LEC 2 د.علي الشالجي
Complicated Head Injury
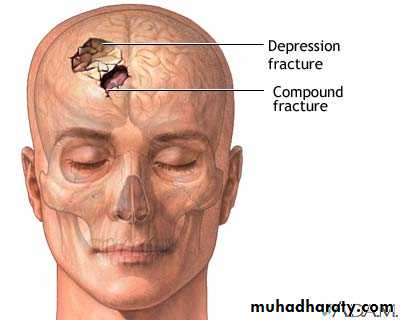
I- Penetrating Head Injury:Compound depressed Fracture
Divided into 2 categories:A. Penetrating head injury.
B. Fractured base of skull.
Skull Fracture
Linear Fracture Compound depressed Fracture
A: Penetrating (or compound depressed fracture):
Usually caused by local trauma by a sharp object or a heavy small object (e.g. hammer) or bullet or missile injury.Usually there is a depressed fracture of skull with or without tear of the dura and the contents of the brain can come out of the wound; therefore there is a high possibility of infection; however the injury to the brain is focal and not diffused unlike blunt fracture so the patient can be good if we avoid infection.
Usually the patient is conscious, unless the sharp object penetrated to the brain stem, in such a case the patient is presented unconscious.
Diagnosis:
Sometimes just by inspection we can see the brain tissue out, or by palpation we can feel the depressed segment, but sometimes the inner table is the, only depressed part (inner table is the inner side of the skull bone), so the X-ray is the most essential and diagnostic procedure (and this may be the only case in which the skull X-ray is very essential for diagnosis).Surgical management:
Usually under GA and in the 1st 24 hour if the dura isn't torn; and if there is dural tear (with the brain tissue coming out), then it should be done in the first 6 hours.We do wound debridement and removal of the depressed segment with closure of the dural and skull in multiple layers.
Heavy antibiotic post-operatively preferably combination from those antibiotic that cross the BBB.
Procedure:
Here, our primary goal is to prevent infection, the depressed bone is liable for necrosis and then infection and abscess, so the idea is just wound debridement.
So we make an S-shape incision (extending from the wound which is usually small), then we remove dead tissue and hair inside the wound, and if there's foreign body close to the wound we remove it. If the foreign body (the missile or the bullet) is distant, we don't try to remove it, because the idea here is not to remove the foreign body.
