Dental caries
Dental caries can be defined as demineralization of the tooth surface caused by bacteria. The term dental caries is used to describe the results of a localized chemical dissolution of the tooth surface caused by metabolic events taking place in the biofilm (dental plaque) covering the affected area. The destruction can affect enamel, dentin and cementum.Dental caries lesions may develop at any tooth site in the oral cavity where a biofilm (Dental plaque) develops and remains for a period of time.
The dissolution (demineralization) when pH drops below a certain level in the biofilm (Dental plaque) and the redeposition (remineralization) of minerals when pH goes up take place in the enamel surface at the interface between the biofilm and the tooth surface. These processes occur numerous times during a day and can be modified extensively.
Dental plaque
Dental plaque is an adherent deposit of bacteria and their products, which forms on all tooth surfaces and cause caries.
Dental plaque is (biofilm) community of microorganisms attached to a surface. The organisms are organized into a three-dimensional structure enclosed in a matrix of extracellular material.
Dental plaque formation can be described as:
1- Formation of pellicle: an acellular, film, derived from saliva, which forms on a tooth surface.
2- Within 4 hours, single bacterial cells colonize the pellicle. A large proportion of these are streptococci There are also Acintomyces species and Gram-negative bacteria.
Only about 2% of the initial streptococci are mutans streptococci.
3- next 24 hours formation of distinct microcolonies.
4- In 14 days the Streptococcus-dominated plaque changes to a plaque dominated by Actinomyces. Thus the population shifts; this is called microbial succession.
5- In 2weeks the plaque is mature but there are considerable site-to-site variations in its composition.
Factor that influences the metabolic processes:
1-the composition and thickness of the biofilm(Dental plaque).
2-the salivary secretion rate and composition .
3-the diet .
4-fluoride ion concentration in the oral fluids .
Enamel and dentine structure
Enamel consists of crystals of hydroxyapatite packed tightly together in an orderly arrangement (the enamel prisms). enamel has a glass-like appearance and it is translucent, allowing the colour of the dentine to shine through it. Even though crystal packing is very tight, each crystal is actually separated from its neighbours by tiny intercrystalline spaces or pores. These spaces are filled with water and organic material. When enamel is exposed to acids produced in the microbial biofilm, mineral is removed from the surface of the crystal which shrinks in size. Thus, the intercrystalline spaces enlarge and the tissue becomes more porous. This increase in porosity can be seen clinically as a white spot.
Dentine is a vital tissue permeated by tubules containing the cell processes of the odontoblasts. This vital tissue defends itself from any assault, such as caries, by tubular sclerosis. This is the deposition of mineral along and within the dentinal tubules resulting in their gradual occlusion. In addition, the odontoblasts form tertiary dentine at the pulp–dentine border in response to the stimulus.
histological changes in enamel before cavitation (white spot dental caries lesion).
1-Surface zone.
2-body of lesion.
3-dark zone.
4-translucent zone.
The shape of dental caries lesion in enamel
1- smooth surface: the lesion is classically triangular in shape. It follows the direction of the enamel prisms. The shape of the lesion and the activity of the lesion entirely reflect the specific environmental conditions of the overlying biofilm.2-Occlusally: purely because of the sloping fissure walls and the direction of the enamel prisms, the lesion assumes an undermining character. This explains why in the more advanced lesion, where there appears to be a small hole in the tooth, something apparently so small on the surface can be so large when entered with a burr . Once a cavity forms on this surface it is narrower at the top than at the base.
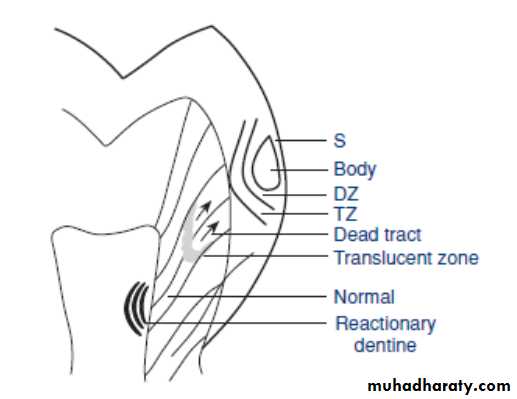
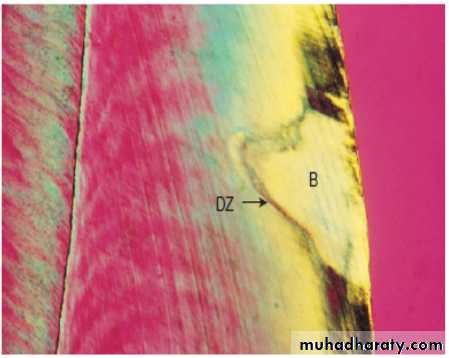
histological changes in dentine
The dentine has been reacting to the carious process in the biofilm(dental plaque)long before a cavity forms. Dentine is a vital tissue, permeated by the tubules containing the cell processes of the odontoblasts, and it defends itself by the tubular sclerosis within the dentine and the formation of tertiary dentine (also called reactionary dentine or reparative dentine) at the pulp-dentine border.Tubular sclerosis is the deposition of mineral within the dentinal tubules and it requires the presence of a vital odontoblast. It can be seen in the light microscope where a traverse through the centre of the enamel lesion crosses the enamel–dentine junction. The enamel demineralization has increased the enamel porosity and permeability and this dentine reaction corresponds to the most porous part of the enamel lesion, which in turn corresponds to the activity of the biofilm .
