The Specific Immune Response
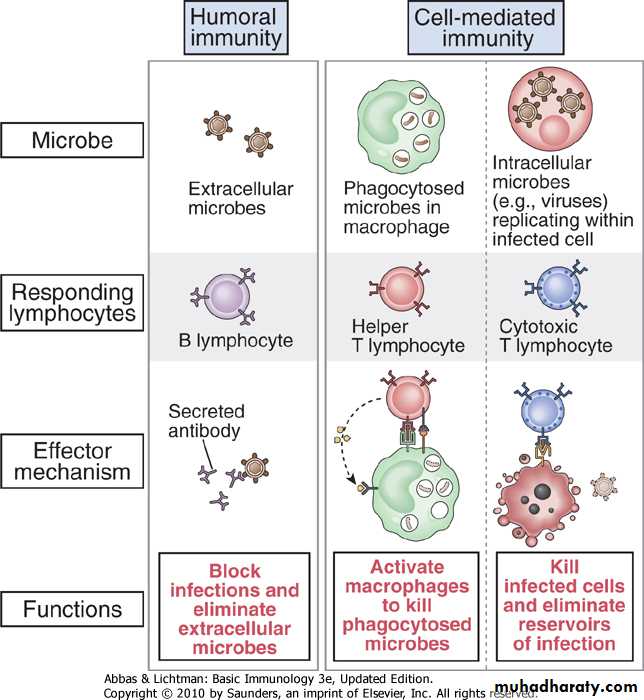
Overview of the specific (adaptive) immune response - continue1. Cell Mediated Immunity ( T cell mediated immunty)
Key players : T lymphocytes. Two types:Cytotoxic T cells (CTL) or (CD8+)
T helpers ( TH) cells (CD4+)
- Cytotoxic T cell directly attack and destroy antigen-bearing cells especialy
virally infected cells and tumours
- Helper T cells act indirectly by secreting proteins called cytokines that
activate other cells such as macrophages to destroy the antigen-bearingcells
- Particularly useful in eradicating pathogenic bacteria especially
intracellular bacteria
Can you give some examples for intracellular bacteria????
• Act indirectly by secreting chemical mediators called cytokines that
Activate other cells such as macrophages to destroy the antigen-bearing cells- Activated macrophages can then kill intracellular pathogens that would
normally divide in a non-activated macrophage
- Activated macrophages also kill foreign mammalian cells
(tissue transplantation) and in some cases tumor cells (haveSpecific antigens that are not found on normal cells)
Cellular immune response by TH cells (CD4+)
1st step : foreign antigen will be captured and engulfed by the phagocytes (macrophages) and another cell type called dendritic cells at the site of infection
• (internalization)
• - What are dendritic cells?
Mechanism of cellular immune response by TH cells (CD4+)Dendritic Cells
Named so because they resemble dendrites of neurons
