• Movement disorder
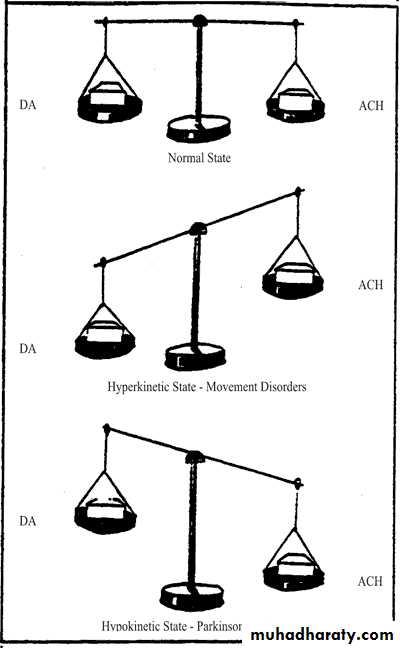
Movement disorders (sometimes called extrapyramidal disorders) impair the regulation of voluntary motor activity without directly affecting strength, sensation, or cerebellar function. They include hyperkinetic disorders associated with abnormal, involuntary movements and hypokinetic disorders characterized by poverty of movement.
hyperkinetic disorders of abnormal movements can be classified as tremor, chorea, athetosis or dystonia, ballismus, myoclonus, or tics. And examlpe of Hypokinetic is Parkinson .
Parkinson disease
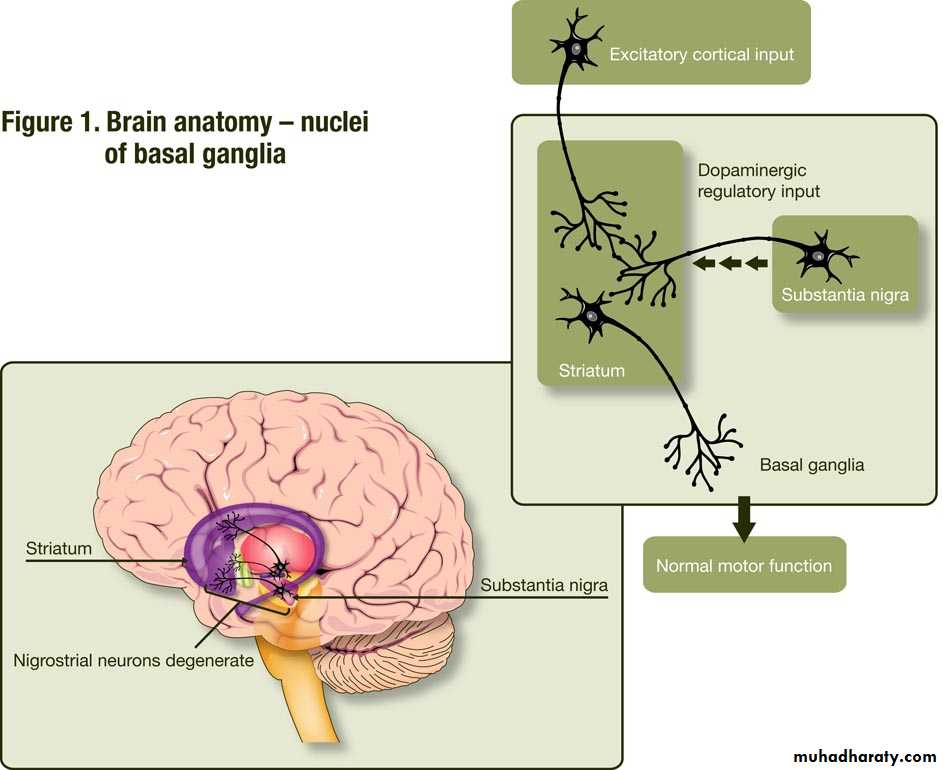
Parkinson's disease is one the commonest neurodegenerative disease. Parkinson’s disease (PD) is a neurodegenerative
disorder associated with a loss of dopamine-producing neurons in the substantia nigra.
The disease was described by James Parkinson in 1817.
PD slightly more common in men than women. The mean age of onset is about 60 years, but cases can be seen in patients in their 20s, and even younger.