Then we come to the depressed segment, if we try to remove it immediately, it will be pushed and twist the brain tissue and cause more damage. So we make a Burr hole in the skull adjacent to it, and start dimpling the bone around it (we may lose some bone tissue but we will save the brain from the necrotic bony fragment), then we take out the bone fragment and we clean the wound with normal saline, remove adjacent foreign bodies and we suture the dura and close the wound, and start with prophylactic antibiotics, usually combination.
Prognosis:
Is usually good unless there is:- Infection.
- Intracranial bleeding.
- Sinus involvement or a vital area of the brain.
- In case of bullet injury through and through, the mortality rate here is 100%.
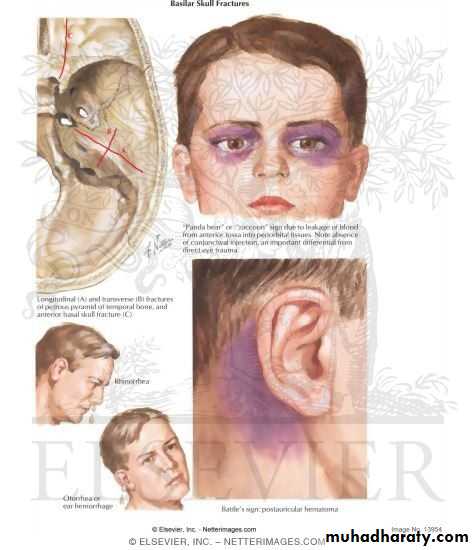
B: Fracture of the base of the skull:
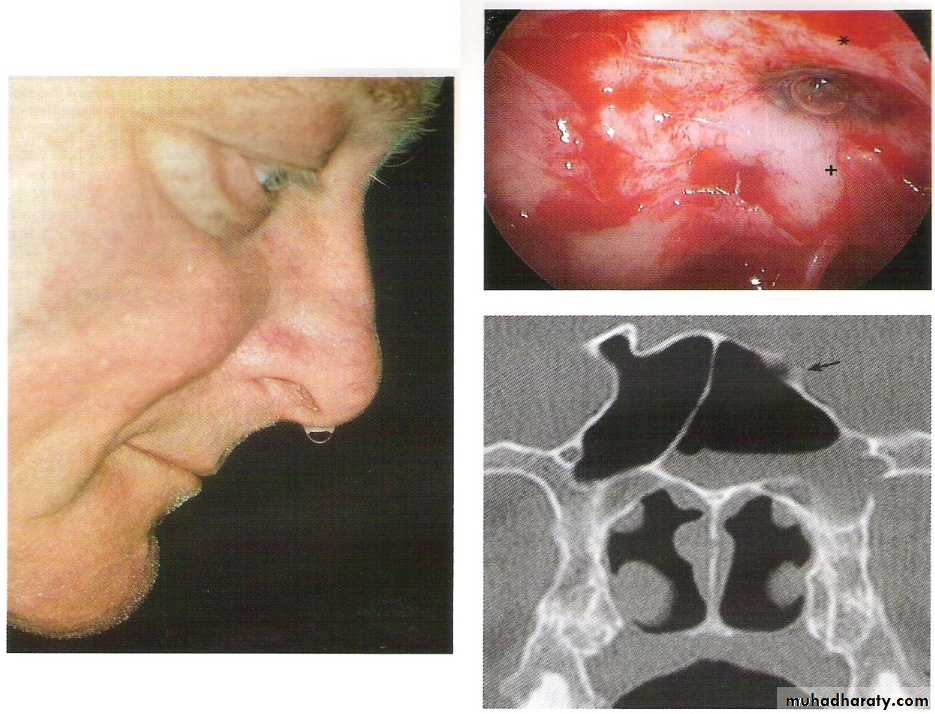
In this instance, there's high possibility of dural tear, because the dura mater here is very adherent to the bone. It is regarded as a compound fracture if the fracture line involves the paranasal sinuses; therefore we can get leak with a possibility of meningitis or aerocele (pneumatocephaus).CSF leak is either from the ear and called "Otorrhea" which is not very serious unless there is chronic infection as chronic otitis media, or the leak is from the nose and called "Rhinorrhea" and a salty test will be felt in the mouth, it is more serious as the nose is usually the site of infection or nosocomial organisms.
We take a sample from the fluid and test it in lab for sugar, because CSF is the only fluid in this area that contains glucose to be sure that the leaking fluid is CSF.
SO, signs of fractured base of the skull:
1. Raccoon eye (periorbital ecchymosis) due to leakage of blood from the ant. fossa into the periorbital fissures, there is absence of conjunctival reaction an important difference for direct eye trauma2. Battle’s sign (postauricular hematoma)
3. CSF Otorrhea and Rhinorrhea
CSF otorrhoea
CSF rhinorrhoea
Raccoon eye
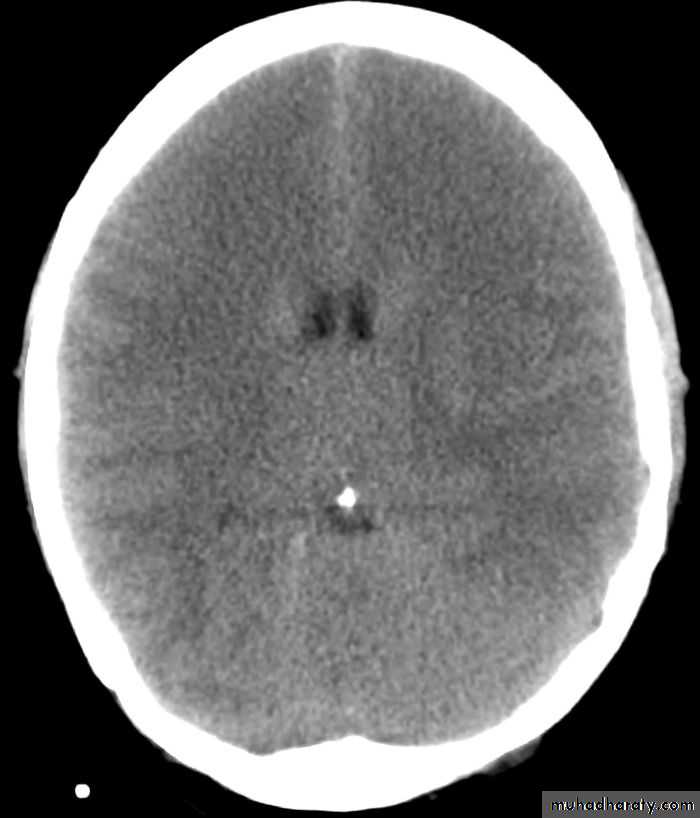
pneumocephalus
Management:Here, we try to be as conservative as we can, we put the patient in head-up position our management is as follows:
Swab for the culture and sensitivity from the nose, throat and conjunctiva (due to nasolacrimal duct) in case of rhinorrhea.
