects develop (drug levels may be helpful)
Optimize compliance (use minimum number of doses per day)
If first drug fails (seizures continue or side-effects develop), start second first-line drug, followed if possible by gradual withdrawal of first
If second drug fails (seizures continue or side-effects develop), start second-line drug in combination with preferred first-line drug at maximum tolerated dose (beware interactions)
If this combination fails (seizures continue or side-effects develop), replace second-line drug with alternative second-line drug
If this combination fails, check compliance and reconsider diagnosis (Are events seizures? Occult lesion? Treatment compliance/alcohol?)
Consider alternative, non-drug treatments (e.g. epilepsy surgery, vagal nerve stimulation)
Use minimum number of drugs in combination at any one time
Epilepsy type
First-lineSecond-line
Third-line
Focal onset and/or
secondary GTCS
Lamotrigine
Carbamazepine
Levetiracetam
Sodium- valproate
Topiramate
Gabapentin
Oxcarbazepine
Phenobarbital
Phenytoin
GTCS
Sodium -valproate
Levetiracetam
Lamotrigine
Topiramate
Carbamazepine
Phenytoin
Absence
Ethosuximide
Sodium- valproate
Lamotrigine
Clonazepam
Myoclonic
Sodium -valproate
Levetiracetam
Clonazepam
Lamotrigine
Phenobarbital
Lifestyle advice
Patients should be advised to avoid activities where they might place themselves or others at risk if they have a seizure. This applies at work, at home and at leisure. At home, only shallow baths (or showers) should be taken. Prolonged cycle journeys should be discouraged until reasonable freedom from seizures has been achieved. Activities requiring prolonged proximity to water (swimming, fishing or boating) should always be carried out in the company of someone who is aware of the risks and the potential need for rescue measures. Driving regulations vary between countries, and the patient should be made aware of these. Certain occupations, such as firefighter or airline pilot, are not open to anyone who has a previous or active diagnosis of epilepsy.
Differential diagnosis of epilepsy
Syncope
Hypoglycemia
Transient ischemic attack
Pseduoseizure
Idiopathic generalized epilepsy
This term should be used to denote presumed genetic basis. Idiopathic generalized epilepsy (IGE) accounts for about 10–20% of all patients with epilepsy.
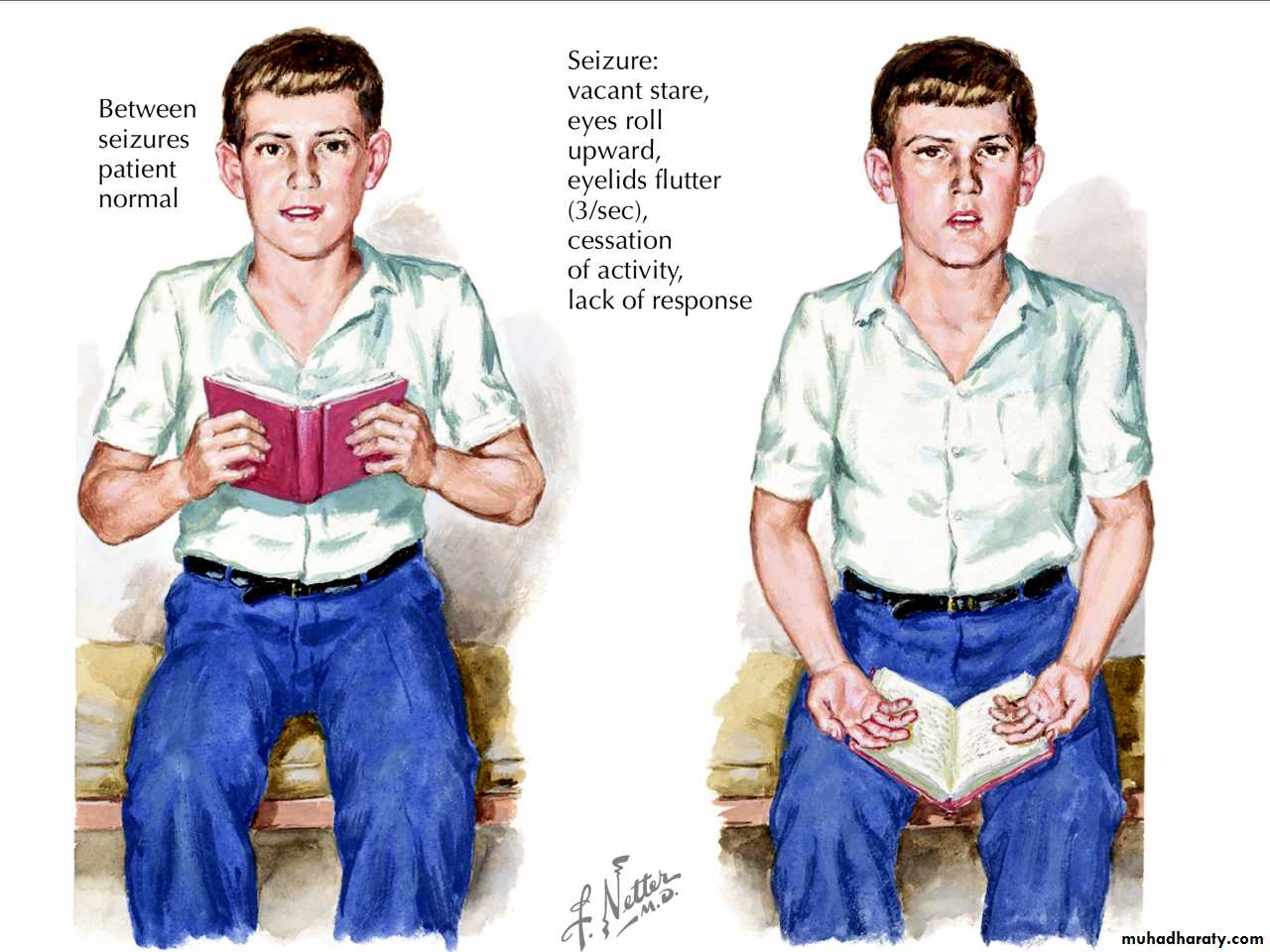
Childhood absence epilepsy