Diagnosis of a parkinsonian syndrum
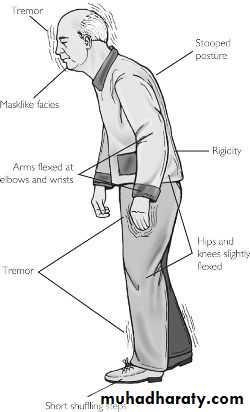
• Bradykinesia (slowness of initiation of voluntary movement with progressive reduction in speed and amplitude of repetitive actions)• Muscular rigidity
• 4–6 Hz rest tremor
• Postural instability not caused by primary visual, vestibular, cerebellar or proprioceptive dysfunction.
Other Motor Features
MicrographiaMasked facies (hypomimia)
Reduced eye blink
Soft voice (hypophonia)
Dysphagia
Freezing
Nonmotor Features
Anosmia
pain
Mood disorders (e.g. depression)
Sleep disturbances
Epidemiology and Pathologenesis
Hallmark features of PD are degeneration of dopaminergic neurons in the substantia nigra.The studies suggest that environmental factors likely play the more important role in patients older than 50 years, with genetic factors being more important in younger patients. Epidemiologic studies suggest increased risk with exposure to pesticides, rural living, and drinking well water and reduced risk with cigarette smoking and caffeine.
Differential diagnosis
Secondary ParkinsonismDrug-induced (Dopamine-blocking agents such as the Antipsychotic )
Infection
Vascular
Normal-pressure hydrocephalus
Trauma
Liver failure
Toxins (e.g., carbon monoxide, manganese, cyanide, hexane, methanol, carbon disulfide)
Other Neurodegenerative Disorders
Wilson's disease
Huntington's disease
------------------------------------------------------
Treatment of Parkinson's Disease
1- Levo DopaDopamine does not cross the blood-brain barrier (BBB), so clinical trials were initiated with levodopa, a precursor of dopamine. Levodopa is routinely administered in combination with a peripheral decarboxylase inhibitor (carbidopa or benserazide) to prevent its peripheral metabolism to dopamine and the development of nausea and vomiting levodopa is still the most potent and effective symptomatic treatment for PD, and remain the ‘gold standard’.
It is usual to start with half a tablet of 25/100 (PDI/levodopa)strength b.d. or t.d. for a couple of weeks, then doubling the dose and waiting to judge the effect over time with continued treatment, however, the duration of benefit following an individual dose becomes progressively shorter until it approaches the half-life of the drug. This loss of benefit is known as the wearing-off effect. At the same time, many patients develop dyskinesias,these tend to occur at the time of maximal clinical benefit and peak plasma concentration (peak-dose dyskinesia). In more advanced states, patients may cycle between "on" periods complicated by disabling dyskinesias and "off" periods in which they suffer severe parkinsonism.
Strategies to Treat Motor Fluctuations
(1) Increase LD/CD from 3 to 4 times daily(2) Substitute sustained release LD/CD
(3) Add dopamine agonist
(4) Add COMT inhibitor
• End-of-Dose Deterioration
• Add sustained-release LD/CD at bedtime
(2) Add dopamine agonist at bedtime• at night ‘‘Off ’’ Dystonia
(1) Smaller doses of levodopa taken more frequently
(2) Add dopamine agonist, decrease levodopa
(3) Add amantadine
Peak-Dose Dyskinesia
• 2-Dopamine agonists
• Dopamine agonists stimulate dopamine receptors directly. Six oral agonists (bromocriptine, lisuride, pergolide , cabergoline,ropinirole and pramipexole) ,one transdermal agonist (rotigotine) and Apomorphine administered SC are available,thsese agonist may given before levodopa is introduced especially in young age , these drugs cause fluctuations and dyskinesias much less frequently.,
3- Catechol-O-methyl transferase (COMT) inhibitors
Entacapone (peripheral) and tolcapone (peripheral and central COMT inhibitor) block the conversion of levodopa to 3-O-methyldopa, its principal metabolite so increase the duration effect of levodopa.A combined tablet containing levodopa, carbidopa and entacapone (Stalevo) is available.