Prophylactic antibiotics (usually combination); If meningitis develop, still antibiotics is the measure of choice.
We can minimize the CSF leak by two ways:
Diuretics.
We do lumbar puncture because the leak is caused mostly by increased
intracranial pressure, so the LP will reduce the intracranial pressure.
Usually a plug is formed which close the area of leak and stop it; but if the leak continues more than one week then surgical repair is indicated by craniotomy and dural closure; but there should be no meningitis because the wound will reopen again and the surgery will fail, so we should treat meningitis first by antibiotics and wait until it disappear to be able to perform surgery.
Aerocele: air will enter the dura through a defect and may collect in the brain substance.
- By X- ray we may see bubbles.- Rx is usually conservative and very rarely surgical.
Note: LP is contraindicated if there's a brain mass because we are afraid of coning of this mass.
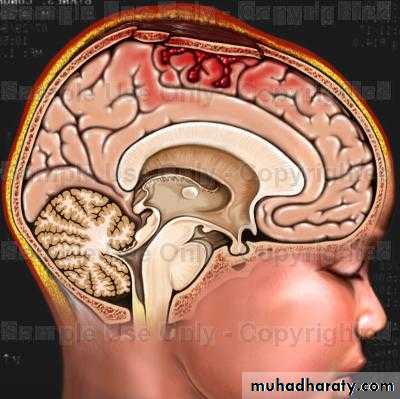
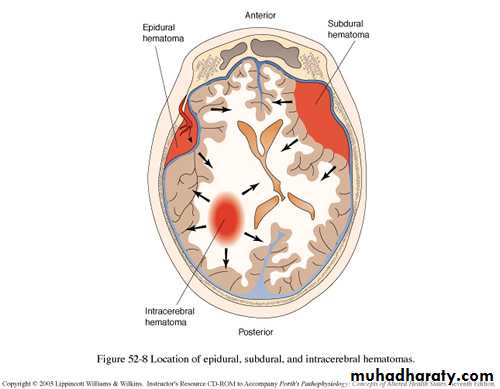
II- Intracranial Hemorrhage (Hematoma):
Extradural hematoma.
Subdural hematoma.Intracerebral hematoma.
Intraventricular hemorrhage.
Subarachnoid hemorrhage.
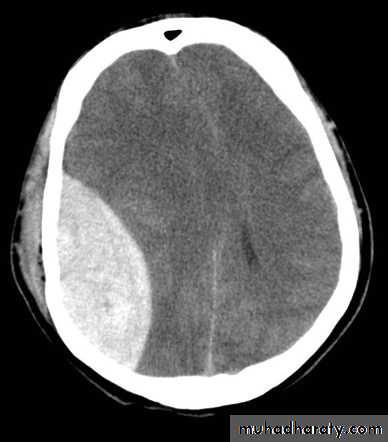
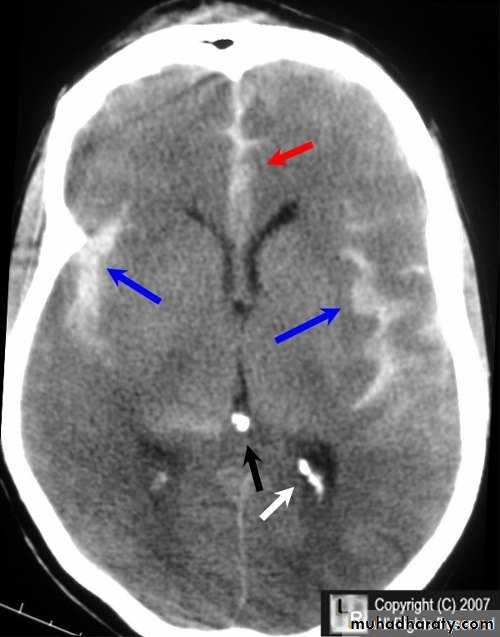
A. Extradural Hematoma:
Classically consist of a clot in the extradural space (between the bone and dura), biconvex in shape usually in the temporal area from bleeding of the middle meningeal artery (branch of maxillary artery) or its branches.25% of cases develop in other areas of brain as the frontal, parietal or posterior fossa.