This condition, more common in girls, appears in childhood (peak age 6–7 years), and is not associated with learning disability or other neurological problems. The seizures take the form of generalized absence attacks. These comprise an abrupt sudden loss of consciousness and the cessation of all motor activity. Tone is preserved, and there is no fall. The patient is not in contact with the environment, the attack ends as abruptly as it is started, and previous activity is resumed as if nothing had happened. There is no confusion and the patient is often unaware that an attack has occurred.
Juvenile myoclonic epilepsy
This is the most common subtype of IGE, and accounts for up to 10% of all epilepsies. The characteristic seizures are brief myoclonic jerks, occurring in the first hour or so after awakening, and usually in bursts. These are sudden, shock-like jerks, affecting mainly the shoulders and arms, usually but not always symmetrically. It is often not clear whether consciousness was retained or lost.
The myoclonus develops between the ages of 12 and 18 years. In about 80% of cases, generalized tonic– clonic seizures also occur, usually months or years after the onset of myoclonus, complete response to treatment can be expected in 80–90% of cases, but lifelong therapy may be needed.
Withdrawing anticonvulsant therapy
Withdrawal of medication may be considered after a patient has been seizure-free for more than 2 years. Childhood-onset epilepsy, particularly classical absence seizures, carries the best prognosis for successful drug withdrawal. Other epilepsy syndromes, such as juvenile myoclonic epilepsy, have a marked tendency to recur after drug withdrawal. Seizures that begin in adult life, particularly those with partial features, are also likely to recur, especially if there is an identified structural lesion Overall, the recurrence rate after drug withdrawal depends on the individual’s epilepsy history. Patients should be advised of the risks of recurrence, to allow them to decide whether or not they wish to withdraw. If undertaken, withdrawal should be done slowly, reducing the drug dose gradually over weeks or months. Withdrawal may necessitate precautions around driving or occupation.Epilepsy surgery
Some patients with drug-resistant epilepsy benefit from surgical resection of epileptogenic brain tissue. Less invasive treatments, including vagal nerve stimulation, lobectomy, lesionectomy, carpouscalositomy may also be helpful in some patients.
All those who continue to experience seizures despite appropriate drug treatment should be considered for surgical treatment.