• (THEY ARE NOT NEURONS!!!)
Their main fucntion is to capture , concentrate and present antigens to lympnocytes ( APC)
Origin : stem cells in bone marrow
Several Type
• Langerhans (LC) found in skin
• Circuilating DCs
• Myeloid (MDC1 and MDC2)
• Plasmacytoid
• Interstitial DCs
• Heart, lungs, liver, intestines
• Interdigitating DCs, T-cell areas of lymph nodes and Thymic medulla
•
Mechanism of cellular immune response by TH cells (CD4+)
Next , internalized antigen is processed inside the macrophages and dendritic cells where the antigen is degraded and fragment of it binds to MHC class II molecule(Major Histocompatibility Class I I molecule)
Major Histocompatibility complex proteins are found on the surface of cells:: T cells cannot recognize foreign antigens unless they are associated with these MHC proteins
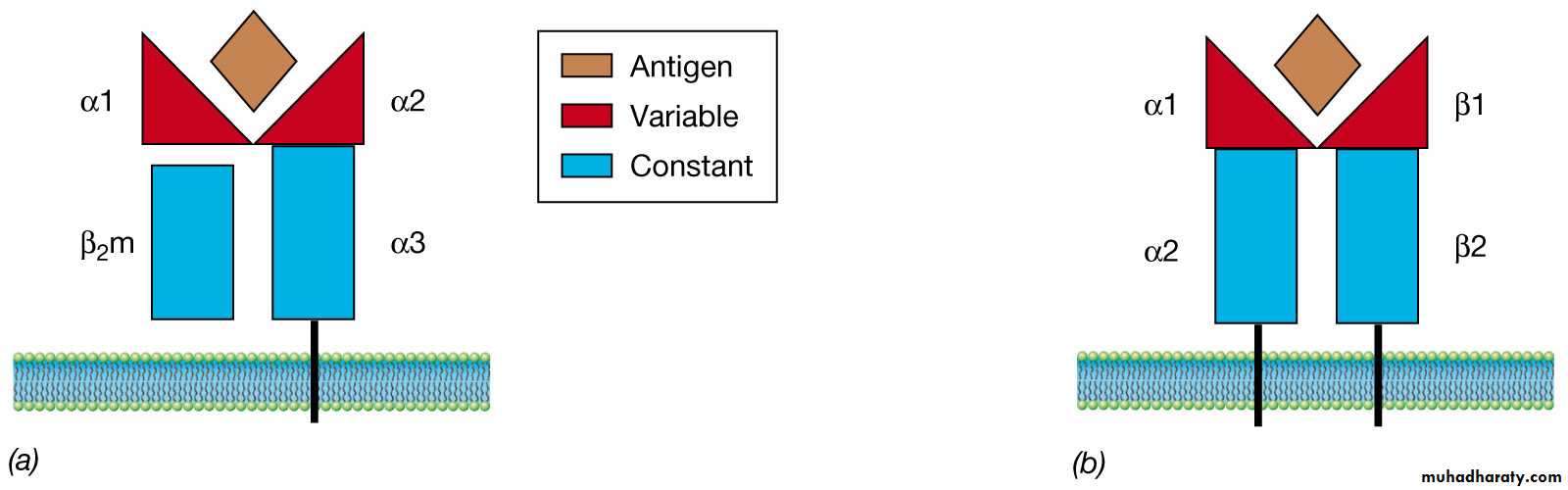
Class I MHC proteins are
found on the surface of ALL
nucleated cells
Class II MHC proteins are only
found on the surface of
B lymphocytes, macrophages
and other antigen presenting cells
ALL MHC proteins are imbedded in the cytoplasmic membrane of
cells and project outward from the cell surface
THEN , the processed antigens bind to Class I I
• (Ag-MHC class II complex ) are transported to the cell surface where they expressed.- The macrophages and dendritic cells now move toward regional lymph nodes under the influence of certain chemical substances (chemotaxis)
Mechanism of cellular immune response by TH cells (CD4+)