Source of bleeding is usually from middle meningeal artery or its branches; sometimes from fracture site of skull, but the bleeding from an artery is usually more severe when the artery opens than that of bleeding due to fracture.
Also the source of bleeding can be venous sinuses.
Clinical features:
Classical story of minor blow on the temple, the patient will have a brief loss of consciousness due to concussion, followed by recovery then few hours later the patient will develop a throbbing headache then deteriorated level of consciousness. The period of recovery is called the "lucid period" or "lucid Interval".80% of cases there will be fracture of skull.
75% there will be amnesia to the accident, sometimes there is no lucid period, and this is called "unclassical".On Examination :
There is usually a boggy swelling (collection of hematoma at the site of injury).
There's deteroratlon of the level of consciousness and restlessness.
There'll be dilatation of the pupil on the affected side (ipsilateral) with
hemiparesis on the contralateral side.
Blood pressure will be increased and there'll be bradycardia.
Dignosis:
CT scan or MRI.On CT scan there'll be a hyperdense biconvex extradural lesion.
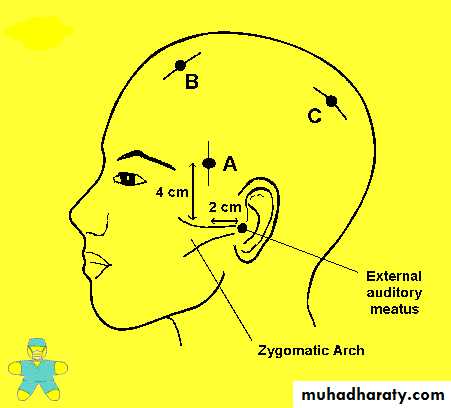
If there's no CT scan we may need to do excretory burr holes (as when we do laparotomy for the diagnosis) so in skull we make a hole, if blood comes out before reaching the dura then it is a extradural hematoma.
Treatment;
It is a top neurological emergency; we do:1. Immediate craniotomy:
We make 4 holes and match between them then we pick the bone up, evacuate hematoma, repair and replace the bone in its place. Or,
2. Craniectomy:
Also we pick the damaged bone and remove hematoma but the place stays without bone.
Prognosis:
If management is early and properly the prognosis is extremely good; if late and poorly management the prognosis is gloomy. The most important complication of surgery is recurrence.
B. Subdural Hematoma:
This is more common than extradural hematoma, the bleeder is usually venous from the bridging veins connecting the cortex to the sagittal sinus; i.e. there's direct injury to the brain.This is more serious than extradural hematoma because here, we're dealing with two problems: the mass (the hematoma} pressing on the brain, in addition to the direc damage to the brain tissue caused by the same accident that caused the bleeding.
It is divided into:
1) Acute subdural hematoma:
In the first 24 hours of the accident, the patient is unconscious in the whole course.
Diagnosis is by CT scan which will show a hyperdense mass.
Prognosis is usually bad and Treatment is by craniotomy, evacuate the hematoma, look for the bleeder and stop it thermally. Craniotomy is an obligation here because the injury is recent and the bleeder is still there, so if we do burr holes and evacuate the hematoma it may recollect again after a while.
2) Subacute subdural hematoma:
Usually 2-14 days from injury, usually suspected when head injury fail to improve at expected rate (the patient should improve after 3 days, if not then it's Subacute).Diagnosis: CT scan, it will show hyperdense or isodense lesion.
Treatment: evacuation by burr holes or craniotomy.
3) Chronic subdural hematoma:
Very common in elderly people by a minor trauma, certain brain tumors,idiopathic hypertension or decreased coagulability.
The patient usually complains of headache, apathy, personality changes, and
can be easily missed as dementia.
Diagnosis: CT scan which shows crescent shape hypodense lesion in the
subdural space.
Treatment: usually burr holes.
In acute type if we remove the hematoma, it may recur again because the cause is still there; while in chronic type the bleeder is already dosed so if we remove hematoma, there's no recurrence (here the bleeder is not active, and there's no possibility of recollection of hematoma).