Status epilepticus
Status epilepticus is seizure activity not resolving spontaneously, or recurrent seizure with no recovery of consciousness in between. Persisting seizure activity has a recognized mortality and is a medical emergency. Diagnosis is usually clinical and can be made on the basis of the description of prolonged rigidity and/or clonic movements with loss of awareness. In patients with pre-existing epilepsy, the most likely cause is a fall in anti-epileptic drug levels.
In de novo status epilepticus, it is essential to exclude precipitants such as infection (meningitis, encephalitis), neoplasia and metabolic derangement (hypoglycemia, hyponatremia, hypocalcaemia).
Management of status epilepticus
Initial
Ensure airway is patent; give oxygen to prevent cerebral Hypoxia
Check pulse, blood pressure, and respiratory rate
Secure intravenous access
Send blood for: Glucose, urea and electrolytes, calcium and magnesium, liver function, anti-epileptic drug levels ,full blood count, Storing a sample for future analysis (e.g. drug misuse)
Correct any metabolic trigger, e.g. hypoglycemia
If seizures continue for > 5 mins: give diazepam 10 mg IV (or rectally) or lorazepam 4 mg IV; repeat once only after 15 mins.
Ongoing
If seizures continue after 30 mins IV infusion (with cardiac monitoring) with one of:Phenytoin: 15 mg/kg at 50 mg/min
Fosphenytoin: 15 mg/kg at 100 mg/min
Phenobarbital: 10 mg/kg at 100 mg/min
Give attention for cardiac monitor and pulse oximetry
Monitor neurological condition, blood pressure, respiration; check blood gases
If seizures still continue after 30–60 mins
Transfer to intensive care
Start treatment for refractory status with intubation, ventilation and general anesthesia using propofol or thiopental
EEG monitor
Once status controlled
Commence longer-term anticonvulsant medication with one of:
Sodium valproate 10 mg/kg IV over 3–5 mins, then 800–2000 mg/day
Carbamazepine 400 mg by nasogastric tube, then 400–1200 mg/day.
END
Appendix:
Note: the below appendix were added by the students (it’s not included in lecture)
Causes of seizure:
Please note: Seizures of unclear etiology are called epilepsy. If there is a clear cause, it is not epilepsy.
Link to obstetrics: A 23 year old female presents to the ER with a first-time seizure during the eighth month of her first pregnancy. Is this seizure more likely to be related to her pregnancy or to a preexisting condition?
Answer: First- time seizure in pregnancy is more likely to be due to eclampsia! Which typically follows preeclampsia, a serious complication of high blood pressure during pregnancy.
Link to obstetrics: A 23 year old female presents to the ER with a first-time seizure during the eighth month of her first pregnancy. Is this seizure more likely to be related to her pregnancy or to a preexisting condition?
Answer: First- time seizure in pregnancy is more likely to be due to eclampsia! Which typically follows preeclampsia, a serious complication of high blood pressure during pregnancy.
Link to pediatrics: If a child is brought from school to his/her pediatrician after experiencing multiple intermittent 5-seconds episodes of staring into space and is not doing well in his class.
Think about Generalized absence (petit mal) seizures which usually presents in young age group. (Drug of Choice for this case: Ethosuximide)
Link to pediatrics: If a child is brought from school to his/her pediatrician after experiencing multiple intermittent 5-seconds episodes of staring into space and is not doing well in his class.
Think about Generalized absence (petit mal) seizures which usually presents in young age group. (Drug of Choice for this case: Ethosuximide)
Phases of Tonic-Clonic seizure:
Case presentation: A 27-year-old man is having breakfast with his wife when suddenly he arches his back, turns his head to the side, shrieks loudly, and falls to the ground. His arms and legs remain extended for approximately 30 seconds, after which his arms and legs begin to flex and extend rhythmically for the next 2 minutes. The patient's wife calls 911, and on arrival the paramedics find the patient lying on the floor. He appears stuporous but can respond to vocal commands. He has bitten his tongue badly, and is soiled from having lost control of bowel and bladder functions. The patient is confused and appears to have no knowledge of what has happened to him. The paramedics transfer the patient to the ambulance and bring him to the emergency department for further evaluation.