In the regional lymph nodes the phagocytes and dendritic cells present the antigen in association with MHC class II molecule to CD4+lymphocytes.
That is why macrophages and dendritic cells are called antigen presenting cells (APC).
Mechanism of cellular immune response by TH cells (CD4+)Class II MHC proteins and helper T cells (TH)
The Class II proteins and antigenare expressed on B cells, APCs
and macrophages
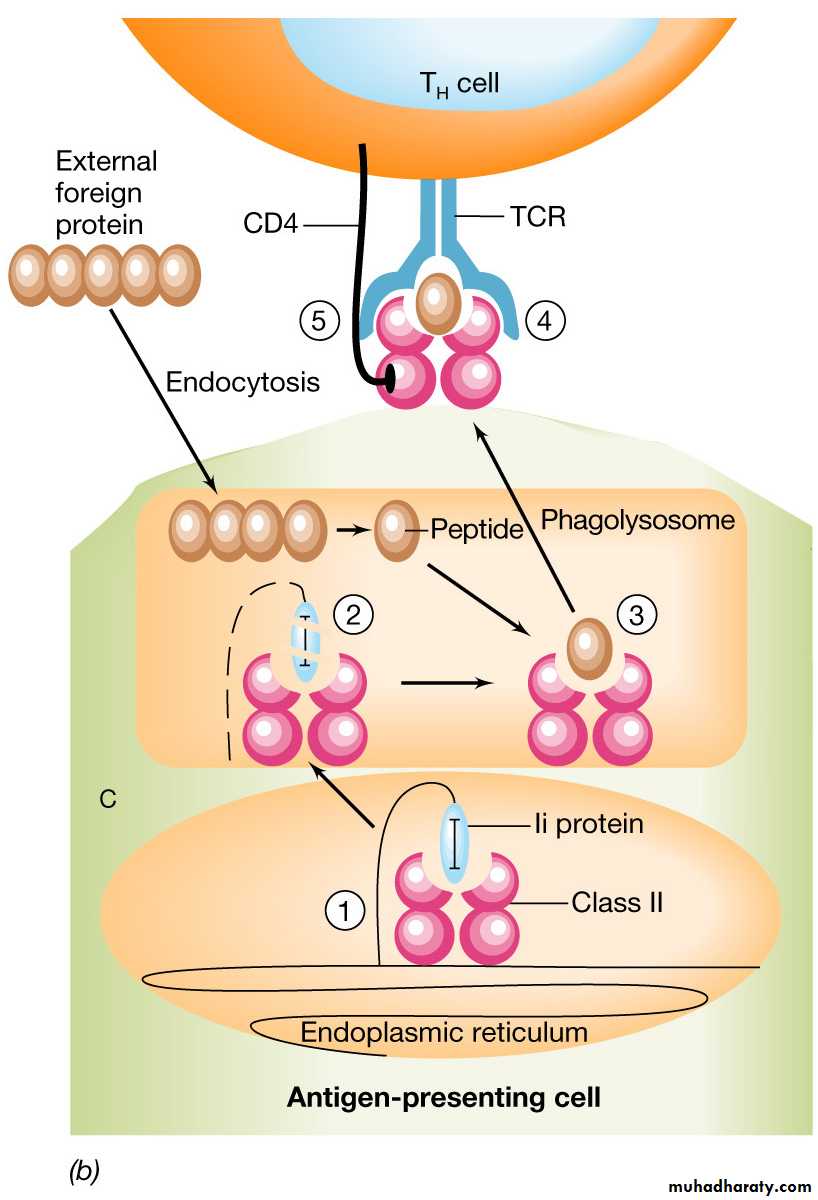
1. The APC takes up an external foreign
protein via phagocytosis or endocytosis
2. Class II proteins are produced in the
endoplasmic reticulum and assembled
with a blocking protein (Ii) or invarient
chain
3. The Class II proteins enter the
phagolysosome where the Ii is degraded
and the partially processed antigen
binds to the class II molecule
4. The complex is translocated to the
surface of the APC where it interacts
with the TCR of a T helper cell
The part of the CD4+ that comes in contact with the antigen - MHC class II complex is called TCR (T Cell Receptor).
Cell- cell interaction mediated by TCR (from CD4+ T lymphocytes) and antigen - MHC class II complex (from macrophages or dendritic cells) will activate TH CD4 + to produce chemical mediators called cytokines (hormones of the immune system) :
• Interferon - gamma ( IFN- gamma)
• Tumour necrosis factor - alpha (TNF-alpha)
• Granulocyte monocyte- colony stimulating factor (GM-CSF)
Mechanism of cellular immune response by TH cells (CD4+)