When contact between the enamel lesion and the enamel–dentine junction is established, the first sign of dentine demineralization can be seen along the junction as a brownish discolouration within the contact area of the enamel lesion and the junction. Demineralization of outer dentine is now surrounded by sclerotic reactions corresponding to the less advanced peripheral parts of the enamel lesion.
Dentine changes in cavitated lesion
1-the zone of destruction: following exposure of dentine to the mass of bacteria in the cavity, the most superficial part of the dentine is decomposed by the action of acids and proteolytic microorganisms.2-the zone of penetration: tubular invasion of bacteria is frequently seen beneath the first zone.
3- Area of demineralized: dentine which does not yet contain bacteria .
4- Dead tracts : the odontoblast processes have been destroyed without producing tubular sclerosis.
5-liquefaction foci: tubules are invaded by bacteria and groups of tubules coalesce.
6-transverse clefts: destruction may also advance along the incremental lines of growth which are at right angles to the tubules.
The defence reactions of tubular sclerosis and tertiary dentine formation continue as a response to these destructive processes. Both processes reduce the permeability of the dentine, although tertiary dentine is less well mineralized than primary or secondary dentine and contains irregular dentinal tubules.
Caries lesions can be classified according to their anatomical site.
1-pits and fissures.2-smooth surfaces.
lesions may start on enamel (enamel caries) or on the exposed root cementum and dentin (root caries).
Caries lesions may also be classified to:
1-Primary caries
Which is caries on natural, intact tooth surfaces.
2-recurrent or secondary caries
Which define as a lesion developing at a tooth surface adjacent to a filling , its etiology is similar to that of primary caries.
3-Residual caries
Which is demineralized tissue that has been left behind before a filling is placed.
Another Classification of dental caries
1- cavitated lesion .
2- non-cavitated.
classification according to their activity
1-active caries lesion.
A lesion considered to be progressing .
2-arrested caries lesions or inactive caries lesions.
lesions that may have formed years previously and then stopped further progression.
the clinical distinction between active and inactive (arrested) lesions is sometimes difficult.
white-spot, early, initial or incipient caries
Definition of incipient is ‘beginning’; an initial stage. In other words, an initial lesion appears as a white, opaque change (a white spot). carious lesion on enamel that can be detected with the naked eye.Root-surface caries
Active lesions were described as soft or leathery and were usually found at plaque-retention sites next to the gingival margin or along the cement-enamel junction. Inactive lesions were typically located at some distance from the gingival margin, felt hard on gentle probing and often presented with a shiny appearance.
Rampant caries
The name given to multiple active carious lesions occurring in the same patient. This frequently involves surfaces of teeth that do not usually experience dental caries. These patients with rampant caries can be classified :
bottle or nursing caries.
early childhood caries.
radiation caries or drug-induced caries.
Hidden caries
A term used to describe lesions in dentin that are missed on a visual examination but are largeenough and demineralized enough to be detected radio graphically.
Why do we diagnose caries?
1- detecting and excluding disease
2- assessing prognosis
3- contributing to the decision-making process with regard to further diagnostic and therapeutic management
4-informing the patient
5- monitoring the clinical course of the disease.
diagnostic classifications
1-Visual–tactile caries examination
A-Sensible use of the probe
If the teeth are heavily covered by plaque, it may be necessary to clean the dentition before a proper caries diagnosis can be performed .Sticky adhering plaque covering a chalky/ opaque enamel lesion is strongly indicative of activity.
The probe serves two purposes: first, to remove the biofilm (using the side of the probe) to check
for signs of demineralization and surface break and, secondly, to ‘feel’ the surface texture of a lesion, as sensed through minute vibrations of the instrument by the supporting fingers when moving the tip of the probe at an angle of 20–40 degrees across the surface . It may take some training to learn this tactile skill, but once it has been acquired it is an important adjunct to the visual assessment.
A clinical caries examination performed according to these principles takes about 5–10 min, depending on the caries status of the patient.
