1
طب بغداد
2015-2016
Sclera and Episclera
Applied anatomy:
The sclera: Scleral stroma is composed of collagen bundles of varying size
and shape that are not as uniformly oriented as in the cornea. The scleral stroma
is largely avascular.
Anteriorly the episclera consists of a dense vascular connective tissue, which
lies between the superficial stroma and Tenon`s capsule.
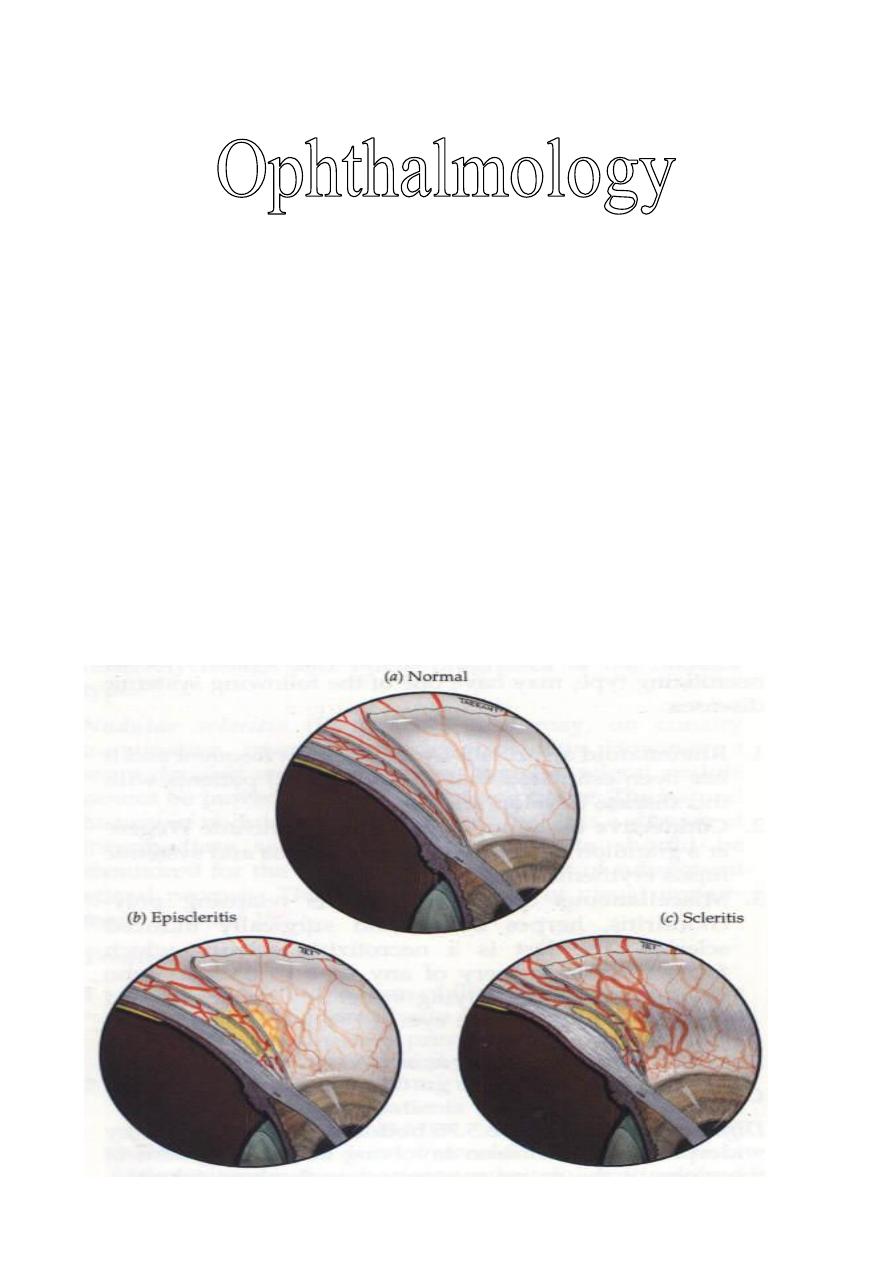
So anteriorly, there are three vascular layers that cover the anterior sclera:
1- The conjunctival vessels: The most superficial arteries, they are tortuous
and the veins are straight. Maximum congestion is seen in conjunctivitis.