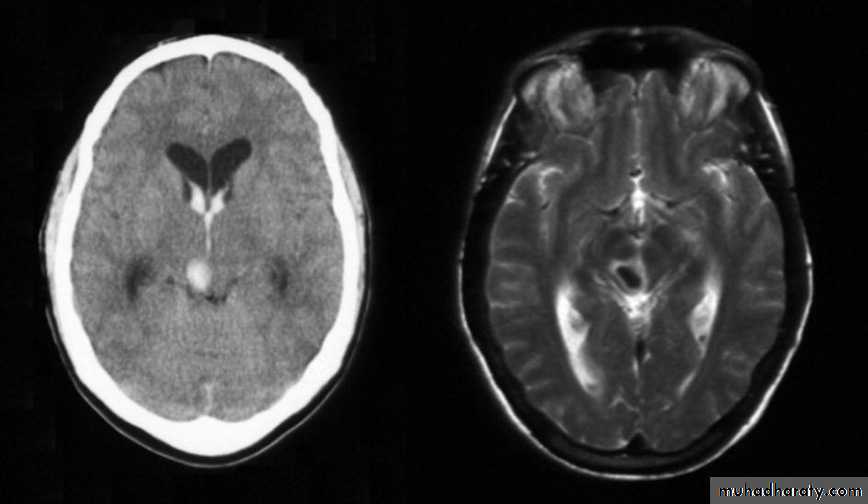
Acute subdural hematoma
Subacute subdural hematomaChronic subdural hematoma
C. Intracerebral Hemorrhage:Not very common after head injury, there may be focal signs.
Diagnosis: CT scan will show Intracerebral (parenchymal) hyperdense lesion.
Treatment: here the decision to do surgery or not is one of the most difficult decisions, because the cases are individual, there's no rule for treatment and it depends on instant decisions of the surgeon. We can't do burr holes and explore because if we do, we'll see the normal white dura mater, and we can't go punching the brain by a brain needle just to look for hematoma.
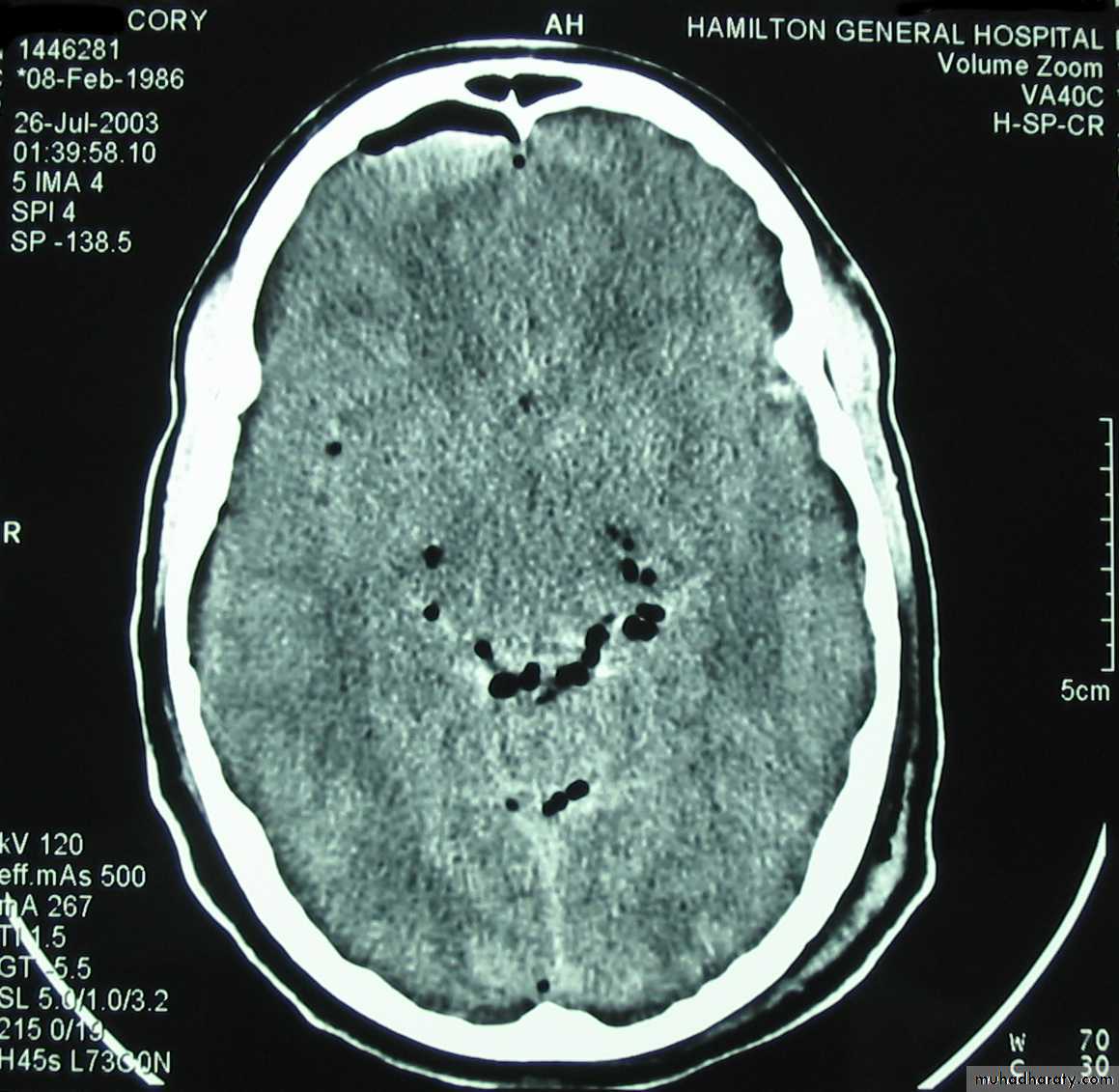
D. Intraventricular Hemorrhage:
• Blood filling ventricle (usually due to a blunt injury).• Treatment is conservative.
E. Subarachnoid Hemorrhage:
• The most common bleeding following head injury, but it's not significant.• Usually there's severe headache with meningism.
• Treatment is only analgesics.
A few drops of blood can cause severe headache so the only significance of subarachnoid hemorrhage is the severe headache (A case of severe headache following head injury is almost always subarachnoid hemorrhage).
III- Brain edema:
A frequent complication of head injury: it is an expansion of the extra vascular fluid compartment in the brain. The edema usually reaches its maximum limit after 48 hours.Bram edema can lead to increased intracranial pressure. Increased intracranial pressure can lead to Ischemia and the decreased blood supply to the brain leads to more edema due to congestion. So there