B-Additional aids in visual–tactile caries diagnosis
1-Tooth separation
It can help to identify the presence of a cavity on contacting approximal surfaces. With this technique orthodontic elastic separators are applied for 2–3 days around the contact areas of surfaces to be diagnosed, after which access to inspection and probing .
disadvantage
1- accessibility for inspection after tooth separation is not always improved as much as needed,
2-and the use of the technique may create some discomfort, especially in patients with established dentitions.
3-it requires an extra visit.
at present the technique is not recommended for routine use in general practice.
2-Magnification
Some contemporary textbooks advocate the use of magnification in caries diagnosis. Indeed, most dentists above the age of 40 should be concerned with potential eyesight difficulties and wear glasses.
2-radiographic method
The most commonly used radiographic method for detecting caries is the bitewing technique. The purpose of bitewing examination is to detect lesions that are clinically ‘hidden’ from a careful clinical–visual examination, such as when an adjacent tooth prevents the dentist from seeing an approximal lesion. The radiograph will also help to estimate the depth of this lesion. Furthermore, bitewing radiographs should always be examined for occlusal caries in dentin.
limitations
1-not determine whether a cavity is present. As with any diagnostic method.
2-there are also inherent errors.
3-the risks of exposing a person to ionizing radiation have to be considered and balanced against the benefits of bitewing examination.
A-Bitewing with film and with digital receptors
Digital radiography is now increasingly used in clinical practice and radiography based on film may therefore not be relevant in the near future. Current digital intraoral radiography systems and recently developed fast dental films have been reported to be as accurate as traditional films for the detection of caries .
advantages of digital radiography :
1-The facilities for density and contrast enhancement can optimize the diagnostic quality and reduce retakes.
2- The radiation dose is lower.
3- No wet chemicals are involved in processing.
4- The technique is less time consuming.
B-Tuned aperture computed tomography
Recently introduced diagnostic methods based on digital radiography are tuned aperture computed tomography (TACT) and limited cone beam computed tomography.
Both methods construct radiographic slices of different thickness of teeth. The slices can be viewed for the presence of radiolucencies. In addition, the slices can be brought together in a three-dimensional computer model called a pseudohologram. These slices and pseudoholograms perform adequately in the detection of small primary and recurrent carious lesions.
Limitation:
1- performance in occlusal and approximal caries diagnosis is not significantly better than
film radiography and digital radiography .
2-the device is currently too expensive to be used in a small clinical practice.
3-Methods based on light
A-Laser light-induced fluorescence
Laser light is composed of electromagnetic waves with equal wavelengths and equal phases. Some materials possess the characteristic of fluorescence when illuminated with (laser) light. Fluorescence is a phenomenon by which the wavelength of the emitted light (coming from the light source) is changed into a larger wavelength as it travels back for detection. The larger wavelength is caused by some loss of energy to the surrounding tissue and therefore will have a different color from the emitting light. By using a filter through which only the fluorescent light may pass, the intensity of the fluorescent light can be measured. The intensity of the fluorescent light is proportional to the amount of material that causes the fluorescence.
B-DIAGNOdent
When red light with a wavelength of 655 nm is applied, caries-induced changes in teeth lead to increased fluorescence.
The DIAGNOdent is based on this principle. The fluorescent light is measured and its intensity is an indication of the depth of the caries lesion. The intensity of the fluorescent light is displayed as a number ranging from 0 to 99, with 0 indicating a minimum and 99 a maximum of fluorescent light .
Clinically visible whitespot lesions are measurable with this device.
C- Fiber-optic transillumination (FOTI)
is a diagnostic method by which visible light is transmitted through the tooth from an intense light source, e.g. from a fine probe with an exit diameter of 0.3–0.5 mm. If the transmitted light reveals a shadow when the tooth is observed from the occlusal surface this may be associated with the presence of a carious lesion. The narrow beam of light is of crucial importance when the technique is used in the premolar and
molar region. For optimal performance the probe should be brought in from the buccal or lingual aspect at an angle of about 45 degrees to the approximal surfaces pointing apically, while looking for dark shadows in the enamel or dentin . Shadows are best noticed when the office light is switched off.
Advantage:
1-a simple
2- fast
3- cheap
4- method well known to most practitioners for diagnosing approximal caries in the anterior teeth.
D- Digital imaging fiber-optic transillumination
The technique of digital imaging fiber-optic transillumination (DIFOTI) was introduced to replacing the human eye in Fiber-optic transillumination with a receptor that lesions involving over half of the enamel were better detected than lesions restricted to only the outer half of enamel for both smooth and occlusal surfaces. In other words, DIFOTI may not be able to detect small lesions, such as lesions within half of enamel thickness, and this is not as good as a visual examination .