2- The vessels within Tenon`s capsule: They are straight with a radial
configuration. In episcleritis, maximal congestion occurs within this vascular
plexus.
3- The deep vascular plexus: Lies in the superficial part of the sclera and
shows maximal congestion in scleritis.
* Examination in daylight is important to localize the level of maximal
injection.
Lecture: 10
Dr. Najah

2
Episcleritis
It is a common, benign, self-limiting and frequently recurrent disorder,
which typically affects young adults. Occasionally may be associated with
systemic disease but never progress to true scleritis. It is of two types: Simple
and nodular.
Presentation:
Patient is presented with unilateral redness associated with mild discomfort,
tenderness and watering eye.
Signs:
1- Simple episcleritis:
It is the commonest type, characterized by sectoral or -less commonly-
diffuse redness that resolves spontaneously within 1-2weeks.
2- Nodular episcleritis:
It is characterized by a localized, raised congested nodule which take longer
time (more than 1-2weeks) to resolve.
Treatment: (not always required unless symptoms are significant)
1- Simple lubricants or vasoconstrictors: Suffice in most mild cases.
2- Oral NSAIDs: Flurbiprofen 100 mg t.i.d for few days may be required for
severe recurrent or prolonged inflammation.
3- Topical steroids: Helpful, but increase recurrence rate.
Scleritis
It is characterized by
edema and cellular infiltration of the entire thickness of
the sclera.
Causes and associations:
1- Systemic associations: In 50% of cases.
Rheumatoid arthritis is by far the most common.
Others include: Wegener`s granulomatosis, relapsing polychondritis and
polyarteritis nodosa.
2- Surgically induced: Scleritis follows ocular surgery is typically presents
within six months post-operatively. e.g. retinal re attachment surgery.
3- Infectious: Most frequently occurs by spread of infection from a corneal
ulcer, after trauma or follow excision of a pterygium with adjunctive beta
irradiation or mitomycin C which are used to prevent recurrence of ptrygium.
The most frequent organisms are:
- Pseudomonas aeroginosa, it is difficult to be treated and has poor prognosis.
- Streptococcus pneumoniae.
- Staphylococcus aureus.
- Varicella Zoster virus.
Fungal scleritis is very rare.

3
Anatomical classification of scleritis:
1- Anterior scleritis (98%):
a- Non-necrotizing (85%): Two types; diffuse and nodular.
b- Necrotizing (13%): Also two types; with inflammation or without
inflammation.
2- Posterior scleritis (2%).
Anterior non-necrotizing scleritis
Presentation:
It is similar to episcleritis although discomfort may be more severe.
Signs:
1- Diffuse scleritis:
It is characterized by widespread inflammation involving a sector or entire
anterior sclera. The condition is relatively benign and neither progress to the
nodular type nor becomes necrotizing.
2- Nodular scleritis:
On cursory examination, it resembles nodular episcleritis, but the nodule
cannot be moved over the underlying tissue. It is of intermediate severity
(more severe than diffuse) and affects visual acuity in 25% of cases duo to its
complications.
Treatment of anterior non-necrotizing scleritis:
1- Oral NSAIDs: Such as Flubiprofen 100 mg t.i.d or meloxicam 7.5 mg t.i.d
for initial treatment.
2- Oral prednisolone: 40-80 mg daily, in patients resistant or intolerant to
NSAIDs.
3- Combined therapy: NSAIDs + low dose of steroid, in patients who
respond inadequately to either drug alone.
4- Sub Tenon`s steroid injection: Triamcinolone acetonide (long acting
steroid) 40 mg/ml is safe and effective alternative to systemic treatment.
Anterior necrotizing scleritis with inflammation
It is the most severe and distressing form of scleritis, bilateral in 60% of
cases, but not necessarily simultaneously, most patients have an associating
systemic vascular disease with mortality rate of 25% within 5 years. Visual
prognosis is poor.