Mechanism of cellular immune response by TH cells (CD4+)These cytokines further stimulate macrophages to increase phagocytic activity and to in turn produce cytokines that promote inflammation
Class II MHC proteins and helper T cells (TH)
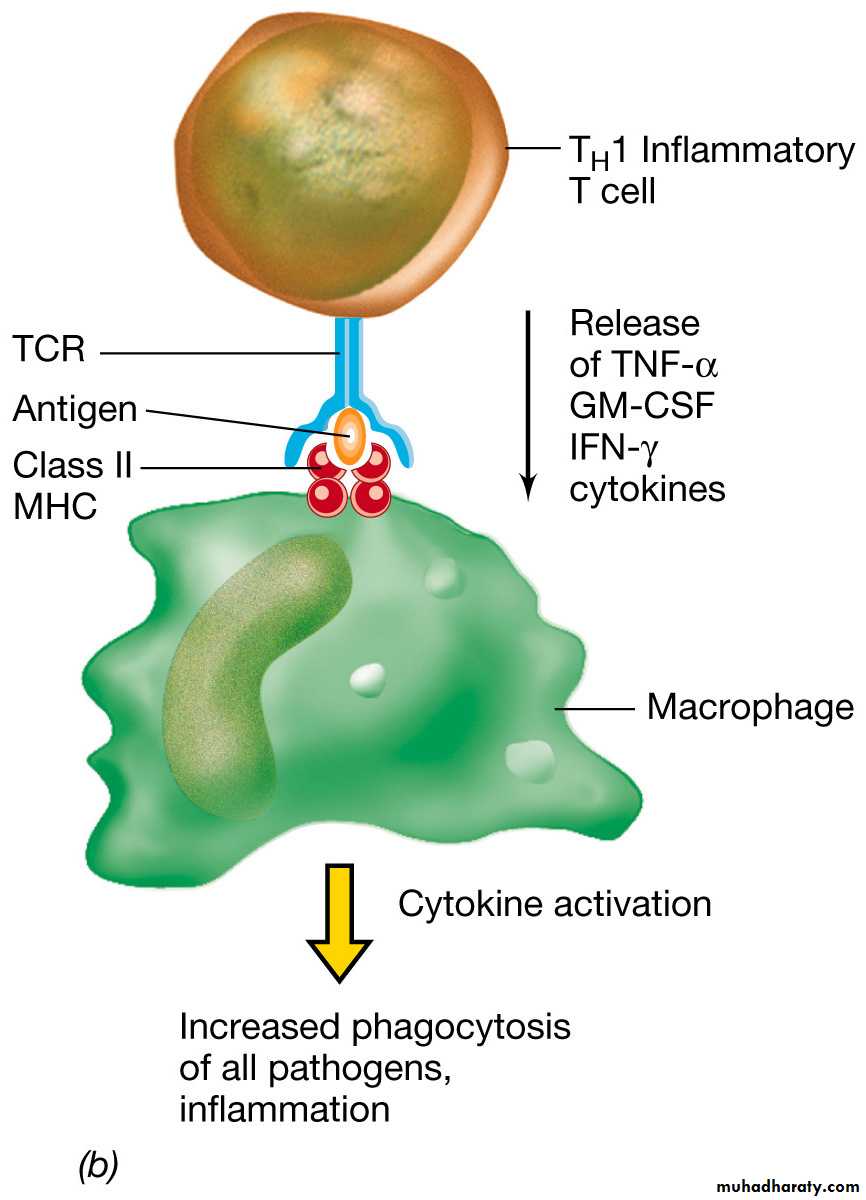
Specialized TH cell involved inthe inflammatory response
Cell-cell interaction mediated
by the TCR and the class IIMHC-antigen complex activates
The TH cell which produces
cytokines
TNF-alpha (tumor necrosis factor)
IFN-gamma (interferon)
GM-CSF (granulocyte-monocyte
colony stimulating factor)
These cytokines further stimulate
macrophages to increase phagocytic
activity and to in turn produce cytokines
that promote inflammation
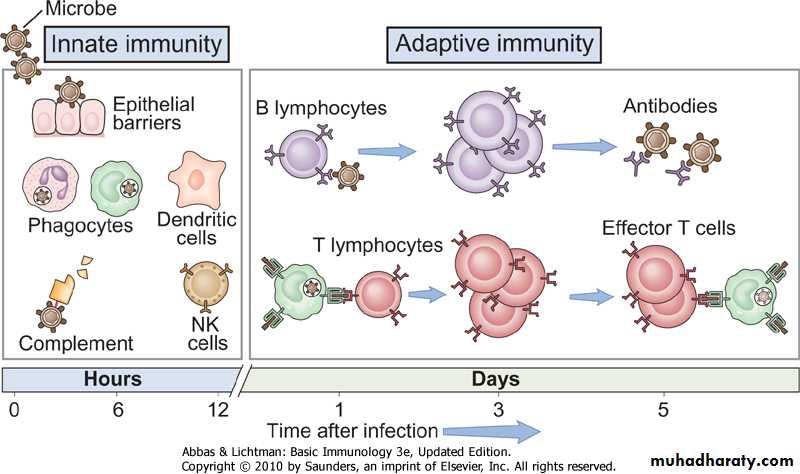
Types of Specific (adaptive) immunity
Humoral immunityCellular immunity
Specific immune response - humoral immunity
B cell mediated immunity through the production of antibodies.Particularly effective against pathogens such as viruses and extracellular bacteria in the blood or lymph and also against soluble pathogen products such toxins
B - lymphocytes
+
=
Humoral immunity
Antibodies
Humoral immunity: B- Lymphocytes
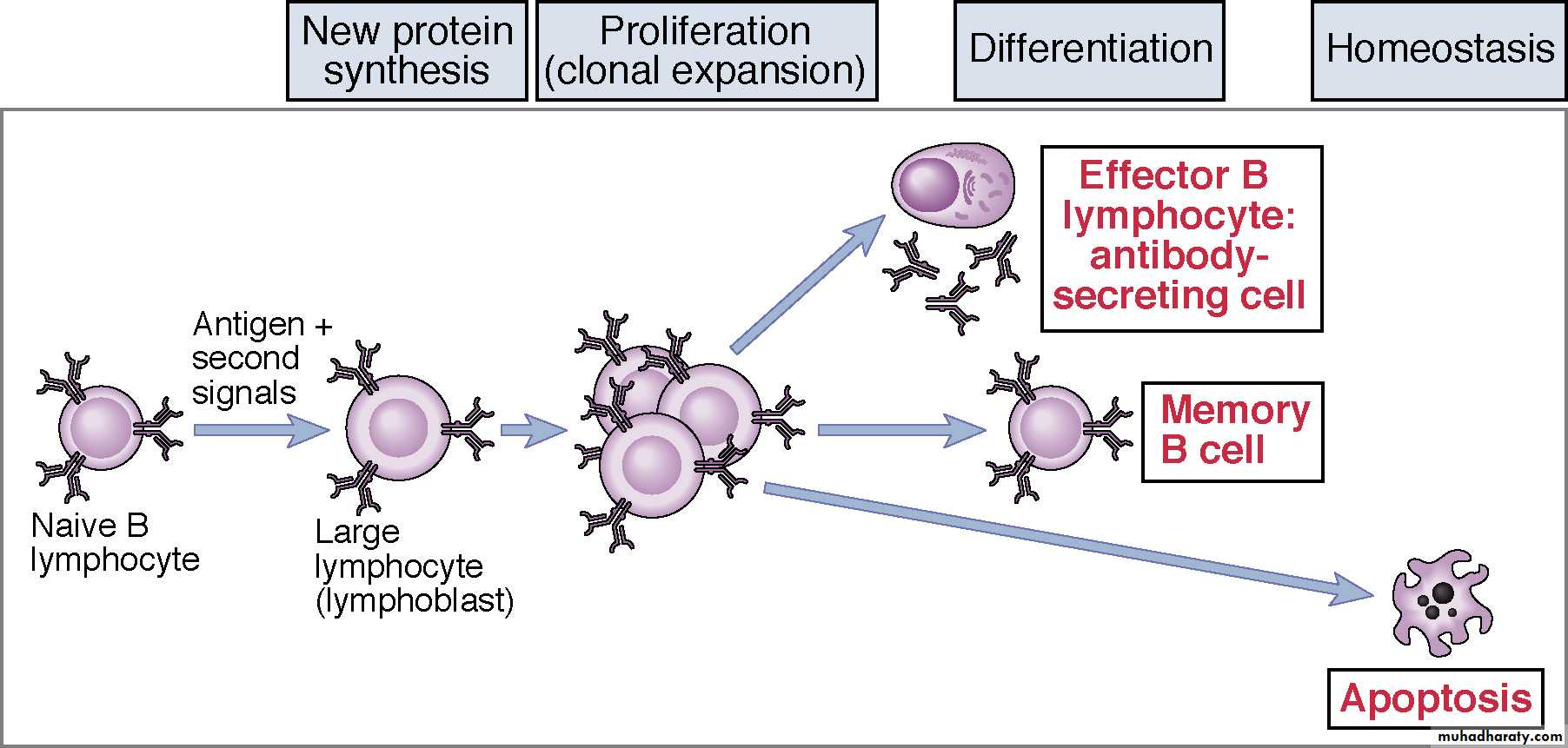
Origin and Maturation: Bone marrow• - B- lymphocytes from the bone marrow are released into circulation in a resting state and they do not secrete antibodies
• - Instead, resting B-lymphocytes display membrane bound antibodies (immunoglobulins) usually in the form of mIgD or mIgM