• 4-Monoamine oxidase B (MAO-B) inhibitors
Selegiline and rasagiline are inhibitors of MAO-B, the iso-enzyme (MAO-B) responsible for catabolizing dopamine to homovanillic acid (HVA).lead to increase the duration effect of levodopa.5-Anticholinergics
Anticholinergics often restricted to reducing tremor. eg. trihexyphynidyl ,procyclidin .6-Amantadine
This drug has several actions: an amphetamine-like effect (releasing presynaptic dopamine stores); a mild anticholinergic effect.Surgery for PD
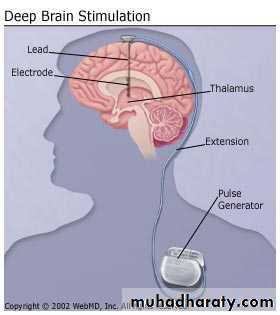
it was appreciated that lesions placed into the nucleus of the thalamus reduced contralateral tremor without inducing hemiparesis, but these lesions did not meaningfully help other more disabling features of PD. Lesions placed in the GPi (globus palidus interna) improved rigidity and bradykinesia as well as tremorDeep brain stimulation (DBS)
Most surgical procedures for PD performed today utilize deep brain stimulation (DBS). Here, an electrode is placed into the target area and connected to a stimulator inserted SC over the chest wall. DBS simulates the effects of a lesion without necessitating a brain lesion, Stimulation of thalamus lead to decrease tremor ,stimulation of Globus Pallidus Interna lead to decrease rigidity and bradykinesia.
• TREMOR
• A tremor is a rhythmic oscillatory movement best characterized by its relationship to voluntary motor activity, i.e., according to whether it occurs at rest, during maintenance of a particular posture, or during movement so tremor can be classified to: rest and action tremor• Action tremor is classified into:
• postural tremor
• intention tremor
Action tremor
1-Postural tremorPhysiologic tremor
Enhanced physiologic tremor causes are:
Anxiety or fear
Excessive physical activity or sleep deprivation
Sedative drug or alcohol withdrawal
Drug toxicity (lithium, bronchodilators, sodium valproate, tricyclic anti depressants)
Thyrotoxicosis
Carbon monoxide poisoning
Familial (autosomal dominant) or idiopathic (benign essential) tremor
Wilson disease
Asterixis
2-Intention tremor
Cerebellar disorders
Wilson disease
Drug toxicity (e.g., alcohol, anticonvulsants, sedatives)
Rest tremor
ParkinsonismWilson disease
---------------------------------------------
PHYSIOLOGIC TREMORAn 8- to 12-Hz tremor of the outstretched hands is a normal finding. Its physiologic basis is uncertain.
• ENHANCED PHYSIOLOGIC TREMOR
Physiologic tremor may be enhanced by fear or anxiety. A more conspicuous postural tremor may also be found following excessive physical activity or sleep deprivation and other causes mentioned above.Benign essential tremor
This is commonly inherited as an autosomal dominant trait.
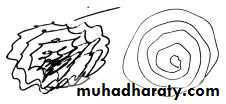
Most people with essential tremor (ET) have little or no disability ET is a 4-Hz to 12-Hz postural tremor, typically seen as adduction-abduction of the fingers or flexion-extension of the wrist; pronation-supination of the wrist can occur, but it is more typical of PD. The tremor may start on one side, but as a rule it becomes bilateral with time. The handwriting remains large (unlike PD) but may often be severely affected and illegible. The head is the next most frequent area to be affected, with a vertical ‘‘yes-yes’’ or horizontal ‘‘no-no’’
tremor. The voice, tongue, and chin may all be involved as well.
Criteria of essential tremor
Core Criteria
Bilateral action tremor of the hands and forearms (not rest tremor)
Absence of other neurologic signs
May have isolated head tremor
Secondary Criteria
Long duration (>3 years)
Positive family history
Beneficial response to alcohol
• Treatment
• Propranolol• About 50% of patients will experience relief with propranolol and other B-adrenergic antagonists. Doses generally are rather large, with optimal response in the 240 mg to 320 mg range.
• Primidone
• Because the main side effect of primidone is sedation, it should be started at 25 mg at bedtime and increased very slowly by 25-mg increments. If needed, a low dose may be added in the morning. Doses above 250 mg to 350 mg are rarely needed.
• Topiramate
• have suggested some improvement in ET
• Surgical treatment
• Stereotactic lesioning of the ventral intermediate• nucleus (VIM) of the thalamus has produced the greatest response in patients with severe tremor.
• deep brain stimulation (DBS) of the VIM nucleus of the thalamus , has become the surgical procedure of choice
Befor treatment After treatment