Presentation:
Gradual pain and localized redness. The pain becomes severe and persistent
and radiates to the temple, brow or jaw.
4
Signs: (In chronological order)
1- Congestion of the deep vascular plexus.
2- Distortion and occlusion of blood vessels producing avascular patches.
3- Scleral necrosis.
4- Spreading of scleral necrosis.
5- Upon resolution; a bluish tinge appears secondary to scleral thinning (the
sclera becomes transparent so that the underlying choroidal pigment becomes
visible when viewed in daylight).
Complications:
1- Staphyloma formation: Bulging of the sclera secondary to severe scleral
thinning, especially if it is associated with raised intra-ocular pressure.
2- Anterior uveitis: Reflects extension of inflammation to the uvea in severe
disease causing longstanding uveitis, which may results in secondary cataracts,
glaucoma and macular edema.
Treatment of anterior necrotizing scleritis with inflammation:
1- Oral prednisolone: 60-120mg daily for 2-3 days and usually has dramatic
effect on the severity of pain, which is an important indication of active
disease. The dose tapered accordingly.
2-
Immunosuppressive
agents:
Cyclophsphamide,
azathioprine
or
cyclosporine in steroid resistant cases.
3- Combined therapy: Pulsed IV methyl prednisolone 500-1000 mg and
cyclophosphamide 500 mg. it is used in minority of patients who are:
a- Fail to resolve with oral therapy.
b- Established scleral necrosis.
Anterior necrotizing scleritis without inflammation
(Scleromalacia perforans)
Typically occurs in women with longstanding rheumatoid arthritis and is
usually bilateral.
Signs: (In chronological order)
1- Asymptomatic: yellow necrotic scleral patches in uninflamed sclera.
2- Enlargement of necrosis and spreading.
3- Scleral thinning and exposure of underlying uvea.
4- Staphyloma formation but perforation is rare unless the intraocular pressure
is elevated.
Treatment: It is ineffective.

5
Posterior scleritis
It is uncommon and often misdiagnosed because it may confused with other
inflammatory and neoplastic condition, F:M ratio is 2:1, one third of cases are
under 40 years of age at presentation.
Patients >50 years are at high risk of harboring a systemic disease and visual
loss. 2/3 of cases are unilateral, visual prognosis is guarded. There may be
extension of the inflammation to the extraocular tissues causing inflammation
of the extraocular muscles and involvement of the cranial nerves (3
rd
. 4
th
and
6
th
)
Presentation:
The most common symptoms are pain and decreased visual acuity (vision is
affected more than that in anterior scleritis). Why?
Signs:
1- External signs:
Lid oedema, proptosis and ophthalmoplegia associated anterior scleritis is
present in about one third (1/3) of cases.
2- Fundus findings:
Disc swelling, macular oedema, choroids folds (Due to pushing effect from
behind), exudative retinal detachments, choroidal detachments and subretinal
lipid exudation.
Investigations:
1- Ultrasound (U/S): Thickening (oedema and exudation) of the posterior
sclera and fluid in Tenon space giving rise to the characteristic "T-sign", the
stem of the "T" is made by the optic nerve and the upper part of "T" is made
by the thickening of the sclera.
2- CT scan: Demonstrates posterior scleral thickening.
Differential diagnosis:
1- Optic neuritis: There is disc swelling, pain and poor visual acuity.
2- Rhegmatogenous retinal detachments: A rhegmatogenous retinal
detachment (RD) occurs when fluid from the vitreous cavity passes through a
break or hole in the neurosensory retina into the potential space between the
retinal pigment epithelium (RPE) and the neurosensory retina.
3- Choroidal tumor: There is exudation, choroidal detachments and folds.
4- Orbital inflammatory disease or mass: There is proptosis, choroidal folds
causing poor visual acuity.
5- Uveal effusion syndrome: Fluid between choroids and sclera for unknown
etiology.
6- Intra-ocular lymphoma.

6
Treatment of posterior scleritis:
- In young patients: Without systemic disease, usually respond to NSAIDs.
- In elderly patients: With associated systemic disease is as for anterior
necrotizing scleritis.
The End