• - After activation by antigen, B- lymphocyte divides ( clonal expansion)
• . Some differentiated into plasma cells which secrete antibodies, die within 1- 2 weeks.
• . Some change into memory cells- display same membrane bound antibodies as parent cell.
Phases of B-lymphocyte activation
Antigen
Mechanism of humoral immune response by B - lymphocytesResting B - lymphocyte is coated with membrane bound antibodies or immunoglobulin (mIg) on the surface of the lymphocytes
The first step in the initiation of the humoral immune response is the binding of the antigen to the mIg
Resting B - lymphocyte
+
mIg
Antigens
B - lymphocyteMechanism of humoral immune response by B - lymphocytes
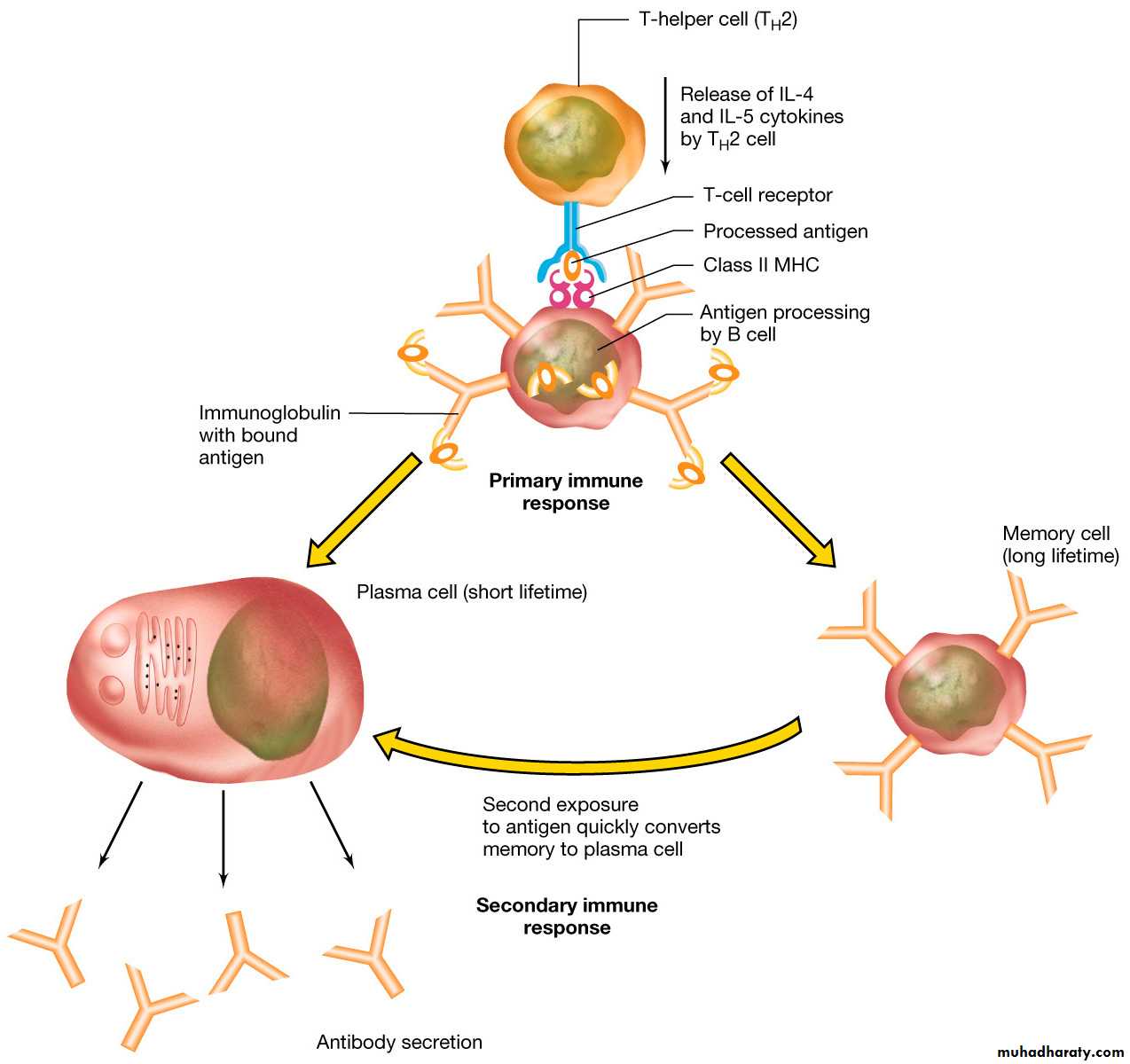
The mIg- antigen complex is then endocytosed and complexed with MHC class II molecule and then surface expressedHere , B - lymphocyte acts as APC where it presents the antigen-MHC class II complex to TH cells
Now, TH cells start to secrete cytokines ( IL-4 and IL-5) that stimulate B-lymphocyte to divide (clonal expansion) and differentiate into plasma cells
• (1 B cell --> 4,000 Ab-secreting cells --> ~1012 antibody molecules/hour)
Mechanism of humoral immune response by B - lymphocytes
Plasma cells start to secrete antibodies (short half life, die in 1-2 weeks).Some dividing B- lymphocytes change into memory cells where they display same mIg as parent B- cell and change rapidly into plsama cells when encountering same antigen for second time (secondary immune response.