will be a vicious circle until there's shooting of intracranial pressure and this will lead to cerebral herniation as an attempt to compact the increased intracranial pressure, herniation can cause serious reduction in the blood supply of the brain.
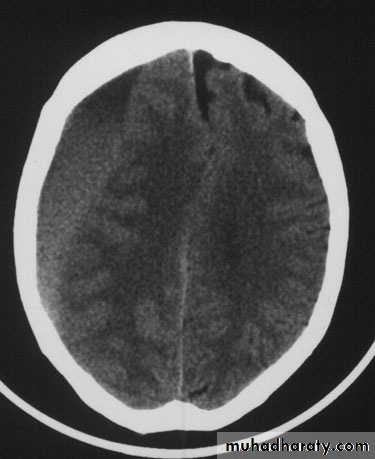
Normal brain oedematous brain
Diagnosis:Clinically by deterioration of the general condition.
CT scan will show decrease in the size of the ventricles because when
there's edema it will press the brain and lead to decrease in the ventricles
size, also there will be decrease in the density of brain tissue (the color of the
brain tissue will be slightly lighter), but these findings are usually not
significant
Diagnosis is not easy because the ventricles are already small in size, so it is almost diagnosed by exclusion of hematoma or other causes.
Management:
Diuretics: Use more than 1 type of diuretics:
Hyperosmolar diuretics as manitol (0.25 - lg/kg) in 30 min. and to be repeated every 6 hours.
Furosemtde (Lasix).
Urea, If the renal function is normal.
Hyperventilation: causes increased O2 and decreased in CO2, this will lead to vasoconstriction, and it is applied by putting the patient on ventilator.
* Hyperventilation to cause vasoconstriction (as oxygen is the best vasoconstrictor) so that we decrease the amount of blood reaching the brain without affecting oxygenation of the brain.
Steroids are not used anymore in the management of brain edema or head
Injury.
Complications:
late complication of head injury (after 2 years):1. Epilepsy.
2. Post-traumatic syndrome (neuropsychiatry manifestation)