Primary immune response is usually mediated by IgM while the secondary immune response is stronger and mediated by IgG.
Note : In secondary immune response , memory cells conver timmediately to plasma cells and produce IgG in high amounts without the aid of helper T cells
Class II MHC proteins, helper T cells that stimulate antibody producing cells—the B cells
B cells are coated with
antibodies that react with
specific antigens
When the antigen binds to the
antibody, the B cell first acts
as an APC.
The bound antigen is endo
cytosed and complexed with
MHC II and then surface
expressed
The surface
expressed complex
interacts with and
activates TH cells that produce
the cytokines interleukin 4 & 5
IL4 and 5 stimulates the B cells to produce
identical memory B cells and antibody
secreting plasma cells that secrete the
same antibody
Secific immune response-Summary
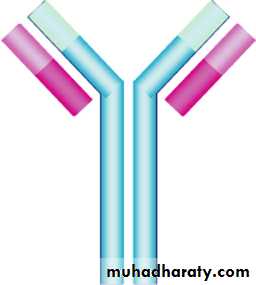
Antibody (Immunoglobulin) Structure
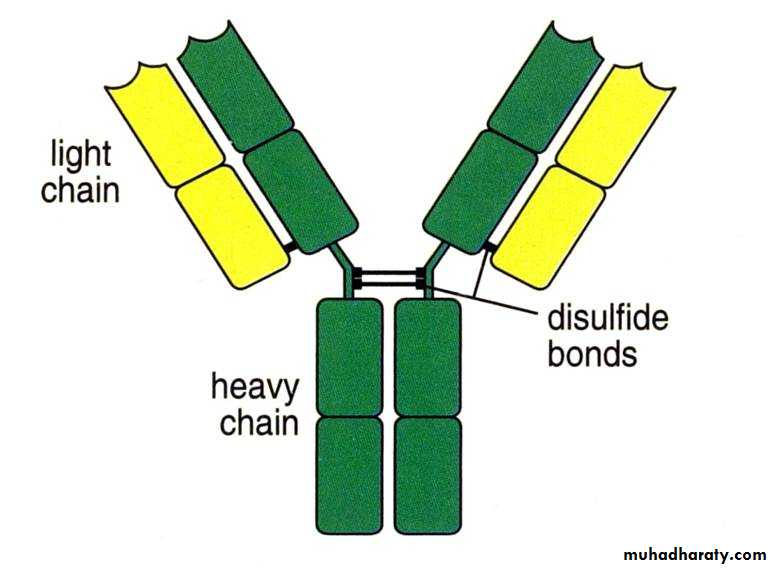
5 classes: IgG, IgM,IgA, IgD and IgECommon structure , four polypeptide chains:
• - Two identical heavy (H) chains, each carrying covalently attached oligosaccharide groups (50-70 kDa)
• - Two identical, non-glycosylated light
• (L) chains (23kDa)
Within the immunoglobulin, disulphide bonds join together:
• - Two heavy chains
• - Heavy chains to the light chains
The disulphide bonds joining the antibody heavy chains are located in a flexible region of the heavy chain known as the hinge region.
•
Heavy chain determines the Ig class:
IgG : gamma HCIgA: alpha HC
IgD: delta HC
IgM: mu HC
IgE:epsilon HC
Light chain either kappa or lambda irrespetive of Ig class
Antibody (Immunoglobulin) Structure
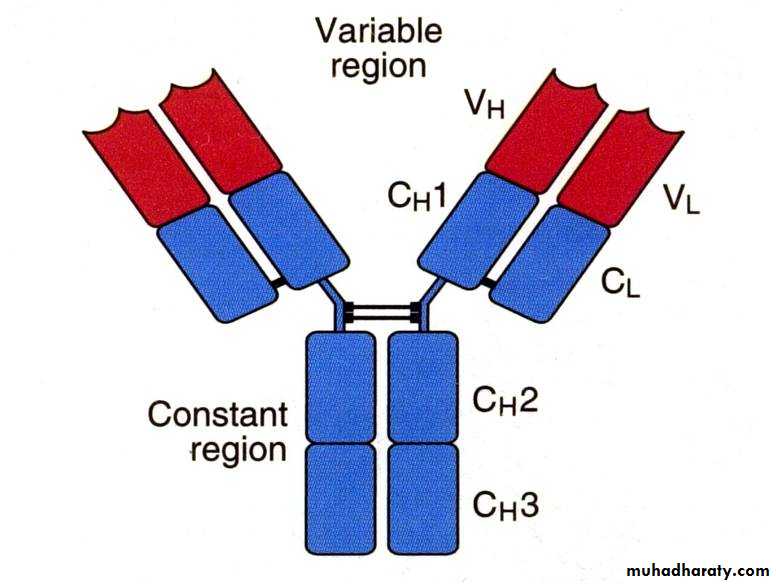
Based on variability of amino acid sequences, both H and L chains can be divided into:
• - VH and CH domains(variable and constant)
• - VL and CL domains (vaiable and constant)
The variable domains are attached to the constant domains.
As the name implies, the variable domains vary in their amino acid sequence from one antibody molecule to another, providing the vast diversity the immune system needs to fight foreign invaders.
The antigen binding site is formed where a heavy chain variable domain (VH) and a light chain variable domain (VL) come close together. These parts show the biggest difference among different antibodies.
Antigen binding site
Proteolytic treatment of Ig with protease enzymesWhen the immunoglobulin is treated with proteolytic enzymes (proteases), such as pepsin or papain, it is broken at the hinge region into two fragments known as Fab
• (Fragment for antigen binding) and Fc
• (Fragment Crystalizable).
The immunoglobulin specifity is determined by the Fab fragment, as well as its capability to react with the antigen.
(Fc) cannot bind with antigens, but is responsible for biological effector functions like complement fixation, binding to macrophages, natural killer cells and neutrophils.
IgG
IgM
IgA
IgD
IgE
Structure
Monomer
Pentamer
Dimer
Monomer
Monomer
Serum %
80%
5-10%
10-15%
0.2%
0.002%
Location
Blood,lymph,intestine
Blood,lymph,B cells as monomer
Secretions( tears, milk), blood,lymph
Blood, lymph, B cells
Mast cells , basophils,blood
Placenta transfer
Yes
No
No
No
No
Complement fixation
Yes
Yes
No
No
No
Function
Neutralize viruses and toxins, enhance phagocytosis, protect fetus
1ry immune response
Localized protection on mucous surfaces
Serum function not known,initiation of immune response on B cells
Allergic reaction and lysis of parasitic worms
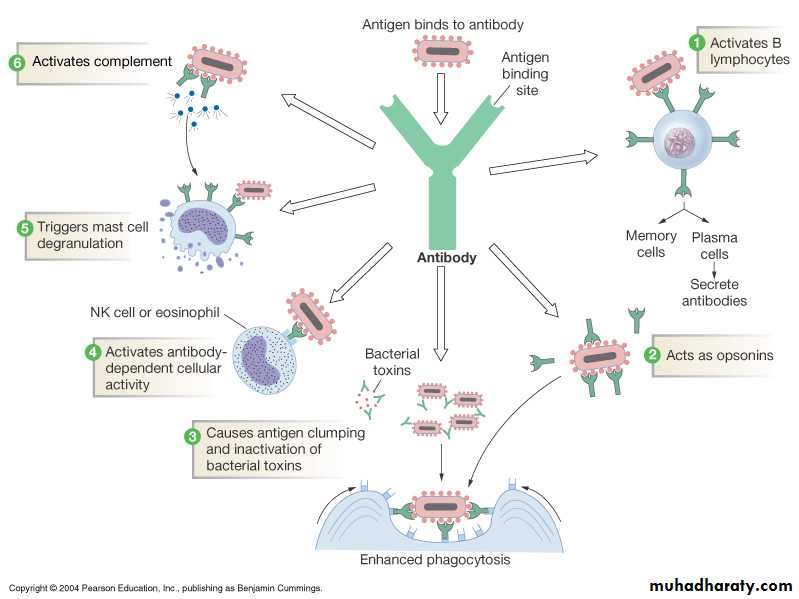
Antibody (Immunoglobulin) functions
• 1. mIgs activate B- lymphocytes when comes in contact with antigen
• 2. Secreted Ig neutralizes the effect of viruses , extracellular bacteria and toxins
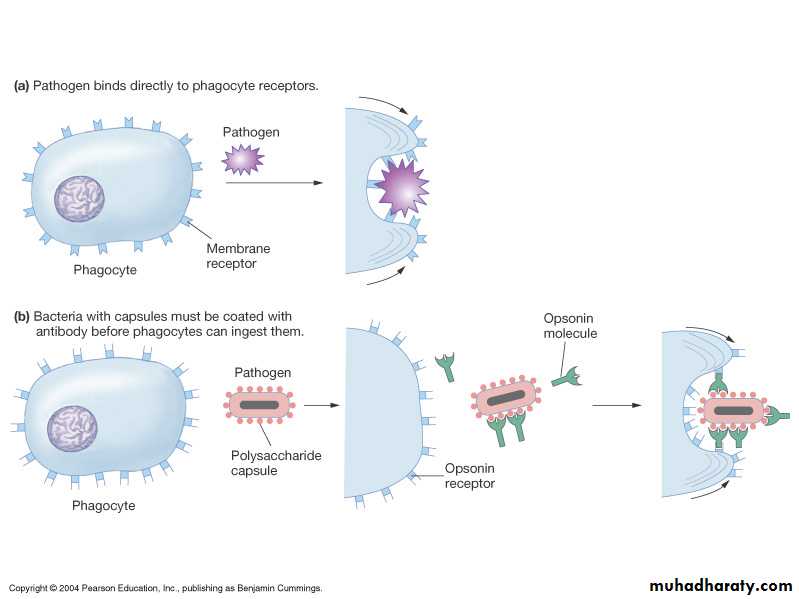
• 3. Opsonization: bind pathogens for recognition by other immune cells (e.g. phagocytes)
• Opsonins- are the tagging proteins that make unrecognizable particles into “food” for phagocytes.
Antibody (Immunoglobulin) functions
Antibody (Immunoglobulin) functions• 4. Mast cell degranulation:
Mast cells contain histamine in intracellular granules
Binding of IgE to cell surface receptors on a mast cell primes the cell to respond to allergen
Introduction of allergen and its subsequent binding to IgE stimulates the mast cell to degranulate and release of histamine
Mast cell
+IgE
Mast cell
Mast cell
AntigensAntibody (Immunoglobulin) functions
• 5- Antibody dependant-cellular cytotoxicity (ADCC)• - Classically mediated by NK, but also by eosinophils and neutrophils
• - Part of the adaptive immune response (depend on antibodies)
Antibodies bind antigen on the surface of target cells
NK ells express CD16, a receptor for Fc , recognize cell bound antibodies
Relese of perofrins and granzymes by NK ells
Cell death
Antibody (Immunoglobulin) functions
• 6. Complement activation
• Will be discussed in details in next lecture
Monoclonal Vs polyclonal antibodies
• Polyclonal antibody• Multiple clones from multiple B - lymphocytes each of which recognizes different epitope on same antigen
Antigen
B-lymphocyte
B-lymphocyteB-lymphocyte
Monoclonal Vs polyclonal antibodies
• Monoclonal antibody• Single clone from single B - lymphocyte recognizes single specific epitope on antigen
Antigen